Introduction
Bone metabolism is rigorously controlled by two
different functional cell types-osteoblasts and osteoclasts
(1,2). Osteoblasts are responsible for bone
formation and osteoclasts for bone resorption. Bone tissue
continues to regenerate in a process known as ‘bone remodeling’.
The process of bone remodeling starts with osteoclastic bone
resorption and osteoblasts subsequently migrate to the sites
resorbed by osteoclasts, resulting in the stimulation of bone
formation. The orchestrated coupling of osteoblasts and osteoclasts
maintains the appropriate bone mass. Metabolic bone diseases,
including osteoporosis, are caused by the impairment of bone
remodeling. Accumulating evidence indicates that osteoblast
migration is pivotal for numerous processes in physiological bone
metabolism, including responses to mechanical loading (1,3,4).
In addition, it has been indicated that osteoblast migration is
essential for processes associated with pathological conditions of
the bone, including tumor metastasis and the repair of bone
fracture (5). It is widely
recognized that various humoral factors, including epidermal growth
factor (EGF), have important roles in bone metabolism (3,4,6).
As for the effects of EGF on osteoblasts, EGF reportedly stimulates
their proliferation but suppresses their differentiation (7–10).
In addition, it has been indicated that EGF enhances osteoblast
migration (11). The migration of
mesenchymal progenitors was reported to be mediated via
phosphatidylinositol-3 kinase (PI3K)/Akt and p38 mitogen-activated
protein kinase (MAPK) through the EGF receptor, which is activated
by an EGF ligand released from osteoblasts (12). Regarding the intracellular
signaling associated with the EGF-induced migration of osteoblasts,
a recent study by our group suggested that p44/p42 MAPK, p38 MAPK,
stress-activated protein kinase (SAPK)/c-Jun N-terminal kinase
(JNK) and Akt function as positive regulators in osteoblast-like
MC3T3-E1 cells (13).
It is generally established that natural polyphenols
contained in beverages and foods are beneficial for human health
through exerting anti-oxidative, anti-inflammatory and anti-tumor
effects (14,15). Regarding the effects of natural
polyphenolic compounds, several epidemiological studies indicate
that chlorogenic acid, a major phenolic compound in coffee, and
(−)-epigallocatechin gallate (EGCG), a major polyphenol in green
tea, has beneficial properties on human health (16–18). As for the potential benefit on
bone tissue, it is known that green tea consumption in elderly
individuals leads to an increase of bone mass, improves the bone
mineral density and decreases the risk of fracture (19). Chlorogenic acid has been reported
to cause an increase of mineralization in rat tibia and improves
the mechanical properties of the femoral diaphysis (20). In addition, it has been indicated
that chlorogenic acid suppresses osteoclastic bone resorption due
to downregulation of receptor activator of nuclear factor-κB-ligand
and its downstream effects (21).
However, EGCG was reported to promote osteoblastic bone formation
and inhibit osteoclastic bone resorption (19,22). However, the mechanisms underlying
the effects of chlorogenic acid or EGCG on bone metabolism remain
to be clarified.
In the present study, it was investigated whether
chlorogenic acid or EGCG affect the EGF induced-migration of
osteoblast-like MC3T3-E1 cells. It was demonstrated that not
chlorogenic acid but EGCG reduces the EGF-induced migration of
osteoblasts through the suppression of p38 MAPK.
Materials and methods
Materials
Chlorogenic acid and EGCG were obtained from
Sigma-Aldrich (Merck KGaA, Darmstadt, Germany). EGF was purchased
from R&D Systems, Inc. (Minneapolis, MN, USA). Antibodies to
phosphorylated p38 MAPK (cat. no. 4511), p38 MAPK (cat. no. 9212),
phosphorylated p44/p42 MAPK (cat. no. 9101), p44/p42 MAPK (cat. no.
9102), phosphorylated SAPK/JNK (cat. no. 9251), SAPK/JNK (cat. no.
9252), phosphorylated Akt (cat. no. 9275) and Akt (cat. no. 9272)
were purchased from Cell Signaling Technology, Inc. (Beverly, MA,
USA). GAPDH antibodies (cat. no. sc-25778) were obtained from Santa
Cruz Biotechnology, Inc. (Dallas, TX, USA). An ECL Western blotting
detection system (cat. no. RPN2108) was obtained from GE Healthcare
UK Ltd. (Little Chalfont, UK). Chlorogenic acid was dissolved in
ethanol and EGCG was dissolved in dimethyl sulfoxide to prepare
stock solutions. The maximum concentration of dimethyl sulfoxide or
ethanol during incubations was 0.1%, which did not affect the cell
migration assay or the western blot analysis.
Cell culture
Cloned osteoblast-like MC3T3-E1 cells that have been
derived from newborn mouse calvaria (23) were provided by Dr Masayoshi
Kumegawa (Meikai University, Sakado, Japan), and maintained as
previously described (24). In
brief, the cells were cultured in α-minimum essential medium
(α-MEM) obtained from Sigma-Aldrich (Merck KGaA) containing 10%
fetal bovine serum (FBS) obtained from Gibco (Thermo Fisher
Scientific, Inc., Waltham, MA, USA) at 37°C in a humidified
atmosphere of 5% CO2/95% air. The cells were seeded into
90-mm diameter dishes (2×105 cells/dish) in α-MEM
containing 10% FBS. After 5 days, the medium was replaced with
α-MEM containing 0.3% FBS. After 48 h, the cells were subjected to
western blot analysis initiated by the EGCG pretreatment. For the
cell migration assay, the cells cultured in α-MEM containing 10%
FBS for 3 days were sub-cultured in α-MEM containing 0.3% FBS for 6
h, and were then used for the experiments.
Cell migration assay
A Transwell cell migration assay was performed as
described previously (25) using
Boyden chambers (polycarbonate membrane with 8-µm pores;
Transwell®; Corning Costar Corp., Cambridge, MA, USA).
In brief, the cultured cells were trypsinized and seeded onto the
upper chamber at 1×105 cells/well in α-MEM containing
0.3% FBS. EGF (10 ng/ml) was added to the lower chamber in α-MEM
containing 0.3% FBS and the cells were incubated for 16 h at 37°C.
Subsequently, the cells on the upper surface of the membrane were
mechanically removed. The migrated cells adherent to the lower side
of the membrane were fixed with 4% paraformaldehyde for 10 min at
room temperature, and stained with 1:1,000 of DAPI solution (Wako
Pure Chemical Industries, Ltd., Osaka, Japan) with 0.1% bovine
serum albumin in phosphate buffered saline for 10 min at room
temperature. Images of the migrated cells were captured under the
fluorescent microscope (BZ-9000; Keyence Co., Ltd., Tokyo, Japan)
at a magnification of ×20 and the cells were quantified by counting
the stained cells in three randomly chosen fields. When indicated,
the cells were pre-treated with chlorogenic acid or EGCG for 60 min
at 37°C.
For the wound-healing assay, the cultured cells were
seeded at 1×105 cells/well into an Ibidi Culture-Insert
2 Well (Ibidi, Martinsried, Germany) with a 500-µm margin
from the side of the well and allowed to grow for 24 h. After the
culture insert had been removed, the cells were stimulated with 30
ng/ml EGF for 8 h. Images of the cells were captured using an EOS
Kiss X4 digital camera (Canon, Tokyo, Japan) connected to a CK40
culture microscope (Olympus Optical Co. Ltd., Tokyo, Japan) prior
to EGF stimulation and after 8 h. The area into which the cells
migrated was measured using ImageJ software (version 1.48; National
Institutes of Health, Bethesda, MD, USA).
Western blot analysis
The cultured cells were pre-treated with various
doses of EGCG for 60 min and then stimulated with either 50 ng/ml
EGF or vehicle in 1 ml α-MEM containing 0.3% FBS for the indicated
durations. The cells were then lysed, homogenized and sonicated in
a lysis buffer containing 62.5 mM Tris/HCl, pH 6.8, 2% SDS, 50 mM
dithiothreitol and 10% glycerol. SDS-PAGE was performed by the
method of Laemmli (26) in 10%
polyacrylamide gels. The protein was fractionated and transferred
onto an Immun-Blot polyvinylidene difluoride membrane (Bio-Rad
Laboratories, Hercules, CA, USA). The membranes were blocked with
5% fat-free dry milk in Tris-buffered saline-Tween-20 (TBS-T; 20 mM
Tris/HCl, pH 7.6, 137 mM NaCl, 0.1% Tween 20) for 1 h prior to
incubation with the primary antibodies. Western blot analysis was
performed as described previously (27) using antibodies to phosphorylated
p38 MAPK, p38 MAPK, phosphorylated p44/p42 MAPK, p44/p42 MAPK,
phosphorylated SAPK/JNK, SAPK/JNK, phosphorylated Akt, Akt and
GAPDH as primary antibodies and peroxidase-labeled antibodies
raised in goat against rabbit immunoglobulin G (cat. no. 5110-0336;
KPL Inc., Gaithersburg, MD, USA) as secondary antibodies. The
primary and secondary antibodies were diluted at 1:1,000 with 5%
fat-free dry milk in TBS-T, and incubated for 24 h at 4 °C and for
60 min at room temperature, respectively. The peroxidase activity
on the polyvinylidene difluoride sheet was visualized by means of
the ECL western blotting detection system and images were captured
on X-ray film (Fujifilm, Tokyo, Japan). Densitometric analysis was
performed using a scanner and image analysis software (ImageJ
version 1.48). The phosphorylated protein levels were calculated as
follows: The background-subtracted signal intensity of each
phosphorylation signal was respectively normalized to the total
protein signal and plotted as the fold increase in comparison to
that of the control cells treated without stimulation.
Statistical analysis
The data were analyzed by analysis of variance
followed by Bonferroni’s method for multiple comparisons between
pairs. P<0.05 was considered to indicate a statistically
significant difference. Microsoft Excel 2010 ver. 14.0 (Microsoft
Corporation, Redmond, WA, USA) was used for the analysis. Values
are expressed as the mean ± standard error of the mean of
triplicate determinations from three independent cell
preparations.
Results
EGCG attenuates the EGF-induced migration
of MC3T3-E1 cells
A recent study by our group has demonstrated that
resveratrol suppresses the EGF-induced migration of osteoblast-like
MC3T3-E1 cells by using a Transwell cell migration assay (13). In the present study, the effect of
chlorogenic acid on EGF-induced migration in MC3T3-E1 cells was
examined. However, chlorogenic acid at concentrations of up to 50
µM did not affect the EGF-induced migration in the Transwell
cell migration assay (Fig.
1).
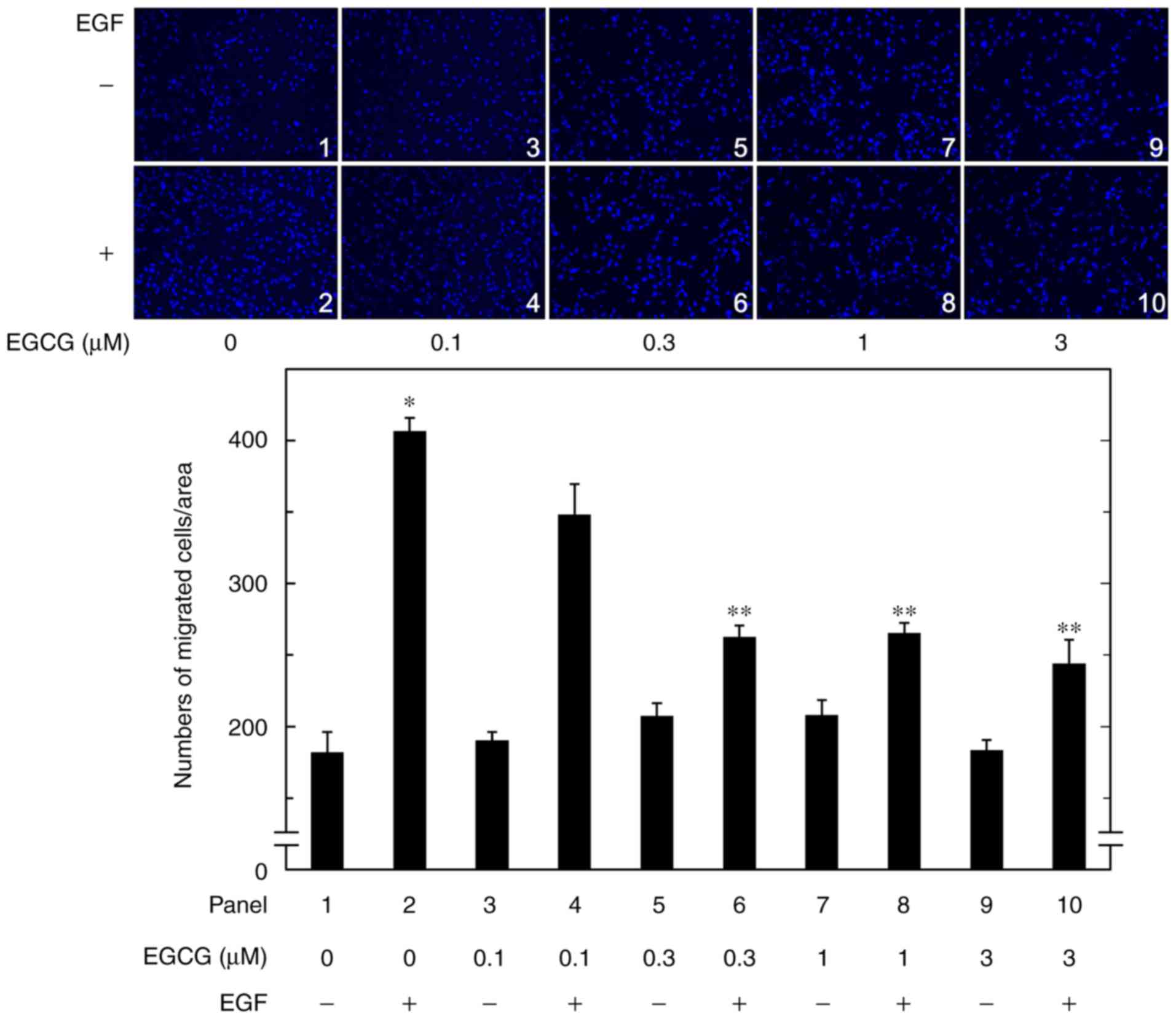
Next, the effect of EGCG on the EGF-induced
migration of MC3T3-E1 cells was examined. EGCG, which had little
effect on the cell migration in the absence of EGF, significantly
reduced the EGF-induced migration in the Transwell cell migration
assay (Fig. 2). The suppressive
effect of EGCG on the cell migration was dose-dependent over the
concentration range of 0.3–3.0 µM. In addition, the
wound-healing assay confirmed that the EGF-induced migration of
osteoblast-like MC3T3-E1 cells was markedly attenuated by EGCG at 3
µM (Fig. 3).
Effects of EGCG on the EGF-induced
phosphorylation of p44/p42 MAPK, p38 MAPK, SAPK/JNK and Akt in
MC3T3-E1 cells
A previous study by our group has demonstrated that
the EGF-induced migration of osteoblast-like MC3T3-E1 cells
proceeds via phosphorylation of p44/p42 MAPK, p38 MAPK, SAPK/JNK
and Akt (13). In order to
elucidate how EGCG suppresses the EGF-induced migration of
osteoblast-like MC3T3-E1 cells, the effects of EGCG on the
EGF-stimulated phosphorylation of p44/p42 MAPK, p38 MAPK, SAPK/JNK
and Akt were examined. EGCG significantly attenuated the
EGF-induced phosphorylation of p38 MAPK in MC3T3-E1 cells (Fig. 4). However, EGCG failed to affect
the phosphorylation of p44/p42 MAPK, SAPK/JNK and Akt in these
cells (Figs. 5Figure 6–7).
Discussion
In the present study, it was demonstrated that EGCG,
a major constituent of green tea catechins, significantly
suppressed EGF-stimulated migration of osteoblast-like MC3T3-E1
cells. The inhibitory effect of EGCG on the cell migration was
significant even at 0.3 µM. Since it has been indicated that
the plasma concentration of EGCG in humans reaches 0.1–0.3
µM after moderate green tea consumption (28), it is probable that the effect of
EGCG on osteoblast migration is physiologically relevant for green
tea drinkers. However, chlorogenic acid, a major polyphenol in
coffee, had no effect on the EGF-stimulated cell migration in the
present study. Next, the exact mechanism underlying the inhibition
of EGF-stimulated osteoblast-like MC3T3-E1 cell migration by EGCG
was investigated. With regard to the intracellular signaling of EGF
in osteoblasts, it has been reported that parathyroid hormone
stimulates the release of amphiregulin, an EGF ligand, in
osteoblasts. The released amphiregulin subsequently promotes the
migration of mesenchymal progenitors due to activation of PI3K/Akt
and p38 MAPK through binding to EGF receptor (12). A recent study by our group has
indicated that the EGF-induced MC3T3-E1 cell migration is mediated
at least partially through p44/p42 MAPK, p38 MAPK, SAPK/JNK and
Akt, but not p70 S6 kinase or Rho-kinase, suggesting that p44/p42
MAPK, p38 MAPK, SAPK/JNK and Akt act as mediators in the migration
(13). In the present study, it
was revealed that EGCG markedly reduced the EGF-induced
phosphorylation of p38 MAPK in MC3T3-E1 cells. However, EGCG had
little effect on the phosphorylation of p44/p42 MAPK, SAPK/JNK and
Akt induced by EGF. Based on these results, it is most likely that
EGCG inhibits EGF-induced migration of osteoblast-like MC3T3-E1
cells by suppressing the phosphorylation of p38 MAPK.
Emerging evidence indicates that osteoblast
migration to the sites resorbed by osteoclasts is pivotal not only
for physiological bone metabolism, including skeletal development
and bone remodeling, but also for processes associated with
pathological conditions of the bone, including osteoporosis, bone
fracture repair and tumor metastasis (3–5).
An appropriate amount of migration of osteoblasts is required for
the regulation of bone turnover, and such an adequate migration is
considered to be essential for the maintenance of the quantity of
bone mass as well as bone quality. Taking these points into
account, it appears likely that EGCG modulates osteoblast
migration, resulting in the regulation of adequate bone
remodeling.
EGCG is the most abundant catechin occurring in
green tea (17,19). It is currently recognized that
green tea consumption leads to an increase of bone mass, improves
the bone mineral density and decreases the risk of bone fracture
(19). EGCG reportedly inhibits
the migration of several malignant cell types, including skin
cancer (29), prostate cancer
(30) and pancreatic cancer cells
(31). Regarding non-malignant
cells, it has been indicated that EGCG suppresses endothelial cell
migration (32). In addition, in
alveolar bone cells, lower concentrations of EGCG (1, 5 and 10
µM) alone reportedly have no effect on the migration,
whereas higher concentrations of EGCG (25 and 50 µM) alone
decrease the cell migration as revealed by a wound-healing assay
(33). In the present study, a
Transwell cell migration assay demonstrated that a lower
concentration of EGCG, which had little effect on the cell
migration in the absence of EGF, significantly reduced the
EGF-induced migration of osteoblast-like MC3T3-E1 cells. The
suppressive effect of EGCG was dose-dependent over the range of
0.3–3 µM. Furthermore, EGCG at 3 µM markedly
suppressed the EGF-induced MC3T3-E1 cell migration in a
wound-healing assay. The ability of EGCG to suppress EGF-induced
osteoblast migration may be a mechanism of its beneficial effects
on proper bone remodeling, which explains for the favorable effects
of EGCG on bone health. Further studies are in progress to
elucidate the molecular mechanisms underlying the inhibitory
effects of EGCG on EGF-induced migration of osteoblasts.
In conclusion, the results of the present study
suggest that EGCG but not chlorogenic acid significantly reduces
EGF-induced osteoblast migration and that the inhibitory effect of
EGCG is exerted at least partially through the inhibition of p38
MAPK activation triggered by EGF.
Funding
This investigation was supported in part by
Grants-in-Aid for Scientific Research from the Ministry of
Education (grant no. 26462289 to OK and grant no. 15K10487 to HT),
a Grant-in-Aid for Scientific Research from the Ministry of Health,
Labor and Welfare (grant no. H25-Aging-General-004 to HT), and the
Research Funding for Longevity Sciences from the National Center
for Geriatrics and Gerontology, Japan (grant nos. 25-4 and 26-12 to
HT).
Authors’ contributions
TK, TO and OK conceived and designed the
experiments. TK, KF, GS and RMN performed the experiments. TK, KF,
GS RMN, HT and OK analyzed the data. TK, TO, HT and OK wrote the
manuscript. All authors read and approved the final manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Acknowledgements
The authors would like to thank Mrs. Yumiko Kurokawa
(Department of Pharmacology, Gifu University Graduate School of
Medicine, Gifu, Japan) for technical assistance.
References
|
1
|
Karsenty G and Wangner EF: Reaching a
genetic and molecular understanding of skeletal development. Dev
Cell. 2:389–406. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kular J, Tickner J, Chim SM and Xu J: An
overview of the regulation of bone remodeling at cellular level.
Clin Biochem. 45:863–873. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Khan SN, Bostrom MP and Lane JM: Bone
growth factors. Orthop Clin North Am. 31:375–388. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lieberman JR, Daluiski A and Einhorn TA:
The role of growth factors in the repair of bone. Biology and
clinical applications. J Bone Joint Surg Am. 84-A:1032–1044. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Reddi AH, Roodman D, Freeman C and Mohla
S: Mechanisms of tumor metastasis to the bone: Challenges and
opportunities. J Bone Miner Res. 18:190–194. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schneider MR, Sibilia M and Erben RC: The
EGFR network in bone biology and pathology. Trends Endocrinol
Metab. 20:517–524. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kumegawa M, Hiramatsu M, Hatakeyama K,
Yajima T, Kodama H, Osaki T and Kurisu K: Effects of epidermal
growth factor on osteoblastic cells in vitro. Calcif Tissue Int.
35:542–548. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hata R, Hori H, Nagai Y, Tanaka S, Kondo
M, Hiramatsu M, Utsumi N and Kumegawa M: Selective inhibition of
type 1 collagen synthesis in osteoblastic cells by epidermal growth
factor. Endocrinology. 115:867–876. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ng KW, Partridge NC, Niall M and Martin
TJ: Stimulation of DNA synthesis by epidermal growth factor in
osteoblast-like cells. Calcif Tissue Int. 35:624–628. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fang MA, Kujubu DA and Hahn TJ: The
effects of prostaglandin E2, parathyroid hormone, and epidermal
growth factor on mitogenesis, signaling, and primary response genes
in UMR 10601 osteoblast-like cells. Endocrinology. 131:2113–2119.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vukicevic S, Kleinman HK, Luyten FP, Roche
AB and Reddi AH: Identification of multiple active growth factors
in basement membrane Matrigel suggests caution in interpretation of
cellular activity related to extracellular matrix components. Exp
Cell Res. 202:1–8. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhu J, Siclari VA, Liu F, Spatz JM,
Chandra A, Divieti Pajevic P and Qin L: Amphiregulin-EGFR signaling
mediates the migration of bone marrow mesenchymal progenitors
toward PTH-stimulated osteoblasts and osteocytes. PLoS One.
7:e500992012. View Article : Google Scholar
|
|
13
|
Kawabata T, Tokuda H, Fujita K, Kainuma S,
Sakai G, Matsushima-Nishiwaki R, Kozawa O and Otsuka T: Resveratrol
inhibits the epidermal growth factor-induced migration of
osteo-blasts: The suppression of SAPK/JNK and Akt. Cell Physiol
Biochem. 43:1025–1036. 2017. View Article : Google Scholar
|
|
14
|
Jankun J, Selman SH, Wiercz RS and
Skrzypczak-Jankun E: Why drinking green tea could prevent cancer.
Nature. 387:5611997. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Koo SH and Montminy M: In vino veritas: A
tale of two sirt1s. Cell. 127:1091–1093. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
George SE, Ramalakshmi K and Mohan Rao LJ:
A perception on health benefits of coffee. Crit Rev Food Sci Nutr.
48:464–486. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Thielecke F and Boschmann M: The potential
role of green tea catechins in the prevention of the metabolic
syndrome-a review. Phytochemistry. 70:11–24. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shimizu M, Adachi S, Masuda M, Kozawa O
and Moriwaki H: Cancer chemoprevention with green tea catechins by
targeting receptor tyrosine kinases. Mol Nutr Food Res. 55:832–843.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shen CL, Yeh JK, Cao JJ and Wang JS: Green
tea and bone metabolism. Nutr Res. 29:437–456. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Folwarczna J, Pytlik M, Zych M, Cegieła U,
Nowinska B, Kaczmarczyk-Sedlak I, Sliwinski L, Trzeciak H and
Trzeciak HI: Effects of caffeic and chlorogenic acids on the rat
skeletal system. Eur Rev Med Pharmacol Sci. 19:682–693.
2015.PubMed/NCBI
|
|
21
|
Kwak SC, Lee C, Kim JY, Oh HM, So HS, Lee
MS, Rho MC and Oh J: Chlorogenic acid inhibits osteoclast
differentiation and bone resorption by downregulation of receptor
activator of nuclear factor kappaB ligand-induced nuclear factor of
activated T cells c1 expression. Biol Pharm Bull. 36:1779–1786.
2013. View Article : Google Scholar
|
|
22
|
Singh R, Akhtar N and Haqqi TM: Green tea
polyphenol epigal-locatechin-3-gallate: Inflammation and arthritis.
[Corrected]. Life Sci. 86:907–918. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sudo H, Kodama H, Amagai Y, Yamamoto S and
Kasai S: In vitro differentiation and calcification in a new clonal
osteogenic cell line derived from newborn mouse calvaria. J Cell
Biol. 96:191–198. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kozawa O, Tokuda H, Miwa M, Kotoyori J and
Oiso Y: Cross-talk regulation between cyclic AMP production and
phosphoinositide hydrolysis induced by prostaglandin E2
in osteoblast-like cells. Exp Cell Res. 198:130–134. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Karagiosis SA, Chrisler WB, Bollinger N
and Karin NJ: Lysophosphatidic acid-induced ERK activation and
chemotaxis in MC3T3-E1 preosteoblasts are independent of EGF
receptor transactivation. J Cell Physiol. 219:716–723. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Laemmli UK: Cleavage of structural
proteins during the assembly of the head of bacteriophage T4.
Nature. 227:680–685. 1970. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kato K, Ito H, Hasegawa K, Inaguma Y,
Kozawa O and Asano T: Modulation of the stress-induced synthesis of
hsp27 and αB-crystallin by cyclic AMP in C6 rat glioma cells. J
Neurochem. 66:946–950. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yang CS, Chen LS, Lee ML, Balentine D, Kuo
MC and Schantz SP: Blood and urine levels of tea catechins after
ingestion of different amounts of green tea by human volunteers.
Cancer Epidemiol Biomark Prev. 7:351–354. 1998.
|
|
29
|
Liu JS, Chen SH, Lin CL, Tsai SH and Liang
YC: Inhibition of melanoma growth and metastasis by combination
with (−)-epigal-locatechin-3-gallate and dacarbazine in mice. J
Cell Biochem. 83:631–642. 2001. View
Article : Google Scholar
|
|
30
|
Siddiqui IA, Malik A, Adhami VM, Asim M,
Hafeez BB, Sarfaraz S and Mukhtar H: Green tea polyphenol EGCG
sensitizes human prostate carcinoma LNCaP cells to TRAIL-mediated
apoptosis and synergistically inhibits biomarkers associated with
angiogenesis and metastasis. Oncogene. 27:2055–2063. 2008.
View Article : Google Scholar
|
|
31
|
Shankar S, Ganapathy S, Hingorani SR and
Srivastava RK: EGCG inhibits growth, invasion, angiogenesis and
metastasis of pancreatic cancer. Front Biosci. 13:440–452. 2008.
View Article : Google Scholar
|
|
32
|
Singh AK, Seth P, Anthony P, Husain MM,
Madhavan S, Mukhtar H and Maheshwari RK: Green tea constituent
epigal-locatechin-3-gallate inhibits angiogenic differentiation of
human endothelial cells. Arch Biochem Biophys. 401:29–37. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mah YJ, Song JS, Kim SO, Lee JH, Jeon M,
Jung UW, Moon SJ, Kim JH and Choi HJ: The effect of
epigallocatechin-3-gallate (EGCG) on human alveolar bone cells both
in vitro and in vivo. Arch Oral Biol. 59:539–549. 2014. View Article : Google Scholar : PubMed/NCBI
|