Introduction
Hip fractures pose a significant risk of morbidity
and mortality to patients, resulting in high public health costs. A
previous provisional study predicted that the frequency of hip
fractures will rise exponentially with aging populations, with
4.5-6.3 million being reported annually worldwide by 2050(1). Elderly individuals tend to suffer
from severe health complaints more frequently, particularly hip
fractures (2-4).
Hip fractures in older individuals can incur not only medical
problems but can also limit their self-care abilities whilst
preventing their daily activities, because hip fractures in older
adults will most probably limit their physical activity. In
addition, aging can directly or indirectly affect the health of
older individuals and is associated with high-mortality
diseases.
Mortality is one of the most important outcomes of
hip fractures. Previous studies on hip fractures have focused on
causes, risk factors and predictors of mortality (5-8).
In an observational study, Pollmann et al (5) reported that age, sex, cognitive
impairment and the American Society of Anesthesiologists score are
risk factors of mortality in patients with hip fractures (5). In another study, Garre-Fivelsdal
et al (6) reported that a
standardized clinical pathway significantly reduced the 30-day
mortality in patients with hip fractures (6). Holvik et al (8) also reported that traumatic hip
fractures have higher mortality rates, with trauma being the most
important risk factor.
Effective mortality prediction is therefore crucial
for reducing the risk of such an event, by allowing for the prompt
management of risk factors and vital functions. Therefore, clinical
research and meta-analysis studies have previously examined the
role of neutrophil-to-lymphocyte ratio (NLR),
platelet-to-lymphocyte ratio (PLR), eosinophil-to-lymphocyte ratio
(ELR), hemoglobin-to-red cell distribution width (RDW) ratio (HRR),
mean platelet volume-to-platelet (MPV/PLT) ratio and
monocyte-to-lymphocyte ratio (MLR), in patients with orthopedic
problems (9-14).
The main objective of these ratios is to identify indicators that
could predict mortality and disease-related mortality
accurately.
It may be suggested that in order to reduce the
mortality rate and increase the quality of life after hip fracture,
indicators that can predict mortality and are more easily obtained
in the clinic are needed. Despite the existence of studies on risk
factors and mortality in patients with hip fractures, detailed
studies on the association between mortality and blood parameters
remain scarce. Therefore, the present study aimed to evaluate the
predictive value of blood parameters and ratios for predicting
mortality in patients with hip fractures.
Patients and methods
Study design
The present study was conducted in descriptive
cross-sectional and retrospective study pattern. Patient data were
retrospectively taken from patient files according to the ethical
approval frame. Ethical approval was obtained from Kütahya Health
Sciences University Non-Invasive Clinical Research Ethics Committee
(approval no. E-41997688-050.99-77929).
The present study included 758 patients with hip
fractures attempting to Department of Orthopedics and Traumatology,
Kütahya Health Sciences University Faculty of Medicine (Kütahya,
Turkey) between January 2016 and January 2023. Patient files were
accessed after ethical approval was received, between January 2023
to June 2023. Yao et al (15) reported the NLR as 6.38±4.74 for a
hip fracture population. According to this previous study, power
analysis was calculated from 10% deviation and 90% Confidence and
effect size of 0.250 was found. According to this effect size, the
minimum sample size was calculated as 175 using the G*Power 3.1.9.2
program (Heinrich-Heine-Universität Düsseldorf). In the present
study, >175, which was the calculated minimum required sample
size, was reached. The patients were divided into two groups,
namely mortality (n=464; 61.2%) and survivor (n=294; 38.8%). In
addition, patients in the mortality group were divided into the
following three subgroups: i) Those who succumbed in <1 month
(n=117; 25.2%); ii) those who succumbed between 1 and 12 months
(n=185; 39.9%); and iii) those who succumbed in >12 months
(n=162; 34.9%). In the present study, inclusion criteria were: i)
Patients having hip fractures; ii) patient files having follow up
data for research duration; and iii) patients aged ≥18 (not
pediatric samples). Exclusion criteria were: i) Patient files not
having required data for the research; ii) patients having chronic
health problems affecting results; iii) patients having malign
diseases; iv) patients having comorbidities may affect results; v)
patients having pre-existing conditions which may affect mortality
or blood parameters; and vi) infection reported patient files which
may affect blood parameters.
Data collection process
The hospital automation system and patient files
provided information on blood parameters, postoperative mortality
status, demographics and the number of surgeries performed.
However, the content of indications, information regarding
epicrisis and details on which indication was followed at which
center were unclear because the study was retrospective. Due to
this, indication-associated mortalities that were explicitly stated
as study criteria were disregarded.
Statistical analysis
Frequency analysis was used to generate descriptive
statistics for nominal and ordinal parameters, whereas means ±
standard deviations were used to describe scale parameters.
Kolmogorov-Smirnov test was used to examine the normality of scale
parameters. Fisher's exact test was used to analyze differences
between sex distributions. The U-Mann Whitney test was used for
comparing non-parametric differences, whereas the unpaired t-test
was used to analyze any parametric differences. Since there may be
regression deviations in field difference (16), Cox regression was used for
mortality prediction. Spearman's rank correlation, Cox regression
and receiver operating characteristic (ROC) analysis were used for
relationship analysis. SPSS Statistics for Windows version 25.0
(IBM Corp.) was used for analysis at 95% CI. P<0.05 was
considered to indicate a statistically significant difference.
Results
Baseline characteristics
In total, 70.7% of the surviving patients and 56.9%
of the mortality group were women. The mean age was found to be
80.84±7.03 years in the mortality group and 77.21±7.69 years in the
non-mortality group. Age was ranged between 61-96 years.
Comorbidity were exclusion criteria. Female percentage, hemoglobin
(HGB), eosinophil, lymphocyte, EOS (%), follow-up, ELR and HRR
means were found to be significantly higher in the survivor group
(P<0.05). By contrast, age, RDW coefficient of variation (CV),
MPV, MPV/PLT, NLR, MLR, PLR, mean platelet volume-to-lymphocyte
ratio (MPVLR) and monocyte-to-eosinophil ratio (MER) means were
found to be significantly higher in the mortality group
(P<0.05). The differences between monocytes, neutrophils, PLTs,
and neutrophil-to-monocyte ratios were not significant between the
two groups (Table I).
 | Table IBaseline and clinical parameters of
mortality groups and difference analysis results. |
Table I
Baseline and clinical parameters of
mortality groups and difference analysis results.
| Parameter | No (n=294) | Yes (n=464) | P-value |
|---|
| Sex, n (%) | | |
<0.001a |
|
Female | 208 (70.7) | 264 (56.9) | |
|
Male | 86 (29.3) | 200 (43.1) | |
| Age, years | 77.21±7.69 | 80.84±7.03 |
<0.001b |
| Monocytes, n
(x109/l) | 0.59±0.23 | 0.60±0.27 | 0.498b |
| RDW-CV | 14.33±2.32 | 14.89±2.20 |
<0.001b |
| Neutrophil | 8.33±3.52 | 8.51±4.00 | 0.925b |
| PLT, g/l | 225.49±75.98 | 221.41±81.12 | 0.398b |
| MPV, g/l | 9.13±0.81 | 9.56±1.04 |
<0.001b |
| HGB, g/l | 11.67±1.78 | 11.32±1.75 | 0.007c |
| Eosinophils, n
(x109/l) | 0.14±0.14 | 0.09±0.12 |
<0.001b |
| Lymphocytes, n
(x109/l) | 1.41±0.71 | 1.18±0.64 |
<0.001b |
| EOS, % | 0.14±0.14 | 0.09±0.12 |
<0.001b |
| Follow-up, days | 37.62±14.39 | 12.00±14.52 |
<0.001b |
| ELR | 0.11±0.10 | 0.08±0.10 |
<0.001b |
| HRR | 0.83±0.17 | 0.78±0.17 |
<0.001c |
| MPV/PLT | 0.04±0.02 | 0.05±0.03 | 0.011b |
| NLR | 7.59±5.14 | 9.50±6.49 |
<0.001b |
| MLR | 0.50±0.28 | 0.64±0.38 |
<0.001b |
| PLR | 191.82±94.27 | 238.07±148.53 |
<0.001b |
| MPVLR | 8.10±4.04 | 10.56±5.72 |
<0.001b |
| MER | 13.25±18.29 | 24.89±29.08 |
<0.001b |
| NMR | 15.44±7.40 | 15.89±9.21 | 0.741b |
Mortality (Table
II) was found to be correlated with RDW-CV
(rs=0.189; P<0.01), MPV (rs=0.190;
P<0.01), HGB (rs=-0.102; P<0.01), eosinophil
(rs=-0.227; P<0.01), lymphocyte
(rs=-0.181; P<0.01), EOS % (rs=-0.218;
P<0.01), follow-up (rs=-0.653; P<0.01), ELR
(rs=-0.163; P<0.01), HRR (rs=-0.169;
P<0.01), MPV/PLT (rs=0.092; P<0.01), NLR
(rs=0.135; P<0.01), MLR (rs=0.170;
P<0.01), PLR (r=0.148; P<0.01), MPVLR (rs=0.221;
P<0.01) and MER (rs=0.216; P<0.01).
 | Table IISpearman's rank correlation analysis
between mortality and parameters of patients. |
Table II
Spearman's rank correlation analysis
between mortality and parameters of patients.
| Parameter | rs | P-value |
|---|
| RDW-CV | 0.189 | <0.001 |
| MPV, g/l | 0.190 | <0.001 |
| HGB, g/l | -0.102 | 0.005 |
| Eosinophils, n
(x109/l) | -0.227 | <0.001 |
| Lymphocytes, n
(x109/l) | -0.181 | <0.001 |
| EOS, % | -0.218 | <0.001 |
| Follow-up,
days | -0.653 | <0.001 |
| ELR | -0.163 | <0.001 |
| HRR | -0.169 | <0.001 |
| MPV/PLT | 0.092 | 0.011 |
| NLR | 0.135 | <0.001 |
| MLR | 0.170 | <0.001 |
| PLR | 0.148 | <0.001 |
| MPVLR | 0.221 | <0.001 |
| MER | 0.216 | <0.001 |
Cox regression analysis results
Cox regression analysis results showed that sex
(B=-0.438; P<0.01), age (B=0.040; P<0.01), MPV (B=0.257;
P<0.01), HGB (B=0.238; P<0.01), eosinophil, EOS %
(B=-0.65.30; P<0.01), HRR (B=-4.515; P<0.01) and PLR
(B=0.001; P<0.01) can significantly affect mortality (Table III).
 | Table IIICox regression at multivariate level
for mortality and significantly associated parameters at univariate
level. |
Table III
Cox regression at multivariate level
for mortality and significantly associated parameters at univariate
level.
| | 95.0% CI for
OR |
|---|
| Parameter | B | Standard error | Wald | P-value | OR | Lower | Upper |
|---|
| Sex | -0.438 | 0.098 | 20.086 | <0.001 | 0.645 | 0.533 | 0.781 |
| Age, years | 0.040 | 0.007 | 33.482 | <0.001 | 1.040 | 1.027 | 1.054 |
| RDW-CV | -0.101 | 0.056 | 3.174 | 0.075 | 0.904 | .809 | 1.010 |
| MPV, g/l | 0.257 | 0.055 | 21.811 | <0.001 | 1.293 | 1.161 | 1.440 |
| HGB, g/l | 0.238 | 0.108 | 4.816 | 0.028 | 1.268 | 1.026 | 1.568 |
| Eosinophil | -65.350 | 18.069 | 13.081 | <0.001 | 0.000 | 0.000 | 0.000 |
| Lymphocytes, n
(x109/l) | -0.109 | 0.148 | 0.543 | 0.461 | 0.897 | .671 | 1.198 |
| EOS (%) | 65.546 | 18.012 | 13.242 | <0.001 |
2.92x1028 |
1.36x1013 |
6.28x1043 |
| ELR | -1.233 | 1.260 | 0.957 | 0.328 | 0.291 | 0.025 | 3.445 |
| HRR | -4.515 | 1.483 | 9.265 | 0.002 | 0.011 | 0.001 | 0.200 |
| MPV/PLT | 3.432 | 2.949 | 1.354 | 0.245 | 30.942 | 0.096 | 10023.797 |
| NLR | -0.006 | 0.013 | 0.241 | 0.624 | 0.994 | 0.969 | 1.019 |
| MLR | 0.013 | 0.213 | 0.004 | 0.950 | 1.013 | 0.667 | 1.539 |
| PLR | 0.001 | 0.001 | 5.044 | 0.025 | 1.001 | 1.000 | 1.003 |
| MPVLR | -0.018 | 0.019 | 0.874 | 0.350 | 0.982 | 0.945 | 1.020 |
| MER | 0.005 | 0.003 | 3.041 | 0.081 | 1.005 | 0.999 | 1.010 |
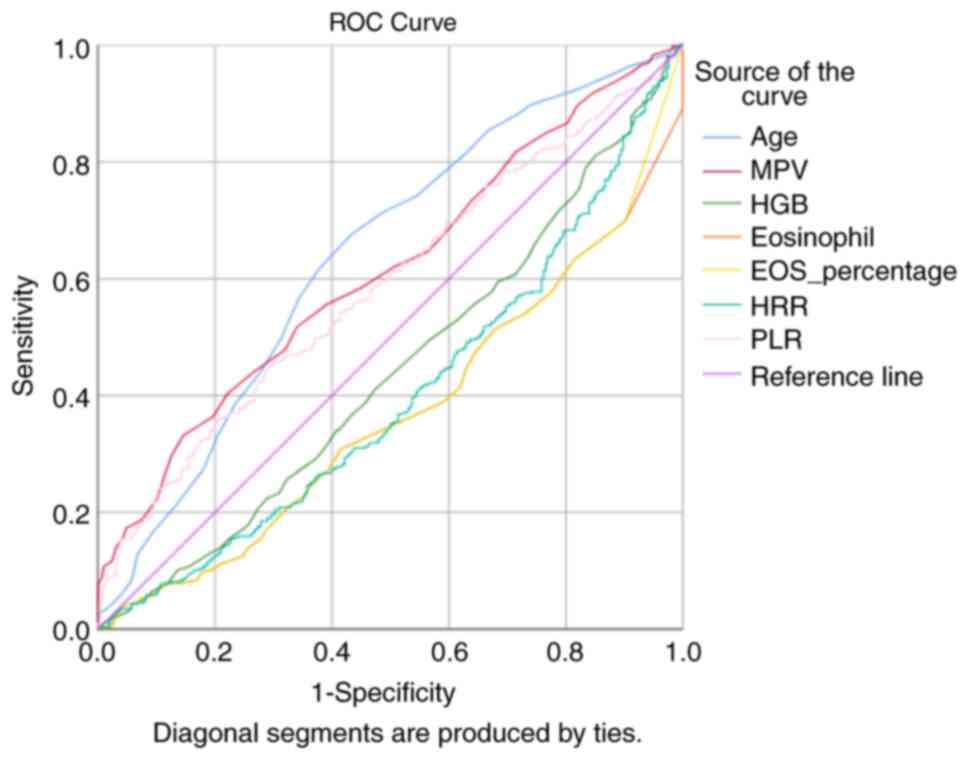
ROC analysis results
Although the predictive value of all regression
parameters following Cox regression were significant (P<0.05),
their area under the curve (AUC) values were found to be closer,
where age had the highest predictive value, followed by eosinophil,
EOS (%), MPV, HRR, PLR and HGB (Table
IV).
 | Table IVReceiver operating curve results for
significantly regressed parameters following Cox regression. |
Table IV
Receiver operating curve results for
significantly regressed parameters following Cox regression.
| | Asymptotic 95%
CI |
|---|
| Variables | Area under the
curve | Standard error | P-value | Lower bound | Upper bound |
|---|
| Age | 0.638 | 0.021 | <0.001 | 0.597 | 0.679 |
| MPV, g/l | 0.612 | 0.020 | <0.001 | 0.572 | 0.652 |
| HGB, g/l | 0.560 | 0.021 | 0.005 | 0.398 | 0.482 |
| Eosinophils, n
(x109/l) | 0.634 | 0.020 | <0.001 | 0.327 | 0.405 |
| EOS (%) | 0.628 | 0.020 | <0.001 | 0.332 | 0.411 |
| HRR | 0.600 | 0.021 | <0.001 | 0.359 | 0.441 |
| PLR | 0.587 | 0.021 | <0.001 | 0.547 | 0.628 |
An age cut-off of 74.50 years had a sensitivity of
81.5% and specificity of 37.1%, an MPV cut-off of 8.85 had a
sensitivity of 73.5% and specificity of 36.1%, an HGB cut-off of
11.05 had a sensitivity of 55.6% and specificity of 35.7%, an EOS
cut-off of 0.065 had a sensitivity of 47.6% and specificity of
35.4%, an HRR cut-off of 0.7587 had a sensitivity of 55.2% and
specificity of 30.3%, whilst a PLR cut-off of 152.6198 had a
sensitivity of 67.2% and specificity of 41.8%, for hip
fracture-related mortality (Fig.
1).
Spearman's rank correlation analysis showed that
patient parameters, namely, age (B=-0.168; P<0.01), RDW-CV
(B=-0.091; P<0.05), HGB (B=0.136; P<0.01) and HRR (B=0.155;
P<0.01), significantly correlated with mortality occurring in
<1 month (Table V).
 | Table VSpearman's rank correlation analysis
between 30-day mortality and parameters of patients. |
Table V
Spearman's rank correlation analysis
between 30-day mortality and parameters of patients.
| Mortality after
<1 month | rs | P-values |
|---|
| RDW-CV | -0.091 | 0.050 |
| MPV, g/l | -0.024 | 0.610 |
| HGB, g/l | 0.136 | 0.003 |
| Eosinophil, n
(x109/l) | 0.010 | 0.832 |
| Lymphocyte, n
(x109/l) | 0.019 | 0.690 |
| EOS (%) | 0.002 | 0.972 |
| ELR | -0.009 | 0.848 |
| HRR | 0.155 | 0.001 |
| MPV_PLT | -0.070 | 0.134 |
| NLR | -0.008 | 0.868 |
| MLR | -0.053 | 0.254 |
| PLR | 0.007 | 0.873 |
| MPVLR | -0.022 | 0.644 |
| MER | -0.016 | 0.734 |
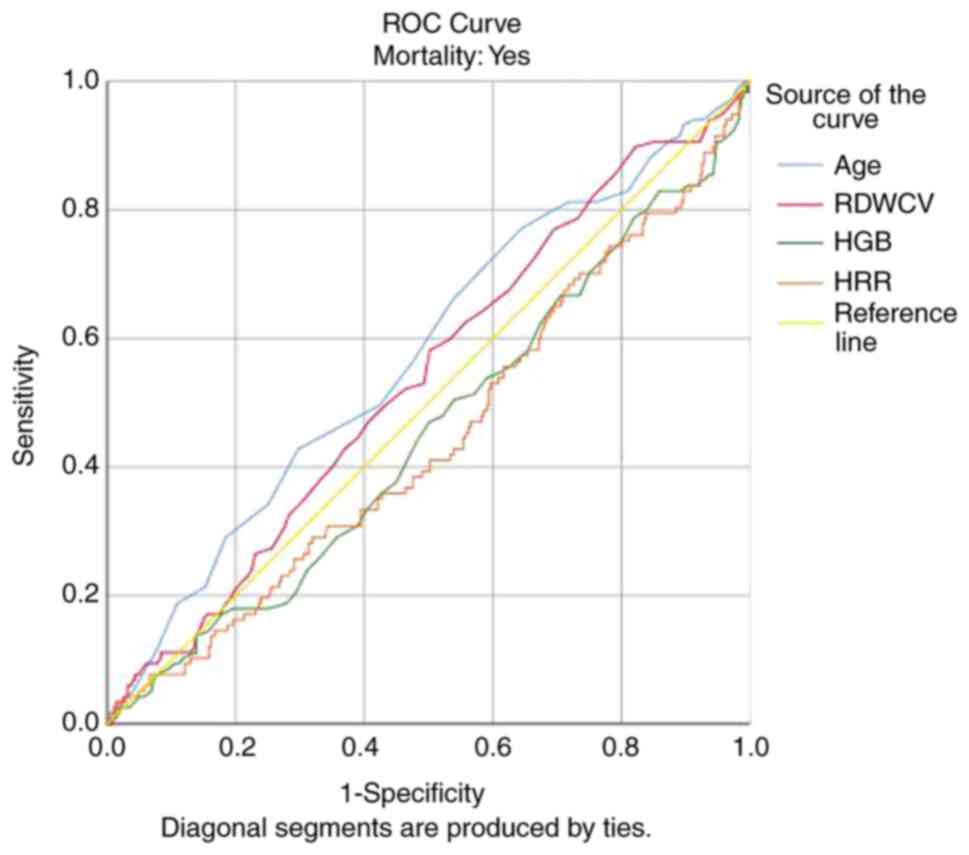
The results of the ROC curve analysis showed that
age had a predictive value for mortality occurring <1 month
after hip fractures (AUC=0.574; P<0.05; Table VI).
 | Table VIReceiver operating characteristic
curve analysis results for mortality at <1 month. |
Table VI
Receiver operating characteristic
curve analysis results for mortality at <1 month.
| | Asymptotic 95%
CI |
|---|
| Variables | Area under the
curve | Standard error | P-value | Lower bound | Upper bound |
|---|
| Age | 0.574 | 0.031 | 0.016 | 0.514 | 0.634 |
| RDW-CV | 0.539 | 0.030 | 0.211 | 0.479 | 0.598 |
| HGB, g/l | 0.453 | 0.031 | 0.126 | 0.392 | 0.514 |
| HRR | 0.445 | 0.031 | 0.074 | 0.384 | 0.506 |
An age cut-off of 79.50 years had a sensitivity of
70.9% and specificity of 41.5%, whereas an age cut-off of 83.50
years had a sensitivity of 46.2% and specificity of 64.0% for
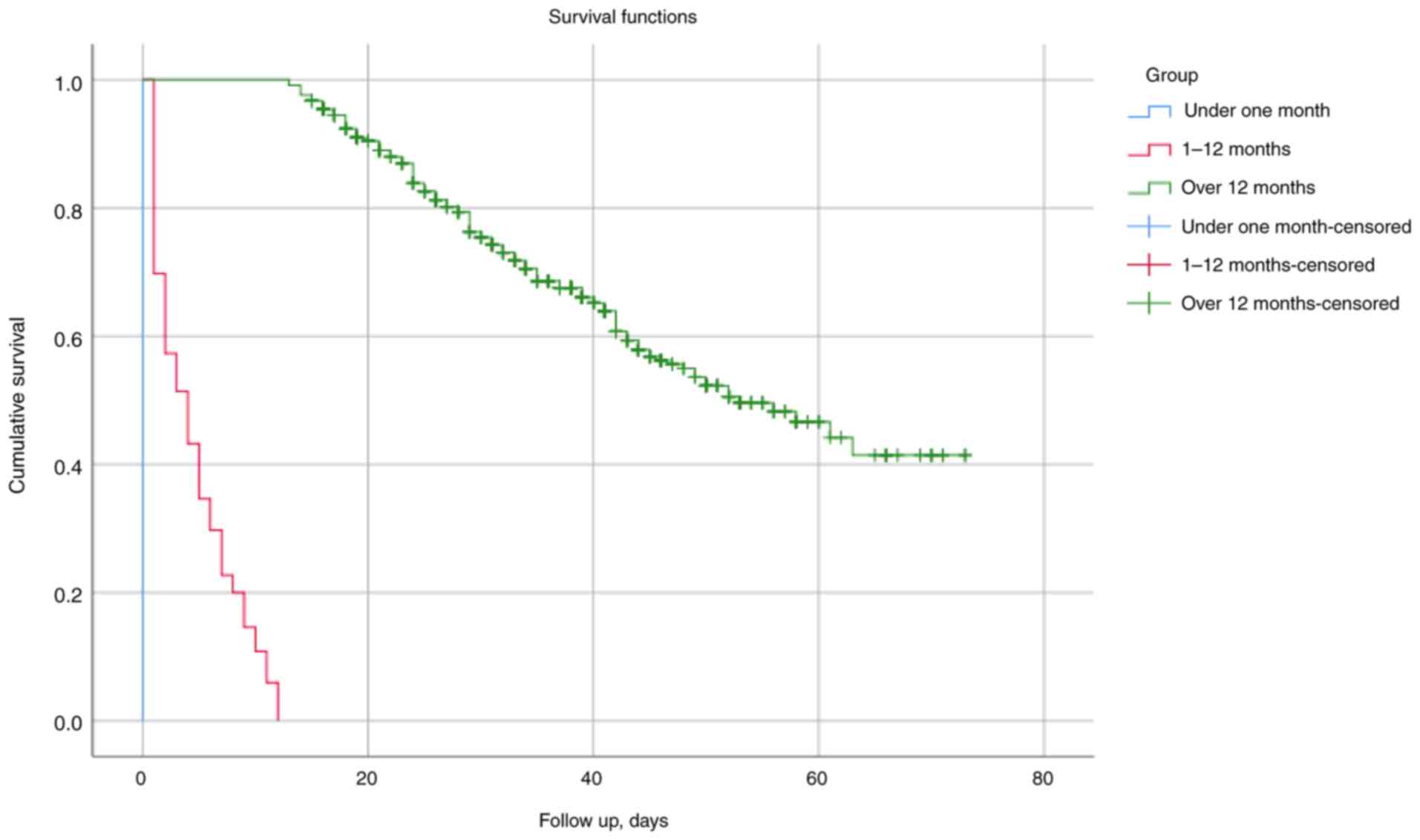
mortality occurring in <1 month (Fig. 2). Kaplan-Meier Analysis for 30-day
mortality and 1-year mortality was also shown in Fig. 3.
The sample was grouped according to the cut-off
points obtained, and these were also displayed with a cross table.
Test results for cut-off values for HLR and PLR for mortality
showed that HRR cut-off of 0.7587 had a sensitivity of 55.2% and
specificity of 30.3%, whereas a PLR cutoff of 152.6198 had a
sensitivity of 67.2% and specificity of 41.8% for hip
fracture-related mortality (Table
VII).
 | Table VIITest results for cut off values for
HLR and PLR for mortality using Fisher's exact test. |
Table VII
Test results for cut off values for
HLR and PLR for mortality using Fisher's exact test.
| | Mortality | |
|---|
| Variables | No | Yes | P-value |
|---|
| HRR <0.7587 | 89 (30.3) | 208 (44.8) | <0.001 |
| HRR >0.7587 | 205 (69.7) | 256 (55.2) | |
| PLR
<152.6198 | 123 (41.8) | 152 (32.8) | 0.007 |
| PLR
>152.6198 | 171 (58.2) | 312 (67.2) | |
Discussion
In the present study, blood parameters that can
affect hip fracture-related mortality were examined in a
multivariate analysis. Specifically, medical records of 294 and 464
patients who survived or succumbed following hip fracture surgery
were retrospectively reviewed. Blood parameter ratios and basic
blood parameters of the patients were then used to analyze
indicator rates in the literature.
Despite advancements in its diagnosis and treatment,
hip fracture-associated mortality remain a significant public
health problem (17-20).
Kjærvik et al (7)
previously reported that patients with hip fractures have a
cumulative mortality rate of 16% within the first 12 months and 41%
within 6 years (7). In another
study, Holvik et al (8)
reported a 30-day mortality of 24.3% after hip fractures (8). By contrast, Meyer et al
(3) reported a 30-day mortality
rate of 4.5-6.4% in women and 9.5-11.8% in men following hip
fracture. In the present study, the 30-day mortality rate was
reported to be 15.4%, where the 1-year mortality rate was 24.4% in
the entire sample. The rates obtained in the present study are
consistent with those of previous studies, presenting high
mortality rates following hip fracture.
Although currently no data support a specific
demographic structure for hip fractures, it may be argued that it
is more common in older, female individuals (21-23).
In a previous study by Wang et al (12), the mean age of patients with hip
fractures was 79.31 years and 66.96% of the patients were female.
In the study by Garre-Fivelsdal et al (6), the mean age of the patients was
between 80.0 and 79.7 years and the proportion of female patients
was between 66.7-65.9%. However, Pollmann et al (5) previously reported that 67.9-69.2%
patients with hip fractures were female, with a mean age of
79.6-79.7 years (5). In the
present study, the mean age of the patients was 80.84 years in the
mortality group and 77.21 years in the survivor group, of which
56.9% of the patients in the mortality group and 70.7% in the
survivor group were female. This suggests that the present results
are consistent with those of previous studies.
Previous studies have examined the prospect of using
blood parameters to estimate hip fracture-related mortality.
However, only a few variables were included in these studies
(24-26).
Wang et al (12) reported
that older patients with PLR of ≥189 are at risk of mortality
within 1 year. In the present study, the predictive value of HRR
and PLR on hip fracture-related mortality was statistically
significant. HRR had a predictive value over 30-day mortality.
Research gives important clues for hip fractures and
mortality; there are a number of confounder factors such as blood
disorders, immunological diseases and immunodeficiency disorders,
medications (especially corticosteroids) and infections. Although
an area affected by such a number of factors may seem ineffective
in terms of generalization at first glance, the large number of
cases where these factors are excluded demonstrates the clinical
value of the research results. In addition, although the research
excludes confounders, it will form a basis for gradually studying
the effects of these confounders in further research.
In the present study, changes in blood values over
time were not analyzed because of the predictive importance of
blood values at the first application. In addition, once the
patient comes to the clinic and starts receiving intervention,
there will be medications given for the determination of blood
values, follow-up period and a number of confounders; therefore,
since invasive procedures are involved, the predictive value in
blood parameters will not be reliable. Hence, blood values at the
time of application were examined predictively and
cross-sectionally.
The retrospective study design was the primary
limitation of the present study. It is difficult to follow-up
patients because of various reasons, such as difficulty in
following up hip fracture-related mortality and patients in
time-based studies frequently change healthcare institutions.
However, in prospective studies, obtaining a large sample size and
following up with patients pose significant challenges. In
addition, the present study was conducted in a single center
(Department of Orthopedics and Traumatology, Kütahya Health
Sciences University Faculty of Medicine). Within society within a
certain hospital, district and demographic structure, the lifestyle
of individuals and their health levels can show similarities.
Therefore, multicenter studies are required to take into account
the possible effects of demographic variables and different
regions. However, multicenter studies can also pose serious
problems regarding permission, procedure, data integrity and
continuity. Therefore, as in other studies, the present study
employed a single-center research design. It is also noteworthy
that the use of public hospital data in the present study is an
important limitation. Data records are not kept regularly in public
hospitals in the region and patients changing addresses or health
institutions can also be considered as a limitation.
The fact that public hospital data was used in the
research is an important limitation. Data records are not kept
regularly in public hospitals in the region and patients changing
addresses or health institutions can also be considered as a
limitation. Although in the past, only forensic cases were recorded
with regard to fractures, when clinical observations and patient
age ranges are taken into account, it may be stated that the
majority of fractures are mainly caused by falls and have high
severity.
The most notable contribution of the present study
to the field is the evaluation of indicators that may be predictive
of hip fracture-related mortality. Accordingly, the present study
aimed to predict and reduce mortality in patients with hip
fractures. This structure gives it a pragmatic feature in research
and clinical applications. In addition, the present study examined
variables that may have different abilities to predict mortality of
patients with hip fractures. To the best of the authors' knowledge,
the present study can be considered the first in the field.
Previous studies on mortality following hip fracture diagnosis have
generally focused on a few biomarkers. Finding variables and novel
indicators associated with mortality can make a positive
contribution to the field in fighting the disease and improving the
quality of life of individuals during the treatment process. Hip
fracture cases are important both because they reduce the daily
life quality of individuals and because they create a public health
burden economically. Blood parameters are routinely checked and
relatively easily obtained values. Even if there is no definitive
diagnosis regarding mortality by looking at these, giving an idea
can provide significant clinical benefit in terms of closer
follow-up of patients. In different areas, multivariate evaluation
of blood parameters, as in the present study, can provide clinical
benefit. In this respect, the research can also be a guide for
further literature studies.
To conclude, the HRR was found to have a predictive
value for hip fracture-related mortality and 30-day mortality,
whereas the PLR could only predict hip fracture-related mortality.
Predicting the risk of hip fracture-associated mortality is
crucial, particularly in older, female patients, which can possibly
be estimated with HRR and PLR. They can be readily measured in a
time efficient manner in clinical settings. By considering the
effect of other mortality-related parameters, the life expectancy
and quality of patients can be increased.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
Statistical analysis was performed by TCD and MK.
Data collection was by TCD and MK. Literature review was by AOÜ, SY
and FK. TCD and MK confirm the authenticity of all the raw data.
TCD and MK wrote the manuscript. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Ethical approval was obtained from Kütahya Health
Sciences University Non-Invasive Clinical Research Ethics
Committee, Kütahya, Turkey (approval no. E-41997688-050.99-74729).
According to research design and ethical approval, patient consent
was not required for the present retrospective study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nethander M, Coward E, Reimann E, Grahnemo
L, Gabrielsen ME and Wibom C: Estonian Biobank Research Team. Mägi
R, Funck-Brentano T, Hoff M, et al: Assessment of the genetic and
clinical determinants of hip fracture risk: Genome-wide association
and Mendelian randomization study. Cell Rep Med.
3(100776)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zhang YW, Lu PP, Li YJ, Dai GC, Chen MH,
Zhao YK, Cao MM and Rui YF: Prevalence, characteristics, and
associated risk factors of the elderly with hip fractures: A
cross-sectional analysis of NHANES 2005-2010. Clin Interv Aging.
16:177–185. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Meyer AC, Ek S, Drefahl S, Ahlbom A,
Hedström M and Modig K: Trends in hip fracture incidence,
recurrence, and survival by education and comorbidity: A Swedish
register-based study. Epidemiology. 32:425–433. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Llopis-Cardona F, Armero C, Hurtado I,
García-Sempere A, Peiró S, Rodríguez-Bernal CL and Sanfélix-Gimeno
G: Incidence of subsequent hip fracture and mortality in elderly
patients: A multistate population-based cohort study in Eastern
Spain. J Bone Miner Res. 37:1200–1208. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pollmann CT, Røtterud JH, Gjertsen JE,
Dahl FA, Lenvik O and Årøen A: Fast track hip fracture care and
mortality-an observational study of 2230 patients. BMC
Musculoskelet Disord. 20(248)2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Garre-Fivelsdal TE, Gjertsen JE, Dybvik E
and Bakken MS: A standardized clinical pathway for hip fracture
patients is associated with reduced mortality: Data from the
Norwegian hip fracture register. Eur Geriatr Med. 14:557–564.
2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kjærvik C, Gjertsen JE, Stensland E,
Saltyte-Benth J and Soereide O: Modifiable and non-modifiable risk
factors in hip fracture mortality in Norway, 2014 to 2018: A linked
multiregistry study. Bone Joint J. 104-B:884–893. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Holvik K, Ellingsen CL, Solbakken SM,
Finnes TE, Talsnes O, Grimnes G, Tell GS, Søgaard AJ and Meyer HE:
Cause-specific excess mortality after hip fracture: The Norwegian
epidemiologic osteoporosis studies (NOREPOS). BMC Geriatr.
23(201)2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chen Z, Zhao G, Chen F, Xia J and Jiang L:
The prognostic significance of the neutrophil-to-lymphocyte ratio
and the platelet-to-lymphocyte ratio in giant cell tumor of the
extremities. BMC Cancer. 19(329)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gao Z, Zhao K, Jin L, Lian X, Zhang Z, Ma
L and Hou Z: Combination of neutrophil to lymphocyte ratio,
platelet to lymphocyte ratio with plasma D-dimer level to improve
the diagnosis of deep venous thrombosis (DVT) following ankle
fracture. J Orthop Surg Res. 18(362)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yapar A, Tokgöz MA, Yapar D, Atalay İB,
Ulucaköy C and Güngör BŞ: Diagnostic and prognostic role of
neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and
lymphocyte/monocyte ratio in patients with osteosarcoma. Jt Dis
Relat Surg. 32:489–496. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wang Z, Wang H, Yang L, Jiang W, Chen X
and Liu Y: High platelet-to-lymphocyte ratio predicts poor survival
of elderly patients with hip fracture. Int Orthop. 45:13–21.
2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang Z, Wang Y, Wang Y, Chen W and Zhang
Y: Are postoperative NLR and PLR associated with the magnitude of
surgery-related trauma in young and middle-aged patients with
bicondylar tibial plateau fractures? A retrospective study. BMC
Musculoskelet Disord. 22(816)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhang X, Duan J, Wen Z, Xiong H, Chen X,
Liu Y, Liao K and Huang C: Are the derived indexes of peripheral
whole blood cell counts (NLR, PLR, LMR/MLR) clinically significant
prognostic biomarkers in multiple Myeloma? A systematic review and
meta-analysis. Front Oncol. 11(766672)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yao W, Wang W, Tang W, Lv Q and Ding W:
Neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio
(PLR), and systemic immune inflammation index (SII) to predict
postoperative pneumonia in elderly hip fracture patients. J Orthop
Surg Res. 18(673)2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yılmaz K and Turanlı M: A
multi-disciplinary investigation of linearization deviations in
different regression models. Asian J Probab Stat. 22:15–19.
2023.
|
|
17
|
Tarazona-Santabalbina FJ, Ojeda-Thies C,
Figueroa Rodríguez J, Cassinello-Ogea C and Caeiro JR:
Orthogeriatric management: Improvements in outcomes during hospital
admission due to hip fracture. Int J Environ Res Public Health.
18(3049)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Boutera A, Dybvik E, Hallan G and Gjertsen
JE: Is there a weekend effect after hip fracture surgery? A study
of 74,410 hip fractures reported to the Norwegian hip fracture
register. Acta Orthop. 91:63–68. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lewis SR, Macey R, Eardley WG, Dixon JR,
Cook J and Griffin XL: Internal fixation implants for intracapsular
hip fractures in older adults. Cochrane Database Syst Rev.
3(CD013409)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ratnasamy PP, Rudisill KE, Oghenesume OP,
Riedel MD and Grauer JN: Risk of contralateral hip fracture
following initial hip fracture among geriatric fragility fracture
patients. J Am Acad Orthop Surg Glob Res Rev.
7(e23.00001)2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Schemitsch E, Adachi JD, Brown JP, Tarride
JE, Burke N, Oliveira T and Slatkovska L: Hip fracture predicts
subsequent hip fracture: A retrospective observational study to
support a call to early hip fracture prevention efforts in
post-fracture patients. Osteoporos Int. 33:113–122. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Nijmeijer WS, Voorthuis BJ,
Groothuis-Oudshoorn CGM, Würdemann FS, van der Velde D,
Vollenbroek-Hutten MMR and Hegeman JH: Dutch Hip Fracture Audit
Taskforce Indicators Group. The prediction of early mortality
following hip fracture surgery in patients aged 90 years and older:
The Almelo hip fracture score 90 (AHFS90). Osteoporos
Int. 34:867–877. 2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ding L, Wei J and Wang B: The impact of
COVID-19 on the prevalence, mortality, and associated risk factors
for mortality in patients with hip fractures: A meta-analysis. J Am
Med Dir Assoc. 24:846–854. 2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Turgut N and Ünal AM: Standard and newly
defined prognostic factors affecting early mortality after hip
fractures. Cureus. 14(e21464)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ekinci M, Bayram S, Gunen E, Col KA,
Yildirim AM and Yilmaz M: C-reactive protein level, admission to
intensive care unit, and high American society of anesthesiologists
score affect early and late postoperative mortality in geriatric
patients with hip fracture. Hip Pelvis. 33:200–210. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Niu S, Pei Y, Hu X, Ding D and Jiang G:
Relationship between the neutrophil-to-lymphocyte ratio or
platelet-to-lymphocyte ratio and deep venous thrombosis (DVT)
following femoral neck fractures in the elderly. Front Surg.
9(1001432)2022.PubMed/NCBI View Article : Google Scholar
|