Introduction
Thyroid diseases encompass a spectrum of conditions,
ranging from aberrant growth disorders, such as benign nodules and
cancer, to hormonal disorders, including hypothyroidism,
hyperthyroidism and thyroid storm (TS). TS is a life-threatening
exacerbation of the hyperthyroid state (1). The primary characteristic of TS is
multi-organ dysfunction that can involve the cardiovascular,
thermoregulatory, gastrointestinal-hepatic and central nervous
systems (2,3). The incidence of TS is difficult to
approximate because of its rarity and absence of universally
approved criteria for its diagnosis (4-6).
At present, the diagnosis of TS is based on laboratory tests [low
to undetectable thyroid-stimulating hormone (TSH) <0.01 µIU/ml
with elevated free thyroxine and free triiodothyronine], coupled
with the presence of severe signs and symptoms, including
hyperpyrexia, cardiovascular dysfunction, gastrointestinal symptoms
and altered mental status (2,3). At
present, there are two scoring systems that may assist, including
the Burch-Wartofsky Point Scale (BWPS) and the Japan Thyroid
Association criteria (2,3). The main treatment method for TS is
medical management, including antithyroid drugs (propylthiouracil
and methimazole), iodine, glucocorticoids and β-adrenergic blockers
(7).
Acute airway obstruction is a life-threatening
disease that requires emergency intervention (8,9).
Acute airway obstructions induced by thyroid lesions are mostly
attributed to poorly differentiated and anaplastic thyroid
malignancies (8,9). In addition, a large benign thyroid
goitre can compress the trachea and induce airway obstruction
(8,9). The main treatment strategy for this
condition is the removal of this pressure immediately through
surgery, as is the case for large benign thyroid goitres (10). In the present report, a rare case
of TS accompanied by acute airway obstruction was documented. It is
hard to perform a thyroidectomy immediately as the thyroid surgery
may increase the severity of the TS. Therefore, in the present
study, TS was firstly controlled by medical treatment and then a
thyroidectomy was performed to solve the airway obstruction. The
patient recovered and was eventually discharged from the hospital
with prompt and effective treatment.
Case report
A 63-year-old female patient presented to the
Emergency Department of Weifang People's Hospital (Weifang, China)
with complaints of abdominal pain, dyspnoea and fever in April
2023. The patient had suffered from thyroid goitre, which has been
growing steadily but slowly for >30 years. Intermittent dyspnoea
episodes began 5 years prior, but they became more severe during
the 3 weeks prior to presentation. In addition, the patient had a
history of hyperthyroidism for 3 years, was irregularly receiving
methimazole for treatment and their biochemical tests yielded
relatively normal laboratory examination results. The liver
[glutamic-pyruvic transaminase, 23 U/l (normal range, 0-40 U/l);
glutamic oxalacetic transaminase, 331 U/l (normal range, 0-40 U/l)]
and kidney [creatinine, 44 µmol/l (normal range, 41-81 µmol/l)]
functions were normal. Vital signs on arrival were as follows:
Rectally measured temperature of 39.5˚C; heart rate of 125 beats
per min; respiratory rate of 30 breaths per min; and blood pressure
of 131/69 mmHg. Physical examination revealed a large mass on the
anterior neck without ulceration or discharge. The mass was not
tender but was warm to the touch, with a firm-to-hard consistency.
Laboratory tests (Table I) showed
TSH at <0.01 µIU/ml (normal range, 0.38-4.34 µIU/ml), free
triiodothyronine at 30.84 pmol/l (normal range, 2.77-6.31 pmol/l)
and free thyroxine at 106.72 pmol/l (normal range, 10.44-24.38
pmol/l). These laboratory test results showed that the patient had
hyperthyroidism.
 | Table ISummary of the laboratory test results
of the patient. |
Table I
Summary of the laboratory test results
of the patient.
| Parameter | Day 1 | Day 7 | Day 22 | Day 53 | Normal range |
|---|
| Free
triiodothyronine, pmol/l | 30.84 | 7.66 | 5.74 | 4.95 | 2.77-6.31 |
| Free thyroxine,
pmol/l | 106.72 | 29.04 | 18.63 | 14.32 | 10.44-24.38 |
| Thyroid-stimulating
hormone, µIU/ml | <0.01 | <0.01 | <0.01 | 2.68 | 0.38-4.34 |
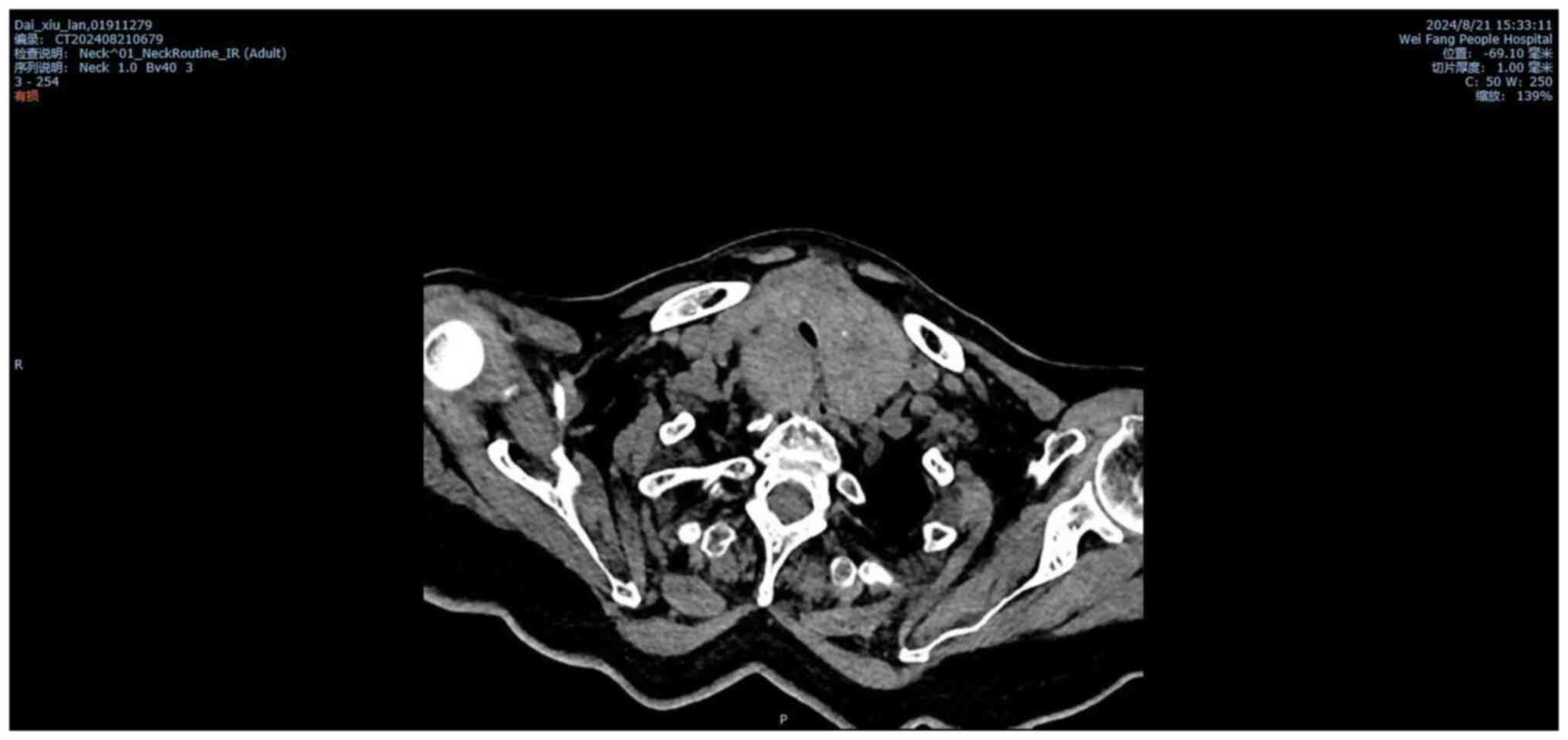
The electrocardiogram displayed marked sinus
tachycardia. Neck CT images revealed an enlarged bilateral thyroid
compressing most of the tracheal lumen, with the narrowest diameter
of the stenosis being 4.6 mm (Fig.
1). CT scan of the brain and abdomen yielded normal results
(data not shown).
Given the rapidly aggravating respiratory distress,
the patient immediately underwent an endotracheal intubation
without anaesthesia and was transferred to the intensive care
unit.
BWPS was calculated to be 70 points (with ≥45 points
indicating TS) (2,3) and the patient was diagnosed with TS
and acute airway obstruction. Treatment was promptly initiated with
nasogastric propylthiouracil (250 mg every 4 h), sodium iodide
(0.25 ml every 6 h), hydrocortisone (100 mg every 8 h) and esmolol
(10 mg every 4 h). Temperature was controlled with a cooling
blanket. In total, 7 days later, the vital signs were as follows:
Rectally measured temperature of 37.5˚C; heart rate of 92 beats per
min; and blood pressure of 125/90 mmHg. Thyroid function tests
showed TSH to be <0.01 µIU/ml, free triiodothyronine at 7.66
pmol/l and free thyroxine at 29.04 pmol/l. However, the intubation
could not be removed because of the stenosis of the trachea.
Therefore, the multidisciplinary team decided to perform a
thyroidectomy to reduce the bleeding and relapse immediately after
the TS had been controlled with medical treatment. Following
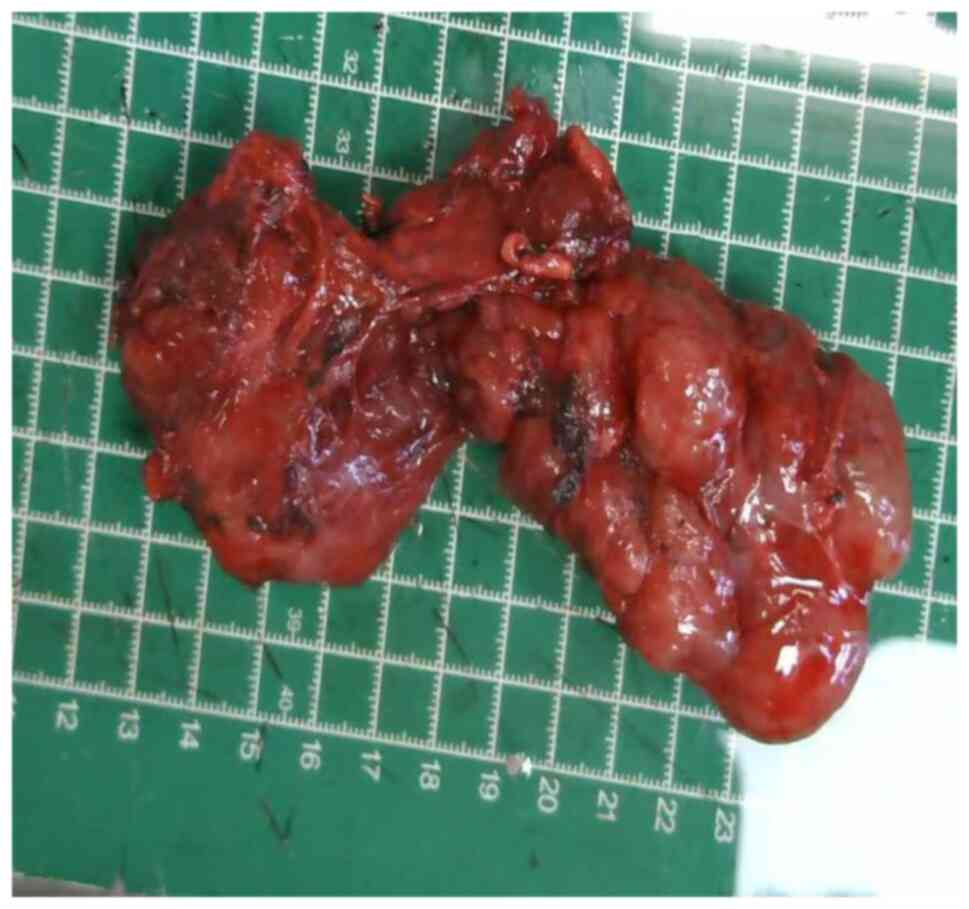
suggestions from the multidisciplinary team, a total thyroidectomy
was performed. During the gross examination, the thyroid was
composed of multiple nodules and the total volume of thyroid was
10x7x7 cm. (Fig. 2). Recurrent
laryngeal nerve and parathyroid glands were identified and
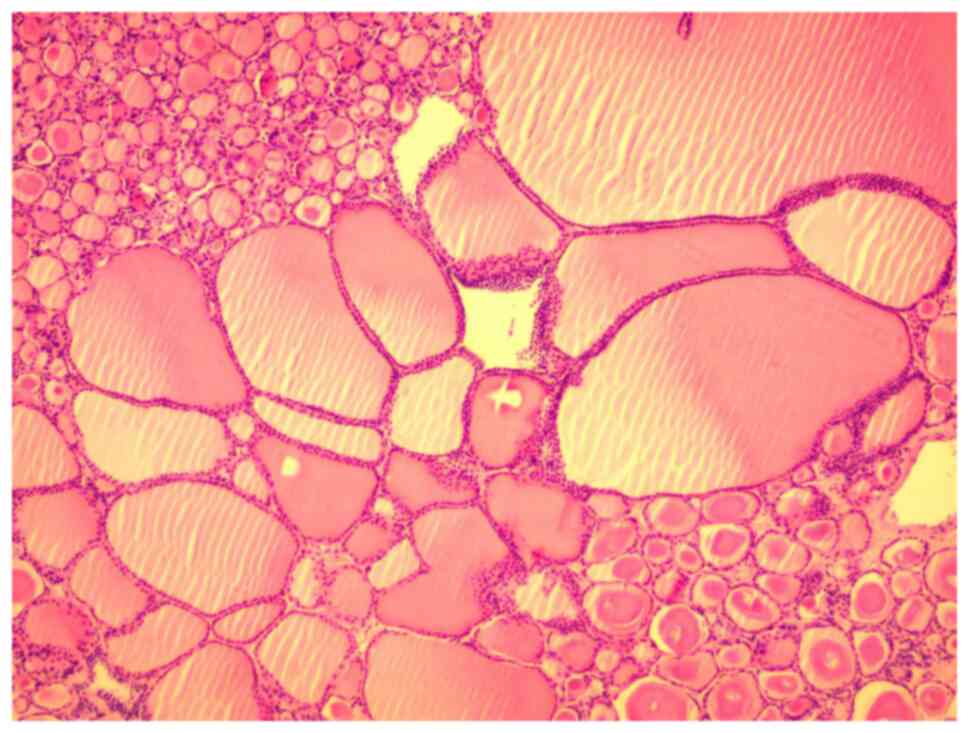
protected during the procedure. Specimens were fixed with 4%
formalin at room temperature for 12 h, embedded in paraffin, cut
into 4-µm sections, stained for 5 min at room temperature with
hematoxylin and eosin, and observed under a light microscope (x200
magnification). The thyroid demonstrated a benign multinodular
structure (Fig. 3). After surgery,
the patient was transferred to the thyroid surgery ward and their
vital signs were comparable to those at day 7. The intubation was
removed immediately after surgery. Sodium iodide (0.25 ml every 12
h) and hydrocortisone (100 mg every 12 h) were administered for 7
days after surgery. A total of 14 days after the surgery, thyroid
function tests revealed a TSH level at <0.01 µIU/ml, free
triiodothyronine at 5.74 pmol/l and free thyroxine at 18.63 pmol/l.
These results showed that the hyperthyroidism had been completely
controlled. Based on these laboratory findings and clinical
examinations, the patient's TS and trachea stenosis were deemed to
have been effectively resolved. The patient was subsequently
discharged from the hospital 15 days after the surgery.
Replacement therapy with L-thyroxine (75 µg/per day;
lifetime) began on the day that the patient was discharged from
hospital. Upon follow-up in the Thyroid Clinic of Weifang People's
Hospital, 1 month after discharge from the hospital, the patient
had normal thyroid function (TSH, 2.32 µIU/ml; free thyroxine,
14.32 pmol/l; and free triiodothyronine, 4.95 pmol/l) and did not
complain of dyspnoea. The patient has since been lost to
follow-up.
Discussion
TS is a life-threatening condition induced by
hyperthyroidism and causes multi-organ dysfunction (2,3). The
diagnosis of TS is based on laboratory tests and the presence of
severe signs and symptoms with evidence of thyrotoxicosis (2,3). TS
should be considered as one of the diagnostic possibilities in
patients with known hyperthyroidism (11,12).
Laboratory tests will typically show the TSH serum level to be low
to undetectable, whereas that of free thyroxine and free
triiodothyronine is typically elevated (11,12).
A number of precipitating factors can translate simple
thyrotoxicosis into the metabolic crisis of TS (2,3). For
example, patients with inadequately treated hyperthyroidism are at
a particularly increased risk of TS (2,3).
However, thyroid surgery without adequate drug control of
hyperthyroidism remains the most common cause of TS, although the
increased use of radioactive iodine has drastically reduced the
risk of TS due to this cause (11,12).
In addition, parturition, major trauma, non-thyroid surgery,
infection or iodine exposure from radiocontrast dyes may induce TS
in patients with thyrotoxicosis (2,3). In
the present case, the patient had a history of hyperthyroidism and
lacked a standardized treatment regimen. The compression of the
trachea induced by the goitre caused dyspnoea, which can induce a
stress response in the body. During the stress response, additional
thyroid hormones can be released into the bloodstream (11,12).
Therefore, the compression of trachea may have been one of the
causes of TS.
Hyperpyrexia (>39˚C) is universal in almost every
patient with TS (2,3). Overall, 84% of TS patients have
cardiovascular dysfunction, including tachycardia, systolic heart
failure with pulmonary and peripheral oedema, and high output heart
failure (2,3). In the present study, the patient had
tachycardia with a heart rate of 125 beats per min. A total of 51%
of patients with TS also suffer from gastrointestinal symptoms,
such as nausea, vomiting, diarrhoea, jaundice, hepatic injury and
abdominal pain (2,3). In addition, altered mental status,
including confusion, stupor and coma, are some of the other common
symptoms of hyperthyroidism (2,3). TS
remains a diagnostic challenge, because of non-specific and varied
characteristics on presentation. Various diagnostic systems, such
as the BWPS or Japan Thyroid Association criteria (2,3),
have been previously established to facilitate the diagnosis and
evaluation of the severity of TS (13,14).
In the present case, the patient had symptoms of thermoregulatory
dysfunction, tachycardia and abdominal pain, whereas the BWPS was
calculated to be 70 points (≥45 points indicating TS). Therefore,
the patient was diagnosed with TS.
The treatment of TS should be initiated once its
diagnosis is suspected due to the 10% mortality rate associated
with this condition (2,3). A multidisciplinary team should be
organized immediately to successfully offer the patient all
possible therapeutic options. Management aims should include
attaining a euthyroid state through medical management (antithyroid
drugs and iodine) and definitive treatment through surgery. In
general, the patients with TS should be admitted to the intensive
care unit for aggressive medical management and undergo definitive
treatment. The medical treatment should not only target the
synthesis and release of thyroid hormone but also attempt to
minimize the effects of circulating thyroid hormones and prevent
end-stage organ damage (2,3). The initial management for the present
case involved the use of antithyroid hormones synthesis drugs
(propylthiouracil), antithyroid hormones synthesis drug (sodium
iodide) and an antithyroid peripheral conversion drug
(hydrocortisone), which stabilized the hemodynamic status.
Acute airway obstruction was another issue that had
to be resolved for the patient in the present report. This is a
life-threatening condition that can be caused by upper respiratory
tract infections, resulting in oedema and retention of secretions,
sudden intrathyroidal haemorrhage and tracheal stenosis or collapse
(8,9). In the present case, the cause of
acute airway obstruction was compression by the enlarged thyroid.
In addition, airway compression may be an aetiological factor and
aggravated symptom of TS. The most effective treatment method for
this condition appears to be the physical removal of airway
obstruction induced by the enlarged goitre. However, the
cardiovascular dysfunction induced by TS impedes treatment
execution because of the high mortality rates of the former
(8,9). In addition, thyroid surgery may
increase the severity of TS (2,3).
These issues cause difficulty in the design of an optimal treatment
strategy. Ultimately, in the present case, the multidisciplinary
team decided to perform thyroidectomy to reduce the bleeding and
relapse immediately after TS was controlled with medical
treatment.
A previous case report showed a case of a
42-year-old male patient with acute airway obstruction induced by a
giant thyroid accompanied by TS (15). The patient had undergone emergency
total thyroidectomy due to the failure of tracheostomy. Although
the symptoms of TS had not worsened in the perioperative period,
the TS and airway obstruction was completely resolved similar to
the present case. However, surgery in cases of uncontrolled
hyperthyroidism may enhance the crisis of TS (2,3). In
the present case, a female patient with acute airway obstruction
and TS was presented. Specifically, the symptoms of TS were firstly
controlled, followed by thyroidectomy. Due to the difficulty of
tracheostomy, endotracheal intubation was performed to establish
the breathing passage, which provided vital additional time for
controlling the TS.
In conclusion, TS and acute airway obstruction are
both rare but potentially life-threatening disorders associated
with a high mortality rate. However, optimal medical treatment,
including antithyroid hormones synthesis drugs (propylthiouracil),
antithyroid hormones synthesis drug (sodium iodide) and an
antithyroid peripheral conversion drug (hydrocortisone), to control
the symptom of TS and then emergency thyroid surgery appear to be
safe options for patients with TS.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YW and JH conceived the case report. YW, LW and JH
performed the surgery. ZY, KM, LW and JH collected and analysed the
data. ZY and LW wrote and revised the manuscript. YW and JH
confirmed the authenticity of all the raw data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Weifang People's Hospital (Weifang, China; approval
no. WF202404001).
Patient consent for publication
Written informed consent was provided by the patient
for the case report to be published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lahey FH: Apathetic thyroidism. Ann Surg.
93:1026–1030. 1931.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tsakiridis I, Giouleka S, Kourtis A,
Mamopoulos A, Athanasiadis A and Dagklis T: Thyroid disease in
pregnancy: A descriptive review of guidelines. Obstet Gynecol Surv.
77:45–62. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wiersinga WM, Poppe KG and Effraimidis G:
Hyperthyroidism: Aetiology, pathogenesis, diagnosis, management,
complications, and prognosis. Lancet Diabetes Endocrinol.
11:282–298. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Galindo RJ, Hurtado CR, Pasquel FJ, García
Tome R, Peng L and Umpierrez GE: National trends in incidence,
mortality, and clinical outcomes of patients hospitalized for
thyrotoxicosis with and without thyroid storm in the United States,
2004-2013. Thyroid. 29:36–43. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Akamizu T, Satoh T, Isozaki O, Suzuki A,
Wakino S, Iburi T, Tsuboi K, Monden T, Kouki T, Otani H, et al:
Diagnostic criteria, clinical features, and incidence of thyroid
storm based on nationwide surveys. Thyroid. 22:661–679.
2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ono Y, Ono S, Yasunaga H, Matsui H,
Fushimi K and Tanaka Y: Factors associated with mortality of
thyroid storm: Analysis using a National inpatient database in
Japan. Medicine (Baltimore). 95(e2848)2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Farooqi S, Raj S, Koyfman A and Long B:
High risk and low prevalence diseases: Thyroid storm. Am J Emerg
Med. 69:127–135. 2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Eskander A, de Almeida JR and Irish JC:
Acute upper airway obstruction. N Engl J Med. 381:1940–1949.
2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yoyo M: Medicine and society in
martinique. Interaction between society and medical practice. Union
Med Can. 109 (Suppl):S23–S27. 1980.PubMed/NCBI(In French).
|
|
10
|
Yildirim E: Principles of urgent
management of acute airway obstruction. Thorac Surg Clin.
28:415–428. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chiha M, Samarasinghe S and Kabaker AS:
Thyroid storm: An updated review. J Intensive Care Med. 30:131–140.
2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
De Almeida R, McCalmon S and Cabandugama
PK: Clinical review and update on the management of thyroid storm.
Mo Med. 119:366–371. 2022.PubMed/NCBI
|
|
13
|
Burch HB and Wartofsky L: Life-threatening
thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am.
22:263–277. 1993.PubMed/NCBI
|
|
14
|
Satoh T, Isozaki O, Suzuki A, Wakino S,
Iburi T, Tsuboi K, Kanamoto N, Otani H, Furukawa Y, Teramukai S and
Akamizu T: 2016 Guidelines for the management of thyroid storm from
The Japan Thyroid Association and Japan Endocrine Society (First
edition). Endocr J. 63:1025–1064. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Matsushita A, Hosokawa S, Mochizuki D,
Okamura J, Funai K and Mineta H: Emergent thyroidectomy with
sternotomy due to acute respiratory failure with severe thyroid
storm. Ann R Coll Surg Engl. 100:e1–e3. 2018.PubMed/NCBI View Article : Google Scholar
|