Introduction
Non-alcoholic fatty liver disease (NAFLD) is one of
the most prevalent types of liver diseases. NAFLD prevalence has
increased with the change in eating habits, thus identifying
effective treatment for NAFLD is a significant public health
objective. Lifestyle-related factors such as poor diet, obesity,
excessive alcohol intake, diabetes and hyperlipidemia have all been
proposed to contribute to NAFLD. In addition to the development of
a fatty liver, NAFLD patients may also exhibit inflammation,
necrosis and fibrosis of the liver, which are known as
non-alcoholic steatohepatitis (NASH) (1). This disease may progress to
cirrhosis of the liver and hepatocellular carcinoma (HCC).
Lifestyle interventions such as improvement of eating habits or
physical activity are commonly recommended for NAFLD and NASH, but
no effective medical therapy for these diseases has been
established although many medications for the treatment of NAFLD
are undergoing clinical trials in the Western countries.
Green tea contains high levels of flavonoids, which
have antioxidant properties. Catechin, one of the main flavonoids
in green tea, has recently attracted attention for its antitumor
and anti-arteriosclerotic effects. Catechins account for ~20% of
the flavonoids in green tea leaves. They have been found to
decrease oxidative stress (2) and
to exert anti-virus (3,4), anti-thrombotic (5), anti-allergenic (6), anticancer (7), anti-hypertensive (8) and anti-hyperglycemic effects
(9,10). In addition, results of animal
experiments have indicated that catechins affect the lipid
metabolism by decreasing triglyceride and total cholesterol levels
(11) and enhancing energy
utilization (12). However, the
effect of the green tea with high-density catechins on humans and
its detailed mechanism have yet to be clarified. To the best of our
knowledge, this is the first study to examine the effects of green
tea containing high-density catechins on NAFLD in humans. We report
herein the results of a double-blind, controlled study examining
the effects of green tea containing high-density catechins and a
catechin-free green tea-flavored control beverage on liver function
and fatty liver status in NAFLD patients. We found that NAFLD
patients consuming green tea with high-density catechins for 12
weeks showed improved liver function and reduced liver fat
deposition. In addition, we examined the safety of consuming green
tea with high-density catechins for NAFLD patients.
Materials and methods
Subject selection
In total, 17 NAFLD patients (7 men and 10 women),
aged 20–70 years, were included in this randomized, double-blind,
controlled, investigator-initiated trial. The exclusion criteria
were the presence of severe acute or chronic diseases (liver, heart
or renal failure), infectious or autoimmune liver diseases
(positive for hepatitis B surface antigens, anti-hepatitis C virus,
anti-nuclear or anti-mitochondrial antibodies), known allergies to
compounds of tea or polyphenol-rich food, acute infectious
diseases, diseases involving systemic inflammation, participation
in another study within the last month, alcohol abuse and the use
of concomitant supplements. Green tea adjusted to 1,080 mg/700 ml
or 200 mg/700 ml catechin content and green tea-flavored beverage
(0 mg/700 ml catechin content) were prepared by Kao Corporation
(Tokyo, Japan). The beverages were packaged in 350 ml steel cans
with an identical appearance and distributed to patients by
courier. An independent investigator performed subject
randomization. All the patients provided informed written consent
to participate in the study. The study was performed at the Kurume
University Hospital and the study protocol conformed to the ethics
guidelines of the 1975 Helsinki Declaration, as reflected in prior
approval by the institutional Ethics Committee of the Kurume
University School of Medicine.
Experimental protocol
Each patient was instructed to refrain from eating
flavonoid-rich foods and supplements during the trial and was then
instructed to fast for 8 h before undergoing the examinations,
which were always performed in the morning. These included clinical
examination (height, weight and body fat percentage), blood and
urine sampling and routine abdominal ultrasonography. Body mass
index (BMI) was calculated as weight in kilograms divided by the
square of height in meters. The rate of body fat was estimated by
bioelectrical impedance analysis performed using
InnerScan® (Tanita BC-511, Tanita Corporation, Tokyo,
Japan) (13,14). The green tea beverages were
consumed for 12 weeks. During this period, patients underwent
follow-up examinations in the fourth, eighth and twelfth week.
Additional follow-up data were collected four weeks after the end
of the green tea consumption. Quantitative abdominal computerized
tomography (CT) was performed at the beginning and the end of the
study period.
Green teas and placebo (control)
Patients were randomized to consume one of the three
types of green tea for 12 weeks. Green tea containing 1,080 mg/700
ml or 200 mg/700 ml catechins and green tea-flavored beverage (0
mg/700 ml catechins) were prepared by Kao Corporation (Tokyo,
Japan). Patients consumed 700 ml of green tea every day with meals.
The tea containing 200 mg catechins per 700 ml was similar in
catechin contents to most commercially available green teas. The
intake quantity of 700 ml per day is typical of Japanese tea
intake. Caffeine content, another component of green tea, was
normalized in all three teas to 120 mg per 700 ml.
Quantitative abdominal CT
Abdominal CT was performed to determine the size of
each patient’s liver and spleen. Findings of many reports have
shown that CT liver attenuation corrected for spleen attenuation
allows more accurate evaluations of the pathological
hepatosteatosis (15–17). Therefore we measured liver
attenuation at five sites by CT, one in each hepatic segment from
segment II to segment VIII (Couinaud classification), in order to
calculate the average liver attenuation. Similarly we also measured
spleen attenuation at five sites and calculated the average spleen
attenuation. The ratio of liver to spleen attenuation was then
calculated and values were compared before and after green tea
consumption.
Biomarkers of oxidative stress
Recently, 8-isoprostane (prostaglandin F2α) has
attracted attention as an in vivo indicator of oxidative
stress due to its relative stability among prostaglandin isomers
(18,19). Urine 8-isoprostane was measured
using an EIA kit (Cayman Chemical Company, MI, United States). This
assay was based on competition between 8-isoprostane and an
8-isoprostane-acetylcholinesterase conjugate (8-isoprostane tracer)
for a limited number of 8-isoprostane-specific rabbit anti-serum
binding sites. As the concentration of the 8-isoprostane tracer
remained constant while the concentration of 8-isoprostane varied,
the amount of 8-isoprostane tracer that was able to bind to the
rabbit anti-serum was inversely proportional to the concentration
of 8-isoprostane in the well. This rabbit anti-serum-8-isoprostane
complex bound to a mouse monoclonal anti-rabbit IgG antibody that
was also attached to the well. The plate was washed to remove any
unbound reagents and then acetylcholinesterase substrate was added
to the well. The product of this enzymatic reaction had a distinct
yellow color and was absorbed strongly at 412 nm. The intensity of
this color, determined spectrophotometrically, was proportional to
the amount of 8-isoprostane tracer bound to the well. Data were
corrected for urine creatinine and the urine 8-isoprostane
(pg/ml)/creatinine (mg/ml) ratio was expressed as urine
8-isoprostane (pg/mg creatinine).
Statistical analysis
Data are expressed as means ± SD. Associations among
the three patient groups for baseline characteristics, liver CT
attenuation and urine 8-isoprostane were compared using analysis of
variance (ANOVA). Within each group, comparisons were made using
the Student’s paired t-test. P<0.05 was considered statistically
significant. Statistical analyses were performed using AIST-ANOVA
developed by the National Metrology Institute of Japan (NMIJ) and
National Institute of Advanced Industrial Science and Technology
(AIST) for statistical analysis.
Results
Subject demographics
Seventeen patients were included in the present
study and were randomized to consume either green tea with high- or
low-density catechins or a control beverage with no catechins.
Clinical and laboratory characteristics of the study population are
presented in Tables I and
II, respectively. There were no
significant differences among the three groups for clinical
characteristics at baseline, including age, body weight, body fat
percentage or BMI (Table I).
There were also no significant differences among the three groups
in laboratory data at baseline (Table II).
 | Table IBaseline clinical characteristics
(n=17). |
Table I
Baseline clinical characteristics
(n=17).
| Group | Placebo (n=5) | Low-density catechins
(n=5) | High-density
catechins (n=7) | P-value |
|---|
| Age (years) | 54.2±8.1 | 51.4±14.8 | 47.1±17.2 | 0.30 |
| Body weight (kg) | 74.1±18.3 | 77.6±13.8 | 70.7±13.0 | 0.74 |
| Body fat (%) | 36.1±6.2 | 36.0±4.8 | 34.3±6.9 | 0.85 |
| Body mass index
(kg/m2) | 30.0±4.4 | 29.1±1.8 | 28.0±2.0 | 0.48 |
 | Table IIBaseline laboratory characteristics (n
= 17). |
Table II
Baseline laboratory characteristics (n
= 17).
| Group | Placebo (n=5) | Low-density catechins
(n=5) | High-density
catechins (n=7) | P-value |
|---|
| AST (IU/l) | 110±58 | 104±47 | 120±57 | 0.88 |
| ALT (IU/l) | 94±50 | 81±47 | 101±95 | 0.89 |
| LDH (IU/l) | 225±39 | 220±32 | 224±59 | 0.96 |
| ALP (IU/l) | 198±75 | 246±82 | 230±63 | 0.61 |
| γ-GTP (IU/l) | 69±54 | 74±44 | 81±51 | 0.33 |
| Ch-E (IU/l) | 194±24 | 201±32 | 191±42 | 0.53 |
| Total protein
(g/dl) | 7.9±1.0 | 7.5±0.9 | 7.1±0.7 | 0.20 |
| Total bilirubin
(mg/dl) | 0.8±0.4 | 0.9±0.3 | 0.9±0.3 | 0.70 |
| BUN (mg/dl) | 10.1±5.0 | 9.5±3.8 | 11.0±3.4 | 0.51 |
| Creatinine
(mg/dl) | 0.9±0.4 | 1.0±0.3 | 1.1±0.2 | 0.64 |
| Total cholesterol
(mg/dl) | 161±59 | 197±33 | 189±55 | 0.61 |
| Glucose
(mg/dl) | 97±18 | 99±21 | 94±19 | 0.18 |
| Hemoglobin
(g/dl) | 12.8±1.2 | 14.1±2.4 | 11.5±1.9 | 0.56 |
| Erythrocytes
(104/μl) | 390±41 | 411±60 | 405±55 | 0.21 |
| MCV (fl) | 90.3±7.0 | 89.5±8.1 | 91.2±9.4 | 0.87 |
| MCH (pg) | 31.4±3.0 | 30.8±2.5 | 32.5±2.9 | 0.90 |
| Thrombocytes
(104/μl) | 19.5±5.5 | 17.9±6.8 | 18.6±4.9 | 0.84 |
| Leukocytes
(103/μl) | 6.3±2.1 | 5.2±2.9 | 6.2±1.9 | 0.87 |
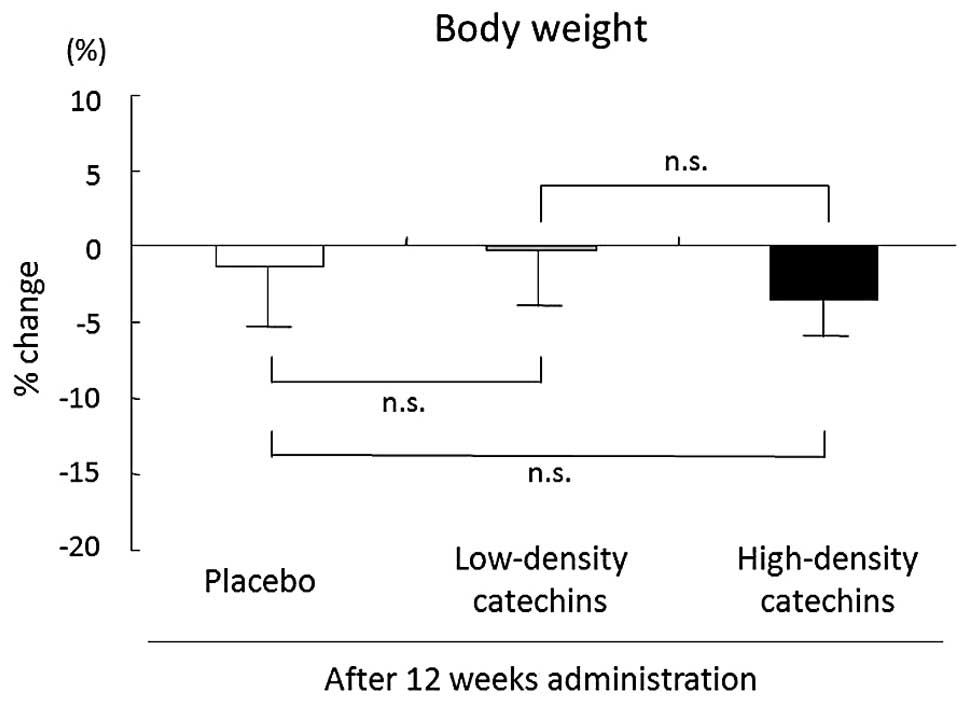
Reduction of body fat percentage in the
high-density catechin group
Comparison of the data at baseline and 12 weeks
later showed that the largest decrease in body weight occurred in
the high-density catechin group. However, there was no significant
difference in the percentage change of body weight among the three
groups (high-density catechins, −3.8±2.7%; low-density catechins,
−0.9±3.5%; placebo, −1.4±3.7%; Fig.
1).
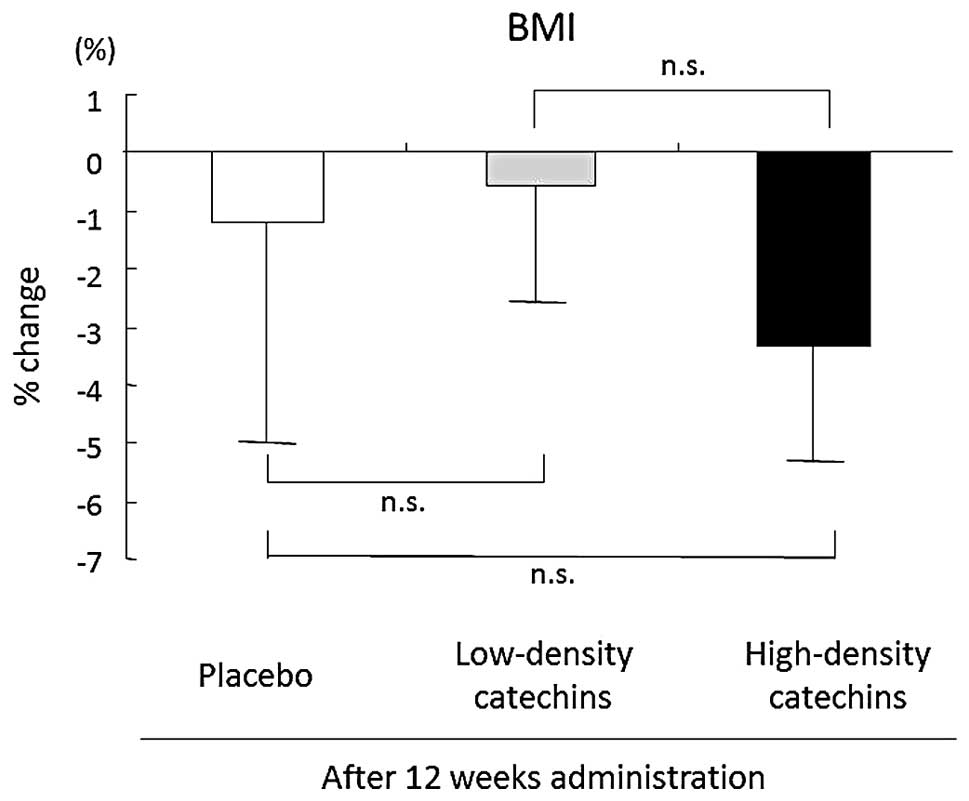
BMI also decreased after 12 weeks of tea
consumption, but there was no significant difference among the
three groups (high-density catechins, −3.3±1.9%; low-density
catechins, −0.5±2.0%; placebo, −1.2±3.9%; Fig. 2).
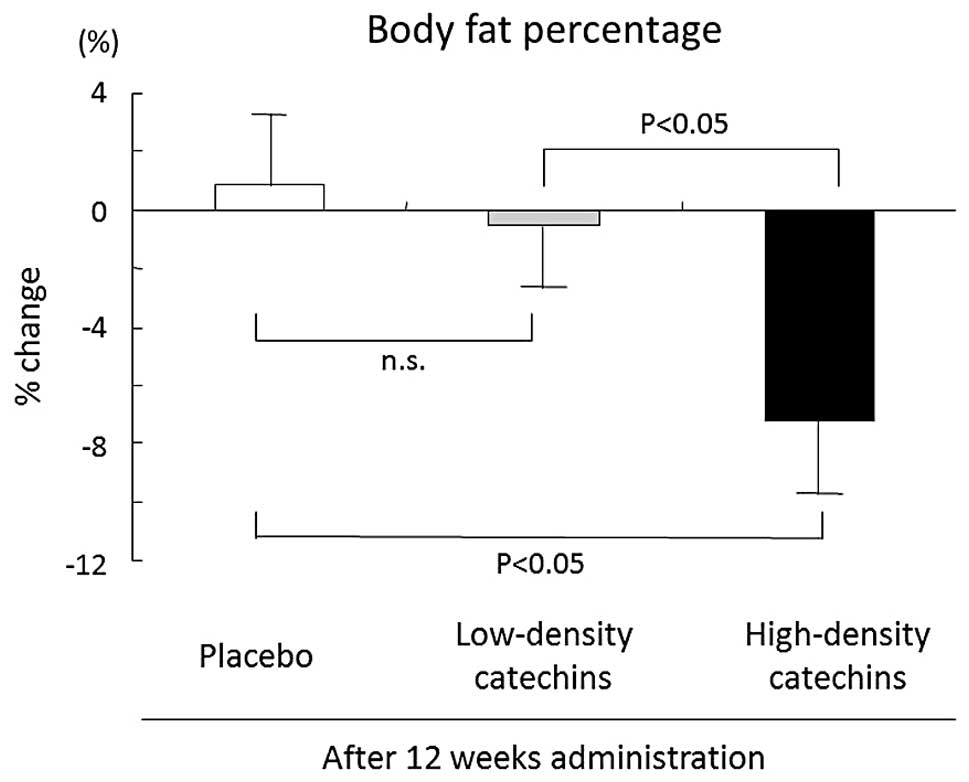
Body fat percentage decreased significantly from
34.3±6.9% (baseline) to 31.8±6.0% after 12 weeks of high-density
catechin tea consumption (P<0.05). Body fat percentage decreased
significantly more in the high-density catechin group (−7.3±2.2%)
than in the placebo (0.9±2.1%) and low-density catechin (−0.6±2.4%)
groups after 12 weeks (Fig.
3).
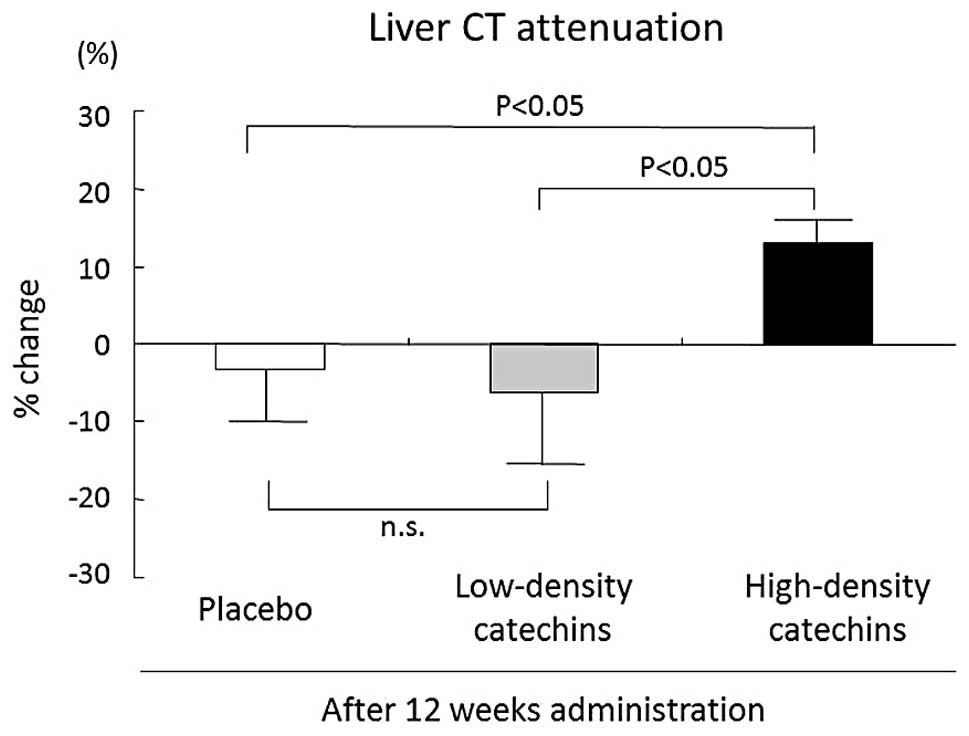
The liver-to-spleen CT attenuation ratio increased
from 91.8±4.6% (baseline) to 101.8±4.7% after 12 weeks of
consumption of high-density catechin tea. The liver-to-spleen CT
attenuation ratio showed greater improvement in all patients in the
high-density catechin group (11.3±2.8%) than in the placebo
(−3.3±8.5%) and low-density catechin (−6.1±12.1%) groups (Fig. 4).
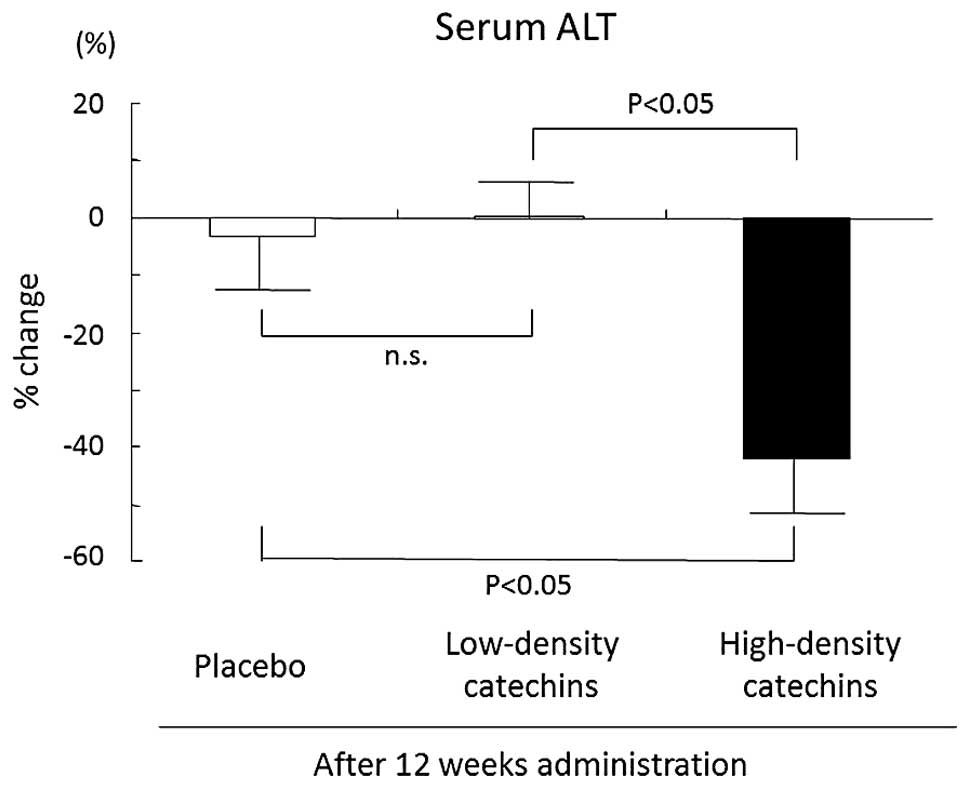
Improvement of serum alanine
aminotransferase (ALT) levels by high-density catechin
treatment
Serum ALT is an important marker of liver
inflammation. Percentage change in serum ALT levels was
significantly more negative in the high-density catechin group
(−42.1±11.3%) than in the placebo (−3.1±7.8%) and low-density
catechin (0.5±5.1%) groups after 12 weeks of consumption of
high-density catechin tea (Fig.
5).
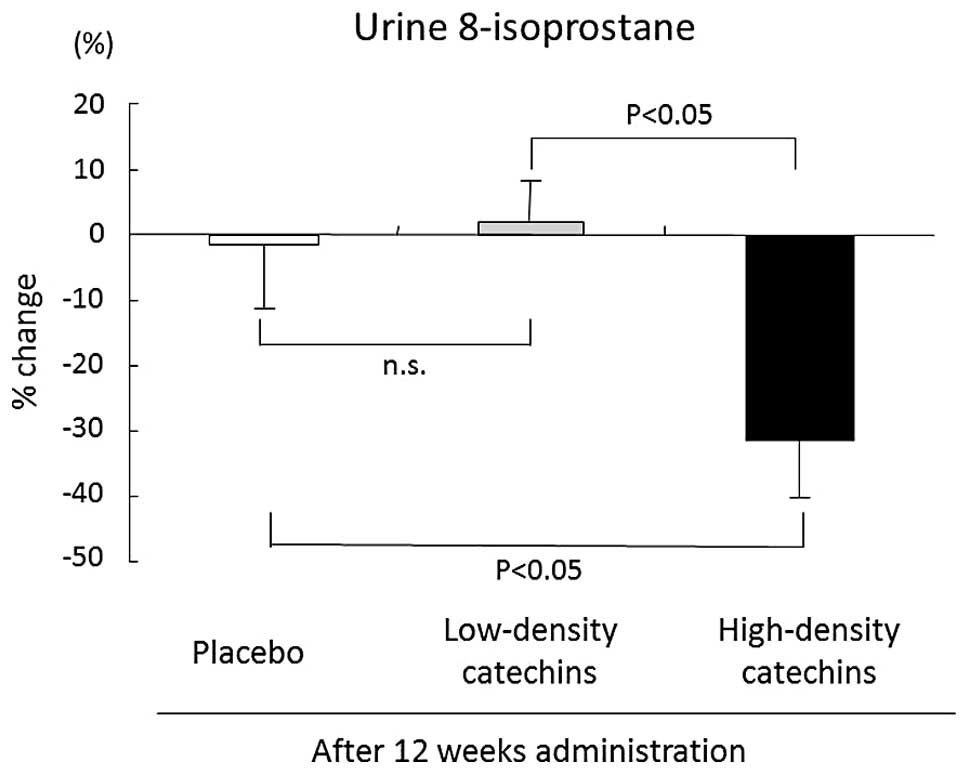
Reduction of urinary 8-isoprostane
excretion by high-density catechin treatment
Urine 8-isoprostane is a specific marker of
oxidative stress. Urine 8-isoprostane excretion was reduced from
249.6±11.6 pg (baseline) to 172.0±9.0 pg after 12 weeks of
high-density catechin tea consumption. The percentage change in
8-isoprostane levels was worse in the high-density catechin group
(−31.1±9.0%) than in the placebo (−1.7±9.1%) or low-density
catechin (2.1±6.1%) groups (Fig.
6).
Discussion
NAFLD is a prevalent disease that is detected by
medical examination and ultrasonography. Among NAFLD categories,
patients with NASH, which is similar to alcoholic steatohepatitis
in terms of pathological findings, have a poor prognosis (20). The lesions most commonly accepted
with NASH include steatosis, ballooning degeneration of hepatocyte,
mild diffuse lobular mixed acute and chronic inflammation and
perivenular and perisinusoidal collagen deposition. Mallory’s
hyaline, vacuolated nuclei in periportal hepatocytes, lobular
lipogranulomas and PAS-diastase-resistant Kupffer cells are also
common in NASH. NASH may be an underlying cause of cryptogenic
cirrhosis (21,22). The worldwide epidemic of obesity
has increased the awareness of NAFLD from that of a curiosity to
one of a potentially progressive liver disease that increases the
risk of cirrhosis and HCC (23).
A report by Marrero et al (24) indicated that cryptogenic liver
disease is a common etiology of diseases in patients with HCC.
NAFLD has been reported to account for at least 13% of HCC cases
(24). Cryptogenic cirrhosis
patients were found to have higher plasma levels of glucose,
cholesterol and triglyceride, all parameters of insulin resistance
(22). Obesity is an independent
risk factor for HCC in patients with cryptogenic cirrhosis
(25). Not all cases of NAFLD
progress to cirrhosis and liver cancer. Early diagnosis and
treatment of NAFLD may prevent progression to cirrhosis. As
reported above, the improvement of eating habits is necessary to
improve hyperlipidemia, insulin resistance and obesity.
As for whether green tea is effective for the
improvement of insulin resistance and hyperlipidemia when consumed
with a meal, the present study indicates that it is effective for
treatment in NAFLD. It is believed that dietary therapy is
preferable to medical therapy for the treatment of NAFLD,
considering the mechanism of onset, but lifestyle changes can be
difficult to implement. Thus, the development of an effective
medical therapy is necessary. Epigallocatechin gallate (EGCG), the
main catechin in green tea, is believed to reduce liver oxidation
stress. The components of NAFLD have not yet been fully elucidated,
but the following steps are considered to be the main mechanism.
Free fatty acids are absorbed by the liver through the intestinal
tract after a meal and are oxidized by mitochondria and
peroxisomes. If fatty acid uptake by hepatocytes increases, fatty
acid pools in the liver increase and accumulate in the hepatocytes
as acylglycerol, increasing the load on hepatic mitochondria. Fatty
acids that are not metabolized by mitochondria undergo ω or β
oxidation by microsomes or peroxisomes. If a large quantity of
fatty acids continues to be deposited in the liver, accumulation of
acylglycerol in the hepatocytes induces oxidative stress that may
progress to NAFLD (26). It is
thought that EGCG reduces oxidative stress in hepatocytes through
its potent antioxidant activity. Our study showed that the group
consuming 1,080 mg of catechins per day had significantly lower
levels of urine 8-isoprostane, a marker of oxidative stress, at the
end of the study than at baseline. The low-density catechin and
placebo groups did not show decreased oxidative stress, suggesting
that it is necessary to consume ~1 g of catechins every day to
reduce oxidative stress.
Catechins have inhibition effects on lipase, an
enzyme related to glucose and fat absorption. EGCG shows inhibitory
activity against lipase at a concentration of 0.349 μM (IC50)
(27). In addition, catechins are
reported to have inhibitory effects on α-amylase and α-glucosidase
(27,28). A clinical study of
hypertriacylglycerolaemia showed that the increase of
triacylglycerol levels in the plasma after oral administration of
butter was blunted by ~29% in response to catechin consumption
(29). If fat absorption in the
intestinal tract is decreased, liver fatty acid uptake also
decreases, which may help prevent the onset of NAFLD.
It has been shown that catechins promote lipid
metabolism in the liver (30).
Body weight and adiposity were blunted by catechin administration
in the obese mouse model C57BL/6J. Increased mRNA expression of
acyl-CoA oxidase (ACO), one of the peroxisomal β-oxidizing enzymes
and medium-chain acyl-CoA dehydrogenase (MCAD), a mitochondrial
β-oxidizing enzyme, was observed in the liver of the catechin
administration group. Increased hepatocellular mitochondrial
β-oxidation activity promotes the breakdown of fatty acids and it
is thought that it acts as a protective mechanism against
NAFLD.
Catechins are a natural iron chelator and also serve
to influence internal absorption of iron. A controlled study
looking at the effects of EGCG on non-heme iron absorption showed
that it was decreased by 27% in patients consuming 300 mg EGCG
compared with controls consuming placebo (31). Reports on NASH patients showed
that elevated iron stores, iron absorption in the liver (32) and serum ALT levels were decreased
by bloodletting treatment (33).
Restricting iron absorption through catechins may therefore be
effective treatment for NAFLD.
NAFLD is a widespread disease and some cases of
NAFLD progress to NASH. It is thought that the existence of
steatosis and hepatitis is crucial for a diagnosis of NASH, which
can be confirmed by a liver biopsy. Liver biopsy is the golden
standard for NASH diagnosis. However, many patients without
symptoms who present abnormal serum data, suggesting the presence
of NAFLD, do not undergo a liver biopsy. For the present study, we
used ultrasonography and X-ray CT to monitor NAFLD as these methods
are non-invasive and follow-up data can be collected. Blood
biochemistry was used for the determination of hepatitis and
steatosis status (34). The
present study included only patients who had been diagnosed with
NAFLD by a specialist. We instructed some participants to consume
tea containing five times as much catechin content as normal tea
for 12 weeks and did not observe any negative side effects in this
group.
The mechanism of onset of NAFLD and NASH has still
not been fully elucidated (35).
The mechanism by which ingestion of catechins decreases fat
accumulation in the liver has also not been determined. Liver fat
was decreased along with an oxidative stress marker in response to
the consumption of a high catechin tea. Liver inflammation and
blood biochemistry also improved in this group. Findings of this
study suggest that catechins are useful for the treatment of
NAFLD.
Acknowledgements
The study was supported, in part, by the Japan
National Science Foundation (grant no. 16590651). All the tea was
provided by Kao Corporation, Japan. However, Kao Corporation was
not involved in the funding of or in any part of the study. Part of
this study was presented at the 41st annual meeting of the European
Association for the Study of the Liver.
Abbreviations:
|
ALT
|
alanine aminotransferase
|
|
BMI
|
body mass index
|
|
CT
|
computed tomography
|
|
EGCG
|
epigallocatechin gallate
|
|
HCC
|
hepatocellular carcinoma
|
|
NAFLD
|
non-alcoholic fatty liver disease
|
|
NASH
|
non-alcoholic steatohepatitis
|
References
|
1
|
Neuschwander-Tetri BA and Caldwell SH:
Nonalcoholic steatohepatitis: summary of an AASLD single topic
conference. Hepatology. 38:1202–1219. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hakim IA, Harris RB, Brown S, et al:
Effect of increased tea consumption on oxidative DNA damage among
smokers: a randomized controlled study. J Nutr. 133:3303S–3309S.
2003.PubMed/NCBI
|
|
3
|
Hamza A and Zhan CG: How can
(−)-epigallocatechin gallate from green tea prevent HIV-1
infection? Mechanistic insights from computational modeling and the
implication for rational design of anti-HIV-1 entry inhibitors. J
Phys Chem B. 110:2910–2917. 2006.
|
|
4
|
Xu J, Wang J, Deng F, Hu Z and Wang H:
Green tea extract and its major component epigallocatechin gallate
inhibits hepatitis B virus in vitro. Antiviral Res. 78:242–249.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Stangl V, Lorenz M and Stangl K: The role
of tea and tea flavonoids in cardiovascular health. Mol Nutr Food
Res. 50:218–228. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Maeda-Yamamoto M, Inagaki N, Kitaura J, et
al: O-methylated catechins from tea leaves inhibit multiple protein
kinases in mast cells. J Immunol. 172:4486–4492. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Khan N and Mukhtar H: Multitargeted
therapy of cancer by green tea polyphenols. Cancer Lett.
269:269–280. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim JA, Formoso G, Li Y, et al:
Epigallocatechin gallate, a green tea polyphenol, mediates
NO-dependent vasodilation using signaling pathways in vascular
endothelium requiring reactive oxygen species and Fyn. J Biol Chem.
282:13736–13745. 2007. View Article : Google Scholar
|
|
9
|
Wolfram S: Effects of green tea and EGCG
on cardiovascular and metabolic health. J Am Coll Nutr.
26:373S–388S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ueda M, Nishiumi S, Nagayasu H, Fukuda I,
Yoshida K and Ashida H: Epigallocatechin gallate promotes GLUT4
translocation in skeletal muscle. Biochem Biophys Res Commun.
377:286–290. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Koo SI and Noh SK: Green tea as inhibitor
of the intestinal absorption of lipids: potential mechanism for its
lipid-lowering effect. J Nutr Biochem. 18:179–183. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Murase T, Haramizu S, Shimotoyodome A,
Tokimitsu I and Hase T: Green tea extract improves running
endurance in mice by stimulating lipid utilization during exercise.
Am J Physiol Regul Integr Comp Physiol. 290:R1550–R1556. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kyle UG, Genton L, Hans D and Pichard C:
Validation of a bioelectrical impedance analysis equation to
predict appendicular skeletal muscle mass (ASMM). Clin Nutr.
22:537–543. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lukaski HC: Applications of bioelectrical
impedance analysis: a critical review. Basic Life Sci. 55:365–374.
1990.PubMed/NCBI
|
|
15
|
Duman DG, Celikel C, Tuney D, Imeryuz N,
Avsar E and Tozun N: Computed tomography in nonalcoholic fatty
liver disease: a useful tool for hepatosteatosis assessment? Dig
Dis Sci. 51:346–351. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Church TS, Kuk JL, Ross R, Priest EL,
Biltoft E and Blair SN: Association of cardiorespiratory fitness,
body mass index, and waist circumference to nonalcoholic fatty
liver disease. Gastroenterology. 130:2023–2030. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Oliva MR, Mortele KJ, Segatto E, et al:
Computed tomography features of nonalcoholic steatohepatitis with
histopathologic correlation. J Comput Assist Tomogr. 30:37–43.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Devaraj S, Hirany SV, Burk RF and Jialal
I: Divergence between LDL oxidative susceptibility and urinary
F(2)-isoprostanes as measures of oxidative stress in type 2
diabetes. Clin Chem. 47:1974–1979. 2001.PubMed/NCBI
|
|
19
|
Patrono C and FitzGerald GA: Isoprostanes:
potential markers of oxidant stress in atherothrombotic disease.
Arterioscler Thromb Vasc Biol. 17:2309–2315. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Powell EE, Cooksley WG, Hanson R, Searle
J, Halliday JW and Powell LW: The natural history of nonalcoholic
steatohepatitis: a follow-up study of forty-two patients for up to
21 years. Hepatology. 11:74–80. 1990.PubMed/NCBI
|
|
21
|
Brunt EM: Nonalcoholic steatohepatitis:
definition and pathology. Semin Liver Dis. 21:3–16. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bugianesi E, Leone N, Vanni E, et al:
Expanding the natural history of nonalcoholic steatohepatitis: from
cryptogenic cirrhosis to hepatocellular carcinoma.
Gastroenterology. 123:134–140. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Brunt EM: Nonalcoholic steatohepatitis:
pathologic features and differential diagnosis. Semin Diagn Pathol.
22:330–338. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Marrero JA, Fontana RJ, Su GL, Conjeevaram
HS, Emick DM and Lok AS: NAFLD may be a common underlying liver
disease in patients with hepatocellular carcinoma in the United
States. Hepatology. 36:1349–1354. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Caldwell SH, Oelsner DH, Iezzoni JC,
Hespenheide EE, Battle EH and Driscoll CJ: Cryptogenic cirrhosis:
clinical characterization and risk factors for underlying disease.
Hepatology. 29:664–669. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kersten S, Seydoux J, Peters JM, Gonzalez
FJ, Desvergne B and Wahli W: Peroxisome proliferator-activated
receptor alpha mediates the adaptive response to fasting. J Clin
Invest. 103:1489–1498. 1999. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nakai M, Fukui Y, Asami S, et al:
Inhibitory effects of oolong tea polyphenols on pancreatic lipase
in vitro. J Agric Food Chem. 53:4593–4598. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Matsui T, Yoshimoto C, Osajima K, Oki T
and Osajima Y: In vitro survey of alpha-glucosidase inhibitory food
components. Biosci Biotechnol Biochem. 60:2019–2022. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Unno T, Tago M, Suzuki Y, et al: Effect of
tea catechins on postprandial plasma lipid responses in human
subjects. Br J Nutr. 93:543–547. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Murase T, Nagasawa A, Suzuki J, Hase T and
Tokimitsu I: Beneficial effects of tea catechins on diet-induced
obesity: stimulation of lipid catabolism in the liver. Int J Obes
Relat Metab Disord. 26:1459–1464. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ullmann U, Haller J, Bakker GC, Brink EJ
and Weber P: Epigallocatechin gallate (EGCG) (TEAVIGO) does not
impair nonhaem-iron absorption in man. Phytomedicine. 12:410–415.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kohgo Y, Ohtake T, Ikuta K, Suzuki Y,
Torimoto Y and Kato J: Dysregulation of systemic iron metabolism in
alcoholic liver diseases. J Gastroenterol Hepatol. 23(Suppl 1):
S78–S81. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sumida Y, Kanemasa K, Fukumoto K, et al:
Effect of iron reduction by phlebotomy in Japanese patients with
nonalcoholic steatohepatitis: A pilot study. Hepatol Res.
36:315–321. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chalasani N, Younossi Z, Lavine JE, et al:
The diagnosis and management of non-alcoholic fatty liver disease:
practice guideline by the American Gastroenterological Association,
American Association for the study of liver diseases, and American
College of Gastroenterology. Gastroenterology. 142:1592–1609. 2012.
View Article : Google Scholar
|
|
35
|
Farrell GC, van Rooyen D, Gan L and
Chitturi S: NASH is an inflammatory disorder: pathogenic,
prognostic and therapeutic implications. Gut Liver. 6:149–171.
2012. View Article : Google Scholar : PubMed/NCBI
|