Introduction
Dental implants are commonly used in dentistry to
replace missing teeth. Despite the high success rate of dental
implants, complications are often encountered. A lot of
complications occur during the implant surgery, when vital
structures such as the nerves, vessels and sinus space are injured.
Of these complications, nerve injury is one of the most unpleasant
and troublesome for both the patient and dentist (1). Nerve injury may occur during
anesthetic injection, flap reflection, flap traction and implant
osteotomy (2,3) in the inferior alveolar, mental and
lingual nerves. Alteration in sensation manifests in the mucosa,
lower lip and chin after the nerve injury, and ranges from mild
numbness to complete anesthesia (2,3).
Generally, the first choice in treating the nerve
injury is a combination of medication and physiotherapy (4). Common medication includes oral
steroids to reduce neuritis and edema, vitamin B12 to promote
regeneration of nerve terminals, and adenosine triphosphate (ATP)
to increase blood flow by vasodilation (5). Physiotherapy, including laser
therapy and hot-pack treatment, is also effective at increasing
regional blood flow (5). However,
as reported by Kim et al (4) these therapies are limited in their
ability to treat nerve injury. Nearly 70% of patients with inferior
alveolar nerve injury showed no improvement in sensation or
dysesthesia with medication or physiotherapy, possibly due to the
low plasma concentration of the medicine at the nerve injury sites
and the short length of the physiotherapy treatment (4).
As an alternative treatment for nerve injury, growth
factors have also been previously studied, owing to the modulatory
role they play in the secretion of neurotrophic factors and
proliferation of neural cells (6,7).
An appropriate source for delivering growth factors is through
platelet concentrates. Platelets are known to release a variety of
growth factors, such as platelet-derived growth factor (PDGF),
vascular endothelial growth factor (VEGF), transforming growth
factor (TGF) and insulin-like growth factor (IGF) (8,9).
Numerous techniques have been developed to make platelet
concentrates (8,10), and concentrated growth factor
(CGF) belongs to a new generation of platelet concentrates, which
was first introduced by Sacco (unpublished data). CGF, which is
generated by centrifuging venous blood, has a fibrin matrix that
contains a high concentration of platelets, leukocytes and growth
factors. CGF has been found to increase bone formation (11–13), the proliferation of periodontal
ligament cells (14), and the
syndesmosis union rate in cases of total ankle replacement
(15) depending on the released
growth factors. However, the effect of CGF on peripheral nerve
regeneration has not been investigated previously, to the best of
our knowledge.
Schwan cells (SCs) have been shown to play a
critical and substantial role in peripheral nerve regeneration.
Following peripheral nerve injury, SCs proliferate, form a Büngner
belt and devour the debris of denatured axons and myelin together
with macrophages. At the same time, SCs also secrete a range of
neurotrophic factors, including nerve growth factor (NGF) and glial
cell line-derived neurotrophic factor (GDNF), which play
neuron-protective and axon-inducive roles. It has previously been
suggested that the proliferation and increased secretory function
of Schwan cells contribute to the regeneration of neural tissue
(16–19).
The aims of the present study were as follows: i) to
investigate the effect of CGF on the proliferation and secretion of
neurotrophic factors in SCs in vitro; and ii) to evaluate
functional nerve recovery following CGF treatment using a rat model
of sciatic nerve crush injury in vivo. The final purpose of
this study was to examine the possibility of CGF being clinically
applied as a treatment for nerve injuries caused by dental implant
surgery.
Materials and methods
Preparation of CGF
All experiments were carried out in accordance with
the Guidance Suggestions for the Care and Use of Laboratory
Animals, formulated by the Ministry of Science and Technology of
China. CGF was prepared according to Sacco's protocol (unpublished
data). For the purposes of our study, a total of 46 Wistar rats
(10–12 weeks old, weighing 250 g) were purchased from the Center
for Laboratory Animals, Medical College, Jilin University, Jilin,
China. These rats (a different set of rats for each) was used for
the preparation of CGF and for the model of sciatic nerve crush
injury. In our study, 46 rats were used in total, among which 12
were used in the in vivo experiments and 34 were used to
prepare the CGF extract for the in vitro experiments. For
the in vivo experiments, 6 rats were used to draw blood to
prepare the CGF membrane and 6 were used for functional analysis.
We ensured that all rats had similar platelet counts by subjecting
the whole blood of the rats to platelet counting using a cell
counter (MEK-6318K, Nihon Kohden, Tokyo, Japan). The rats showed a
mean platelet count of 680×109/l. Briefly, for the
preparation of CGF, 5 ml venous blood was drawn from each Wistar
rat, into a sterile glass tube without any anticoagulant solution.
The tube was subsequently immediately centrifuged at 400 × g in
Medifuge (Silfradent, Sofia, Italy) at a fixed temperature, and the
rotor turned at alternating, controlled speeds. Following
centrifugation, the blood in the tube was separated into three
layers. CGF was the middle layer, and it was mechanically separated
and gently compressed into a thin membrane. All animal experiments
were approved by the Ethics Committee of Jilin University.
Scanning electron microscopy (SEM)
In the present study, the surface structure of CGF
was observed using an SEM microscope (S-3400N; Hitachi
High-Technologies America, Schaumburg, IL, USA). The CGF membrane
was fixed in 2.5% glutaraldehyde solution (Sigma-Aldrich) and
dehydrated by passing through a graded series of ethanol-water
mixtures. After drying, the sample was coated with gold, and
examined using SEM. The SEM images were subsequently exported to
cellSens Entry software (Olympus Life Science, Europe GMBH,
Hamburg, Germany), in order to measure the pore size of CGF based
on the smallest and largest identifiable pores in the
representative image.
Preparation of CGF extract
In order to minimize the difference between
different CGF membranes, the soluble component of CGF was used to
produce conditioned media to treat the SC cell line in culture. To
make the conditioned medium, two CGF membranes were placed in a
15-ml flacon tube containing 5 ml fresh Dulbecco's modified Eagle's
medium (DMEM; Gibco, Carlsbad, CA, USA) without fetal bovine serum.
The medium was marked as 200% CGF. It was collected 7 days later
and centrifuged (400 × g for 5 min) to pellet the platelets and red
blood cells. The 200% CGF was diluted to obtain 100 and 50% CGF.
All the extracts were stored at −80°C for future use.
Cell proliferation assay
The number of viable cells was evaluated by cell
counting kit-8 (CCK-8) assay. The RSC96 Schwann cell line, which
was obtained from The Chinese Academy of Sciences (Shanghai,
China), is a spontaneously transformed rat Schwann cell line
derived from the long-term culture of rat primary SCs. To test the
effect of CGF on cell proliferation, RSC96 SCs were seeded into
96-well plates at a density of 1,000 cells/well in DMEM, and
allowed to attach overnight in a humidified atmosphere at 37°C with
5% CO2. Subsequently, the culture medium was changed to
DMEM or CGF extracts supplemented with 10% FBS (Gibco, Sydney,
Australia). CGF extracts at different concentrations (200, 100 and
50%) were used in order to find the optimal concentration. At 1, 3
and 5 days following treatment, 10 µl CCK-8 reagent
(Dojindo, Kumamoto, Japan) was added to each well. After 1 h
incubation at 37°C, the absorbance values were measured at 450 nm
using a microplate reader (Infinite 200 Pro, Tecan, Männedorf,
Switzerland).
Cell cycle analysis
RSC96 Schwann cells were seeded in 6-well plates.
After pre-incubation, the culture medium was changed to DMEM or CGF
extract (100%) supplemented with 10% FBS. At 1, 2 and 3 days, cells
were detached from plate surfaces using 0.25% EDTA-free trypsin,
and fixed with 70% alcohol for 30 min at 4°C. Cells were then
washed twice with PBS, centrifuged, and labeled with 0.5 ml
propidium iodide (Dingguo, Beijing, China). Cells were then
incubated for 30 min in the dark at 4°C and detected by a flow
cytometer (BD Pharmingen, San Diego, CA, USA).
Reverse transcription-quantitative PCR
(RT-qPCR)
The mRNA expression of NGF and GDNF was analyzed by
RT-qPCR. RSC96 Schwann cells were seeded into 6-well plates, and
the culture medium was changed to DMEM or CGF extract (100%)
supplemented with 10% FBS. At 1, 2 and 3 days after culture, total
RNA was extracted using TRIzol reagent (Invitrogen, Carlsbad, CA,
USA) and was reverse transcribed using a Revert Aid kit according
to the manufacturer's instructions (Takara Bio, Otsu, Japan). SYBR
Premix Ex Taq (Takara Bio) was used to assess NGF and GDNF gene
expression in an Exicycler 96 real-time PCR system (Bioneer,
Daejeon, Korea). Samples were normalized to
glyceraldehyde-3-phosphate-dehydrogenase (GAPDH). Changes in gene
expression were calculated using the 2−ΔΔCt method. The
primer sequences were as follows: NGF forward, 5′-TCAACA
GGACTCACAGGAGCA-3′ and reverse, 5′-GGTCTTATC TCCAACCCACACAC-3′ ;
GDNF forward, 5′-CAGAGGGAA AGGTCGCAGAG-3′ and reverse,
5′-ATCAGTTCCTCCTTG GTTTCGTAG-3′; and GAPDH forward 5′-GGCACAGTC
AAGGCTGAGAATG-3′ and reverse, 5′-ATGGTGGTGAAG ACGCCAGTA-3′, as
previously reported (20).
Western blot analysis
The protein expression of NGF and GDNF was
investigated by western blot analysis. RSC96 Schwann cells were
seeded into 6-well plates, and culture medium was changed to DMEM
or CGF extract (100%) supplemented with 10% FBS. At days 1, 2 and
3, cells were washed twice using PBS, and then lysed on ice with
lysis solution [radioimmunoprecipitation assay buffer with 1%
phenylmethylsulfonyl fluoride (Biyuntian, Haimen, China)]. Cell
lysates were collected and centrifuged at 10,000 × g for 10 min at
4°C. Supernatants were collected, and protein concentrations were
determined using a bicinchoninic acid assay (BCA). The extracted
proteins were mixed with 5X loading buffer and degenerated in
boiling water for 5 min. Equal amounts of protein (40 µg)
were loaded onto a polyacrymide gel and run at 80 V for 150 min,
and were then transferred to polyvinylidene fluoride film
(Millipore, Bedford, MA, USA) at 70 V for 90 min. The membranes
were blocked with skimmed powdered milk for 90 min, and then
incubated with primer antibodies against NGF (rabbit anti-rat,
1:1,000, cat. no. WL0151; Wanleibio, Shenyang, China) and GDNF
(rabbit anti-rat, 1:400, cat. no. PB0045; Boster Biological
Technology, Ltd. (Wuhan, China) overnight at 4°C. Samples were
eluted four times with TTBS and then incubated with horseradish
peroxidase- conjugated secondary antibodies (goat anti-rabbit,
1:5,000, cat. no. A0208, Biyuntian) for 45 min at 37°C. An ECL
chemiluminescence assay was used for chemiluminescence-based
immunodetection of HRP. The intensities of the bands, which are
representative of protein levels, were determined using
Gel-Pro-Analyzer 3.0 (Media Cybernetics, Rockville, MD, USA).
β-actin was used to normalize target proteins.
Animals and surgical procedures
A rat model of sciatic nerve crush injury has been
previously used as a model of axonotmesis (21). Briefly, rats weighing 250 g were
anesthetized by injection of sodium pentobarbital (30 mg/kg).
Surgical sites were shaved and prepared. Both the left and the
right sciatic nerves were exposed. Subsequently, no. 5 jeweler's
forceps were applied to crush each nerve for 10 sec above the
bifurcation of the sciatic nerve. Both right and left nerves of
each rat were crushed, but only the right was treated with CGF
membrane (not CGF extract) and the left was used as a blank control
without CGF membrane. CGF was used only to cover the right sciatic
nerve crush sites. After surgery, the musculature and the skin were
sutured separately.
Functional analysis
Functional nerve recovery of the animals was
assessed through the use of a sciatic functional index (SFI),
according to the methods reported by Bain et al (22). Walking track analysis was
performed 7 days after the surgery. Briefly, the hind feet of the
rats were colored with ink before they walked, in order that they
would leave footprints on the paper. SFI was calculated using the
following formula: SFI = −38.3 × (EPL − NPL)/NPL + 109.5 × (ETS −
NTS)/ NTS + 13.3 × (EIT−NIT)/NIT − 8.8. In this formula, PL
indicates the length of the third toe to the heel; TS, the length
of the first to the fifth toe; PL, the length of the second to the
forth toe; E represented the CGF-treated side and N represented the
non-Walking track analysis treated side. Generally, a value of SFI
which was approximately −100 indicated total nerve impairment, and
0 indicated normal nerve function. Following functional analysis,
the rats were sacrificed by exsanguination via the abdominal
aorta.
Statistical analysis
Data are expressed as the means ± standard deviation
and were analyzed using one-way analysis of variance (ANOVA) with
Tukey's HSD comparison test or by independent-samples t-test. A
p-value <0.05 was considered to indicate a statistically
significant difference.
Results
Characteristics of CGF
Following centrifugation of the whole blood, three
layers were observed in the tube (Fig. 1A). The uppermost layer was a clear
fluid, which was the blood serum. This is composed of the blood
plasma without fibrinogen and coagulation factors. The middle layer
resembled a yellow non-transparent gel, which was CGF; this layer
was composed of the large, dense polymerized fibrin blocks with
aggregated platelets and CGFs. The bottom layer, which looked like
a dark reddish dense gel, mainly consisted of red blood cells. CGF
was mechanically separated by cutting off the red dense gel and
then compressing it into a thin membrane. SEM analysis (Fig. 1B) revealed that CGF had a
fiber-like appearance with a pore size ranging from 0.1 to 1.0
µm. The fibers were discrete and were arranged in a dense
random mesh-like network. An aggregate of platelets was also
observed to be trapped in the fibrin mesh.
Cell proliferation
The effects of CGF extracts on the proliferation of
RSC96 Schwann cells are shown in Fig.
2A. CGF was found to increase SC proliferation; this increase
was concentration-dependent up to 200%, when levels dropped. The
optical densities (indicative of the number of cells) of the
CGF-treated cells were significantly higher than those of the
DMEM-treated cells at 1, 3 and 5 days (p<0.05). In particular,
the cells treated with 100% CGF group but not 200% produced the
highest optical densities of all (p<0.05) at different time
points. Therefore, 100% CGF was selected as the optimal
concentration for later experiments.
Cell cycle analysis
Flow cytometry was used to study cell cycle
distribution by measuring DNA content. Cell cycle refers to the
period from the end of mitosis to the formation of new cells, which
includes four stages, namely G1, S, G2 and M phases. The cell
proliferation index (PI) is the percentage of cells in the S plus
G2/M phases. It is one of the most important indexes for cell
proliferation. We noted that at 1, 2 and 3 days after CGF treatment
the PI in CGF-treated cells was significantly higher than those
treated with the control (p<0.05) (Fig. 2B).
mRNA expression
RT-qPCR was performed to detect mRNA expression of
RSC96 Schwann cells, which were treated with DMEM or CGF extract.
There was no significant difference in NGF and GDNF mRNA expression
in the DMEM-treated cells at different time points. The mRNA
expression of NGF and GDNF in the CGF-treated cells was
significantly higher than those treated with DMEM (p<0.05)
(Fig. 3).
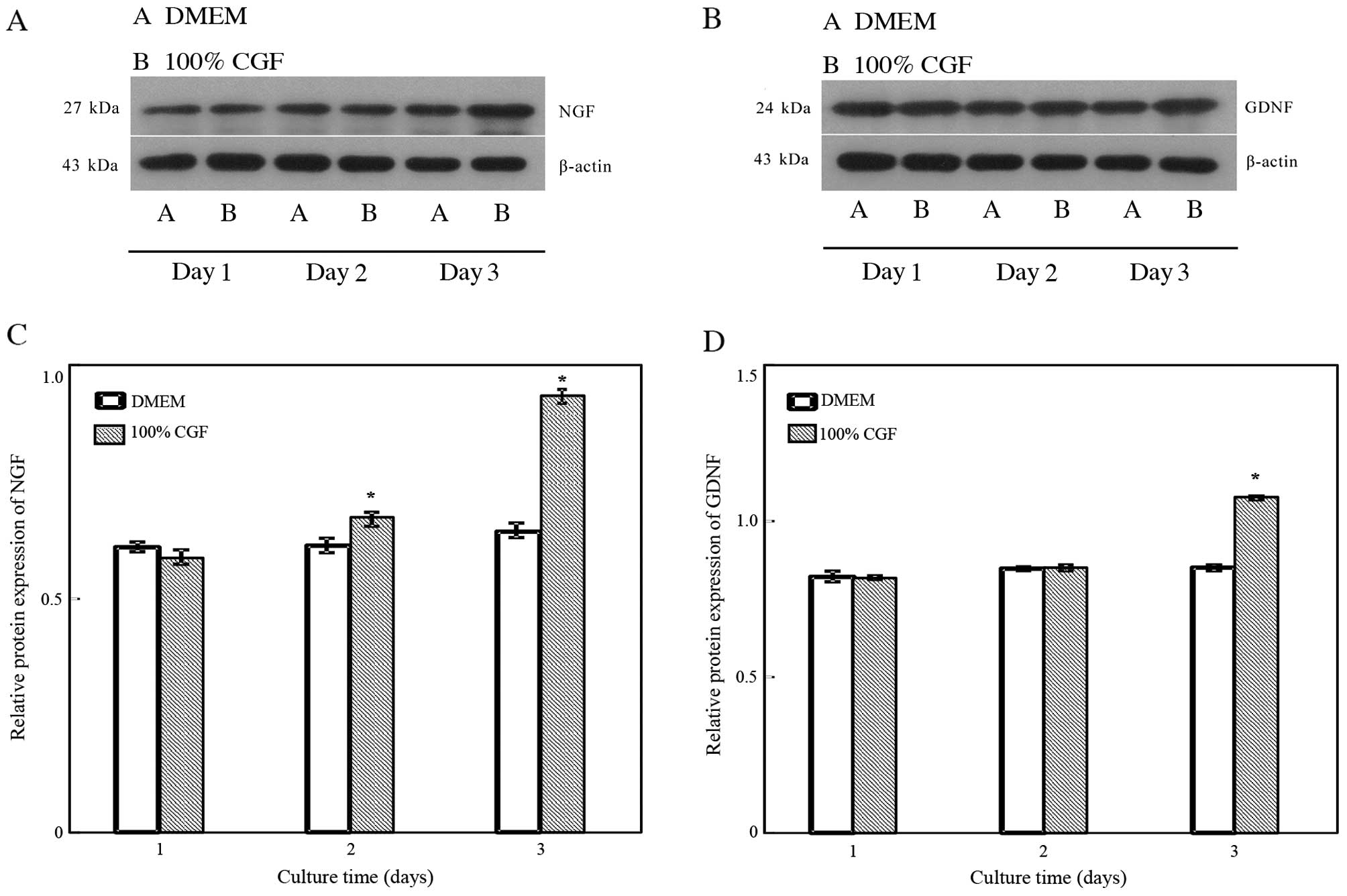
Protein expression
The effects of CGF extract on neurotrophic protein
secretion in RSC96 Schwann cell are illustrated in Fig. 4. NGF protein expression
significantly (p<0.05) increased on days 2 and 3; GDNF protein
expression significantly (p<0.05) increased on day 3. The levels
of NGF protein expression increased approximately 1.1-fold on day 2
and 1.5-fold on day 3. Levels of GDNF protein expression increased
approximately 1.3-fold on day 3.
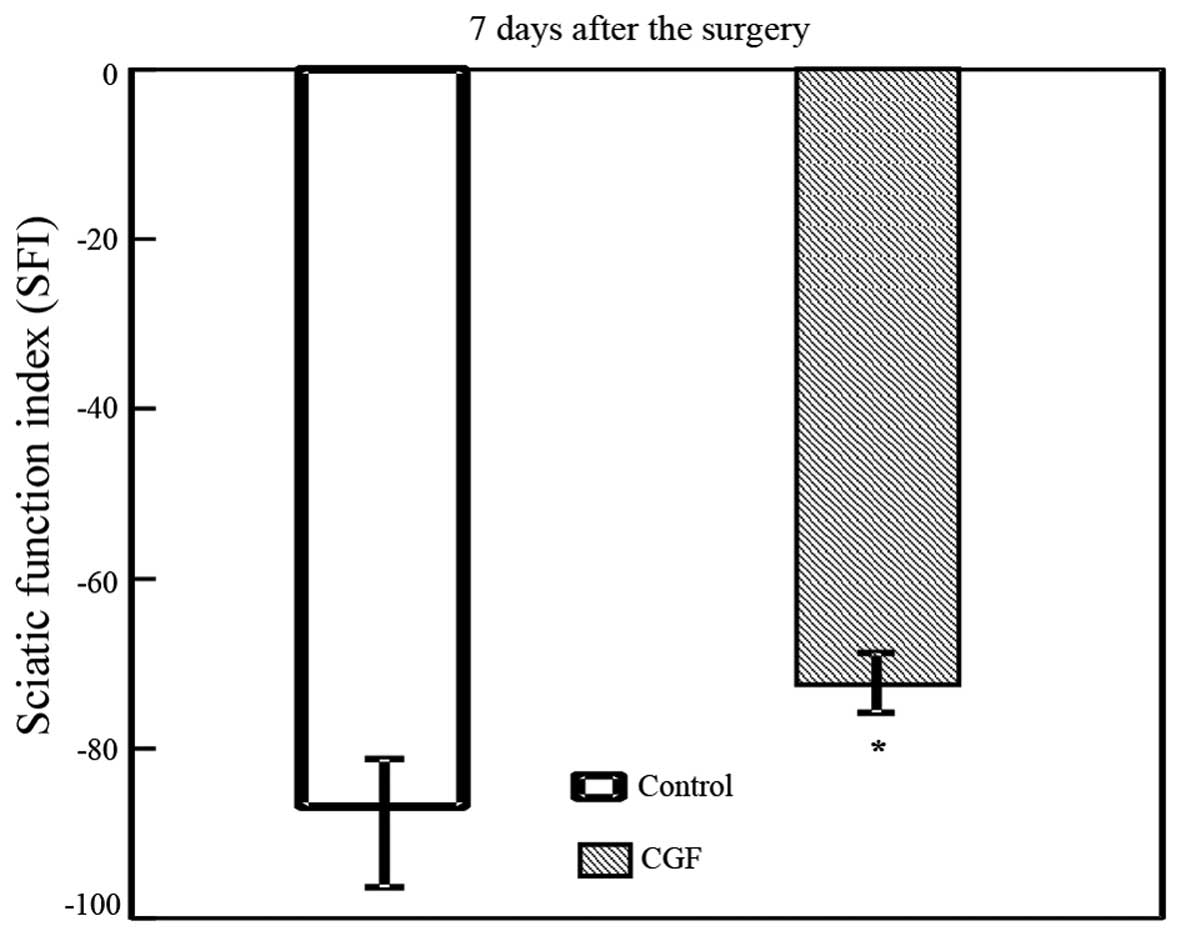
Functional recovery
The results of the functional nerve recovery test
using the walking track indicated different degrees of nerve injury
in rats 7 days after the surgery, as reflected by different SFIs.
The SFI value was significantly increased in the CGF-treated side
compared with the non-treated side (p<0.05), indicating improved
functional nerve recovery in the CGF-treated group (Fig. 5).
Discussion
Nerve injury has previously been shown to be one of
the most serious complications of dental implant surgery. Moreover,
local delivery of growth factors has proven effective in the
treatment of nerve injury. CGF is rich in growth factors and has
gained considerable popularity owing to its autologous nature, easy
collection, simple and cost-effective preparation, and safe
clinical application, without the risks associated with
immunological rejection. In the present study, we demonstrated that
CGF promoted SC proliferation and the secretion of neurotrophic
factors in vitro, and enhanced functional nerve recovery
after injury in vivo, suggesting that CGF provides a way to
regenerate iatrogenic nerve injuries caused by dental implants.
In the present study, an RSC96 Schwann cell line was
selected and subsequently subjected to CGF treatment. Since the
RSC96 Schwann cell line was derived from rats, therefore rat venous
blood was used to prepare CGFs in this experiment. The inferior
vena cava was used to obtain 5 ml of blood from each rat, as it is
possible to obtain more blood from here, as compared to other
locations such as rat tail veins, which provide limited and
insufficient (23) amounts of
blood for making CGF. Reproducibility of the experiment was ensured
by the following, as Li et al have also reported (24): i) CGF was prepared under
consistent preparation conditions, including using a specially
programmed centrifuge with fixed temperature and control speed; ii)
all blood-collecting procedures were finished within 90 sec; iii)
the rats used in the experiment were of similar weight and platelet
counts; and iv) mixed CGF extracts were used instead of CGF
membranes to treat the SCs.
The structure of the fibrin mesh and concentration
of leukocytes are known to affect the release of growth factors
from platelet concentrates (25,26). CGF belongs to the third generation
of platelet concentrate; platelet-rich plasma (PRP) was the first
generation, and platelet-rich fibrin (PRF) the second generation
(27). It has been shown that PRP
formed an unstable matrix that disaggregated after less than 5 days
and led to a quick release of growth factors. PRF, formed by
progressive polymerization, had a more structured fibrin network
that was shown to be intact after 7 days and led to greater growth
factor release. Moreover, SEM analysis demonstrated that CGF had a
natural fibrin framework and many platelets were trapped in this
fibrin mesh, similar to PRF (28). This kind of structure protects
growth factors from proteolysis, and results in lower and sustained
release of growth factors from the fibrin concentrates (29).
CGF membranes were soaked in medium for 7 days to
obtain the extracts used in this study. This time period was
applied based on certain previous studies which have investigated
the release dynamics of growth factors in platelet concentrates
(25,30,31). The release of VEGF and TGF-β1
peaked at 8 h in PRP and at day 7 in PRF. IGF-1 and PDGF were
almost completely released from PRF within the first 8 h and
gradually released from PRF for the first 3 days. These findings
suggest that day 7 is a suitable time point for collecting the
majority of growth factors released from platelet concentrates
(25,30,31).
The fast proliferation of Schwann cells supports the
rapid regeneration of injured peripheral nerves by providing
bioactive substrates needed for axonal outgrowth (32). In this study, both a CCK-8 assay
and cell cycle analysis indicated that CGF promoted RSC96 Schwann
cell proliferation. Similar results have previously been reported,
that CGF stimulated the proliferation of periodontal ligament stem
cells (14) and bone marrow
stromal cells (BMSCs) (33). In
the present study, although the effect of CGF on cell proliferation
was noted to be dose-dependent, the increasing CGF concentration
did not always cause increasing proliferation. We noted that the
optimal concentration of CGF extract (100%) had the most beneficial
effect on RSC96 Schwann cells. Both increased and decreased
concentrations exerted a suboptimal effect on cell proliferation.
This is in line with the conclusions of Graziani et al
(34), who investigated the
effect of different platelet concentrations on osteoblasts and
fibroblasts. They made maximally concentrated platelet preparations
of 420–550% which were diluted with DMEM to attain concentrations
of 250 and 100%. They found that maximal platelet concentration
resulted in inferior proliferation compared with concentrations of
250 and 100%. Liu et al have suggested that decreased
proliferation is pH dependent: high concentrations of platelet
preparations result in pH changes that negatively affect
proliferation (35).
Aside from proliferation, in the present study we
also examined RSC96 Schwann cell function by assessing their
secretion of NGF and GDNF. NGF plays a critical role in nerve
regeneration in the peripheral nerve system. A reduction in the
secretion of NGF results in the failure of axonal regeneration
(36). GDNF belongs to the TGF-β
family of neurotrophic factors and plays various and distinct roles
in the neuronal signaling pathways (37). In our present study, both the mRNA
and protein expression levels of NGF and GDNF were increased by
CGF. Similar results have been previously reported, that NGF and
GDNF expression was promoted by platelet concentrates (20). The mechanisms responsible for this
can be explained as follows. Many growth factors such as IGF, TGF
and PDGF are released from CGF. It has previously been shown that
Schwann cells express growth factor receptors, such as the IGF
receptor, TGF-β receptor and platelet-derived growth factor
receptor (38–40). These findings suggest that CGF
modulates SC secretion through IGF-related, TGF-related and
PDGF-related pathways.
In the present study, we noted that CGF served to
improve functional nerve recovery in a rat model of sciatic nerve
crush injury. This is consistent with reports that platelet
concentrates increased nerve regeneration after injury to the
facial (41) and sciatic nerve
(42) in animal models. These
results suggest that CGF works in vivo, thus supporting the
clinical use of CGF to treat nerve injuries caused by dental
implants. Compared with PRP and PRF, CGF contains more growth
factors, and we suggest that it helps the nerves recover in a
shorter period of time.
CGF is an autogenously generated complex that
contains fibrin matrix and growth factors; it is used in dentistry
for bone regeneration. In the present study we demonstrated the
following: i) CGF increased SC proliferation and secretion of
neurotrophic factors in vitro; and ii) CGF enhanced
functional nerve recovery in an animal model. These findings
suggest that CGF has the potential to enhance peripheral nerve
regeneration, and thus is a promising treatment for nerve injury
caused by dental implant surgery. Further study is required to
elucidate the dominant growth factor-related pathway by which CGF
modulates cell proliferation and secretion. Neurophysiological
experiments should also be evaluated in vivo in order to
investigate the effect of CGF on nerve repair.
Acknowledgments
Financial support from the Funding for Top Talents
among PhD students in Jilin University, the National Natural
Science Foundation of China (Youth Scholar program, grant no.
81400487), Jilin Province Science Foundation for Youths (grant no.
20150520043JH) and the Excellent Youth Scholars of Bethune Medical
Department in Jilin University (grant no. 2013208064) is gratefully
acknowledged.
References
|
1
|
Misch K and Wang HL: Implant surgery
complications: etiology and treatment. Implant Dent. 17:159–168.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Juodzbalys G, Wang HL, Sabalys G,
Sidlauskas A and Galindo-Moreno P: Inferior alveolar nerve injury
associated with implant surgery. Clin Oral Implants Res.
24:183–190. 2013. View Article : Google Scholar
|
|
3
|
Alhassani AA and AlGhamdi AS: Inferior
alveolar nerve injury in implant dentistry: diagnosis, causes,
prevention, and management. J Oral Implantol. 36:401–407. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim YT, Pang KM, Jung HJ, Kim SM, Kim MJ
and Lee JH: Clinical outcome of conservative treatment of injured
inferior alveolar nerve during dental implant placement. J Korean
Assoc Oral Maxillofac Surg. 39:127–133. 2013. View Article : Google Scholar
|
|
5
|
Fukuda K, Ichinohe T and Kaneko Y: Pain
management for nerve injury following dental implant surgery at
Tokyo Dental College Hospital. Int J Dent. 2012:2094742012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee JY, Jahng JW, Kim SM, Kim MJ and Lee
JH: Simultaneous inferior alveolar nerve regeneration and
osseointegration with a nerve growth factor-supplying implant: a
preliminary study. J Oral Maxillofac Surg. 73:410–423. 2015.
View Article : Google Scholar
|
|
7
|
Lee JY, Kim SM, Kim MJ and Lee JH:
Controlled release of nerve growth factor from heparin-conjugated
fibrin gel within the nerve growth factor-delivering implant. J
Korean Assoc Oral Maxillofac Surg. 40:3–10. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Choukroun J, Diss A, Simonpieri A, Girard
MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J and Dohan DM:
Platelet-rich fibrin (PRF): a second-generation platelet
concentrate. Part IV: clinical effects on tissue healing. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 101:e56–e60. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Intini G: The use of platelet-rich plasma
in bone reconstruction therapy. Biomaterials. 30:4956–4966. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Marx RE, Carlson ER, Eichstaedt RM,
Schimmele SR, Strauss JE and Georgeff KR: Platelet-rich plasma:
growth factor enhancement for bone grafts. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 85:638–646. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kim TH, Kim SH, Sándor GK and Kim YD:
Comparison of platelet-rich plasma (PRP), platelet-rich fibrin
(PRF), and concentrated growth factor (CGF) in rabbit-skull defect
healing. Arch Oral Biol. 59:550–558. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim JM, Sohn DS, Bae MS, Moon JW, Lee JH
and Park IS: Flapless transcrestal sinus augmentation using
hydrodynamic piezoelectric internal sinus elevation with autologous
concentrated growth factors alone. Implant Dent. 23:168–174. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sohn DS, Heo JU, Kwak DH, Kim DE, Kim JM,
Moon JW, Lee JH and Park IS: Bone regeneration in the maxillary
sinus using an autologous fibrin-rich block with concentrated
growth factors alone. Implant Dent. 20:389–395. 2011.PubMed/NCBI
|
|
14
|
Yu B and Wang Z: Effect of concentrated
growth factors on beagle periodontal ligament stem cells in vitro.
Mol Med Rep. 9:235–242. 2014.
|
|
15
|
Coetzee JC, Pomeroy GC, Watts JD and
Barrow C: The use of autologous concentrated growth factors to
promote syndesmosis fusion in the agility total ankle replacement.
A preliminary study. Foot Ankle Int. 26:840–846. 2005.PubMed/NCBI
|
|
16
|
Wakatsuki S, Araki T and Sehara-Fujisawa
A: Neuregulin-1/glial growth factor stimulates Schwann cell
migration by inducing α5 β1 integrin-ErbB2-focal adhesion kinase
complex formation. Genes Cells. 19:66–77. 2014. View Article : Google Scholar
|
|
17
|
Yazdani SO, Golestaneh AF, Shafiee A,
Hafizi M, Omrani HA and Soleimani M: Effects of low level laser
therapy on proliferation and neurotrophic factor gene expression of
human schwann cells in vitro. J Photochem Photobiol B. 107:9–13.
2012. View Article : Google Scholar
|
|
18
|
Luo L, Gan L, Liu Y, Tian W, Tong Z, Wang
X, Huselstein C and Chen Y: Construction of nerve guide conduits
from cellulose/soy protein composite membranes combined with
Schwann cells and pyrroloquinoline quinone for the repair of
peripheral nerve defect. Biochem Biophys Res Commun. 457:507–513.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jiang M, Cheng Q, Su W, Wang C, Yang Y,
Cao Z and Ding F: The beneficial effect of chitooligosaccharides on
cell behavior and function of primary Schwann cells is accompanied
by up-regulation of adhesion proteins and neurotrophins. Neurochem
Res. 39:2047–2057. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zheng C, Zhu Q, Liu X, Huang X, He C,
Jiang L, Quan D, Zhou X and Zhu Z: Effect of platelet-rich plasma
(PRP) concentration on proliferation, neurotrophic function and
migration of Schwann cells in vitro. J Tissue Eng Regen Med. May
31–2013.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bridge PM, Ball DJ, Mackinnon SE, Nakao Y,
Brandt K, Hunter DA and Hertl C: Nerve crush injuries - a model for
axonotmesis. Exp Neurol. 127:284–290. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bain JR, Mackinnon SE and Hunter DA:
Functional evaluation of complete sciatic, peroneal, and posterior
tibial nerve lesions in the rat. Plast Reconstr Surg. 83:129–138.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Diehl KH, Hull R, Morton D, Pfister R,
Rabemampianina Y, Smith D, Vidal JM and van de Vorstenbosch C;
European Federation of Pharmaceutical Industries Association and
Europ ean Centre for the Validation of Alternative Methods: A good
practice guide to the administration of substances and removal of
blood, including routes and volumes. J Appl Toxicol. 21:15–23.
2001. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li Q, Pan S, Dangaria SJ, Gopinathan G,
Kolokythas A, Chu S, Geng Y, Zhou Y and Luan X: Platelet-rich
fibrin promotes periodontal regeneration and enhances alveolar bone
augmentation. BioMed Res Int. 2013:6380432013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Schär MO, Diaz-Romero J, Kohl S, Zumstein
MA and Nesic D: Platelet-rich concentrates differentially release
growth factors and induce cell migration in vitro. Clin Orthop
Relat Res. 473:1635–1643. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dohan Ehrenfest DM, Bielecki T, Jimbo R,
Barbé G, Del Corso M, Inchingolo F and Sammartino G: Do the fibrin
architecture and leukocyte content influence the growth factor
release of platelet concentrates? An evidence-based answer
comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte-
and platelet-rich fibrin (L-PRF). Curr Pharm Biotechnol.
13:1145–1152. 2012. View Article : Google Scholar
|
|
27
|
Rodella LF, Favero G, Boninsegna R,
Buffoli B, Labanca M, Scarì G, Sacco L, Batani T and Rezzani R:
Growth factors, CD34 positive cells, and fibrin network analysis in
concentrated growth factors fraction. Microsc Res Tech. 74:772–777.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li Q, Reed DA, Min L, Gopinathan G, Li S,
Dangaria SJ, Li L, Geng Y, Galang MT, Gajendrareddy P, et al:
Lyophilized platelet-rich fibrin (PRF) promotes craniofacial bone
regeneration through Runx2. Int J Mol Sci. 15:8509–8525. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lundquist R, Dziegiel MH and Agren MS:
Bioactivity and stability of endogenous fibrogenic factors in
platelet-rich fibrin. Wound Repair Regen. 16:356–363. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zumstein MA, Berger S, Schober M, Boileau
P, Nyffeler RW, Horn M and Dahinden CA: Leukocyte- and
platelet-rich fibrin (L-PRF) for long-term delivery of growth
factor in rotator cuff repair: review, preliminary results and
future directions. Curr Pharm Biotechnol. 13:1196–1206. 2012.
View Article : Google Scholar
|
|
31
|
Dohan Ehrenfest DM, de Peppo GM, Doglioli
P and Sammartino G: Slow release of growth factors and
thrombospondin-1 in Choukroun's platelet-rich fibrin (PRF): a gold
standard to achieve for all surgical platelet concentrates
technologies. Growth Factors. 27:63–69. 2009. View Article : Google Scholar
|
|
32
|
Liang W, Ge S, Yang L, Yang M, Ye Z, Yan
M, Du J and Luo Z: Ginsenosides Rb1 and Rg1 promote proliferation
and expression of neurotrophic factors in primary Schwann cell
cultures. Brain Res. 1357:19–25. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Honda H, Tamai N, Naka N, Yoshikawa H and
Myoui A: Bone tissue engineering with bone marrow-derived stromal
cells integrated with concentrated growth factor in Rattus
norvegicus calvaria defect model. J Artif Organs. 16:305–315. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Graziani F, Ivanovski S, Cei S, Ducci F,
Tonetti M and Gabriele M: The in vitro effect of different PRP
concentrations on osteoblasts and fibroblasts. Clin Oral Implants
Res. 17:212–219. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liu Y1, Kalén A, Risto O and Wahlström O:
Fibroblast proliferation due to exposure to a platelet concentrate
in vitro is pH dependent. Wound Repair Regen. 10:336–340. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhou YK, Liang Z, Guo Y, Zhang HT and Wang
KH: High glucose upregulates CYP24A1 expression which attenuates
the ability of 1,25(OH)2D3 to increase NGF
secretion in a rat Schwann cell line RSC96. Mol Cell Endocrinol.
404:75–81. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Shakhbazau A, Mohanty C, Shcharbin D,
Bryszewska M, Caminade AM, Majoral JP, Alant J and Midha R:
Doxycycline- regulated GDNF expression promotes axonal regeneration
and functional recovery in transected peripheral nerve. J Control
Release. 172:841–851. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Cheng HL, Shy M and Feldman EL: Regulation
of insulin-like growth factor-binding protein-5 expression during
Schwann cell differentiation. Endocrinology. 140:4478–4485.
1999.PubMed/NCBI
|
|
39
|
D'Antonio M, Droggiti A, Feltri ML, Roes
J, Wrabetz L, Mirsky R and Jessen KR: TGFbeta type II receptor
signaling controls Schwann cell death and proliferation in
developing nerves. J Neurosci. 26:8417–8427. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Badache A and De Vries GH:
Neurofibrosarcoma-derived Schwann cells overexpress
platelet-derived growth factor (PDGF) receptors and are induced to
proliferate by PDGF BB. J Cell Physiol. 177:334–342. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Cho HH, Jang S, Lee SC, Jeong HS, Park JS,
Han JY, Lee KH and Cho YB: Effect of neural-induced mesenchymal
stem cells and platelet-rich plasma on facial nerve regeneration in
an acute nerve injury model. Laryngoscope. 120:907–913.
2010.PubMed/NCBI
|
|
42
|
Lichtenfels M, Colomé L, Sebben AD and
Braga-Silva J: Effect of platelet rich plasma and platelet rich
fibrin on sciatic nerve regeneration in a rat model. Microsurgery.
33:383–390. 2013. View Article : Google Scholar : PubMed/NCBI
|