Introduction
Oral squamous cell carcinoma (OSCC) is the most
common epithelial oral cancer and is characterized by a high
infiltrative potential, which can result in early regional lymph
node involvement and subsequent metastatic spread. Despite advances
in multidisciplinary treatment modalities, including chemotherapy
and/or radiotherapy, no improvement in the 5-year survival rate has
been achieved over the past 20 years (1). In addition, the clinical behavior of
OSCC is difficult to predict, considering classical
histopathological parameters only.
Thus, understanding the molecular mechanisms of
local invasion has become an important goal in the field of head
and neck surgery. Several reports have indicated that local
interactions between cancer cells and stromal cells are important
for the process of invasion and metastasis, including cellular
detachment, proteolytic degradation of the basal lamina, migration
through the extracellular matrix and resistance of apoptosis
(2).
A proto-oncogene which has been suggested to be
associated with OSCC progression is c-Met (3). c-Met encodes the receptor for
hepatocyte growth factor (HGF). This receptor is a 190-kDa
receptor-like tyrosine kinase, comprised of disulfide-linked
subunits 50 (α) and 145 kDa (β) (4). In the fully processed c-Met product,
the α-subunit is completely extracellular and the β-subunit has an
extracellular ligand-binding domain, a single transmembrane domain
and a cytoplasmic tyrosine kinase domain (4). c-Met is found in hepatocytes,
fibrocytes, keratinocytes and melanocytes and also in the kidney,
lung, spleen, hematopoietic cells and ovaries (4). c-Met is activated by HGF, a 100-kDa
heparin-binding polypeptide, which is predominantly expressed by
mesenchymal cells (5). HGF is
structurally related to the family of serine proteases including
plasminogen, prothrombin, urokinase and tissue plasminogen
activator (6).
The HGF/c-Met interaction can promote cell
proliferation, motility, invasiveness, morphogenesis and
angiogenesis in various cell types, including different tumor cells
(6,7). In several clinical studies, high
expression of HGF and c-Met has been shown in various types of
human carcinomas including thyroid, pancreas, prostate and head and
neck cancers (8), and its
expression has been associated with poor prognosis in
nasopharyngeal, esophageal, cervical and breast carcinoma (9). Furthermore, the expression of c-Met
in head and neck squamous cell carcinoma (HNSCC), the
clinicopathological parameters and the survival of HNSCC patients
have been analyzed in various studies (3,10,11),
showing inconsistent results in terms of the prognostic value of
c-Met expression in HNSCC. Therefore, the aim of the present study
was to investigate the expression of c-Met in 211 patients with
OSCC using immunohistochemistry and to analyze its expression in
relation to clinicopathological parameters, in order to verify its
role in the prognostic evaluation of these tumors.
Materials and methods
Specimens for immunohistochemistry
For immunohistochemical evaluation, the routinely
processed paraffin blocks of formalin-fixed OSCC specimens were
obtained from 53 female and 158 male patients who underwent surgery
at the Department of Oral and Maxillofacial Surgery of the
University Hospital Tuebingen, Germany, between 1988 and 1997. The
specimens were retrieved retrospectively from the pathology
archives. The criteria for inclusion in this study included a
histopathological diagnosis of OSCC, no preoperative therapy,
potentially curative radical resection, follow-up data available
and satisfactory tissue preservation.
The mean age of included patients was 58±SD years
(range, 34–93 years). The follow-up period for surviving patients
ranged from 1 to 172 months, with a median of 42 months. Primary
tumor sites were as follows: maxilla, including soft and hard
palate, 13 tumors; floor of the mouth, 79 tumors; tongue, 36
tumors; gingival of the mandible, 22 tumors; retromolar region, 8
tumors; lip, 15 tumors; planum buccale, 17 tumors; all other
locations, 21 tumors. The TNM staging categories were determined
according to the criteria established by the American Joint
Committee on Cancer and the International Union Against Cancer
(UICC) (12). Stage grouping of
the patients was as follows: stage I, 47 patients; stage II, 30
patients; stage III, 27 patients; stage IV, 107 patients. On
histopathologic evaluation of lymph node involvement, 146 tumors
were classified as N0 and 65 tumors were classified as
N1 or N2. One hundred and thirty-five tumors
were ≤4 cm in diameter (T1 and T2) and 76
tumors were >4 cm in diameter (T3 and T4).
Two tumors showed distant metastasis, while 209 tumors did not show
distant metastasis.
Immunohistochemical staining
procedure
Sections (4-μm thick) of paraffin and
formaldehyde-fixed tissue of the resection specimens were cut. For
immunohistochemical staining, sections were deparaffinized and
rehydrated via serial passage through xylene and a graded series of
ethanol. To block endogenous peroxidase activity slices were
treated with 0.3% H2O2 for 10 min. All
specimens were subjected to heat-induced antigen retrieval in
Target Retrieval Solution (Dako Diagnostics, Hamburg, Germany) for
30 min at 95–99°C and then incubated with 10% normal goat serum to
block nonspecific binding. Sections were incubated with the primary
c-Met antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) at a
final dilution of 1:50 at 4°C overnight. After several washing
steps, sections were incubated with biotinylated secondary antibody
and streptavidin peroxidase (HRP) (both from Dako Diagnostics).
Diaminobenzidine chromogen (Dako Diagnostics) was used for
visualization. Nuclei were counterstained with hematoxylin.
Quantitation of immunostaining
results
All sections were immunostained under the same
conditions in order to reduce the variability. Immunostaining was
visualized using a Leica CTR MIC microscope and recorded with a
high-resolution DC300 Leica digital camera (Leica Microsystems,
Wetzlar, Germany). Five fields (under a ×40 objective) from each
OSCC section were randomly selected for assessment. After
conversion to grayscale images (gray values from 0–255), the
c-Met-positive cells were quantified as the percentage of the total
cells in five representative view areas using the Leica QWin image
analysis and image processing software (Leica Microsystems).
Statistical analysis
Statistical analysis was performed using the
Fisher's exact test. A p-value <0.05 was indicative of a
significant difference. Survival analysis was performed using the
the Kaplan-Meier method, and statistical significance was
calculated using the log-rank test.
Results
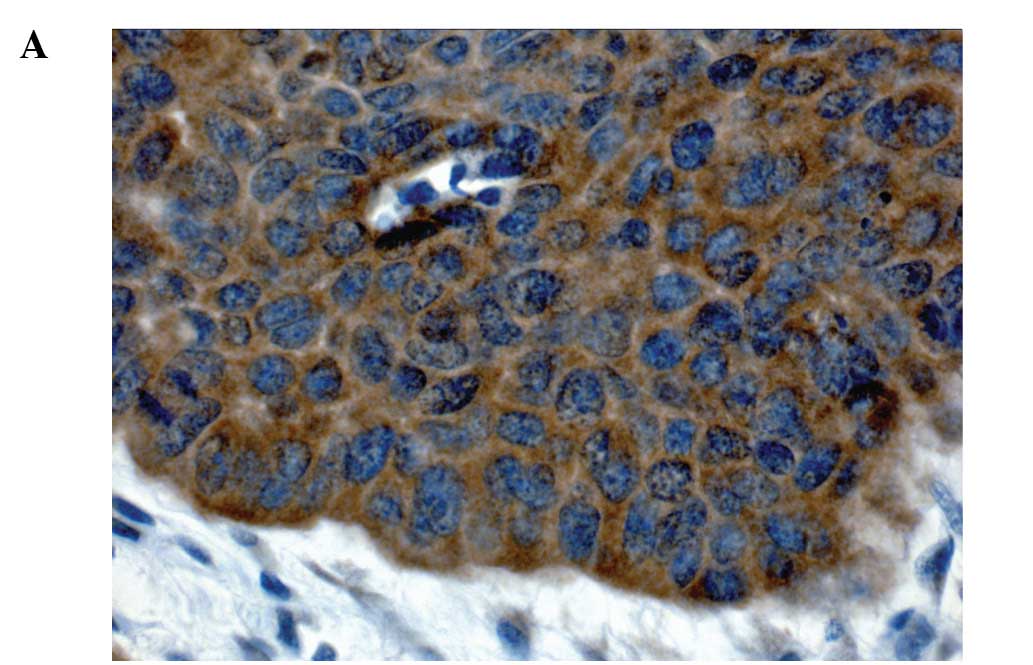
Immunohistochemical staining was performed against
c-Met, and the tumor was defined as negative when antigen
expression was demonstrated in <50% of the carcinoma cells and
as positive when demonstrated in ≥50%, as suggested elsewhere
(13). Of the 211 samples, a
positive result of immunohistochemical staining against c-Met was
observed in 175 (82.9%), while 36 (17.1%) showed no positive
result. c-Met expression was not observed in stromal cells, being
mainly observed in carcinoma cells. In most of the specimens, c-Met
was expressed strongly and diffusely in the cytoplasm of carcinoma
cells (Fig. 1). The relation
between c-Met expression and clinical and histopathological
parameters is summarized in Table
I. The rate of positive c-Met expression was 83.7% in patients
with tumors ≤4 cm in diameter (stages T1 and
T2) and 81.6% in tumors >4 cm in diameter (stages
T3 and T4), with no statistically significant
difference (p=0.706). Positive c-Met expression seemed to be
increased in cases of lymph node metastasis (87.7%); however, there
was no significant difference compared to those without lymph node
metastasis (80.8%) (p=0.242). Where there was no distant
metastasis, positive c-Met expression was observed in 82.8% of the
cases, while c-Met expression was positive in 50% of the cases with
distant metastasis, without any statistical significance (p=0.321).
Positive c-Met expression decreased in stage III and IV carcinomas
(78.4%) compared to stage I and II carcinomas (90.9%) in a
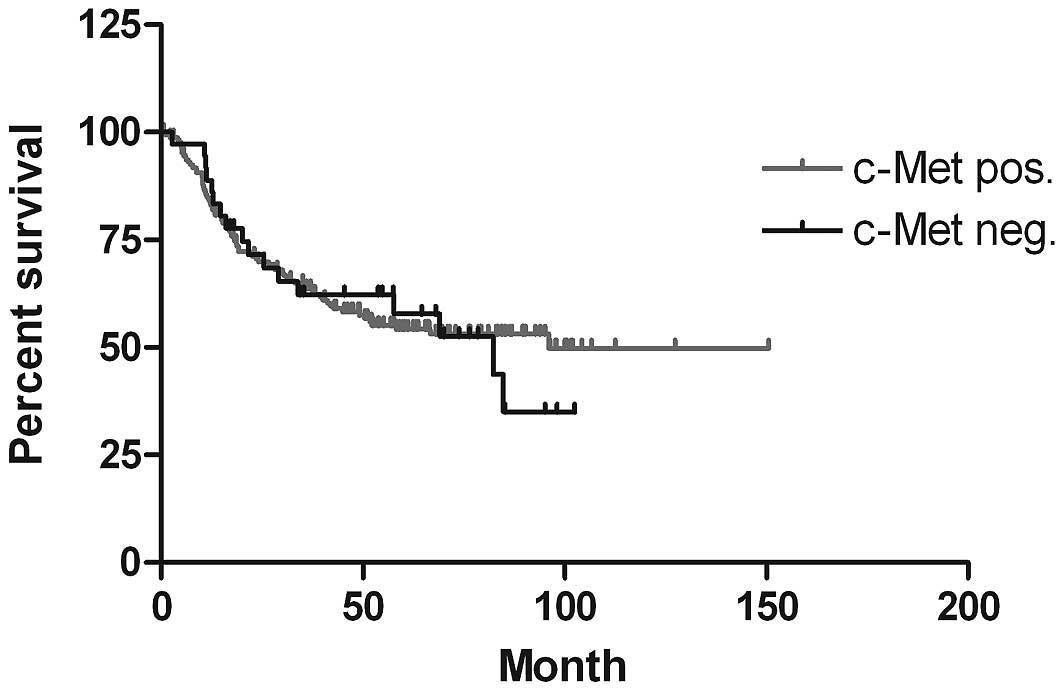
statistically significant manner (p=0.022). Survival analysis was
performed using the Kaplan-Meier method, and statistical
significance was calculated using the log-rank test (Fig. 2). There was no significant
correlation between the groups with negative and positive c-Met
expression (p=0.8244).
 | Table I.Statistical analysis of c-Met
expression and associated clinicopathologic parameters in OSCC. |
Table I.
Statistical analysis of c-Met
expression and associated clinicopathologic parameters in OSCC.
| Expression of c-Met;
n (%)
| |
|---|
| Variable | Negative | Positive | p-valuea |
|---|
| T | | | |
| T1,
T2 (n=135) | 22 (16.3) | 113 (83.7) | 0.706 |
| T3,
T4 (n=76) | 14 (18.4) | 62 (81.6) | |
| N | | | |
| N0
(n=146) | 28 (19.2) | 118 (80.8) | 0.242 |
| N1,
N2 (n=65) | 8 (12.3) | 57 (87.7) | |
| M | | | |
| − (n=209) | 36 (17.2) | 173 (82.8) | 0.321 |
| + (n=2) | 1 (50.0) | 1 (50.0) | |
| Stage | | | |
| I, II (n=77) | 7 (9.1) | 70 (90.9) | 0.022 |
| III, IV
(n=134) | 29 (21.6) | 105 (78.4) | |
Discussion
In several studies, high expression of HGF and c-Met
has been demonstrated in various types of human carcinomas
including thyroid, pancreas, prostate and head and neck cancer
(8). In particular, studies
analyzing c-Met expression in relation to clinical and
histopathological parameters in OSCC patients have arrived at
controversial results. Thus, to date, a definitive conclusion
regarding the prognostic value of c-Met expression in OSCC has not
been made. Therefore, we investigated c-Met expression in a large
number, 211 cases, of OSCC to verify its possible role as a
prognostic marker. A positive c-Met expression, or more than 50% of
the tumor cells showing c-Met staining, was noted in 175 specimens
(82.9%). This result suggests that in most cases of OSCC, c-Met
protein is produced. In addition, Kim et al (14), also using immunohistochemical
staining, showed that 28 of 40 cases (70%) of hypopharyngeal cancer
expressed c-Met, and Sawatsubashi et al (15) demonstrated that 45 of 82 cases
(54.9%) of glottic cancer expressed c-Met. Furthermore, c-Met
expression was detected in corresponding affected lymph nodes
(15–17). In 40 cases of hypopharyngeal
squamous cell carcinoma no significant correlation between c-Met
expression and tumor size, rate of distant metastasis or survival
rate was apparent (14). However,
there was a significant increase in c-Met expression in tumors with
lymph node metastasis. Sawatsubashi et al (15) reported no significant correlation
between c-Met expression and age, gender, histological type, tumor
size or distant metastasis in 82 cases of primary laryngeal
carcinoma, but 10 of 12 cases (83.3%) with lymph node metastasis
showed a significant increase in c-Met expression. Lo Muzio et
al (3) investigated c-Met
expression in 84 patients with OSCC, but no statistical association
between c-Met expression and histological grading, lymph node
status and staging was found, except there was a significant better
survival rate in the group with low c-Met expression than in the
group with high c-Met expression. In the present study, using a
large sample size of 211 specimens, no significant difference in
c-Met expression in stage T1 and T2 tumors in
comparison to stage T3 and T4 was found. In
addition, no significant difference in c-Met expression in cases of
lymph node metastasis compared to those without lymph node
metastasis could be shown. Furthermore, no statistically
significant correlation between the expression of c-Met and
survival rate was apparent. Notably, there was a negative
significant correlation between clinical tumor stage and c-Met
expression.
There are different possible explanations for these
inconsistent results. First of all, in most studies, only small
numbers of specimens were used to investigate c-Met expression in
HNSCC. Kim et al used 40 specimens of hypopharyngeal
squamous cell carcinoma (14), Lo
Muzio et al used 84 specimens of OSCC (3), Sawatsubashi et al investigated
82 patients with laryngeal carcinomas (15) and Marshall and Kornberg used only
27 samples of OSCC (18). On the
other hand, in studies where immunohistochemical staining was used,
various standards were used to determine a ‘positive’ result. In
one study, expression in >10% of cancer cells was considered
positive (19), where in other
studies c-Met expression in >30% of cancer cells was deemed a
positive result (3,14). Consequently, we defined a positive
result only when expression of c-Met was detected in ≥50% of the
cancer cells. Otherwise, human visual assessment of
immunohistochemical staining results is difficult and subjective,
as the counting results may be varied for each observer and between
different observers. The results of quantitative counting and
semi-quantitative counting may also be affected by the experience
and other psychological factors of the pathologists. To exclude
these factors, we objectively quantified the staining result using
the Leica QWin image analysis and image processing software.
However, the important role of the HGF/c-Met
receptor tyrosine kinase system in the invasive behavior of HNSCC
is undisputable, as shown by means of invasion assays in
vitro (20,21). Furthermore, a relationship between
the concentration of HGF in serum or in cancer tissue and the
progression of disease has been noted in patients with gastric,
breast and lung cancer (22).
Uchida et al (10) reported
that fibroblasts of the oral cavity secrete various growth factors,
including HGF, which promote the invasion and metastasis of oral
cancer cells. In addition, significantly higher HGF serum levels
were detected in patients with OSCC when compared with those in
healthy volunteers. Furthermore, after initial treatment, all of
the tumor-free survivors exhibited a decrease in the serum HGF
levels. The exact mechanism of the interaction between HGF and
c-Met has not been fully understood. Various cytokines including
interleukin-1 and -6, tumor necrosis factor-α, which are produced
in the microenvironment of the tumor as a result of the nonspecific
inflammatory response, appear to increase c-Met expression
(23). Furthermore, c-Met
expression was shown to be upregulated by HGF itself, as
demonstrated in vitro by Boccaccio et al (24).
In summary, the immunohistochemical staining of oral
squamous cell cancer tissue of 211 patients revealed high
expression of c-Met. However, the level of c-Met expression showed
no significant correlation in relation to tumor size, lymph node
status, rate of distant metastasis or survival rate. Moreover,
c-Met showed a significant negative correlation to the clinical
stage of the tumor. Even though the HGF/c-Met system appears to
play an important role in the invasive behavior of OSCC, this study
did not verify the role of c-Met as a prognostic marker in patients
with OSCC.
References
|
1.
|
Lothaire P, De Azambuja E, Dequanter D, et
al: Molecular markers of head and neck squamous cell carcinoma:
promising signs in need of prospective evaluation. Head Neck.
28:256–269. 2006.
|
|
2.
|
De Herdt MJ and Baatenburg De Jong RJ: HGF
and c-MET as potential orchestrators of invasive growth in head and
neck squamous cell carcinoma. Front Biosci. 13:2516–2526. 2008.
|
|
3.
|
Lo Muzio L, Farina A, Rubini C, et al:
Effect of c-Met expression on survival in head and neck squamous
cell carcinoma. Tumour Biol. 27:115–121. 2006.
|
|
4.
|
Bottaro DP, Rubin JS, Faletto DL, et al:
Identification of the hepatocyte growth factor receptor as the
c-met proto-oncogene product. Science. 251:802–804. 1991.
|
|
5.
|
Birchmeier C and Gherardi E: Developmental
roles of HGF/SF and its receptor, the c-met tyrosine kinase. Trends
Cell Biol. 8:404–410. 1998.
|
|
6.
|
Nakamura T, Nishizawa T, Hagiya M, et al:
Molecular cloning and expression of human hepatocyte growth factor.
Nature. 342:440–443. 1989.
|
|
7.
|
Zarnegar R and Michalopoulos GK: The many
faces of hepatocyte growth factor: from hepatopoiesis to
hematopoiesis. J Cell Biol. 129:1177–1180. 1995.
|
|
8.
|
Chen YS, Wang JT, Chang YF, et al:
Expression of hepatocyte growth factor and c-met protein is
significantly associated with the progression of oral squamous cell
carcinoma in Taiwan. J Oral Pathol Med. 33:209–217. 2004.
|
|
9.
|
To C and Tsao M: The roles of hepatocyte
growth factor/scatter factor and met receptor in human cancers
(Review). Oncol Rep. 5:1013–1024. 1998.
|
|
10.
|
Uchida D, Kawamata H, Omotehara F, et al:
Role of HGF/c-met system in invasion and metastasis of oral
squamous cell carcinoma cells in vitro and its clinical
significance. Int J Cancer. 93:489–496. 2001.
|
|
11.
|
Matsumoto K, Nakamura T and Kramer RH:
Hepatocyte growth factor/scatter factor induces tyrosine
phosphorylation of focal adhesion kinase (p125(FAK)) and promotes
migration and invasion by oral squamous cell carcinoma cells. J
Biol Chem. 269:31807–31813. 1994.
|
|
12.
|
Patel SG and Shah JP: TNM staging of
cancers of the head and neck: striving for uniformity among
diversity. CA Cancer J Clin. 55:242–258. 2005.
|
|
13.
|
Kunkel M, Reichert T, Benz P, et al:
Overexpression of Glut-1 and increased glucose metabolism in tumors
are associated with a poor prognosis in patients with oral squamous
cell carcinoma. Cancer. 97:1015–1024. 2003.
|
|
14.
|
Kim CH, Moon SK, Bae JH, et al: Expression
of hepatocyte growth factor and c-Met in hypopharyngeal squamous
cell carcinoma. Acta Otolaryngol. 126:88–94. 2006.
|
|
15.
|
Sawatsubashi M, Sasatomi E, Mizokami H,
Tokunaga O and Shin T: Expression of c-Met in laryngeal carcinoma.
Virchows Arch. 432:331–335. 1998.
|
|
16.
|
Galeazzi E, Olivero M, Gervasio FC, et al:
Detection of MET oncogene/hepatocyte growth factor receptor in
lymph node metastases from head and neck squamous cell carcinomas.
Eur Arch Otorhinolaryngol. 254:S138–S143. 1997.
|
|
17.
|
Lo Muzio L, Leonardi R, Mignogna MD, et
al: Scatter factor receptor (c-Met) as possible prognostic factor
in patients with oral squamous cell carcinoma. Anticancer Res.
24:1063–1069. 2004.
|
|
18.
|
Marshall DD and Kornberg LJ:
Overexpression of scatter factor and its receptor (c-met) in oral
squamous cell carcinoma. Laryngoscope. 108:1413–1417. 1998.
|
|
19.
|
Nakajima M, Sawada H, Yamada Y, et al: The
prognostic significance of amplification and overexpression of
c-met and c-erb B-2 in human gastric carcinomas. Cancer.
85:1894–1902. 1999.
|
|
20.
|
Hanzawa M, Shindoh M, Higashino F, et al:
Hepatocyte growth factor upregulates E1AF that induces oral
squamous cell carcinoma cell invasion by activating matrix
metalloproteinase genes. Carcinogenesis. 21:1079–1085. 2000.
|
|
21.
|
Murai M, Shen X, Huang L, et al:
Overexpression of c-met in oral SCC promotes hepatocyte growth
factor-induced disruption of cadherin junctions and invasion. Int J
Oncol. 25:831–840. 2004.
|
|
22.
|
Han SU, Lee JH, Kim WH, Cho YK and Kim MW:
Significant correlation between serum level of hepatocyte growth
factor and progression of gastric carcinoma. World J Surg.
23:1176–1180. 1999.
|
|
23.
|
Moghul A, Lin L, Beedle A, et al:
Modulation of c-MET proto-oncogene (HGF receptor) mRNA abundance by
cytokines and hormones: evidence for rapid decay of the 8 kb c-MET
transcript. Oncogene. 9:2045–2052. 1994.
|
|
24.
|
Boccaccio C, Gaudino G, Gambarotta G,
Galimi F and Comoglio P: Hepatocyte growth factor (HGF) receptor
expression is inducible and is part of the delayed-early response
to HGF. J Biol Chem. 269:12846–12851. 1994.
|