Introduction
Acquired immunodeficiency syndrome (AIDS) is one of
the most important public health problems threatening human health.
In recent years, with the development of highly active
antiretroviral therapy (HAART), the incidence of non-AIDS-defining
cancer (NADC) has increased, especially in patients with lung
cancer, and most patients are in advanced stages of NADC at the
time of diagnosis (1). Numerous
studies and case reports are based on the diagnosis of human
immunodeficiency virus (HIV) infection followed by the diagnosis of
cancer, whereas relatively few cases report diagnosis with AIDS
following the diagnosis with cancer (2,3). The
present study reported a young patient with HIV infection
complicated with lung adenocarcinoma in acute progression. This
case could serve as a reference for clinicians to understand the
disease, reduce missed diagnoses and misdiagnoses, and improve the
prognosis and quality of life of these patients.
Case report
Initial presentation
A 27-year-old male was admitted to Taihe Hospital
(Shiyan, China) in September 2023 due to intermittent chest and
abdominal discomfort for 20 days. 20 days prior to the presentation
at Taihe Hospital, the patient presented with unexplained chest and
abdominal pain and was admitted to the Department of
Gastrointestinal Surgery at a local hospital, where the patient was
diagnosed with ‘ileocecal inflammation and pleural effusion’. A
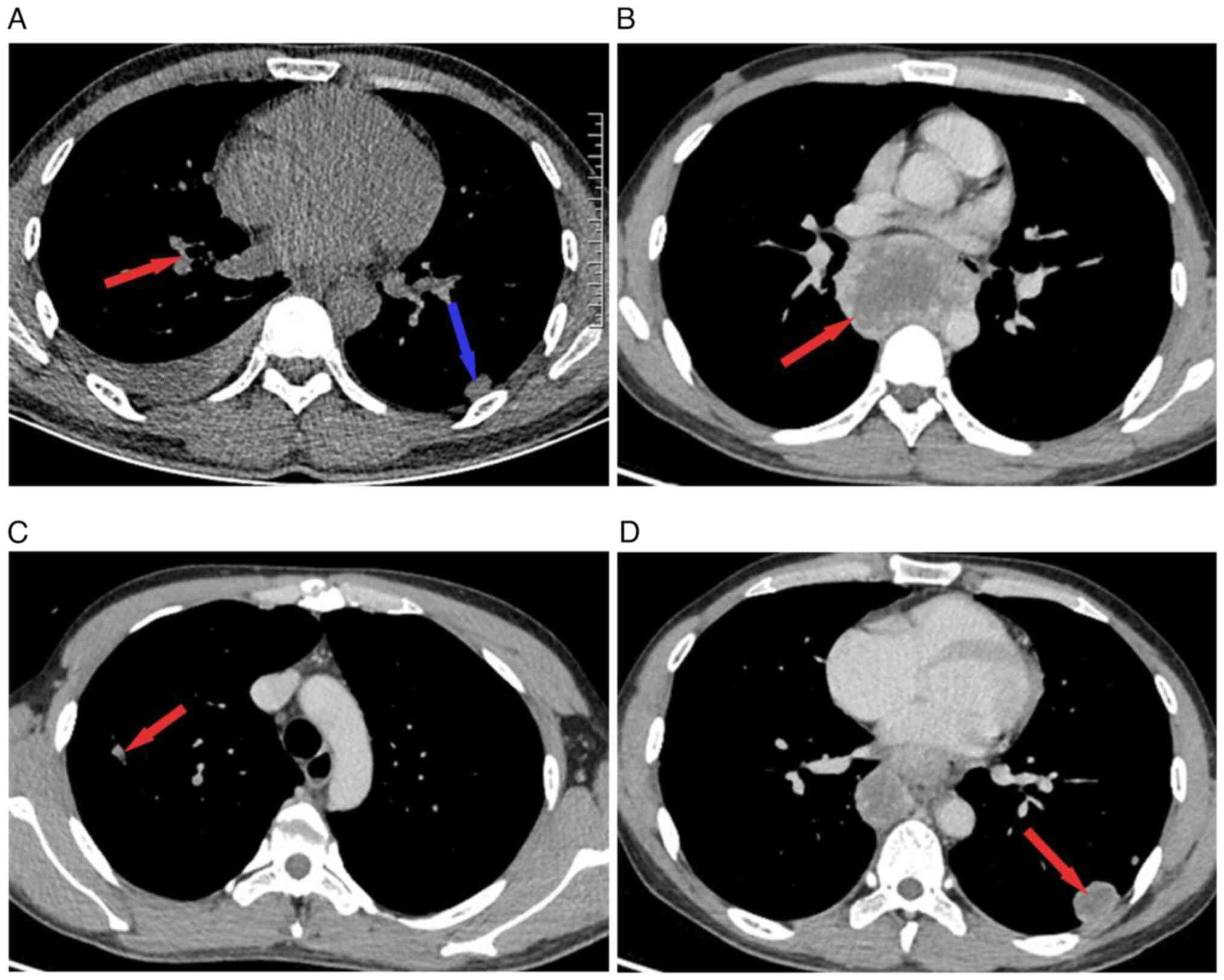
chest computed tomography (CT) scan performed at the beginning of
September, 2023, revealed nodules in the right upper lung and left
lower lung (Fig. 1A). During the
hospitalization, the patient received anti-infection treatment and
was discharged after the condition improved. However, the patient
continued to experience intermittent sternal and epigastric
discomfort outside the hospital, accompanied by nausea and
anorexia. The patient developed fever 5 days later, with a
temperature of ~38˚C, accompanied by a dry cough and no other
symptoms. The patient denied a history of smoking or drinking.
Physical examination revealed that the patient's
body temperature was 36.5˚C, pulse rate was 82 beats/min,
respiratory rate was 20 beats/min, and blood pressure was 123/82
mmHg. Table tennis-sized masses could be felt on both sides of the
neck; these masses were tough in texture, were not tender, and had
good mobility. No abnormalities were observed in other body
systems.
Diagnostic findings
In September, 2023, contrast-enhanced CT revealed
enlarged posterior mediastinal lymph nodes and multiple enlarged
mediastinal lymph nodes (Fig. 1B).
Moreover, there were multiple lesions in both lungs (Fig. 1C and D). Compared with the chest CT performed
at the other hospital, the number of lung nodules had increased and
the mediastinal lymph nodes were markedly enlarged, but the pleural
effusion had disappeared. Laboratory examination revealed the
following results: whole blood leukocytes, 5.72x109/l
[neutrophils, 75.9% (normal range, 40-75%); lymphocytes, 16.3%
(normal range, 20-50%); red blood cells, 4.30x1012/l
(normal range, 4.3-5.8x 1012/l); platelets,
233x109/l (normal range, 125-135x109/l)];
hs-CRP, 88.03 mg/l (normal range, 0-10 mg/l); NSE, 17.5 ng/ml
(normal range, 0-16.3 ng/ml); IL-6, 25.3 pg/ml (normal range, 0-6.6
pg/ml); ESR, 24 mm/h (normal range, 0-15 mm/h); and CEA (normal
range, 0-4.7 ug/l) and PCT (normal range, <0.5 ng/ml).
To clarify the nature of the mediastinal lymph node
lesions, endobronchial ultrasound-guided transbronchial needle
aspiration was performed on September, 2023, and rapid on-site
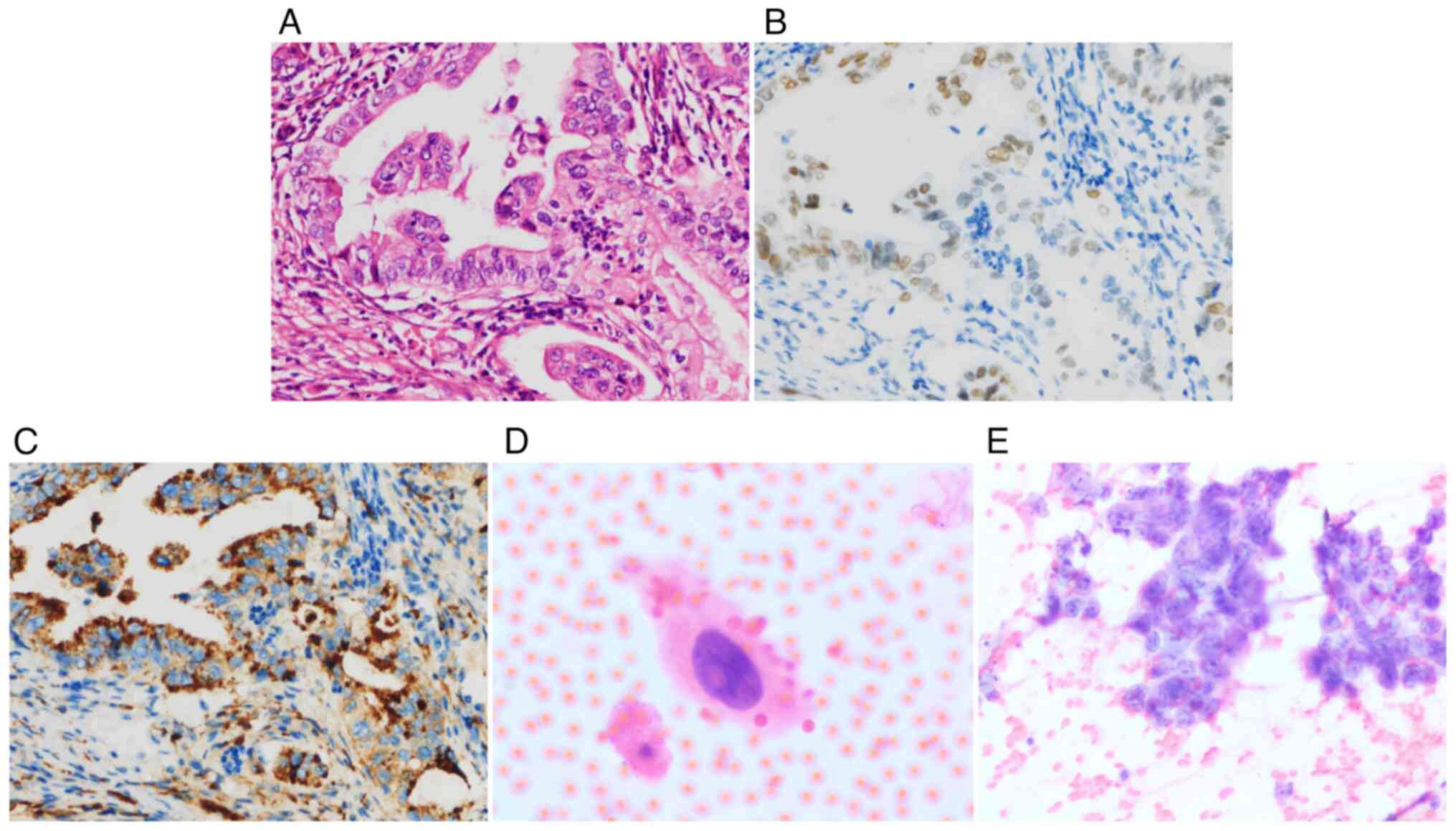
evaluation revealed adenocarcinoma. Histologically, the standard
method by hematoxylin-eosin staining at room temperature revealed a
glandular arrangement of tumor cells, and immunohistochemical
results revealed the following: CK (P(+), CK7(+), CDX2(-),
Ki-67(70%), vimentin(-), Villin(-), TTF-1(+), P63(-), CD5(-),
CD117(-), NapsinA(+), BRG1(+), Pax8(-), and CD30(-). Metastatic
pulmonary adenocarcinoma was confirmed based on the aforementioned
evidence (Figs. 2A-C and S1 and S2). In addition, fluorescence in
situ hybridization (FISH) using a digoxigenin-labeled EBER
probe (OriGene Technologies, Inc.) to detect the expression of EBER
in paraffin sections, revealed negative Epstein-Barr virus encoded
RNA (EBER) results (Fig. S3A).
Sputum Gram staining (Fig. 3B) and
bacterial culture of bronchoalveolar lavage fluid (BALF) revealed
no microorganisms. Acid-fast staining (Fig. S3C) was performed: After the three
steps of primary staining by carbolic acid (cat. no. 1400022; BaSO
Diagnostics Inc.), decolorization with ethanol hydrochloride (cat.
no. 1400022; BaSO Diagnostics Inc.), and counterstaining with
Beauty Blue (cat. no. 1400022; BaSO Diagnostics Inc.), the slides
were observed under a microscope equipped with an oil immersion
objective to observe whether red mycobacteria against a blue
background were present in the smear. Gene X-pert Mycobacterium
tuberculosis (MTB)/rifampicin (RIF) analysis was used to detect
Mycobacterium tuberculosis. The simple protocol was as
follows (4,5): The Gene Xpert MTB/RIF determination
was run on a GeneXpert Dx instrument system (GX-XVI R2; Cepheid),
which includes automated sample purification, nucleic acid
amplification, and sequencing of MTB/rifampicin nucleic acids.
After degradation, decontamination, and concentration, 0.5 ml of
resuspended sediment was transferred to a conical screw-cap tube,
1.5 ml of Xpert MTB/RIF sample reagent was added via a sterile
pipette, and the tube shaken 10-20 times. The sample was incubated
at 20-30˚C for a total of 15 min, entering the incubation period at
a point between 5 and 10 min. Next, the reagent-treated sample was
transferred to the sample chamber of the Xpert MTB/RIF column
(LOT:92008, Cepheid, USA) using a sterile pipette, and this was
then loaded into the GeneXpert Dx instrument system for sample
processing. After inputting sample-related information, the
instrument automatically filtered and washed the sample, released
DNA by ultrasonic lysis and mixed it with PCR reaction reagents,
and detected the fluorescence signal by semi-nested real-time
amplification. The instrument automatically gave the test results
after 2 h but, in this case, none of them revealed acid-fast
bacteria. Cytological examination of the BALF revealed malignant
cells (Fig. 2D). Fine-needle
aspiration smear cytology of the left cervical lymph node revealed
malignancy, which was a metastatic, poorly differentiated carcinoma
(Fig. 2F). Whole-body
18F-FDG positron emission tomography-computed tomography
revealed elevated glucose metabolism in multiple bilateral lung
nodules and a large soft tissue mass in the posterior mediastinum,
bilateral cervical multiple lymph nodes, retroperitoneal lymph
nodes, and bilateral pleural effusions (Fig. S4). Considering that the patient
was a young male and radiologically presented with rapid
progression of lung and mediastinal lesions, antibody testing for
infectious diseases was performed. Laboratory tests revealed
positive results for HIV-antibody by ELISA (Shanghai Cmbio
Company), which mainly utilizes the specific reaction between HIV
antigens and the HIV antibodies, as well as the catalytic reaction
of enzymes on substrates, to detect the HIV antibodies. It revealed
that the CD4/CD8 ratio of <0.5 (normal range, 0.80-2.40), and
CD4+ T-cell count of ≤200 cells/µl by lymphocyte immunoassay, with
a HIV viral load of 120,000 copies/ml by RT-qPCR. Based on the
positive HIV results aforementioned, we did not perform resistance
testing, western blotting, or other methods to further test for
HIV-Ab) At the end of September 2023, the patient asked to be
discharged.
The authors followed up with the patient closely and
learned that the patient had received systemic intravenous
chemotherapy (carboplatin + paclitaxel) and anti-HIV therapy
(tenofovir disoproxil, lamivudine and efavirenz) at other
hospitals. Anti-HIV regimens included tenofovir disoproxil (doses:
300 mg/QD), lamivudine (doses: 300 mg/QD), and efavirenz (doses:
400 mg/QD). However, one month later, the patient developed drug
intolerance, so tenofovir disoproxil (doses: 300 mg/QD) was
replaced with zidovudine (doses: 300 mg/BID). Afterwards, the
patient's drug intolerance improved, and the three drugs were
continuously administered orally. In addition, the patient also
received systemic intravenous chemotherapy, including carboplatin
(250 mg /m2) and paclitaxel (175 mg/m2) for
21 days. The fourth chemotherapy session ended in mid-December. The
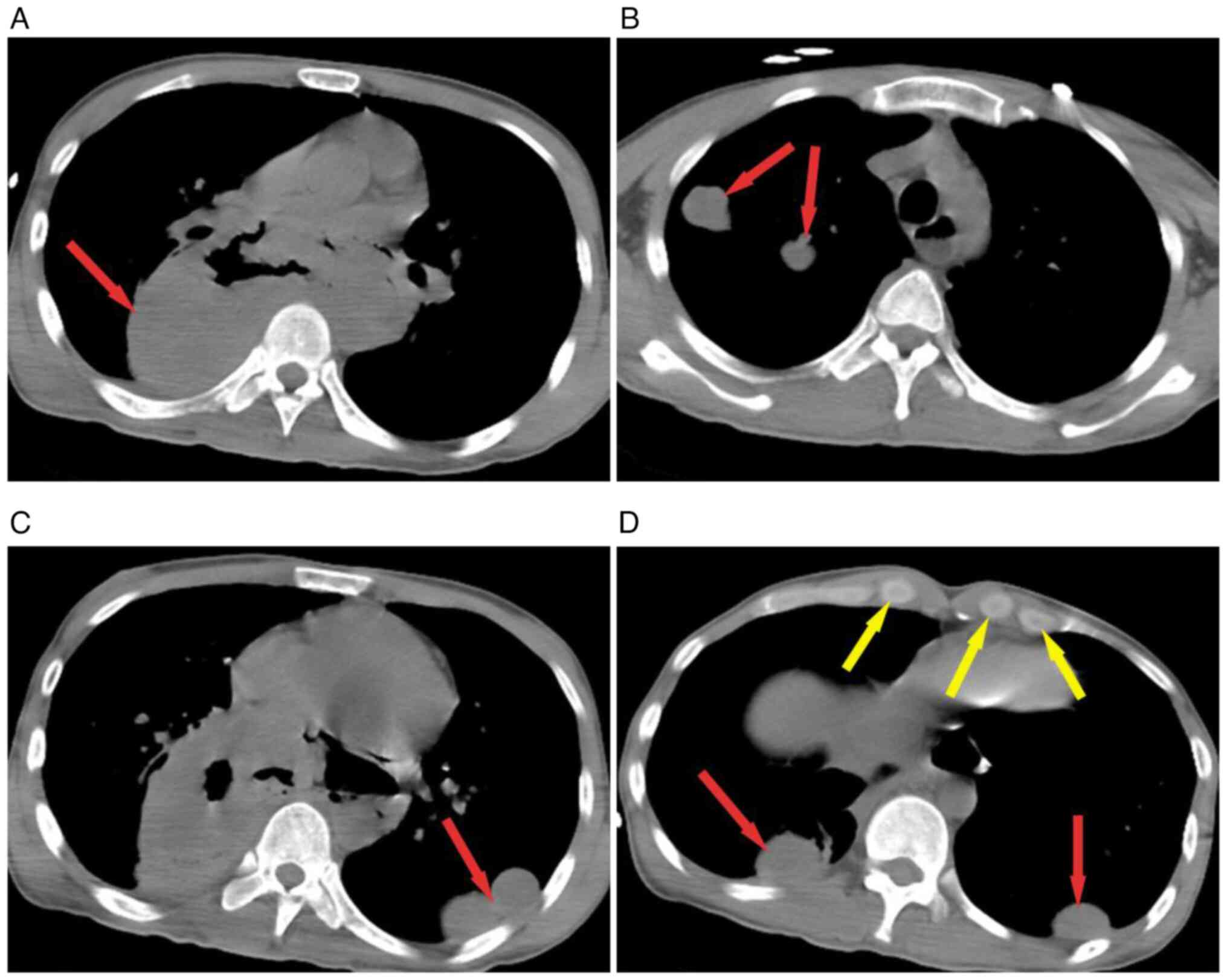
patient was readmitted to Taihe Hospital, (Hubei, China) due to
fever and dyspnea, and contrast-enhanced CT of the chest revealed
carcinoma metastasis in both the lungs and mediastinum, including
the bilateral supraclavicular lymph node. A markedly enlarged
posterior mediastinal mass with air accumulation (esophageal
fistula?) was noted (Fig. 3).
Subsequently, an esophago-mediastinal fistula was confirmed by
esophagography. Septic shock was cured with antibiotics (Merpenem,
1 g, iv, Q8h + teicoplanin, 0.4 g, iv, QD), intravenous nutritional
support, fluid resuscitation and multiorgan system life support,
but intermittent fever was still present. The patient was
discharged after five days and transferred to an infectious disease
hospital for further treatment. Then the patient was lost to
follow-up after 5 months.
Discussion
To further study AIDS in modern medical treatment,
HIV infection combined with malignant tumors is becoming
increasingly common in clinical practice. AIDS-related cancers are
currently divided into AIDS-defining cancers and NADCs. In terms of
AIDS epidemiology, Kaposi's sarcoma, non-Hodgkin's lymphoma, and
cervical cancer are the main types of cancer (6) and are associated with the immune
deficiency status of infected individuals (7,8). In
recent years, the risk of lung cancer, Hodgkin's disease, skin
cancer, anal cancer, and gastrointestinal cancer has increased in
numerous of those living with HIV (PLWH) compared with uninfected
numerous (9). According to two
meta-analyses, standardized incidence ratios for lung cancer were
>2.5 higher in PLWH than in non-HIV patients (7,10).
Studies have suggested that the risk of lung cancer among PLWH
mainly occurs among those aged ≥60 years; however, the risk of lung
cancer is higher among younger age groups (aged 20-49 years)
compared with the general population (11). Despite the increasing number of
HIV-positive patients, most HIV-positive cancer patients without
typical clinical symptoms of AIDS are diagnosed with HIV infection
during hospital visits due to tumors.
The specific cause of HIV infection complicated with
lung cancer is unknown, but almost all studies on lung cancer in
HIV-infected individuals have shown that smoking is an important
risk factor for lung cancer in these individuals. In addition, a
study by Mena et al (12)
suggests that pulmonary infection, immunosuppression and chronic
inflammation, such as in HIV infection, increase the risk of lung
cancer. A large retrospective study (3) confirmed that HIV infection was an
independent risk factor for lung cancer after the exclusion of
major confounding factors such as age and smoking. This may be
associated with HIV causing immune deficiency, which leads to
tumorigenesis. HIV generally affects the innate immune system of
the lungs by infecting airway epithelial cells, alveolar
surface-active proteins, alveolar macrophages, dendritic cells, and
natural killer cells. In addition, it can affect the acquired
immune system of the lungs by causing damage to T cells and
increasing the activation of B cells through immune activation and
immunosuppression (13). In the
present case, the patient had neither a history of smoking nor
chronic lung inflammation and the cause of lung cancer may have
been related to the destruction of cellular immunity following HIV
infection. The progression period of lung cancer lesions in immune
normal patients is ~2 months, whereas the progression of lesions in
HIV-infected patients is faster, usually 3-4 weeks. In this case,
an HIV test was performed and confirmed HIV positivity with
radiology, revealing that the patient's lung cancer was progressing
rapidly. Therefore, HIV screening is necessary when rapidly
progressing lung malignancies are encountered in clinical
practice.
A study of 3,426 HIV-infected patients with lung
cancer revealed that the most common histological subtype was
adenocarcinoma, followed by squamous cell carcinoma, small cell
carcinoma and large cell carcinoma (11), which, as in the present case, is
pathologically confirmed as adenocarcinoma. Most HIV-infected
patients are already in locally advanced or metastatic cancer
(stage III B or IV) when they are diagnosed with lung cancer
(14). The radiological
characteristics of patients with HIV infection complicated with
lung cancer were not markedly different from those of patients with
lung cancer alone. Additionally, most HIV-infected lung cancer
patients present with nonspecific respiratory symptoms such as
cough, chest pain and dyspnea (14). However, unlike previous reports in
the literature, the patient in the present case presented with
chest and abdominal pain and cough. In September, 2023, a chest CT
revealed a large mass in the posterior mediastinum, which was
markedly larger than that observed at the previous hospital. In
December, the giant mediastinal mass was enlarged, accompanied by
pneumatosis and an esophago-mediastinal fistula. While such rapidly
progressing cases are relatively rare, in clinical practice,
HIV-associated lung infections are relatively common, especially in
patients with low-risk lung cancer and it is easy for
pulmonologists or radiologists to overlook the possibility of lung
malignancy when referring to chest CT (14). As the patient in our case had
low-risk factors for lung cancer, including age, no history of
smoking, and no underlying disease of the lung, it was easy to miss
HIV-related lung cancer. As in the present case, the possibility of
HIV infection was not considered before the diagnosis of lung
cancer. In addition, according to the laboratory results, the
patient's CD4+ T-cell count was ≤200 cells/µl, and the CD4/CD8
ratio was abnormal.
Survival is reportedly prolonged following treatment
when CD4+ T-cell counts in HIV-infected patients with
non-small cell lung cancer (NSCLC) are ≥200 cells/µl (15). However, when the CD4+ T-cell count
is <200 cells/µl, the RRs for lung cancer are markedly elevated
(16). Therefore, when diagnosing
HIV-associated lung cancer, it should be systematically considered
that patients should be protected against other opportunistic
infections when initiating therapy, regardless of the
CD4+ T-cell count. In the present case, lung cancer
progressed rapidly, and it is unknown whether there was a
significant decrease in CD4+ T cells that led to an
opportunistic infection. After four rounds of chemotherapy,
tracheal mediastinal fistula and septic shock occurred. With
aggressive symptomatic treatment, the shock was reversed. According
to the international consensus definition of severe lung cancer,
due to various acute or chronic comorbidities, the tumor itself
and/or treatment-related adverse events cause performance status
(PS) scores between 2 and 4, but following supportive treatment and
antitumor therapy, survival benefits and/or improved PS scores are
achieved. Therefore, it was considered that the patient's lung
malignancy reached the diagnostic criteria for severe lung cancer
(17).
Currently, the treatments for lung cancer include
surgery, radiotherapy, chemotherapy, targeted drug therapy, and
immunotherapy, while HAART is still the first-line treatment for
AIDS. For patients with HIV infection complicated with lung cancer,
there is currently no unified treatment. Surgical treatment,
radiation therapy, chemotherapy, targeted therapy and immunotherapy
are recommended. However, the advantages and disadvantages of these
options need to be discussed and the selection should be based on
the patient's physical condition. After definite diagnosis and
staging, the patient was recommended to undergo systemic
chemotherapy immediately but was diagnosed with HIV infection
before antitumor therapy. Specific treatment regimens for
HIV-associated lung cancer are not extensively detailed in most of
the literature. However, a previous case report mentioned a
59-year-old male patient who received cisplatin/vinorelbine
chemotherapy combined with raltegravir for anti-HIV therapy
(18). Marcus et al
(19) reported that if the
co-occurrence of lung cancer and HIV infection is identified,
antiretroviral therapy should be performed as early as possible
following antineoplastic therapy has been initiated if the
patient's condition is stable. Studies have indicated that patients
receiving a combination of antineoplastic agents and HAART achieve
improved remission and survival rates compared with those treated
with chemotherapy alone (20,21).
The patient in the present case received systemic chemotherapy for
antitumor and anti-HIV therapy at another hospital, which had poor
tolerability and poor efficacy. In late December, the patient was
readmitted to Taihe Hospital (Hubei, China) with sepsis, which
illustrates the complexity and individuality of treatment for this
disease. Regarding the prognosis of HIV-infected patients with lung
cancer, Sigel et al (22)
reported that the median overall survival of patients with HIV and
NSCLC was 6 months [95% confidence interval (CI): 5-8 months]. The
present patient has been followed for more than 5 months since
onset and the prognosis is poor.
Based on the present case, other NADCs were
compared. As shown in a study of HIV with breast carcinoma, the age
at the cancer diagnosis was ~20 years younger in the HIV/AIDS
population than in the general population. While it is similar to
lung cancer, there was no direct association between breast
carcinoma and the viral load or CD4+ T-cell count (23). In PLWH, hepatocellular carcinoma is
often diagnosed in the late stage, and the prognosis is affected by
the CD4+ T-cell count and immunosuppression, as in lung cancer
(24). For patients with rapidly
progressing cancer, relevant studies suggest that this may be due
to HIV viral infection shaping and influencing the tumor immune
microenvironment in cancer patients. HIV patients have difficulty
mounting an effective anticancer immune response, as T cells become
exhausted due to the high expression of multiple negative
checkpoint receptors (25,26). HIV-infected individuals are at
increased risk for lung cancer, but routine prevention of the
occurrence and progression of the disease remains a challenge.
The present case differs from previous cases of
HIV-associated cancers as it involves rapidly progressing lung
adenocarcinoma. When investigating the cause of the rapid
progression, it was found that the patient was HIV-positive.
Therefore, for young patients with rapidly progressing malignant
lung tumors, it is crucial to be vigilant about the possibility of
HIV infection. Timely screening and appropriate treatment are
essential. Based on the present study and associated risk factors,
smoking cessation and low-dose CT screening are necessary (27). In clinical practice, patients
suspected of having lung cancer by chest radiology should be
considered according to radiological and clinical characteristics
and young age should not be used as an exclusive diagnostic
standard as. For those with rapid progress, HIV screening should be
performed to avoid misdiagnosis and missed diagnosis. Once patients
are diagnosed with HIV complicated with lung cancer, they should be
treated as early as possible to improve their quality of life and
prolong survival (28).
Supplementary Material
Immunohistochemical staining results
(magnification, x200). immunohistochemical staining of tumor tissue
revealed positive reaction for CK (P), CK7 and Ki-67(70%); while
negative for CDX2, vimentin and Villin.
Immunohistochemical staining results
(magnification, x200). immunohistochemical staining of tumor tissue
revealed positive reaction for BRG1; while negative for P63, CD5,
CD117, Pax8 and CD30.
FISH, Gram stain and acid-fast stain
results. (A) FISH revealed negative EBER results (magnification,
x200). (B) Gram stain (magnification, x400) and (C) acid-fast stain
(magnification, x400) of sputum smear revealed no pathogenic
microorganisms. FISH, fluorescence in situ hybridization; EBER,
Epstein-Barr virus early RNA.
Positron emission tomography revealed
multiple masses in both lung with an elevated glucose uptake. (A) A
mass in the right lung revealed elevated glucose uptake. (B) A
subpleural mass in the left lung revealed elevated glucose
uptake.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
TZ and MW executed the conception or design of the
written study. TZ and HW drafted the manuscript and performed data
acquisition, analysis or interpretation for the study. WH and XQ
made contributions to the interpretation of the data for the work
and critically revised the manuscript for important intellectual
content. QL and TR collected pathological and surgical data from
the patient. WH and QL assisted in updating patient follow-up
information and the literature search. MW, TZ and HW confirmed the
authenticity of all the raw data. All authors read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sigel K, Makinson A and Thaler J: Lung
cancer in persons with HIV. Curr Opin HIV AIDS. 12:31–38.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Burke M, Furman A, Hoffman M, Marmor S,
Blum A and Yust I: Lung cancer in patients with HIV infection: Is
it AIDS-related? Hiv Med. 5:110–114. 2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sigel K, Wisnivesky J, Gordon K, Dubrow R,
Justice A, Brown ST, Goulet J, Butt AA, Crystal S, Rimland D, et
al: HIV as an independent risk factor for incident lung cancer.
AIDS. 26:1017–1025. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kohli M, Schiller I, Dendukuri N, Dheda K,
Denkinger CM, Schumacher SG and Steingart KR: Xpert®
MTB/RIF assay for extrapulmonary tuberculosis and rifampicin
resistance. Cochrane Database Syst Rev. 8(CD012768)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Liu Q, Chen X, Dai X, Liu X, Xu F and Peng
P: Comparative analysis of five inspection techniques for the
application in the diagnosis and treatment of osteoarticular
tuberculosis. Int J Infect Dis. 112:258–263. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Micali C, Russotto Y, Facciolà A, Marino
A, Celesia BM, Pistarà E, Caci G, Nunnari G, Pellicanò GF and
Venanzi Rullo E: Pulmonary kaposi sarcoma without respiratory
symptoms and skin lesions in an HIV-Naïve patient: A case report
and literature review. Infect Dis Rep. 14:228–242. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Grulich AE, Van-Leeuwen MT, Falster MO and
Vajdic CM: Incidence of cancers in people with HIV/AIDS compared
with immunosuppressed transplant recipients: A meta-analysis.
Lancet. 370:59–67. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Pavone G, Marino A, Fisicaro V, Motta L,
Spata A, Martorana F, Spampinato S, Celesia BM, Cacopardo B,
Vigneri P and Nunnari G: Entangled connections: HIV and HPV
interplay in cervical cancer-a comprehensive review. Int J Mol Sci.
25(10358)2024.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yarchoan R and Uldrick TS: HIV-associated
cancers and related diseases. N Engl J Med. 378:1029–1041.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shiels MS, Cole SR, Kirk GD and Poole C: A
meta-analysis of the incidence of non-AIDS cancers in HIV-infected
individuals. J Acquir Immune Defic Syndr. 52:611–622.
2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Haas CB, Engels EA, Horner MJ, Freedman
ND, Luo Q, Gershman S, Qiao B, Pfeiffer RM and Shiels MS: Trends
and risk of lung cancer among people living with HIV in the USA: A
population-based registry linkage study. Lancet HIV. 9:e700–e708.
2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Mena Á, Meijide H and Marcos PJ: Lung
cancer in HIV-infected patients. AIDS Rev. 18:138–144.
2016.PubMed/NCBI
|
|
13
|
Cribbs SK, Crothers K and Morris A:
Pathogenesis of HIV-related lung disease: Immunity, infection, and
inflammation. Physiol Rev. 100:603–632. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mani D, Haigentz M Jr and Aboulafia DM:
Lung cancer in HIV infection. Clin Lung Cancer. 13:6–13.
2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Makinson A, Tenon JC, Eymard-Duvernay S,
Pujol JL, Allavena C, Cuzin L, Poizot-Martin I, de la Tribonnière
X, Cabié A, Pugliese P, et al: Human immunodeficiency virus
infection and non-small cell lung cancer: Survival and toxicity of
antineoplastic chemotherapy in a cohort study. J Thorac Oncol.
6:1022–1029. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Silverberg MJ, Chao C, Leyden WA, Xu L,
Horberg MA, Klein D, Towner WJ, Dubrow R, Quesenberry CP Jr,
Neugebauer RS and Abrams DI: HIV infection, immunodeficiency, viral
replication, and the risk of cancer. Cancer Epidemiol Biomarkers
Prev. 20:2551–2559. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhou C, Li S, Liu J, Chu Q, Miao L, Cai L,
Cai X, Chen Y, Cui F, Dong Y, et al: International consensus on
severe lung cancer-the first edition. Transl Lung Cancer Res.
10:2633–2666. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Okuma Y, Hosomi Y and Imamura A: Lung
cancer patients harboring epidermal growth factor receptor mutation
among those infected by human immunodeficiency virus. Onco Targets
Ther. 8:111–115. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Marcus JL, Chao C, Leyden WA, Xu L, Yu J,
Horberg MA, Klein D, Towner WJ, Quesenberry CP Jr, Abrams DI and
Silverberg MJ: Survival among HIV-infected and HIV-uninfected
individuals with common non-AIDS-defining cancers. Cancer Epidemiol
Biomarkers Prev. 24:1167–1173. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Berretta M, Caraglia M, Martellotta F,
Zappavigna S, Lombardi A, Fierro C, Atripaldi L, Muto T, Valente D,
De Paoli P, et al: Drug-drug interactions based on pharmacogenetic
profile between highly active antiretroviral therapy and
antiblastic chemotherapy in cancer patients with HIV infection.
Front Pharmacol. 7(71)2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ntekim AI and Folasire AM: CD4 count and
anti retroviral therapy for HIV positive patients with cancer in
nigeria-a pilot study. Clin Med Insights Oncol. 4:61–66.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sigel K, Crothers K, Dubrow R, Krauskopf
K, Jao J, Sigel C, Moskowitz A and Wisnivesky J: Prognosis in
HIV-infected patients with non-small cell lung cancer. Br J Cancer.
109:1974–1980. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Marino A, Pavone G, Martorana F, Fisicaro
V, Motta L, Spampinato S, Celesia BM, Cacopardo B, Vigneri P and
Nunnari G: Navigating the nexus: HIV and breast cancer-a critical
review. Int J Mol Sci. 25(3222)2024.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Micali C, Russotto Y, Caci G, Ceccarelli
M, Marino A, Celesia BM, Pellicanò GF, Nunnari G and Venanzi Rullo
E: Loco-regional treatments for hepatocellular carcinoma in people
living with HIV. Infect Dis Rep. 14:43–55. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mylvaganam G, Yanez AG, Maus M and Walker
BD: Toward T cell-mediated control or elimination of HIV
reservoirs: Lessons from cancer immunology. Front Immunol.
10(2109)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Huang SH, McCann CD, Mota TM, Wang C,
Lipkin SM and Jones RB: Have cells harboring the HIV reservoir been
immunoedited? Front Immunol. 10(1842)2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Makinson A, Eymard-Duvernay S, Raffi F,
Abgrall S, Bommart S, Zucman D, Valour F, Cheret A, Poizot-Martin
I, Duvivier C, et al: Feasibility and efficacy of early lung cancer
diagnosis with chest computed tomography in HIV-infected smokers.
AIDS. 30:573–582. 2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
El Zarif T, Nassar AH, Adib E, Fitzgerald
BG, Huang J, Mouhieddine TH, Rubinstein PG, Nonato T, McKay RR, Li
M, et al: Safety and activity of immune checkpoint inhibitors in
people living with HIV and CANCER: A real-world report from the
cancer therapy using checkpoint inhibitors in people living with
HIV-international (CATCH-IT) consortium. J Clin Oncol.
41:3712–3723. 2023.PubMed/NCBI View Article : Google Scholar
|