Introduction
Chronic subdural haematoma (chSDH) commonly affects
the elderly population, with the incidence reaching 7.4% in
patients >70 years old (1-3).
Although the prognosis of symptomatic chSDH after surgical
evacuation is usually favorable, the recurrence rate in several
studies was reported to reach up to 34%, with hematoma management
being challenging for the neurosurgeon (2-5).
In the literature, numerous factors were revealed to be related to
chSDH recurrence, including Glasgow Coma Scale (GCS) at admission,
anticoagulant therapy, history of dementia and stroke, hematoma
volume, and surgical technique (6-8).
With regard to surgical approaches, craniotomy with
subsequent membranectomy, twist drill craniostomy, and single or
two burr hole craniotomy with or without enlargement, +/-
irrigation and drainage have been reported in the literature with
different rates of hematoma recurrence and surgical outcome
(2,5,6,8,9). In
addition, middle meningeal artery embolization (eMMA) for the
management of symptomatic chSDH, which is a more recent strategy
for devascularization, has been proposed as an alternative
technique (10,11). However, this method may be
effective only for asymptomatic and/or limited chSDH with no clear
surgical indication (11,12). Additionally, the direct procedural
costs of eMMA are greater compared with chSDH surgical evacuation
(13).
As regards the procedure of single burr hole
surgery, the percentage of its involvement in chSDH recurrence
warrants clarification. Thus, the present study aimed to
investigate the factors related to chSDH recurrence and to evaluate
the efficacy and contribution of the single burr hole technique in
preventing hematoma recurrence.
Patients and methods
Study design and population
The present study represents a single-center,
retrospective study of chSDH cases. All included patients underwent
surgical evacuation for chSDH with single burr hole technique at
the University Hospital of Larisa, (Larisa, Greece) between January
2015 and December 2021. The Institutional Review Board of the
School of Medicine and the School of Health Sciences in the
University of Thessaly approved the present study (approval no.
2591/25-02-2022), and the decision for approval was finalized by
the 33rd General Assembly session on February 28, 2022.
In total, 166 patients (mean age, 75.8 years; 126
men and 40 women) were admitted to the University Hospital of
Larisa with chSDH and 12 (7.2%) were re-operated for hematoma
recurrence during the follow-up. Data collection was performed,
reviewed and analyzed by two physicians (GF and CG), based on the
following inclusion criteria: Patients >8 years of age that
underwent surgical hematoma evacuation with single burr hole
technique between 2015 and 2021. The exclusion criteria included:
Cases with incomplete medical files, cases lost to follow-up, or
cases in which another surgical technique was used. All
participants had a regular follow-up for 1 to 10 years from the day
of discharge from the hospital. Patient outcomes were evaluated
using a computed tomography (CT) scan and a complete neurological
examination at 24 h post-admission. Following discharge from the
hospital the patients were examined at 15 days and at 1, 2 and 3
months. Neurological improvement was characterized by the clinical
advancement in mild hemiparesis, cognitive function and
disorientation, as per the Medical Research Council (MRC) muscle
strength scale. In addition, to compare both groups, outcome
measurements such as postoperative mortality (within the first 30
days after treatment) were collected. All patients were re-operated
on only when they exhibited clinical and radiological
deterioration.
Procedure
All surgical procedures were performed under general
anesthesia or dexmedetomidine sedation in a supine position. The
single burr hole was drilled over the maximum thickness of the
hematoma. The dura matter was opened in a cruciate manner and
coagulated. The external capsule of the hematoma was coagulated and
incised. The subdural collection was then removed and evacuated
with a closed external ventricular drainage system operating in
gravity conditions placed at a low height below the patient's
bed.
Statistical analysis
Statistical analyses were performed using the
Statistical Package for the Social Sciences (SPSS version 11; SPSS,
Inc.). Data are presented as the mean ± standard deviation. The
Shapiro-Wilk test was used for the evaluation of the normality of
the distribution of variables. Fisher's exact test was used for the
categorical variables, and continuous data were evaluated with the
Mann-Whitney U test. Receiver operating characteristic (ROC)
analysis was performed to reveal the implementation of the single
burr hole technique for the surgical evacuation of chSDH in
recognition of unfavorable outcomes (neurological improvement).
P<0.05 was considered to indicate a statistically significant
difference.
Results
The patients were divided into two groups: Group A
included patients treated with surgical hematoma evacuation without
recurrence, and Group B included those who were re-operated on for
hematoma recurrence. These groups were identified based on the
following demographic, clinical, and radiographic data that were
retrieved from the medical archives when available: Age, sex,
anticoagulant therapy, type of anesthesia (general or
dexmedetomidine sedation), history of previous head trauma or brain
stroke event, presurgical imaging findings (laterality, hematoma
density and thickness, midline shift), neurological findings upon
admission (pronator drift test, gait and speech disturbances
related to chSDH), post-surgical imaging findings, history of
diabetes and hypertension, as well as dementia and recurrence
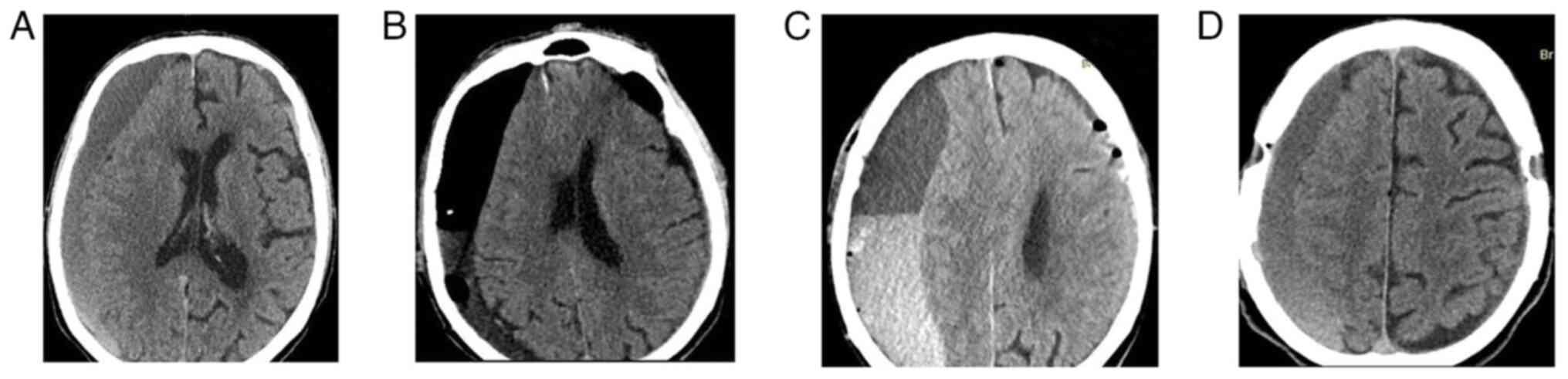
interval (Table I). A case that
was evaluated is presented in Fig.
1.
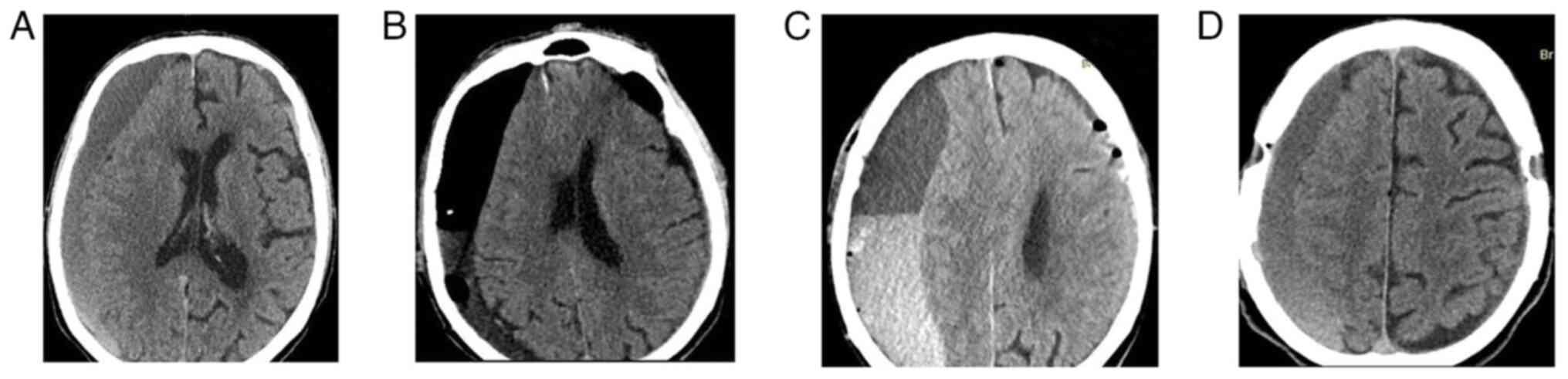 | Figure 1(A) A pre-surgical CT scan (axial
view) revealed a bilateral chronic subdural hematoma in a male
75-year old patient admitted to the Emergency Department of the
General University Hospital of Larisa (Larissa, Greece) (referral
from the peripheral hospital), with left hemiparesis, headache,
dizziness, heart disease treated with antiplatelet medication. Due
to hemiparesis the patient had an abnormal gait, with instability
that emerged from 24 h from onset of symptoms. (B) A 24-h
post-surgical CT scan (axial view) after the first bilateral
hematoma removal, under general anesthesia, with a single burr hole
technique used at both sites. (C) A CT scan (axial view) performed
a month later revealed a new hematoma forming on the right side of
the brain, and the patient was re-admitted to the ED of the General
University Hospital of Larisa, with symptoms of dizziness, headache
and hemiparesis. (D) A 24-h post-surgical CT scan (axial view)
after the recurrence of the hematoma at the right side, 30 days
later, following surgical evacuation under local anesthesia
(dexmedetomidine sedation), using a single burr hole technique
again. ED, Emergency Department, CT, computed tomography. |
 | Table IBaseline demographic characteristics
of patients with chSDH. |
Table I
Baseline demographic characteristics
of patients with chSDH.
| Parameters | All patients | Group A | Group B | P-value |
|---|
| Patients, n (%) | 166 (100.0) | 154 (92.8) | 12 (7.2) | |
| Age, mean ± SD
(years) | 75.8±10 | 75.5±10 | 79.5±9 | 0.141 |
| Sex (male), n
(%) | 126 (75.9) | 118 (71.0) | 8 (4.8) | 0.437 |
| Anticoagulant use, n
(%) | 53 (31.9) | 49 (29.5) | 4 (2.4) | 0.914 |
| Type of anesthesia, n
(%) | | | | |
|
General, n
(%) | 86 (51.8) | 77 (46.3) | 9 (5.4) | 0.095 |
|
Dexmedetomidine
sedation, n (%) | 80 (48.1) | 77 (46.3) | 3 (1.8) | |
| History of previous
head trauma event, n (%) | 145 (87.3) | 135 (81.3) | 10 (6.0) | 0.664 |
| History of brain
stroke event, n (%) | 52 (31.3) | 49 (29.5) | 3 (1.8) | 0.624 |
| Presurgical imaging
findings | | | | |
|
Laterality | | | | |
|
Left,
n (%) | 78 (46.9) | 72 (43.3) | 6 (3.6) | 0.231 |
|
Right,
n (%) | 58 (34.9) | 56 (33.7) | 2 (1.2) | |
|
Bilateral,
n (%) | 30 (18.0) | 26 (15.6) | 4 (2.4) | |
|
Hematoma
density | | | | |
|
Hypodense,
n (%) | 36 (21.6) | 35 (21.0) | 1 (0.6) | 0.244 |
|
Isodense,
n (%) | 46 (27.7) | 41 (24.6) | 5 (3.0) | 0.262 |
|
Hyperdense,
n (%) | 12 (7.2) | 10 (6.0) | 2 (1.2) | 0.190 |
|
Mixed
density, n (%) | 72 (43.3) | 68 (40.9) | 4 (2.4) | 0.466 |
|
Hematoma
thickness, mean ± SD (mm) | 16.5±3.7 | 15.8±2.5 | 25.2±4.9 | 0.001 |
|
Midline
shift, mean ± SD (mm) | 9.5±1.9 | 9.2±1.4 | 13.6±3.2 | 0.001 |
| Neurological findings
at admission | | | | |
|
Positive
pronator drift test, n (%) | 154 (92.7) | 142 (85.5) | 12 (7.2) | 0.315 |
|
Gait
disturbances, n (%) | 107 (64.4) | 98 (59.0) | 9 (5.4) | 0.428 |
|
Speech
disturbances related to chSDH, n (%) | 80 (48.1) | 72 (43.3) | 8 (4.8) | 0.184 |
| Post-surgical (24-h)
imaging findings | | | | |
|
Hematoma
thickness, mean ± SD (mm) | 7.8±2.5 | 7.4±1.7 | 12.8±5.0 | 0.001 |
|
Midline
shift, mean ± SD (mm) | 3.0±1.0 | 3.0±0.8 | 3.9±2.3 | 0.438 |
| Post-surgical
(2-month) imaging findings | | | | |
|
Hematoma
thickness, mean ± SD (mm) | 8.2±3.6 | 7.4±1.7 | 18.9±4.8 | 0.001 |
|
Midline
shift, mean ± SD (mm) | 3.4±1.8 | 3.0±0.8 | 9.1±2.1 | 0.001 |
| Diabetes mellitus,
n (%) | 38 (22.8) | 37 (22.2) | 1 (0.6) | 0.213 |
| Hypertension, n
(%) | 42 (25.3) | 40 (24.0) | 2 (1.2) | 0.475 |
| Dementia, n
(%) | 29 (17.5) | 28 (16.8) | 1 (0.6) | 0.387 |
| Recurrence
interval, mean ± SD (days) | 1.3±6.4 | 0.0±0.0 | 18.8±16.5 | 0.001 |
In total, 166 patients who underwent single burr
hole surgery for chSDH evacuation were enrolled in the present
study. Group A consisted of 154 patients (92.8%) and 12 patients
(7.2%) were included in Group B. Of the 166 included patients, 126
(75.9%) were males, and the median age was 75.8 years. The baseline
characteristics of the study participants are revealed in Table I. Patient outcomes are presented in
Table II. The recurrence interval
was 18.8±16.5 days for Group B (P=0.001), and neurological
improvement occurred in 148 out of 154 patients (96.1%) for Group A
(P=0.002).
 | Table IIOutcomes of patients after chronic
subdural hematoma. |
Table II
Outcomes of patients after chronic
subdural hematoma.
| Parameters | All patients | Group A | Group B | P-value |
|---|
| Recurrence
interval, mean ± SD (days) | 1.3±6.4 | 0.0±0.0 | 18.8±16.5 | 0.001 |
| Neurological
improvement, n (%) | 157 (94.5) | 148 (96.1) | 9(75) | 0.002 |
| Mortality, n
(%) | 4 (2.4) | 3 (1.8) | 1 (8.3) | 0.165 |
Univariate analysis for neurological improvement
revealed that there was a statistically significant difference in
the following parameters: Anticoagulant use (P=0.022), history of
brain stroke event (P=0.019), mixed hematoma density (P=0.045), and
recurrence interval (P=0.002) (Table
III).
 | Table IIIUnivariate analysis for neurological
improvement. |
Table III
Univariate analysis for neurological
improvement.
| Parameters | No improvement | With
improvement | P-value |
|---|
| Groups, n (%) | 157 (94.6) | 9 (5.4) | |
|
Group A, n
(%) | 148 (89.1) | 6 (3.6) | 0.002 |
|
Group B, n
(%) | 9 (5.4) | 3 (1.8) | |
| Age, mean ± SD
(years) | 75.6±10 | 78.6±11.5 | 0.207 |
| Sex (male), n
(%) | 120 (72.2) | 6 (3.6) | 0.505 |
| Anticoagulant use,
n (%) | 47 (28.3) | 6 (3.6) | 0.022 |
| Type of anesthesia,
n (%) | | | |
|
General, n
(%) | 81 (48.7) | 5 (3.0) | 0.817 |
|
Dexmedetomidine
sedation, n (%) | 76 (45.7) | 4 (2.4) | |
| History of previous
head trauma event, n (%) | 139 (83.7) | 6 (3.6) | 0.055 |
| History of brain
stroke event, n (%) | 46 (27.7) | 6 (3.6) | 0.019 |
| Presurgical imaging
findings | | | |
|
Laterality | | | |
|
Left,
n (%) | 74 (44.5) | 4 (2.4) | 0.073 |
|
Right,
n (%) | 57 (34.3) | 1 (0.6) | |
|
Bilateral,
n (%) | 26 (15.6) | 4 (2.4) | |
|
Hematoma
density | | | |
|
Hypodense,
n (%) | 32 (19.2) | 4 (2.4) | 0.088 |
|
Isodense,
n (%) | 44 (26.5) | 2 (1.2) | 0.705 |
|
Hyperdense,
n (%) | 10 (6.0) | 2 (1.2) | 0.074 |
|
Mixed
density, n (%) | 71 (42.7) | 1 (0.6) | 0.045 |
| Hematoma thickness,
mean ± SD (mm) | 16.3±3.4 | 18.7±6.7 | 0.531 |
| Midline shift, mean
± SD (mm) | 9.5±1.8 | 10.5±3.1 | 0.465 |
| Neurological
findings at admission | | | |
|
Positive
pronator drift test, n (%) | 146 (87.9) | 8 (4.8) | 0.644 |
|
Gait
disturbances, n (%) | 99 (59.6) | 8 (4.8) | 0.115 |
|
Speech
disturbances related to chronic subdural hematoma, n (%) | 76 (45.7) | 4 (2.4) | 0.817 |
| Post-surgical
(24-h) imaging findings | | | |
|
Hematoma
thickness, mean ± SD (mm) | 9.1±4.2 | 7.7±2.4 | 0.713 |
|
Midline
shift, mean ± SD (mm) | 3.1±1.9 | 3.0±0.9 | 0.701 |
| Post-surgical
(2-month) imaging findings | | | |
|
Hematoma
thickness, mean ± SD (mm) | 11.3±6.6 | 8.0±3.3 | 0.479 |
|
Midline
Shift, mean ± SD (mm) | 5.1±3.5 | 3.3±1.6 | 0.242 |
| Diabetes mellitus,
n (%) | 34 (20.4) | 4 (2.4) | 0.114 |
| Hypertension, n
(%) | 41 (24.6) | 1 (0.6) | 0.314 |
| Dementia, n
(%) | 26 (15.6) | 3 (1.8) | 0.197 |
| Recurrence
interval, mean ± SD (days) | 1.1±6.1 | 5.7±10 | 0.002 |
| Mortality, n
(%) | 0 (0) | 4 (2.4) | 0.001 |
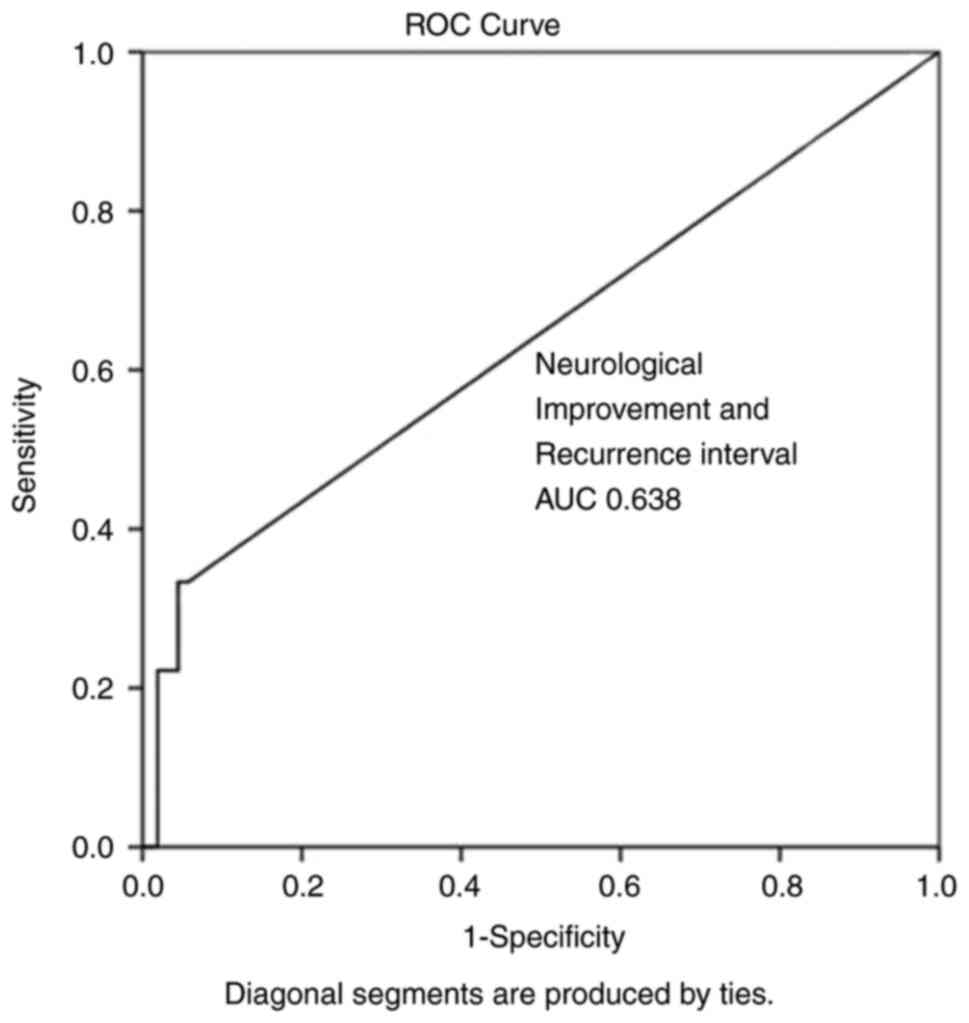
Multivariate analysis (Table IV) revealed that none of the three
parameters (anticoagulant use, history of brain stroke events, and
mixed hematoma density) alone could predict hematoma reappearance.
Overall, recurrence interval was the only independent factor
associated with chSDH recurrence (P=0.023). ROC analysis for
neurological improvement and recurrence interval demonstrated that
a recurrence interval of 16 days after the first hematoma
evacuation has better dispersion (100% sensitivity and 97.5%
specificity) as evaluated by an area under the curve standard error
[AUC(SE)] of [0.638 (0.110)] and (P=0.163) Table V and Fig. 2.
 | Table IVMultivariate analysis for
neurological improvement. |
Table IV
Multivariate analysis for
neurological improvement.
| | 95% CI for Exp
(B) |
|---|
| Parameter | P-value | Exp (B) | Lower | Upper |
|---|
| Anticoagulant use,
n (%) | 0.921 | -0.013 | -0.266 | 0.240 |
| History of brain
stroke event, n (%) | 0.500 | -0.087 | -0.341 | 0.167 |
| Mixed density, n
(%) | 0.057 | 0.066 | -0.002 | 0.134 |
| Recurrence
interval, mean ± SD (days) | 0.023 | -0.006 | -0.011 | -0.001 |
 | Table VROC analysis for Neurological
improvement. |
Table V
ROC analysis for Neurological
improvement.
| Parameters | Area | Standard error | 95% CI
lower-upper | P-value |
|---|
| Anticoagulant, n
(%) | 0.684 | 0.093 | 0.500-0.867 | 0.064 |
| History of brain
stroke event, n (%) | 0.687 | 0.093 | 0.504-0.870 | 0.060 |
| Mixed density, n
(%) | 0.329 | 0.078 | 0.176-0.483 | 0.086 |
| Recurrence
interval, mean ± SD (days) | 0.638 | 0.110 | 0.423-0.854 | 0.163 |
Discussion
In the present study, the hematoma recurrence rate
using single burr hole surgery for chSDH evacuation was 7.2%, which
was relatively small in comparison with other procedures mentioned
in the literature (1-3).
Overall, the results of the present study suggest that the patients
who underwent single burr hole surgery for chSDH evacuation had an
increased risk of hematoma recurrence, if they also used
anticoagulants, had history of a brain stroke event, and mixed
hematoma density observed in CT scans. Notably, when recurrence
occurred, the potential recurrence interval was 16 days after the
first hematoma surgical evacuation.
The mechanisms underlying postoperative recurrence
of chSDHs are multifaceted. Age-related changes in the brain may
contribute to the development of recurrence of chSDH due to the
reduced compliance of the brain (decreased elasticity and atrophic
characteristics), making it harder for the brain to recover after
hematoma removal (14,15). Therefore, damaged postoperative
brain expansion impedes the elimination of the subdural space,
leading to easier shifting of the brain (14,15).
In addition, the main reasons for recurrence after single burr hole
surgery for chSDH, include incomplete flushing, operating at the
wrong time, and poor selection of cases.
An incidentally noticed hematoma no thicker than the
width of the skull, which does not produce symptoms, can generally
be managed conservatively initially, however when symptomatic chSDH
is detected, it usually requires surgical removal (11,12).
With a reported recurrence rate as high as 34% among symptomatic
patients with surgically treated chSDH, recurrence was one of the
main outcome measures analyzed by the present study.
Along these lines, the rate of recurrence in
managing small chSDH with eMMA was found to be 9% in asymptomatic
patients (11,12).
However, the frequency of recurrent cases varies
based on the designated circumstances. The present definition was
based on the association between neurologic and radiologic findings
that was effective in determining the need for re-intervention and
which yielded a 7.2% result.
There is evidence that chSDH could develop in the
presence of potential hemorrhagic diathesis due to receiving
anticoagulation therapy (16). In
addition, recurrent hematoma in the subdural space could be caused
by hemorrhagic diathesis from the anticoagulant medication
(11,17). In the present study, anticoagulant
therapy was not demonstrated to be an independent factor for
hematoma recurrence, and only when combined with other factors
could it lead to a higher likelihood of reoperation.
There are multiple association models investigating
risk factors for chSDH recurrence (18-20).
Among the numerous factors involved in chSDH recurrence, the
density of the hematoma has been reported as an independent
predictor of recurrence. More precisely, patients with mixed chSDH
density, observed in CT scans, had a higher rate of recurrence
(21). However, in the present
study, mixed hematoma density did not prove to be an independent
factor for chSDH recurrence and was only considered in conjunction
with other factors (such as anticoagulant therapy and history of
stroke).
With regard to the time between the first surgical
evacuation of chSDH and recurrence, there is a wide range of time
intervals reported in studies, ranging from 12 to 180 days
(21,22). In the present study, if recurrence
occurred, the potential recurrence interval was 16 days after the
initial surgical removal of the hematoma. It should be noted that
the present study had several limitations. The main limitation was
that it was a single-center study performed by two neurosurgeons
who used the same surgical technique, as well as its retrospective
nature, which could lead to inaccuracies in collecting and
interpreting data from the medical records of patients. In
addition, the neurological outcome of patients after surgical
hematoma evacuation depends on the underlying initial pathology, as
most of the included patients were elderly.
In conclusion, the present study revealed that the
hematoma recurrence rate using single burr hole surgery for chSDH
evacuation was markedly low (7.2%) compared with other procedures
reported in the literature. Overall, the patients who underwent
single burr hole surgery for chSDH evacuation had an increased risk
of hematoma recurrence only when this was in combination with
anticoagulant use, history of a brain stroke event, and mixed
hematoma density observed in CT scans. If recurrence occurred, the
potential recurrence interval was 16 days after the first hematoma
surgical evacuation. The results of the present study were derived
from a single-center study; therefore, multi-center standardized
protocols are required to be developed to improve the evaluation of
patient outcomes. Furthermore, prospective data collection could
provide further insight into the value of the present study's
assessment.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
CG and GF conceptualized the study. CG, VEG, PS, NT,
DAS, GF and KNF substantially contributed to data interpretation
and analysis and wrote and prepared the draft of the manuscript. CG
and GF analyzed the data and provided critical revisions. CG and GF
confirm the authenticity of all the raw data. All authors
contributed to manuscript revision and have read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
The Institutional Review Board of the School of
Medicine and School of Health Sciences of University of Thessaly
approved (approval no. 2591/25-02-2022) the present study and the
decision was finalized by the 33rd General Assembly on 28/02/2022.
The present study was in line with the Declaration of Helsinki
(1995; as revised in Edinburgh in 2000). Written informed consent
was obtained from all the included patients for participating in
the present study.
Patient consent for publication
Written informed consent was obtained from all
included patients or their next-of-kin before surgery for the
publication of any associated images and data.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Fountas K, Kotlia P, Panagiotopoulos V and
Fotakopoulos G: The outcome after surgical vs nonsurgical treatment
of chronic subdural hematoma with dexamethasone. Interdiscip
Neurosurg. 16:70–74. 2019.
|
|
2
|
Pahatouridis D, Alexiou GA, Fotakopoulos
G, Mihos E, Zigouris A, Drosos D and Voulgaris S: Chronic subdural
haematomas: A comparative study of an enlarged single burr hole
versus double burr hole drainage. Neurosurg Rev. 36:151–154;
discussion 154-5. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Javadi A, Amirjamshidi A, Aran S and
Hosseini SH: A randomized controlled trial comparing the outcome of
burr-hole irrigation with and without drainage in the treatment of
chronic subdural hematoma: A preliminary report. World Neurosurg.
75:731–736; discussion 620-3. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lind CR, Lind CJ and Mee EW: Reduction in
the number of repeated operations for the treatment of subacute and
chronic subdural hematomas by placement of subdural drains. J
Neurosurg. 99:44–46. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Markwalder TM and Seiler RW: Chronic
subdural hematomas: To drain or not to drain? Neurosurgery.
16:185–188. 1985.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kotwica Z and Brzeziński J: Chronic
subdural haematoma treated by burr holes and closed system
drainage: Personal experience in 131 patients. Br J Neurosurg.
5:461–465. 1991.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Krupp WF and Jans PJ: Treatment of chronic
subdural haematoma with burr-hole craniostomy and closed drainage.
Br J Neurosurg. 9:619–627. 1995.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gelabert-González M, Iglesias-Pais M,
García-Allut A and Martínez-Rumbo R: Chronic subdural haematoma:
Surgical treatment and outcome in 1000 cases. Clin Neurol
Neurosurg. 107:223–229. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Hamilton MG, Frizzell JB and Tranmer BI:
Chronic subdural hematoma: The role for craniotomy reevaluated.
Neurosurgery. 33:67–72. 1993.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Di Cristofori A, Remida P, Patassini M,
Piergallini L, Buonanno R, Bruno R, Carrabba G, Pavesi G, Iaccarino
C and Giussani CG: Middle meningeal artery embolization for chronic
subdural hematomas. A systematic review of the literature focused
on indications, technical aspects, and future possible
perspectives. Surg Neurol Int. 13(94)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mehta V, Harward SC, Sankey EW, Nayar G
and Codd PJ: Evidence based diagnosis and management of chronic
subdural hematoma: A review of the literature. J Clin Neurosci.
50:7–15. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Catapano JS, Nguyen CL, Wakim AA,
Albuquerque FC and Ducruet AF: Middle meningeal artery embolization
for chronic subdural hematoma. Front Neurol.
11(557233)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Salih M, Khorasanizadeh M, McMillan N,
Gomez-Paz S, Thomas AJ, Ogilvy CS and Moore JM: Cost comparison for
open surgery versus middle meningeal artery embolization in
patients with chronic subdural hematomas: A propensity
score-matched analysis. World Neurosurg. 172:e94–e99.
2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kurokawa Y, Ishizaki E and Inaba K:
Bilateral chronic subdural hematoma cases showing rapid and
progressive aggravation. Surg Neurol. 64:444–449; discussion 449.
2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Torihashi K, Sadamasa N, Yoshida K, Narumi
O, Chin M and Yamagata S: Independent predictors for recurrence of
chronic subdural hematoma: A review of 343 consecutive surgical
cases. Neurosurgery. 63:1125–1129; discussion 1129. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yadav YR, Parihar V, Namdev H and Bajaj J:
Chronic subdural hematoma. Asian J Neurosurg. 11:330–342.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Vuk A, Stancić V, Rincić G, Ledinsky M,
Grbac L and Stancić N: Nontraumatic bilateral subdural hematoma
caused by antiaggregation therapy: Case report and review of the
literature. Acta Clin Croat. 49:163–168. 2010.PubMed/NCBI
|
|
18
|
Fang H, Zhang Z, Liu Y, Wang L, Yang Y, Li
S, Jing X, Bai G and Sheng H: Rigid neuroendoscopy assisted
hematoma resection reduces the recurrence rate of chronic subdural
hematoma with mixed density: A retrospective analytic cohort study.
Front Surg. 9(789118)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Shimizu Y, Park C and Tokuda K: Gradation
density hematoma is a predictor of chronic subdural hematoma
recurrence associated with inflammation of the outer membrane. Clin
Neurol Neurosurg. 194(105839)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Suero Molina E, Borscheid L, Freistühler
M, Zawy Alsofy S, Stummer W and Schipmann S: Risk-assessment in
chronic subdural hematoma evaluated in 148 patients-a score for
predicting recurrence. Clin Neurol Neurosurg.
195(106020)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Liu LX, Cao XD, Ren YM, Zhou LX and Yang
CH: Risk factors for recurrence of chronic subdural hematoma: A
single center experience. World Neurosurg. 132:e506–e513.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chen FM, Wang K, Xu KL, Wang L, Zhan TX,
Cheng F, Wang H, Chen ZB, Gao L and Yang XF: Predictors of acute
intracranial hemorrhage and recurrence of chronic subdural hematoma
following burr hole drainage. BMC Neurol. 20(92)2020.PubMed/NCBI View Article : Google Scholar
|