Introduction
Chemotherapy for metastatic malignant melanoma (MM)
is challenging. In Japan, DAV-Feron therapy, which includes
systemic dacarbazine, nimustine, vincristine administration and
local intracutaneous interferon β injection, is the standard
chemotherapy for metastatic MM. For MM with resistance to DAV-Feron
therapy, DAC-Tam therapy (systemic cisplatin, nimustine,
dacarbazine and oral tamoxifen) is one of the standard choices.
However, it is very difficult for an effective anti-cancer drug to
be selected for MM patients since each drug has a low response rate
of 10 to 20% (1,2). Therefore, establishment of a useful
and tailor-made chemosensitivity test is crucial. In addition, it
is important that a test satisfies the following criteria: i) a
high rate of evaluation of the primary culture; ii) can be applied
to an early MM lesion with a small amount of tumor; iii) the
applied drug concentrations can mimic physiological levels; iv)
able to evaluate an anti-cancer effect without contaminating
fibroblasts. Collagen gel droplet-embedded culture drug sensitivity
test (CD-DST) satisfies the above-mentioned characteristics. In
this report, we tried to adapt the CD-DST for Japanese patients
with MM.
Materials and methods
Patient background
Nineteen samples from 15 MM patients were examined
after obtaining written informed consent (Table I). The patients were managed as
anonymous samples, and personal information, except for clinical
manifestations, were regarded as confidential. The Medical Ethics
Committee of Kyoto University approved this study, which was
conducted in accordance with the principles of the Declaration of
Helsinki. Pathological types included five cases of superficial
spreading melanoma, seven cases of acral lentigenous melanoma, one
case of lentigo maligna melanoma and two cases of nodular melanoma
(Table I).
 | Table I.Summary of the clinical
characteristics and the results of the CD-DST. |
Table I.
Summary of the clinical
characteristics and the results of the CD-DST.
| | | | | DAV-Feron therapy
|
|---|
| Case no. | Tested lesion | Type | Cisplatin | Adriamycin | Dacarbazine | Nimustine | Vincristine |
|---|
| 1-1 | Primary | SSM | 54.9a | 21.8 | 86.9 | 84.7 | 14.9 |
| 1-2 | Skin metastasis | SSM | 96.3 | 53.9 | 100.0 | 100.0 | 60.7 |
| 2-1 | Primary | SSM | UPC | UPC | UPC | UPC | UPC |
| 2-2 | Skin metastasis | SSM | 95.2 | 100.0 | 95.7 | 95.9 | 95.1 |
| 3 | Primary | SSM | UPC | UPC | UPC | UPC | UPC |
| 4-1 | Primary | SSM | 83.1 | 49.3 | 100.0 | 100.0 | 35.0 |
| 4-2 | Skin metastasis | SSM | 70.2 | 39.2 | ND | ND | 29.5 |
| 4-3 | Skin metastasis | SSM | 100.0 | 96.9 | 99.1 | 96.5 | 88.1 |
| 5 | Primary | SSM | 77.4 | 42.7 | 88.7 | 84.2 | 88.7 |
| 6 | Primary | ALM | 62.8 | ND | 96.6 | 100.0 | 46.2 |
| 7 | Primary | ALM | ND | ND | 97.9 | ND | ND |
| 8 | Primary | ALM | UPC | UPC | UPC | UPC | UPC |
| 9 | Primary | ALM | 92.2 | 79.4 | 93.9 | 70.7 | 97.9 |
| 10 | Primary | ALM | 74.5 | 29.7 | 100.0 | 100.0 | 29.7 |
| 11 | Primary | ALM | ND | 53.4 | 96.4 | ND | 55.6 |
| 12 | Skin metastasis | ALM | 84.9 | 62.0 | ND | ND | ND |
| 13 | Primary | LMM | 93.8 | 75.9 | 90.8 | 100.0 | 36.8 |
| 14 | Primary | NM | UPC | UPC | UPC | UPC | UPC |
| 15 | Primary | NM | 87.2 | 98.8 | 100.0 | 82.3 | 73.5 |
Preparation of primary melanoma cells for
testing of the in vitro tumor response
Fresh surgical specimens (∼64 mm3) were
minced into a paste, suspended in Hank’s balanced saline solution
and treated with Dispersion Enzyme Cocktail EZ (Nitta Gelatin Inc.,
Japan) at 37°C for 2 h. After digestion, each sample was
centrifuged at 900 × g for 3 min, the supernatant was removed, and
the dispersed tumor cells were collected through an 80-μm nylon
mesh. The recovered cells were cultured for 12–48 h in a collagen
gel-coated flask (CG-flask; Nitta Gelatin Inc.). The collagen gel
in the CG-flask was dissolved in the cell dispersion in the Enzyme
Cocktail EZ, and only viable cells that adhered to the collagen gel
were collected and used for the CD-DST.
Collagen gel droplet-embedded culture
drug sensitivity test (CD-DST)
CD-DST was performed according to the methods
described previously (3). Briefly,
the prepared tumor cell suspension was added to a neutralized
collagen solution at a final concentration of 1×105
cells/ml. Three drops of the collagen-cell mixture (30 μl/drop)
were placed in each well of a 6-well plate on ice and allowed to
gel at 37°C in a CO2 incubator. The final density was
∼3×103 cells/collagen gel droplet. One hour later, each
well was overlaid with 4 ml PCM-2 medium (Serum-free Medium; Nitta
Gelatin Inc.), each anti-cancer drug was added and incubation was
carried out for the following 7 days. At the end of the incubation,
the cancer cell colonies in the collagen gel droplets were stained
by Neutral red solution for 2 h. Each collagen droplet was fixed
with 10% neutral formalin buffer, washed in water, air dried and
quantified by image analysis. The growth rates in the control
incubations were calculated as the total cell number on day 7/total
cell number on day 0. The in vitro sensitivity was expressed
as the percentage of the T/C ratio, where T is the total cell
number in the treated group and C is the total cell number of the
control group. When the T/C ratio was <50%, the drug sensitivity
was regarded as ‘high sensitive’, while >50% and <65% was
considered as ‘borderline’, and >65% as ‘low sensitive’.
Determination of concentrations of
anti-cancer drugs
A concentration of an anti-cancer drug was
determined by the 24-h area under the concentration-time curve,
when it is administered at an ordinary dose for Japanese patients
with MM (4–6). The concentrations of cisplatin,
adriamycin, dacrbazine, nimustine and vincristine were calculated
as 0.2, 0.02, 0.5, 0.025 and 0.01 μg/ml, respectively.
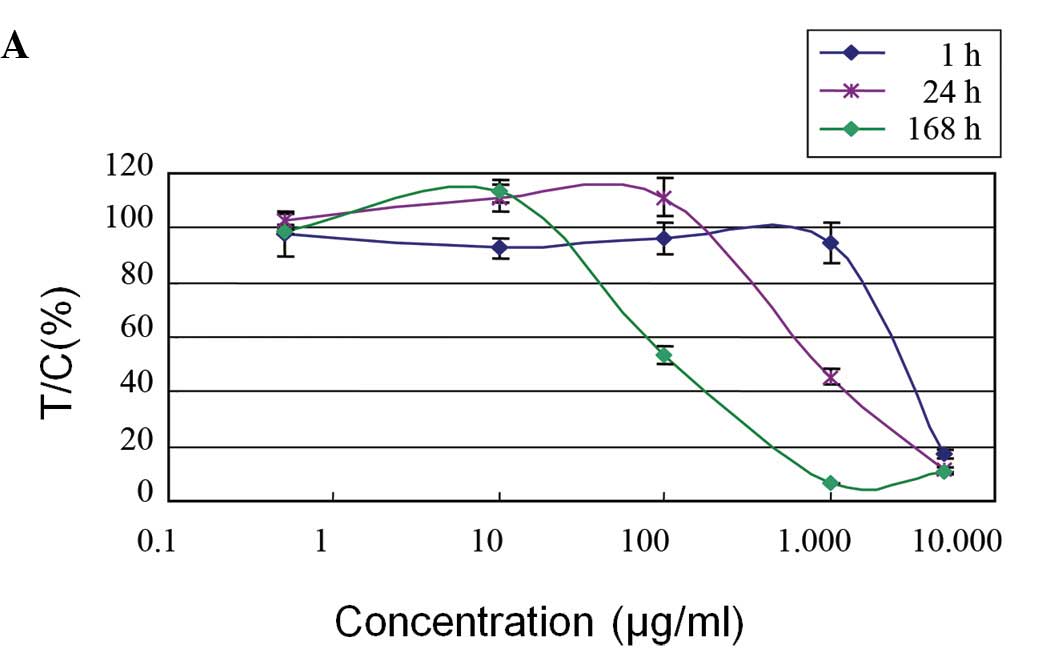
Sensitivities of dacarbazine and
nimustine against the B16 cell line in vitro
B16 cells, a mouse melanoma cell line, were cultured
in DMEM containing 10% fetal bovine serum. B16 cells were collected
by a standard trypsin/EDTA method and cultured in a collagen gel
droplet and exposed to various concentrations of dacarbazine and
nimustine.
Chemotherapy and response assessment
Four patients who completed at least one cycle of
sensitivity-directed chemotherapy were considered evaluable for
response. Tumor response was assessed by computed tomography and/or
magnetic resonance imaging in 12-week intervals and evaluated
according to response evaluation criteria in solid tumors (7).
Results
Evaluation rate of human primary melanoma
cells
The overall evaluation rate in 19 tests was 78.9%
(15/19 tests). The reasons for the unsuccessful four tests included
one bacterial contamination, two cases having overly small
specimens (∼8 mm3), and one case of non-viable cells due
to resecting a sample after an effective chemotherapy (case no. 3).
Multiple lung metastases of case no. 3 showed a complete response
after administration of three courses of DAV-Feron therapy.
Chemosensitivities of human primary
melanoma cells
When the ‘high sensitive’ and ‘borderline’ were
regarded as ‘effective’, the in vitro chemosensitivity rate
of cisplatin, adriamycin and vincristine were 15 (2/13), 62 (8/13)
and 62% (8/13), respectively. No cases showed sensitivity to
dacarbazine and nimustine, which are standard drugs for treatment
to malignant melanoma. Therefore, the chemosensitivity of B16 cells
against nimustine and dacarbazine were evaluated using the CD-DST
(Fig. 1A and B).
For nimustine, the B16 cells showed the same
response curve at various incubation times. A 3-h incubation had
the same anti-proliferation effect compared with a 24-h incubation.
On the other hand, these cells showed no response to dacarbazine at
physiological concentrations (0.1–100 μg/ml) in the CD-DST.
Correlation between the results of the
CD-DST and clinical responses against anti-cancer drugs
We were able to evaluate the association of
chemosensitivity with the clinical response in three cases. In case
no. 1, the patient received chemotherapy of cisplatin and
adriamycin for multiple lung metastases, according to the results
of the CD-DST which showed high sensitivity to these agents
(Table I, case no. 1-1). The lung
metastatic tumors showed partial response; however, skin metastases
appeared as recurrences, showing high resistance to cisplatin and
adriamycin in the CD-DST (Table I,
case no. 1-2). In case no. 2, the CD-DST for the primary lesion was
unsuccessful due to bacterial contamination. The patient was
administered six courses of DAV-Feron therapy; however, skin
metastases occurred, which showed high resistance to vincristine.
In case no. 4, the patient showed high sensitivity to adriamycin
and vincristine in the CD-DST (Table
I, case no. 4-1). After six courses of DAV-Feron therapy as
adjuvant chemotherapy, skin and lung metastases appeared. The
patient underwent chemotherapy with adriamycin and vincristine (AV
therapy) according to the results of the CD-DST, and this treatment
showed ‘partial response’ to the metastatic lung lesions and skin
tumors. A chemosensitivity test of the recurred skin metastases
after AV therapy showed high resistance to adriamycin and
vincristine (Table I, case no.
4-3).
Discussion
The CD-DST method of treating MM cells in a
three-dimensional culture system in a collagen gel drop mimics
tumors in the human body and enables MM cells to grow in
vitro, resulting in a high success rate of primary culture of
MM cells. In addition, serum-free culture for 7 days after drug
exposure prevents the growth of fibroblasts. Moreover,
contamination of fibroblasts is excluded by an image analysis,
which detects the difference in cell shape and Neutral red staining
between fibroblasts and MM cells. In many types of cancers
including lung, breast, colon and gastric, the results of the
CD-DST demonstrated good correlation with their clinical responses
to anti-cancer drugs (8).
In this research, CD-DST exhibited a high success
rate of primary culture of MM cells, which were obtained from small
specimens of primary tumors. This suggests that the CD-DST method
can evaluate the chemosensitivity of MM cells in a primary lesion
and can also predict the effective anti-cancer drugs for future
metastatic lesions in an internal organ when it is difficult to
obtain a biopsy specimen.
The previously reported clinical response rate of MM
cells against standard anti-cancer drugs is 10–20%. Of these,
dacarbazine is one of the most effective anti-cancer drugs for MM.
In this study, dacarbazine showed no sensitivity in the CD-DST
method. Thus, we speculate that dacarbazine is not suitable for
CD-DST, since dacarbazine needs to be activated by the body’s
metabolism in order to produce diazomethane, a strong alkylating
agent which imparts the major anti-cancer effect (9). Diazomethane is not suitable for in
vitro evaluation of the efficacy of dacarbazine due to its
explosive nature. Chemosensitivity data of B16 cells against
dacarbazine also support its prodrug character. Nimstine is a
typical drug, whose anti-tumor effect is dependent on the exposure
concentration. Notably, the exposure time of 3 h may be necessary
to obtain a sufficient anti-tumor effect according to our
experimental data using B16 cell in vitro (Fig. 1B). This evidence allowed us to
apply a higher concentration of nimustine on the MM cells when the
time period was only 3 h. Therefore, we plan to test a higher
concentration of nimustine in our future CD-DST study.
In regards to the drug concentrations, the CD-DST
can evaluate the chemosensitivity of tumor cells at a physiological
concentration mimicking a normal blood concentration. In a large
study of drug sensitivity-directed chemotherapy in metastatic
melanoma using ATP-TCA assay, the concentration of cisplatin was
3.8 μg/ml, compared with 0.2 μg/ml in the present study (10). We suggest that the collagen gel
droplet reconstructs the minimum environment of the human body and
realizes the genuine interaction between MM cells and drugs.
As for the correlation between clinical response and
the results of the in vitro chemosensitivity tests, we
evaluated only a small number of patients. However, a previous
study reported that results of an in vitro chemosensitivity
test predicted the clinical response and prolonged survival in
patients with highly sensitive metastatic MM cells (10). To improve treatment outcome against
MM, we believe that CD-DST might also be useful for predicting its
clinical response. Further study of MM patients tested using CD-DST
before and after chemotherapy is required to establish the clinical
importance of CD-DST as well as a study of its value in other types
of solid tumors (11).
In the future, we believe that the CD-DST method can
be applied to evaluate new anti-cancer drugs against MM, since the
concentration of anti-cancer drugs using the CD-DST method mimics
physiological levels. In addition, a collagen drop reproduces the
conditions in the human body. We are currently planning to assess
new molecular target-based drugs against MM using the CD-DST.
References
|
1.
|
Buzaid AC, Bedikian A and Houghton AN:
Cutaneous Melanoma. 3rd edition. Quality Medical Publishing; St.
Louis: pp. 405–418. 1998
|
|
2.
|
Balch CM, Reintgen DS, Kirkwood JN, et al:
Cancer: Principles and Practice of Oncology (5th edition).
Lippincot-Raven Publishers. Philadelphia: 1947–1994. 1997.
|
|
3.
|
Kobayashi H, Tanisaka K, Doi O, et al: An
in vitro chemosensitivity test for solid human tumors using
collagen gel droplet embedded cultures. Int J Oncol. 11:449–455.
1997.
|
|
4.
|
Mitsuhashi Y, Sugiyama Y, Ozawa S, et al:
Prediction of ANCU plasma concentration-time profiles in humans by
animal scale up. Cancer Chemother Pharmacol. 27:20–26. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Breithaupt H, Dammann A and Aigner K:
Pharmacokinetics of dacarbazine (DITC) and its metabolite
5-aminoimidazole-4-carboxamide (AIC) following different dose
schedules. Cancer Chemother Pharmacol. 9:103–109. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Van den Berg HW, Desai ZR, Wilson R, et
al: The pharmacokinetics of vincristine in man. Cancer Chemother
Pharmacol. 8:215–219. 1982.PubMed/NCBI
|
|
7.
|
Therasse P, Arbuck SG, Eisenhauer EA, et
al: New guidelines to evaluate the response to treatment in solid
tumors. European Organization for Research and Treatment of Cancer,
National Cancer Institute of the United States, National Cancer
Institute of Canada. J Natl Cancer Inst. 92:205–216. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Tanigawa N, Kitaoka A, Yamakawa M, et al:
In vitro chemosensitivity testing of human tumours by collagen gel
droplet culture and image analysis. Anticancer Res. 16:1925–1930.
1996.PubMed/NCBI
|
|
9.
|
Bono VH: Studies on the mechanism of
action of DTIC (NSC-45388). Cancer Treat Rep. 60:141–148.
1976.PubMed/NCBI
|
|
10.
|
Ugurel S, Schadendorf D, Pfohler C, et al:
In vitro drug sensitivity predicts response and survival after
individualized sensitivity-directed chemotherapy in metastatic
melanoma: a multicenter phase II trial of the Dermatologic
Cooperative Oncology Group. Clin Cancer Res. 12:5454–5463. 2006.
View Article : Google Scholar
|
|
11.
|
Kobayashi H: Development of a new in vitro
chemosensitivity test using collagen gel droplet-embedded culture
and image analysis for clinical usefulness. Recent Results Cancer
Res. 161:48–61. 2003. View Article : Google Scholar : PubMed/NCBI
|