Introduction
Platelet activation and aggregation represent the
first step in thrombus formation at an injured vascular site and
play a crucial role in hemostasis. Platelets are activated by
various stimuli, resulting in shape change, adhesion, aggregation
and subsequently, thrombus formation. Thrombus formation is
associated with the release of granule contents, such as
platelet-derived growth factor (PDGF)-AB and serotonin and the
release of inflammatory substances, such as soluble CD40 ligand
(sCD40L). These secreted and generated mediators trigger a positive
feedback mechanism that potentiates platelet activation (1,2).
The expression of heat shock proteins (HSPs) is
induced in a variety of cells in response to various types of
biological stress, such as heat and chemical stress (3). It is generally recognized that HSPs
can act as molecular chaperones, which prevent the aggregation of
unfolded proteins and have cytoprotective functions under certain
stressful conditions. HSP27 (HSPB1) is a member of the
low-molecular-weight HSP family (HSPB) with molecular masses
ranging from 15–30 kDa (3,4).
It is firmly established that HSP27 activity is regulated by
post-translational modifications, such as phosphorylation (3,4).
HSP27 is promptly phosphorylated in response to various types of
stress, as well as following exposure to cytokines and mitogens and
changes from an aggregated form (up to 800 kDa) to a dissociated
form (3,4). Human HSP27 is phosphorylated at
three serine residues (Ser-15, Ser-78 and Ser-82). It is recognized
that the phosphorylation of HSP27 is catalyzed by members of the
mitogen-activated protein (MAP) kinase superfamily, such as p38 MAP
kinase (3,4). However, the precise roles of
phosphorylated HSP27 have not yet been clarified.
Collagen is known to be one of the most important
physiological stimuli for human platelet activation and its
receptors on the platelet membranes are classified into two main
groups, glycoprotein (GP)VI and integrin-α2β1 (5). The firm adhesion of activated
integrin-α2β1 by binding to collagen and the strengthening of
GPVI-collagen interactions lead to integrated signaling and further
upregulation of integrin activities, thus resulting in the
enhancement of granule secretion and the development of coagulant
activity (6–8). It has been reported that p38 MAP
kinase is activated by collagen and regulates the phosphorylation
of HSP27, which is likely to be necessary for human platelet
activation (9). We have
previously demonstrated that the collagen-induced phosphorylation
of HSP27 via p44/p42 MAP kinase is sufficient for the release of
PDGF-AB and sCD40L from human platelets (10). However, the exact role of collagen
in platelet activation remains to be elucidated.
Rac is a member of the Rho family of small GTPases
(11). It is well recognized that
the Rho family regulates cytoskeletal reorganization and gene
expression. Rac is inactive when bound to GDP and is activated upon
the exchange of GDP for GTP, which leads to downstream signaling.
As regards Rac in platelets, it has been shown that platelets
express the Rho family, including Rac (12). In addition, collagen and thrombin
reportedly stimulate the activation of Rac, which is critical for
thrombus formation (12,13). However, the exact role of Rac in
human platelets has not yet been clarified. In the present study,
we investigated the involvement of Rac in the collagen-induced
release of PDGF-AB and sCD40L in human platelets. We demonstrate
that Rac regulates the collagen-induced HSP27 phosphorylation via
p44/p42 MAP kinase in human platelets, resulting in the stimulation
of PDGF-AB secretion and the release of sCD40L.
Materials and methods
Materials
Collagen was purchased from Nycomed Pharma GmbH
(Munich, Germany). NSC23766 was purchased from Tocris Bioscience
(Bristol, UK). Phospho-p44/p42 MAP kinase antibodies and p44/p42
MAP kinase antibodies were from Cell Signaling Technology, Inc.
(Beverly, MA, USA). Phospho-HSP27 (Ser-15) antibodies,
phospho-HSP27 (Ser-78) antibodies and HSP27 antibodies were from
Stressgen Biotechnologies (Victoria, BC, Canada). Phospho-HSP27
(Ser-82) antibodies were from Biomol Research Laboratories
(Plymouth Meeting, PA, USA). GAPDH antibodies were purchased from
Santa Cruz Biotechnology, Inc. (Santa Cruz Biotechnology, Inc., CA,
USA). The ECL Western blotting detection system was purchased from
GE Healthcare (Little Chalfont, UK). Other materials and chemicals
were obtained from commercial sources.
Preparation of platelets
Human blood was donated from healthy volunteers into
a 1/10 volume of 3.8% sodium citrate. Platelet-rich plasma (PRP)
was obtained from blood samples by centrifugation at 155 × g for 12
min at room temperature. Platelet-poor plasma was prepared from the
residual blood by centrifugation at 2,500 × g for 5 min. All
participants signed an informed consent agreement after receiving a
detailed explanation of the study. This study was approved by the
Ethics Committee of Gifu University Graduate School of Medicine.
Gifu, Japan.
Measurement of platelet aggregation
induced by collagen
Platelet aggregation using citrated PRP was carried
out in a PA-200 aggregometer (Kowa Co., Ltd., Tokyo, Japan), which
can determine the size of platelet aggregates based upon the
particle count using a laser scattering method (small size, 9–25
μm; medium size, 25–50 μm; large size, 50–70 μm) (14) at 37°C for 5 min with a stirring
speed of 800 rpm. The percentage of transmittance of the isolated
platelets was recorded as 0% and that of the appropriate
platelet-poor plasma (blank) was recorded as 100%. When indicated,
PRP was pre-treated with NSC23766 for 15 min.
Protein preparation following stimulation
with collagen
Following stimulation with 1.0 μg/ml collagen for 5
min (for measurement of the protein expression levels by western
blot analysis) and for 30 min (for measurement of the levels of
PDGF-AB and sCD40L), the platelet aggregation was terminated by the
addition of an ice-cold EDTA (10 mM) solution, followed by
centrifugation at 10,000 × g at 4°C for 2 min. To perform western
blot analysis, the pellet was washed twice with phosphate-buffered
saline and then lysed and immediately boiled using a lysis buffer
containing 62.5 mM Tris/Cl, pH 6.8, 2% sodium dodecyl sulfate
(SDS), 50 mM dithiothreitol and 10% glycerol as previously
described (15). To measure
PDGF-AB and sCD40L as described below, the supernatant was isolated
and stored at −20°C for subsequent ELISA.
Western blot analysis
Western blot analysis was performed as previously
described (15). Briefly,
SDS-polyacrylamide gel electrophoresis (PAGE) was performed using
the Laemmli method (16) on a 12%
or 10% polyacrylamide gel. Proteins were fractionated and
transferred onto Immnobilion-P membranes (PVDF). The membranes were
blocked with 5% fat-free dry milk in Tris-Buffered saline with 0.1%
Tween-20 (TBS-T, 20 mM Tris, pH 7.6, 137 mM NaCl, 0.1% Tween-20)
for 1 h before incubating them with the indicated primary
antibodies. Phospho-p44/p42 MAP kinase antibodies, p44/p42 MAP
kinase antibodies, phospho-HSP27 (Ser-15) antibodies, phospho-HSP27
(Ser-78) antibodies and phospho-HSP27 (Ser-82) antibodies and
HSP-27 antibodies were used as primary antibodies.
Peroxidase-labeled anti-mouse IgG (Santa Cruz Biotechnology, Inc.)
or anti-rabbit IgG antibodies (KPL, Gaithersburg, MD, USA) were
used as secondary antibodies. The primary and secondary antibodies
were diluted to the optimum concentrations with 5% fat-free dry
milk in PBS-T (phosphate-buffered saline with 0.1% Tween-20). The
peroxidase activity on PVDF membranes was visualized on X-ray films
by means of an ECL western blotting detection system (GE
Healthcare) as described in the manufacturer’s instruction
manual.
Measurement of Rac activity
Following stimulation with 1.0 μg/ml collagen for 0,
1, 3 or 5 min, platelet aggregation was terminated by the addition
of an ice-cold EDTA (10 mM) solution, followed by centrifugation at
10,000 × g at 4°C for 2 min. The pellet was washed twice with
ice-cold Tris-buffered saline and Rac1 activity was determined
using the Rac1 Activation Assay kit (Millipore Corp., Temecula, CA,
USA) as described in the manufacturer’s instruction manual.
Measurement of plasma PDGF-AB and sCD40L
levels
The plasma PDGF-AB and sCD40L levels in the human
samples were determined using PDGF-AB Quantikine ELISA and
sCD40-Ligand Quantikine ELISA kits, respectively, purchased from
R&D systems, Inc. (Minneapolis, MN, USA). All assay procedures
were performed according to the manufacturer’s instructions.
Determination
Densitometric analysis was performed using Molecular
Analyst/Macintosh (Bio-Rad Laboratories, Hercules, CA, USA).
Statistical analysis
All figures shown are from representative results of
five independent experiments. The data are presented as the means ±
SEM. The data were analyzed by the Student’s t-test and a p-value
<0.05 was considered to indicate a statistically significant
difference.
Results
Effect of Rac on collagen-stimulated
human platelets
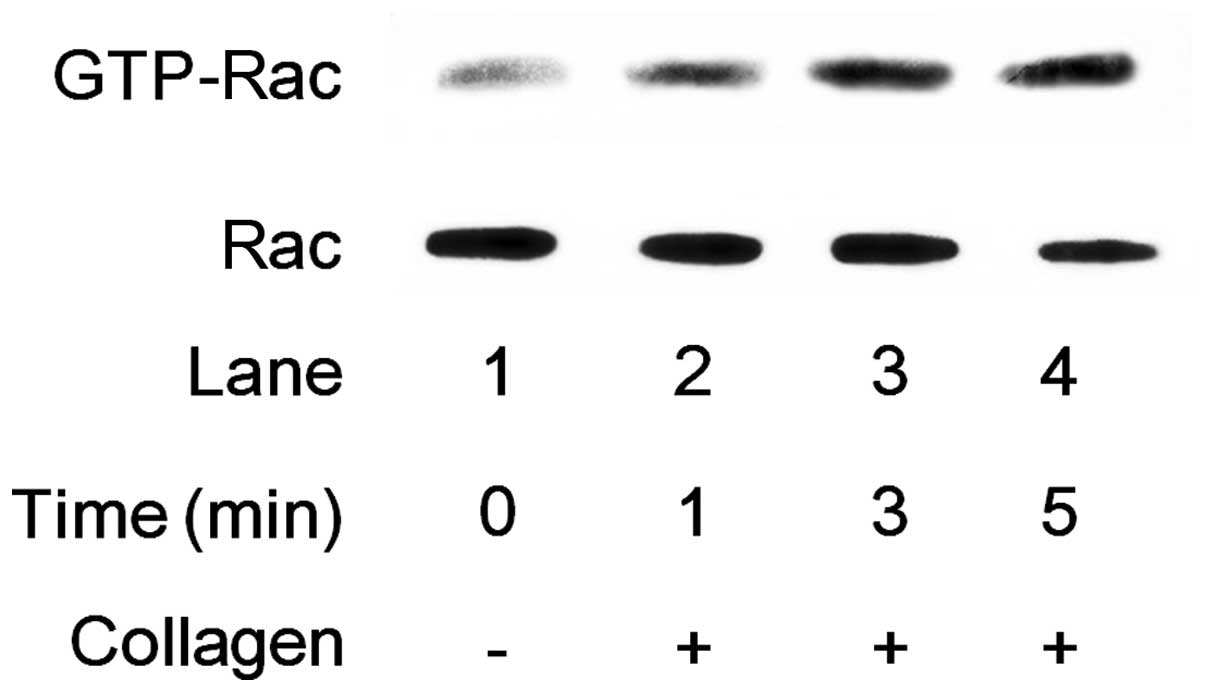
It has been demonstrated that Rac1 is involved in
collagen-induced platelet aggregation (12). Thus, in this study, we first
examined whether collagen stimulates the activation of Rac in human
platelets. Collagen (1.0 μg/ml) markedly increased the GTP-Rac
levels in human platelets in a time-dependent manner (Fig. 1).
Effect of NSC23766 on platelet
aggregation induced by collagen stimulation
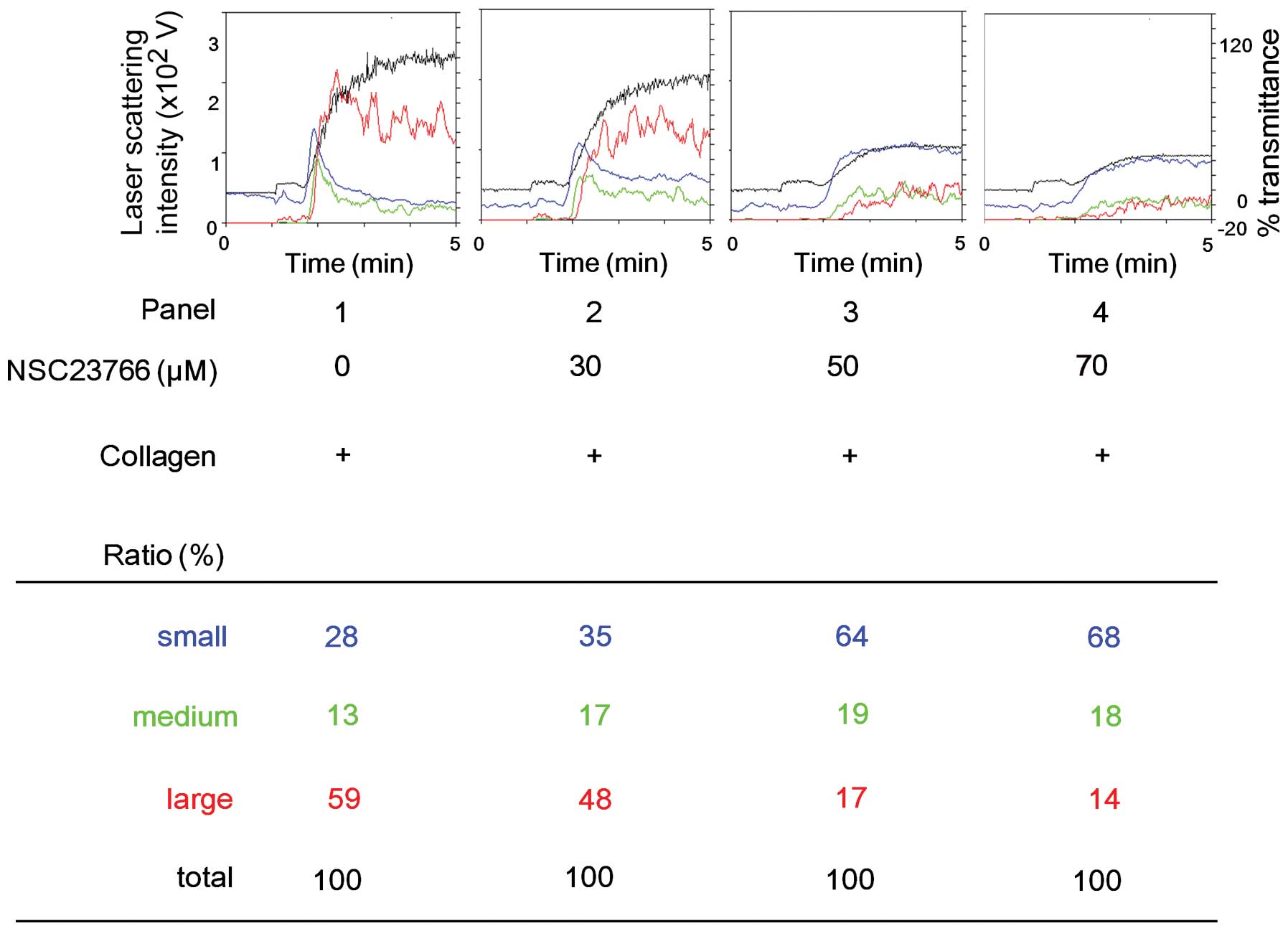
We then examined the effect of NSC23766, a selective
inhibitor of Rac1-guanine nucleotide exchange factor (GEF)
interaction (17), on the
platelet aggregation stimulated by collagen using an aggregometer
with laser scattering methods. NSC23766 markedly suppressed the
collagen-induced platelet aggregation in a dose-dependent manner in
the range between 30–70 μM (Fig.
2). According to an analysis of the size of the platelet
aggregates, the number of large aggregates (50–70 μm) decreased in
a dose-dependent manner following treatment with NSC23766. On the
other hand, NSC23766 markedly increased the number of small
aggregates (9–25 μm) (Fig.
2).
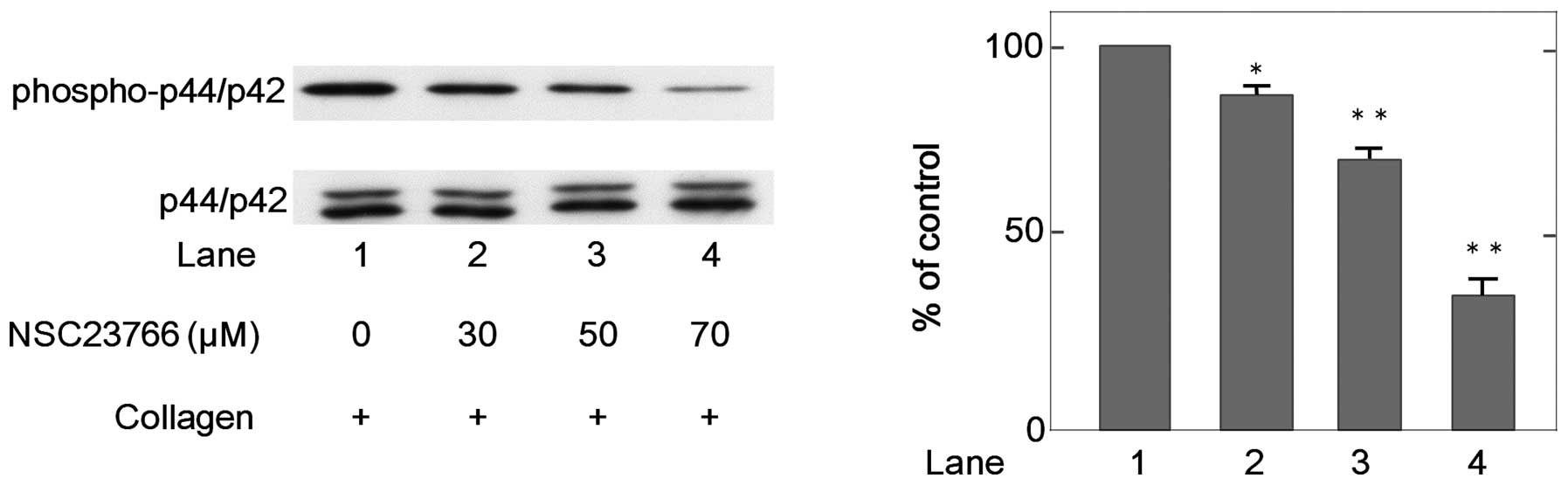
Effects of NSC23766 on the
collagen-induced phosphorylation of p44/p42 MAP kinase and
HSP27
In our previous study (10), we reported that the
phosphorylation of HSP27 via p44/p42 MAP kinase activation is
involved in the collagen-induced release of PDGF-AB and sCD40L from
human platelets. Therefore, in this study, we examined the effects
of NSC23766 on the collagen-induced phosphorylation of p44/p42 MAP
kinase and HSP27 in human platelets. NSC23766 markedly attenuated
the collagen-induced phosphorylation of p44/p42 MAP kinase in a
dose-dependent manner in the range between 30–70 μM (Fig. 3). In addition, NSC23766
significantly suppressed the collagen-induced phosphorylation of
HSP27 at three serine residues (Ser-15, Ser-78 and Ser-82) in human
platelets (Fig. 4).
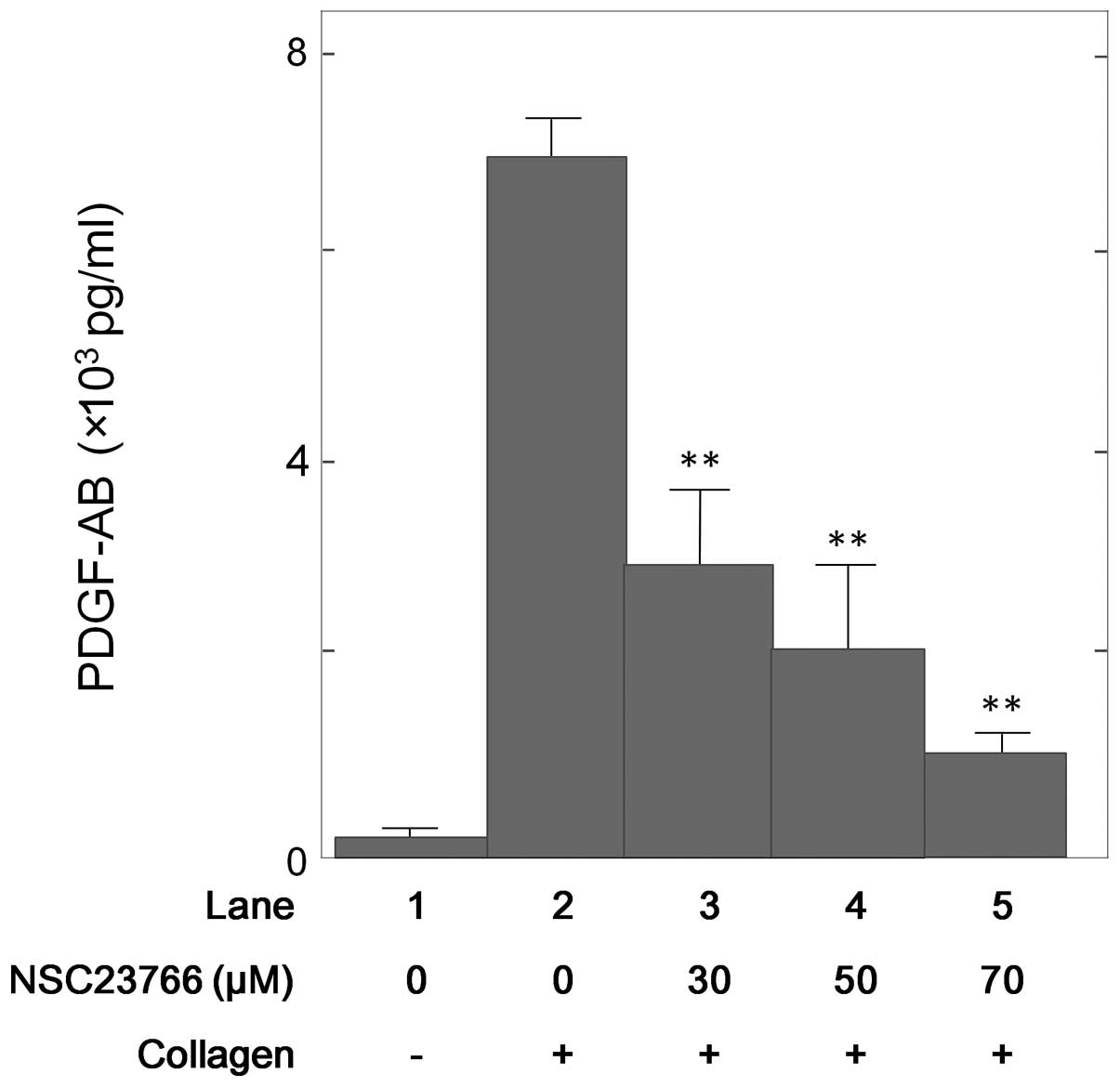
Effect of NSC23766 on the
collagen-induced platelet granule secretion
To evaluate whether NSC23766 affects the
collagen-induced platelet granule secretion, we then examined its
effect on the collagen-induced secretion of PDGF-AB from human
platelets. NSC23766 significantly suppressed the collagen-induced
PDGF-AB secretion from human platelets in a dose-dependent manner
in the range between 30–70 μM (Fig.
5).
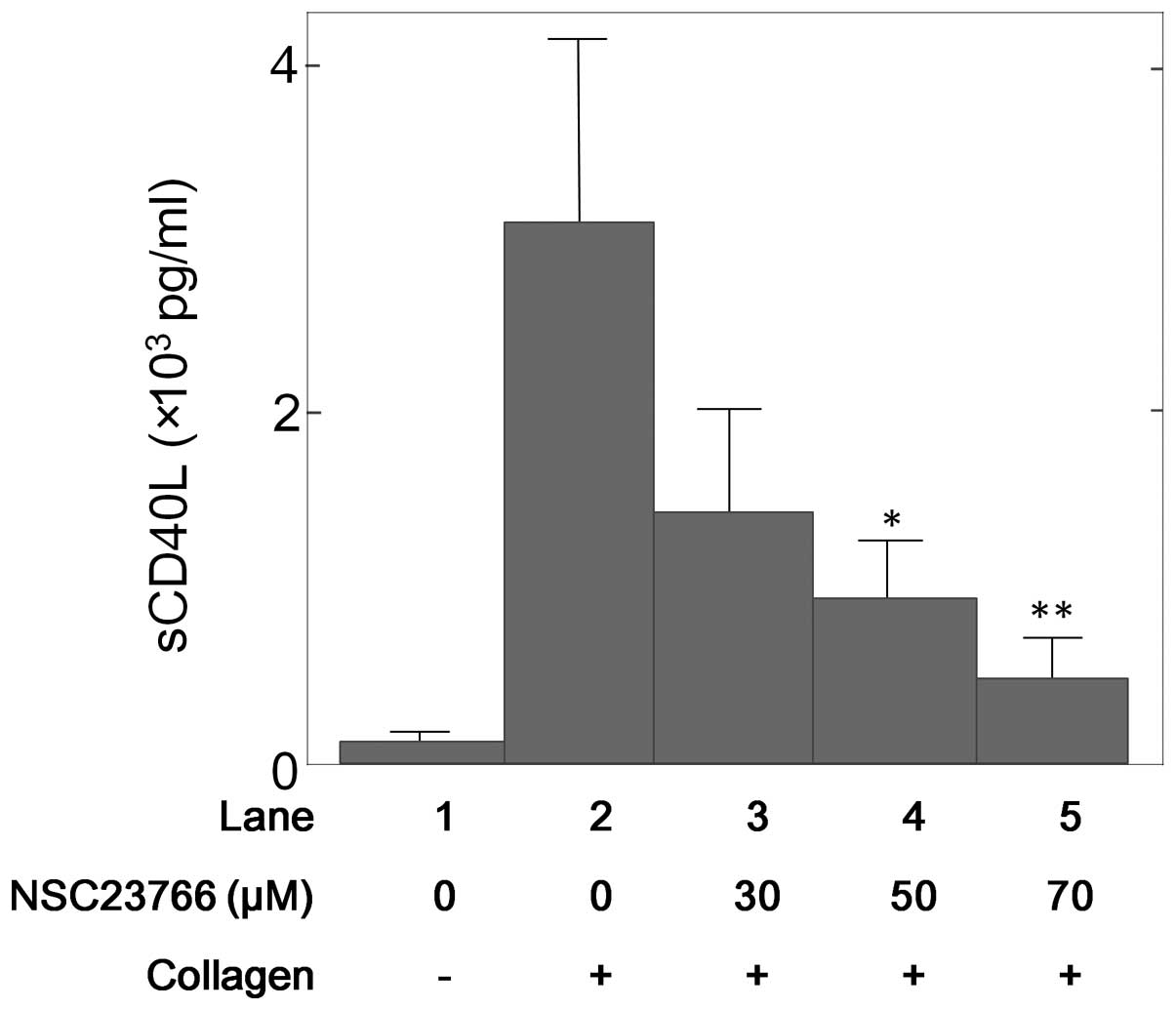
Effect of NSC23766 on the
collagen-induced release of sCD40L from human platelets
Additionally, we examined the effect of NSC23766 on
the collagen-stimulated sCD40L release from human platelets.
NSC23766 significantly reduced the collagen-stimulated release of
sCD40L (Fig. 6) and this
inhibitory effect of NSC23766 was dose-dependent in the range
between 30–70 μM.
Discussion
In the present study, we investigated the exact role
of Rac in the collagen-stimulated activation of human platelets,
paying particular attention to the association between Rac and
HSP27 phosphorylation. It has been reported that collagen
stimulates Rac GTPase activation in human platelets and that Rac is
essential for thrombus formation (12,13). We found that collagen markedly
increased the levels of GTP-Rac in human platelets in a
time-dependent manner. In addition, NSC23766, which is a selective
inhibitor of Rac1-GEF interaction (17), inhibited the collagen-induced
platelet aggregation. According to the size of the platelet
aggregates using a laser scattering method, the ratio of large
platelet aggregates (50–70 μm) decreased in a dose-dependent manner
following treatment with NSC23766, while the ratio of small
platelet aggregates (9–25 μm) markedly increased. In a previous
study (10), we demonstrated that
collagen induces the phosphorylation of HSP27 via p44/p42 MAP
kinase in human platelets, resulting in the stimulation of PDGF-AB
secretion and the release of sCD40L. Therefore, in this study, we
investigated the involvement of Rac in the collagen-stimulated
release of PDGF-AB and sCD40L through HSP27 phosphorylation in
human platelets. NSC23766 markedly suppressed the collagen-induced
phosphorylation of p44/p42 MAP kinase and HSP27 at three residues
(Ser-15, Ser-78 and Ser-82). We also demonstrated that the
collagen-induced granule secretion of PDGF-AB was significantly
decreased by pre-treatment with NSC23766. In addition, NSC23766
attenuated the release of sCD40L stimulated by collagen. Taking our
findings into account as a whole, it is most likely that Rac
activated by collagen functions at a point upstream from p44/p42
MAP kinase and regulates the phosphorylation of HSP27 in human
platelets, resulting in the stimulation of PDGF-AB secretion and
the release of sCD40L.
Collagen is a major component of the extracellular
matrix and plays a central role in the hemostatic cascade at sites
of vascular injury (9,18). It is firmly established that the
materials stored in specific granules, such as dense granules and
α-granules are secreted from activated platelets. Dense granules
contain small non-protein molecules, including adenosine
diphosphate (ADP) and 5-hydroxytryptamine. On the other hand,
α-granules contain large adhesive and healing proteins, such as
PDGF-AB and P-selectin (19).
PDGF-AB released from platelet α-granules is a potent mitogenic
growth factor, which mainly acts on connective tissue, such as
vascular smooth muscle cells and promotes atherosclerosis (20). In addition, activated platelets
release inflammatory mediators of atherosclerosis, such as CD40L.
CD40L is stored in the cytoplasm of unstimulated platelets and
rapidly translocates to the surface following platelet activation
by agonists, such as collagen (21,22). CD40L expressed on the activated
platelet surface undergoes a cleavage that generates a functional
soluble fragment, termed sCD40L. It is recognized that the release
of sCD40L from platelets induces inflammatory responses via CD40,
which is expressed on vascular endothelial cells and neurtrophils
(23). The elevation of plasma
sCD40L is reportedly associated with an increased risk of
cardiovascular events in patients with unstable coronary artery
disease (24). In the present
study, we found that the collagen-induced secretion of PDGF-AB from
α-granules and the release of sCD40L were significantly inhibited
by pre-treatment with NSC23766. Based on these findings, it seems
likely that Rac stimulated by collagen in human platelets may
affect atherosclerosis and inflammation by regulating the levels of
PDGF-AB and the release of sCD40L and that the effect of Rac on
platelets is due to HSP27 phosphorylation via p44/p42 MAP
kinase.
In conclusion, our results strongly suggest that Rac
regulates collagen-induced HSP27 phosphorylation via p44/p42 MAP
kinase in human platelets, resulting in the stimulation of PDGF-AB
secretion and the release of sCD40L.
Acknowledgements
We are very grateful to Yumiko Kurokawa for her
skillful technical assistance. This study was supported in part by
a Grant-in-Aid for Scientific Research (nos. 20590565 and 20591825)
from the Ministry of Education, Science, Sports and Culture of
Japan and a Research Grant for Longevity Sciences (22-4) from the
National Center for Geriatrics and Gerontology, Japan.
References
|
1
|
Kahner BN, Shankar H, Murugappan S, Prasad
GL and Kunapuli SP: Nucleotide receptor signaling in platelets. J
Thromb Haemost. 4:2317–2326. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li Z, Delaney MK, O’Brien KA and Du X:
Signaling during platelet adhesion and activation. Arterioscler
Thromb Vasc Biol. 30:2341–2349. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Benjamin IJ and McMillan DR: Stress (heat
shock) proteins molecular chaperones in cardiovascular biology and
disease. Circ Res. 83:117–132. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mymrikov EV, Seit-Nebi AS and Gusev NB:
Large potentials od small heat shock proteins. Physiol Rev.
91:1123–1159. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kahn ML: Platelet-collagen responses:
molecular basis and therapeutic promise. Semin Thromb Hemost.
30:419–425. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shattil SJ and Newman PJ: Integrins:
dynamic scaffolds for adhesion and signaling in platelets. Blood.
104:1606–1615. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nieswandt B and Watson SP:
Platelet-collagen interaction: is GPVI the central receptor? Blood.
102:449–461. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moroi M and Jung SM: Platelet grycoprotein
VI: its structure and function. Thromb Res. 114:221–233. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saklatvala J, Rawlinson L, Waller RJ,
Sarsfield S, Lee JC, Morton LF, Barnes MJ and Farndale RW: Role for
p38 mitogen-activated protein kinase in platelet aggregation caused
by collagen or a thromboxane analogue. J Biol Chem. 271:6586–6589.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kato H, Adachi S, Doi T,
Matsushima-Nishiwaki R, Minamitani C, Akamatsu S, Enomoto Y, Tokuda
H, Otsuka T, Iwama T, Kozawa O and Ogura S: Mechanism of
collagen-induced release of 5-HT, PDGF-AB and sCD40L from human
platelets: role of HSP27 phosphorylation via p44/p42 MAPK. Thromb
Res. 126:39–43. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Takai Y, Sasaki T and Matozaki T: Small
GTP-binding proteins. Physiol Rev. 81:153–208. 2001.PubMed/NCBI
|
|
12
|
Pleines I, Elvers M, Strehl A, Pozgajova
M, Varga-Szabo D, May F, Chrostek-Grashoff A, Brakebusch C and
Nieswandt B: Rac1 is essential for phospholipase C-γ2 activation in
platelets. Pflugers Arch. 457:1173–1185. 2009.
|
|
13
|
Soulet C, Gendreau S, Missy K, Benard V,
Plantavid M and Payrastre B: Characterisation of Rac activation in
thrombin-and collagen-stimulated human blood platelets. FEBS Lett.
507:253–258. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tohgi H, Takahashi H, Watanabe K, Kuki H
and Shirasawa Y: Development of large platelet aggregates from
small aggregates as determined by laser-light scattering: effects
of aggregant concentration and antiplatelet medication. Thromb
Haemost. 75:838–843. 1996.
|
|
15
|
Kato K, Ito H, Hasegawa K, Inaguma Y,
Kozawa O and Asano T: Modulation of the stress-induced synthesis of
hsp27 and αB-crystallin by cyclic AMP in C6 rat glioma cells. J
Neurochem. 66:946–950. 1996.
|
|
16
|
Laemmli UK: Cleavage of structural
proteins during the assembly of the head of bacteriophage T4.
Nature. 227:680–685. 1970. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gao Y, Dickerson JB, Guo F, Zheng J and
Zheng Y: Rational design and characterization of a Rac
GTPase-specific small molecule inhitor. Proc Natl Acad Sci USA.
101:7618–7623. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Davi G and Patrono C: Platelet activation
and atherothrombosis. N Engl J Med. 357:2482–2494. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rendu F and Brohard-Bohn B: The platelet
release reaction: granules’ constituents, secretion and functions.
Platelets. 12:261–273. 2001.
|
|
20
|
Heldin CH and Westermark B: Mechanism of
action and in vivo role of platelet-derived growth factor. Physiol
Rev. 79:1283–1316. 1999.PubMed/NCBI
|
|
21
|
Hermann A, Rauch BH, Braun M, Schror K and
Weber AA: Platelet CD40 ligand (CD40L)-subcellular localization,
regulation of expression, and inhibition by clopidogrel. Platelets.
12:74–82. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Andre P, Nannizzi-Alaimo L, Prasad SK and
Phillips DR: Platelet-derived CD40L: the switch-hitting player of
cardiovascular disease. Circulation. 106:896–899. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Henn V, Slupsky JR, Grafe M,
Anagnostopoulos I, Forster R, Muller-Berghaus G and Kroczek RA:
CD40 ligand on activated platelets triggers an inflammatory
reaction of endothelial cells. Nature. 391:591–594. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Heeschen C, Dimmeler S, Hamm CW, van den
Brand MJ, Boersma E, Zeiher AM and Simoons ML; CAPTURE Study
Investigators. Soluble CD40 ligand in acute coronary syndromes. N
Engl J Med. 348:1104–1111. 2003. View Article : Google Scholar : PubMed/NCBI
|