Introduction
Follicular thyroid carcinoma (FTC) and papillary
thyroid carcinoma (PTC) are major histological types of thyroid
carcinoma that account for 10–20 and 75–85% of thyroid carcinomas,
respectively (1–3). They are both classified as
differentiated thyroid carcinomas originating from a common cell
type (i.e., follicular cells) (4).
In Japan, according to a nationwide cancer registry by the Japanese
Society of Thyroid Surgery, a total of 52,109 patients with thyroid
carcinoma underwent surgery between 1977 and 2005, including 4,910
(9.4%) cases of FTC and 45,683 (87.7%) cases of PTC [Saikawa et
al, Abstracts of the 40th Annual Meeting of the Japanese
Society of Thyroid Surgery, Japanese Society of Thyroid Surgery:
pp121-136, 2007 (in Japanese)].
The pathological diagnosis and classification of FTC
were based on the recent World Health Organization classification
system (4). FTC is defined by the
presence of vascular and/ or capsular invasion and the absence of
diagnostic nuclear features of papillary carcinoma (4). This carcinoma is further divided into
minimally invasive FTC (MI-FTC) and widely invasive FTC (WI-FTC)
(4,5). MI-FTC has limited capsular and/or
vascular invasion, whereas WI-FTC shows widespread infiltration of
adjacent thyroid tissue and/or blood vessels. For tumors suspected
of being MI-FTC, a standard operation method is thyroid lobectomy
(www.endocrineweb.com/conditions/thyroid/thyroid-operations;
accessed May 10, 2011) (5). MI-FTC
shows good long-term outcomes. However, in some cases, MI-FTC
metastasizes to the lung and bone, exhibiting a poor prognosis
(i.e., metastatic MI-FTC). Nonetheless, distinguishing between
metastatic and non-metastatic MI-FTCs is currently difficult by any
pathological modalities. When distant metastasis is recognized
during the follow-up period, additional therapies, such as
completion total thyroidectomy and radioiodine ablation therapy,
are needed (5). Thus,
identification of prognostic biomarkers for predicting groups at
high risk for metastasis among patients diagnosed with MI-FTC after
the initial operation should be important in the postoperative
follow-up of MI-FTC.
MicroRNAs (miRNAs) are endogenous, non-coding, small
RNAs of 19–23 nucleotides in length that posttranscriptionally
regulate the expression of their target genes at mRNA and/ or
protein levels (6). So far,
several miRNA profiling studies have demonstrated dysregulated
miRNA expression in various types of human carcinomas and the
potential use of miRNAs as diagnostic and/or prognostic markers was
recently described (7–11). In terms of thyroid carcinomas,
several reports have addressed dysregulated miRNA expression in PTC
(12–14). On the other hand, information on
miRNA expression in FTC, especially MI-FTC, is quite limited. In
this study, we aimed to identify novel prognostic factors for
metastatic MI-FTC and performed comprehensive profiling of miRNA
expression in formalin-fixed, paraffin-embedded (FFPE) samples of
FTC obtained at the initial operation using a combination of laser
microdissection (LMD) and quantitative PCR-based array.
Furthermore, we assessed the potential use of miRNAs as novel
biomarkers for the metastatic potential of MI-FTC by logistic
regression analysis.
Materials and methods
Patients and specimens
The records of 34 patients with MI-FTC who underwent
surgery at Kuma Hospital (Hyogo, Japan) and Nippon Medical School
Hospital (Tokyo, Japan) were selected from our archives of around
200 patients with MI-FTC between 1991 and 2009, of which the
proportion of all thyroid cancers was 2–3%. The 34 cases met the
following criteria: i) histopathological evaluation of the primary
surgical specimens as MI-FTC was done according to the criteria of
World Health Organization (4), ii)
patients had undergone Tg (thyroglobulin) testing and neck
ultrasonography routinely for ≥10 years after surgery and iii)
patients were Tg antibodies-negative. This study was carried out in
accordance with the principles embodied in the 1975 Declaration of
Helsinki and informed consent for the use of thyroid tissues was
obtained from each patient. We categorized 34 patients with MI-FTC
into two groups: the metastatic group, M(+) (n=12) and the
non-metastatic group, M(−) (n=22). In the M(+) group, distant
metastasis was recognized after the initial operation established
the diagnosis of MI-FTC. In the M(−) group, no distant metastasis
was recognized postoperatively for ≥10 years. Although patients in
both groups were clinicopathologically diagnosed with MI-FTC at the
time of the initial operation, neither routine pathological
examination nor clinical data could distinguish between the M(+)
and M(−) groups. Clinical characteristics of each individual case
are presented in Table I.
 | Table IClinical features of the MI-FTC
patients in this study. |
Table I
Clinical features of the MI-FTC
patients in this study.
| | | | | | Tg (ng/ml)d | Invasion | Distant metastasis
after surgery |
|---|
|
|
|
|---|
| No. | Metastasis | Sex | Agea | Tumor size
(mm)b | Operation
methodc | Pre-operation | Post-operation | c/ve | Period (month) | Location | Additional
therapies |
|---|
| 1 | + | M | 67 | 49 | Lo | 18.9 | unknown | +/+ | 85 | B | TT and RAT |
| 2f | + | M | 68 | 75 | TT | >8000 | 4.2 | +/+ | 51 | L, B | |
| 3g | + | F | 68 | 90 | TT | >8000 | 130.0 | +/+ | 36 | L | |
| 4 | + | M | 15 | 86 | Lo | 6987.0 | 17.0 | +/+ | 26 | L | TT and RAT |
| 5 | + | F | 51 | 60 | TT | 4067.0 | 11.4 | +/+ | 40 | L | RAT |
| 6 | + | F | 50 | 19 | Lo | 46.6 | 8.1 | +/− | 36 | L, B | TT and RAT |
| 7 | + | F | 58 | 38 | Lo | 179.0 | 10.1 | +/− | 72 | L, B | TT and RAT |
| 8 | + | F | 47 | 23 | Lo | 640.0 | 6.4 | +/+ | 98 | B | TT and RAT |
| 9 | + | M | 72 | 48 | Lo | 770.0 | 17.0 | +/+ | 62 | L | TT and RAT |
| 10 | + | F | 57 | 90 | TT | >8000 | 162.6 | −/+ | 13 | B | RAT |
| 11 | + | M | 54 | 58 | Lo | 83.3 | 25.3 | +/+ | 68 | L | TT and RAT |
| 12 | + | F | 47 | 45 | TT | 3870 | <0.5 | +/− | 26 | B | RAT |
| 13 | − | M | 53 | 45 | Lo | 2118.0 | 13.3 | +/− | | na | |
| 14 | − | F | 49 | 45 | Lo | 814.0 | <2.0 | +/− | | na | |
| 15 | − | F | 55 | 15 | Lo | 51.7 | 17.9 | +/− | | na | |
| 16 | − | F | 38 | 23 | Lo | 581.0 | 17.0 | +/− | | na | |
| 17 | − | F | 63 | 65 | Lo | 1269.0 | 51.3 | +/− | | na | |
| 18 | − | F | 64 | 46 | Lo | 2024.0 | 5.3 | +/− | | na | |
| 19 | − | F | 50 | 28 | Lo | 75.7 | 24.8 | +/+ | | na | |
| 20 | − | F | 33 | 24 | ST | 399.0 | <2.0 | +/+ | | na | |
| 21 | − | F | 37 | 47 | Lo | 81.2 | 3.6 | +/− | | na | |
| 22 | − | F | 28 | 40 | Lo | 183.0 | 37.0 | +/− | | na | |
| 23 | − | F | 37 | 55 | Lo | 1049.0 | 9.6 | +/+ | | na | |
| 24 | − | F | 47 | 57 | Lo | 1724.0 | 13.7 | +/− | | na | |
| 25 | − | M | 74 | 32 | Lo | 50.2 | 19.2 | +/+ | | na | |
| 26 | − | F | 32 | 31 | Lo | 67.6 | 19.0 | +/+ | | na | |
| 27 | − | M | 64 | 49 | Lo | 2153.4 | 20.6 | +/− | | na | |
| 28 | − | M | 35 | 30 | Lo | 401.1 | 10.0 | +/− | | na | |
| 29 | − | F | 29 | 40 | Lo | 1049.2 | 9.5 | +/− | | na | |
| 30 | − | F | 25 | 46 | Lo | 1051.9 | 7.0 | +/− | | na | |
| 31 | − | M | 38 | 44 | TT | 343.4 | <0.5 | +/− | | na | |
| 32 | − | F | 23 | 33 | Lo | 78.6 | 10.8 | +/− | | na | |
| 33 | − | F | 50 | 77 | TT | 4640 | 4.1 | +/− | | na | |
| 34 | − | M | 29 | 78 | Lo | 178.4 | 23.1 | +/− | | na | |
In order to further elucidate the miRNA expression
profile characteristics of metastatic MI-FTC, we also analyzed the
samples of patients with WI-FTC. All the records of patients with
WI-FTC who underwent surgery at Kuma Hospital between 1998 and 2009
were collected (n=13). They met the criterion that
histopathological evaluation of the primary surgical specimens as
WI-FTC was done according to the criteria of World Health
Organization (4); clinical
characteristics of each individual case are presented in Table II.
 | Table IIClinical features of the WI-FTC
patients in this study. |
Table II
Clinical features of the WI-FTC
patients in this study.
| | | | | Distant metastasis
|
|---|
| No. | Metastasis | Sex | Agea | Operation
method | Period (month) | Location | Additional
therapies |
|---|
| 35 | + | M | 43 | Lo | 23 | L | TT and RAT |
| 36 | + | F | 75 | TT | 0 | L, T | RAT |
| 37 | + | F | 76 | TT | 0 | L | RAT |
| 38 | + | F | 60 | TT | 101 | L | RAT |
| 39 | + | F | 56 | TT | 54 | B | RAT |
| 40 | + | F | 34 | TT | 39 | L | RAT |
| 41 | + | F | 42 | TT | 93 | L, B | RAT |
| 42 | + | F | 63 | Lo | 51 | L | TT and RAT |
| 43 | + | M | 63 | TT | 0 | L | RAT |
| 44 | + | F | 65 | TT | 15 | B | RAT |
| 45b | − | F | 39 | Lo | | na | |
| 46b | − | F | 37 | Lo | | na | |
| 47b | − | F | 36 | Lo | | na | |
RNA purification from FFPE samples by
LMD
The 34 archival FFPE samples of MI-FTC and 13 of
WI-FTC were processed into 20-μm sections and subjected to
hematoxylin-eosin staining. We then microdissected areas containing
carcinoma tissues in each section using an LMD microscope (LMD6000
System, Leica, Wetzlar, Germany).
The microdissected tissues were treated with xylene
to remove paraffin and digested in a buffer containing 10% sodium
dodecyl sulfate (Sigma-Aldrich, St. Louis, MO) and 20 mg/ml
proteinase K (Roche Diagnostics, Mannheim, Germany) at 55°C with
continuous stirring for 12 h. Total RNAs in these tissues were then
extracted using Isogen-LS reagent (Wako, Osaka, Japan) according to
the manufacturer’s protocol.
Comprehensive quantitative analysis of
miRNA expression using quantitative PCR-based array
Comprehensive analysis of miRNA expression levels in
MI-FTC was performed by real-time PCR using TaqMan MicroRNA Array
Panels (Applied Biosystems, Foster City, CA), which are designed to
detect 667 human miRNAs. Equal quantities of total RNA isolated
from each of 9 M(+) and 10 M(−) MI-FTC FFPE samples were pooled
within the carcinoma groups. The pooled total RNAs (252 ng) were
reverse-transcribed using Megaplex RT Primers (Applied Biosystems).
These cDNAs were pre-amplified using Megaplex PreAmp Primers
(Applied Biosystems). The pre-amplified products were applied to
real-time PCR using TaqMan MicroRNA Assays Human Panels (A and B,
v2.0) on a 7900HT Fast Real-Time PCR system (Applied Biosystems)
according to the manufacturer’s instructions; miRNA sequences were
annotated by the Sanger Data Base (miRBase) Release 14. Data
obtained with this assay were analyzed using RQ Manager 1.2
(Applied Biosystems). For the quantification of each miRNA
expression level, the relative Ct method (ΔΔCt method) was applied.
Small endogenous nucleolar RNA U44 (RNU44) was used
as an internal control for data normalization.
Quantitative analysis of miRNA expression
by real-time PCR
Expression of individual miRNAs was validated using
TaqMan miRNA assays (Applied Biosystems). Briefly, 10 ng total RNA
was reverse-transcribed using a reverse transcription (RT) primer
specific for individual miRNAs with MultiScribe Reverse
Transcriptase (Applied Biosystems). The RT products were
subsequently subjected to a PCR reaction with primer sets specific
for individual miRNAs. Amplification of miRNA-derived PCR products
was monitored on an ABI 7300 Real-Time PCR system (Applied
Biosystems). All reactions were performed in triplicate and
RNU44 was used as a reference for data normalization. For
absolute quantification of the expression levels of miRNAs,
serially diluted synthetic mimics of these miRNAs and RNU44
(Gene Design, Osaka, Japan) were used as standards.
Statistical analysis
The statistical differences of miRNA expression
among different groups [i.e., M(+) and M(−) MI-FTC groups and
WI-FTC group] were analyzed by Kruskal-Wallis test.
As mentioned above, 9 M(+) and 10 M(−) MI-FTC FFPE
samples were used for comprehensive analysis of miRNA expression
levels in MI-FTC by PCR-based array. These training samples were
later merged into the validation samples using the validation of
miRNA expression in individual MI-FTC samples since it was
difficult to collect further, more testing samples. Leave-one-out
cross-validation was performed to protect overfitting and test the
stability and predictive capability of our model using the entire
34 samples with MI-FTC. The overall predictive accuracy of the
discriminant function, i.e., hit ratio was calculated. The
classification accuracy was considered high when the hit ratio was
calculated to be ≥25% greater than that achieved by chance
(15).
To assess the prognostic value of miRNAs in the
prediction of metastasis after the initial MI-FTC operation, odds
ratios (ORs) with 95% confidence intervals (CIs) were calculated.
Either the χ2 test or the Mann-Whitney U test was used
to examine a possible association between metastatic status and
clinicopathological parameters including miRNAs. Only variables
that were significant in univariate analyses were used in a
multivariate model. Multicollinearity was also assessed by using
the variance inflation factor (VIF); a VIF exceeding 10 was
regarded as indicating serious multicollinearity (16). Forced-entry binary logistic
regression was used to predict the metastasis after the initial
MI-FTC operation. We conducted all analyses using a statistical
software package (SPSS for Windows, version 20, IBM-SPSS, Chicago,
IL) and p-values <0.05 were considered statistically
significant.
Results
Identification of miRNAs upregulated in
FFPE samples of metastatic MI-FTC using a combination method of LMD
and quantitative PCR-based miRNA expression array
To identify miRNAs with aberrant expression in
metastatic MI-FTCs, we performed the initial experiments of
comparison of miRNA expression profiles between 9 M(+) and 10 M(−)
MI-FTC LMD FFPE samples using a real-time PCR-based miRNA
expression profiling array (Table
I; nos. 1–9 and 13–22). The pooled samples (equal amounts of
RNA from each individual samples) were analyzed by real-time
PCR-based array as an initial screening since the amounts of total
RNAs extracted from LMD samples were limited. Considering the
clinical use of miRNAs as potential biomarkers, those expressed at
high levels in MI-FTCs should be advantageous in terms of
sensitivity and reliability. Thus, we first screened miRNAs based
on the Ct values, which were considered to roughly reflect the
expression levels of these miRNAs. We preliminarily examined the
expression levels of some miRNAs with Ct values >25 in the array
analysis and found that in many, if not most, cases, the miRNAs
were expressed at low levels, i.e., these Ct values were >35 or
undetermined (17). It can be
explained by the fact that cDNAs were pre-amplified for the array
analysis. Thus, miRNAs with Ct values ≤25 in either M(+) or M(−)
groups were subjected to further analysis; 178 miRNAs satisfied
this criterion for all samples (Table
III; the full data set is available upon request).
 | Table IIIRepresentative miRNAs highly
upregulated in the metastatic MI-FTC, as revealed by quantitative
PCR-based array. |
Table III
Representative miRNAs highly
upregulated in the metastatic MI-FTC, as revealed by quantitative
PCR-based array.
| | Ct valueb
|
|---|
| miRNAa | Fold change | M(+) | M(−) |
|---|
|
miR-375 | 12.34 | 20.34 | 23.97 |
|
miR-222 | 11.44 | 12.05 | 15.57 |
|
miR-221 | 6.36 | 17.72 | 20.39 |
|
miR-10b | 5.04 | 19.64 | 21.97 |
|
miR-222* | 4.99 | 20.65 | 22.97 |
|
miR-92a | 4.01 | 19.14 | 21.14 |
| miR-16 | 3.70 | 14.45 | 16.34 |
| miR-31 | 3.69 | 18.08 | 19.96 |
| miR-29b | 3.69 | 21.08 | 22.96 |
|
miR-130b* | 3.57 | 23.17 | 25.01 |
| miR-204 | 3.50 | 19.16 | 20.97 |
|
miR-181c | 3.43 | 22.21 | 23.99 |
|
miR-296-5p | 3.39 | 22.15 | 23.91 |
| miR-26a | 3.39 | 16.22 | 17.98 |
| let-7c | 3.36 | 19.90 | 21.65 |
|
miR-135a | 3.32 | 16.26 | 17.99 |
|
miR-125a-5p | 3.31 | 19.23 | 20.96 |
| miR-23b | 3.22 | 20.48 | 22.17 |
|
miR-146a | 3.19 | 17.30 | 18.97 |
|
miR-130b | 3.15 | 22.32 | 23.98 |
| miR-328 | 3.12 | 19.00 | 20.64 |
| miR-454 | 3.11 | 18.43 | 20.07 |
|
miR-106a | 3.10 | 16.32 | 17.95 |
|
miR-130a | 3.10 | 19.79 | 21.42 |
| miR-17 | 3.08 | 17.06 | 18.68 |
| miR-101 | 3.03 | 23.35 | 24.95 |
| miR-320 | 3.00 | 18.39 | 19.97 |
| miR-605 | 3.00 | 23.10 | 24.68 |
In the 178 miRNAs that met the above criteria, we
then focused on the miRNAs that were upregulated or downregulated
by >4.0-fold in the M(+) group compared to the M(−) group since
the amounts of total RNAs extracted from LMD samples were limited.
Six miRNAs, i.e., miR-221, miR-222,
miR-222*, miR-10b, miR-92a and
miR-375, were upregulated. Their expression levels were
upregulated >4-fold in the M(+) group compared to the M(−) group
(Table III). Three miRNAs, i.e.,
miR-221, miR-222 and miR-222*,
belongs to the miR-221/222 cluster. Two miRNAs, i.e.,
miR-888 and miR-891a, were downregulated >4-fold
in the M(+) group compared to the M(−) group; the fold changes for
miR-888 and miR-891a were 0.02 and 0.03,
respectively.
Validation of miRNA expression in
individual FTC samples by quantitative PCR
For the PCR-based array analysis described above, we
used pooled RNA samples from the FTC samples; thus, only the
averaged miRNA expression profiles could be obtained. For the
validation of miRNA expression in individual MI-FTC samples, the
cases of patients with MI-FTC were increased from 19 to 34 [12 and
22 samples for M(+) group and M(−) group, respectively]. However,
due to the limited sample size, cross validation was used to
protect overfitting and test the stability and predictive
capability of our model using the entire 34 samples with MI-FTC.
Clinical characteristics of these cases are summarized in Table IV. As seen in Table IV, only variables that were
significant in univariate analyses were used for the
cross-validation. Prognostic variables were age (continuous),
vascular invasion (dichotomous) and four miRNAs (continuous;
miR-221, miR-222*, miR-10b and
miR-92a). The hit ratio was 76.5%; the cross validated
classification showed that overall 76.5% were correctly
classified.
 | Table IVSummary of clinicopathological
features of the MI-FTC patients in this study. |
Table IV
Summary of clinicopathological
features of the MI-FTC patients in this study.
| M(+) n=12 | M(−) n=22 | P-value |
|---|
| Sex | | | |
| Female/male | 7/5 | 16/6 | 0.315e |
| Age | 54.5±15.2 | 43.3±14.4 | 0.028f |
| Tumor size
(mm) | 56.8±24.5 | 43.2±16.3 | 0.094f |
| Operation
method | | | |
| Lo/ST+ TT | 7/5 | 19/3 | 0.080e |
| Tg (ng/ml)a | | | |
|
Pre-operation | 3388.5±3511.0 | 926.5±1097.3 | 0.217f |
|
Post-operation | 32.8±54.0 | 14.6±12.1 | 0.986f |
| Invasionb | | | |
| Capsular invasion
+/− | 11/1 | 22/0 | 0.353e |
| Vascular invasion
+/− | 9/3 | 5/17 | 0.005e |
| Distant metastasis
after surgery | | | |
| Period
(month) | 51.1±26.1 | na | |
| Location | | | |
| Lung | 8 | na | |
| Bone | 7 | | |
| Additional
therapiesc | 10 | na | |
| Expression level of
miRNAsd | | | |
|
miR-221 | 43.792±41.809 | 9.351±21.818 | <0.001f |
|
miR-222 | 97.800±84.473 | 22.455±42.031 | <0.001f |
|
miR-222* | 0.372±0.250 | 0.102±0.150 | <0.001f |
|
miR-10b | 0.149±0.088 | 0.045±0.045 | <0.001f |
|
miR-92a | 9.032±5.597 | 4.137±3.637 | <0.001f |
|
miR-375 | 0.136±0.209 | 0.065±0.086 | 0.309f |
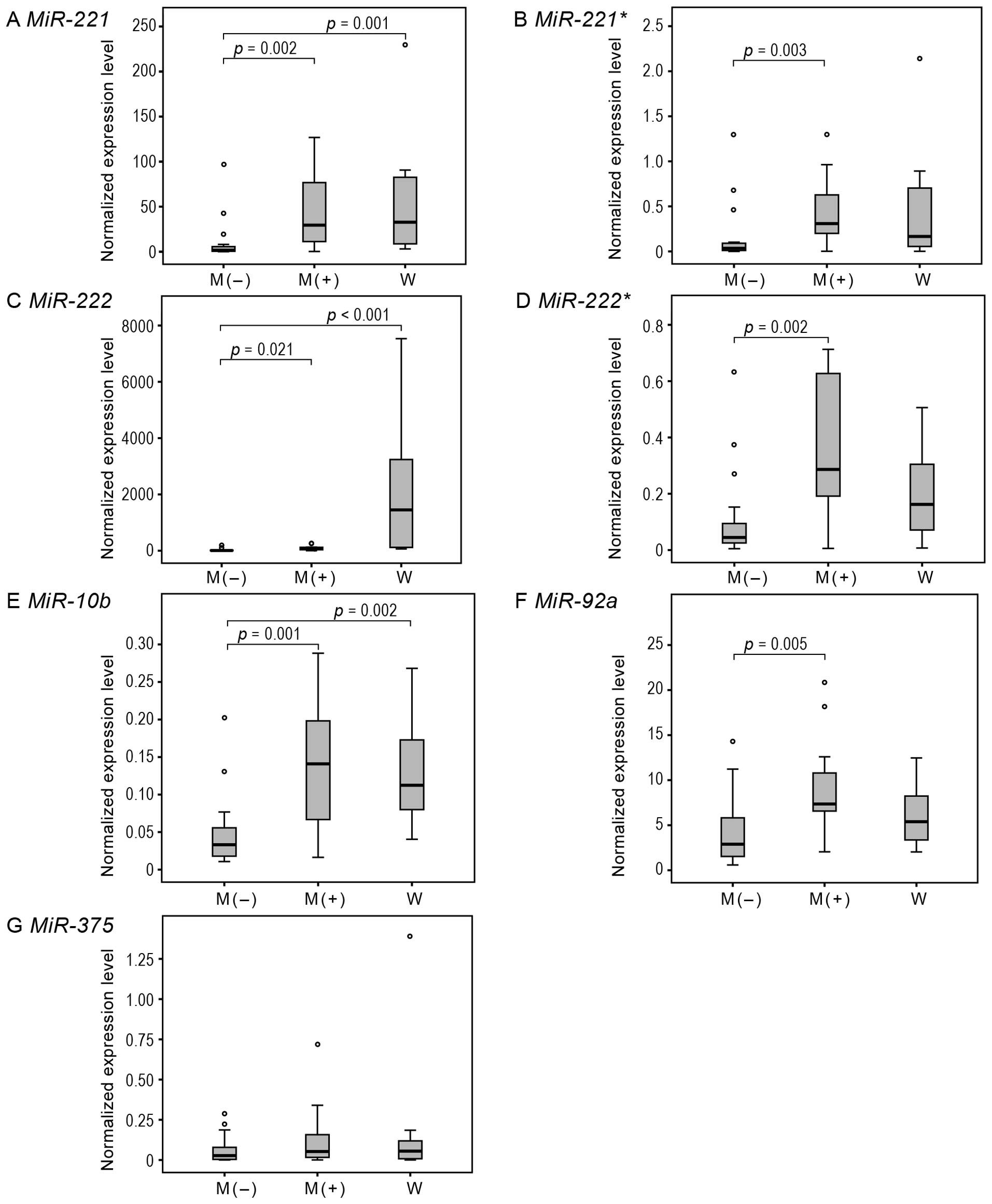
Then, we performed real-time PCR analysis to
quantify and validate the expression of the miRNAs (Figs. 1 and 2). This miRNA expression analysis
revealed that the expression levels of miR-221,
miR-222, miR-222*, miR-10b and
miR-92a were significantly upregulated in M(+) samples
compared to M(−) samples (p=0.002, 0.021, 0.002, 0.001, 0.005,
respectively), whereas, miR-375 was not significantly
upregulated in M(+) samples compared to M(−) samples (p=0.532).
Note that another member of the miR-221/222 cluster,
miR-221*, was also shown to be significantly
upregulated (p=0.003), although this miRNA did not meet the
criterion for the screening based on our array analysis [the
fold-change was 3.63, but Ct values of M(+) and M(−) were 27.12 and
28.98, respectively].
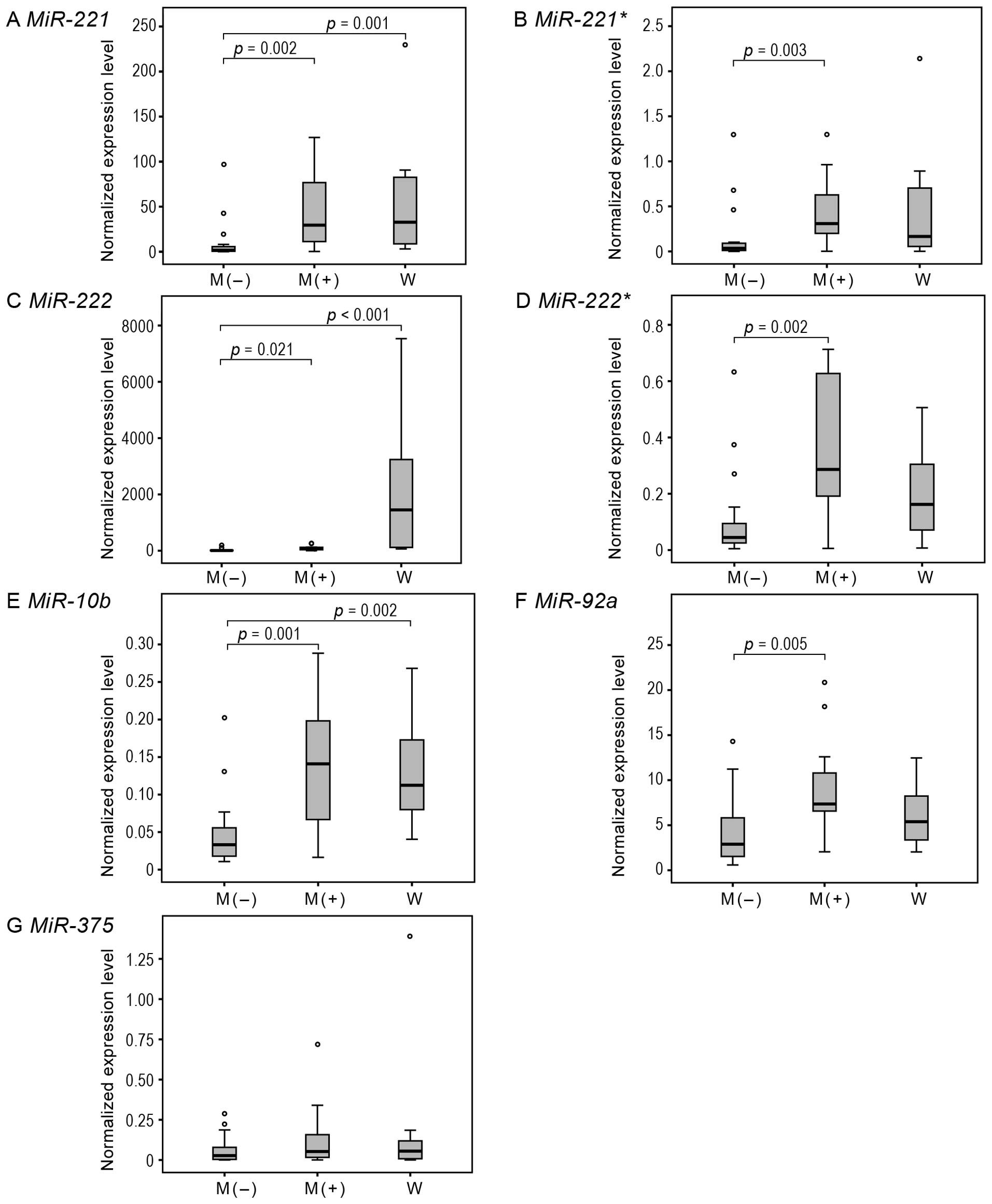 | Figure 1Quantitative PCR analysis to assess
the expression levels of miR-221, miR-221*,
miR-222, miR-222*, miR-10b, miR-92a and
miR-375 in MI-FTC and WI-FTC. Box plots show the expression
levels of these miRNAs in M(+) MI-FTC and WI-FTC (W) samples
compared to those in M(−) MI-FTC samples. The expression levels of
these miRNAs were absolutely quantified and normalized for the
expression level of RNU44 in each sample; miRNA
(amol/μl)/RNU44 (amol/μl). Six miRNAs [(A)
miR-221, (B) miR-221*, (C) miR-222,
(D) miR-222*, (E) miR-10b, (F)
miR-92a and (G) miR-375] are shown to be
significantly upregulated in M(+) samples compared to M(−). Three
miRNAs [(A) miR-221, (C) miR-222 and (E)
miR-10b] are shown to be significantly upregulated in W
samples compared to M(−). Lines inside boxes denote medians, the
boxes represent the interquartile range and whiskers extend to the
most extreme values within 1.5 times the interquartile range.
Outliers are indicated with circles. The statistical differences
among these three groups are analyzed by Kruskal-Wallis test. |
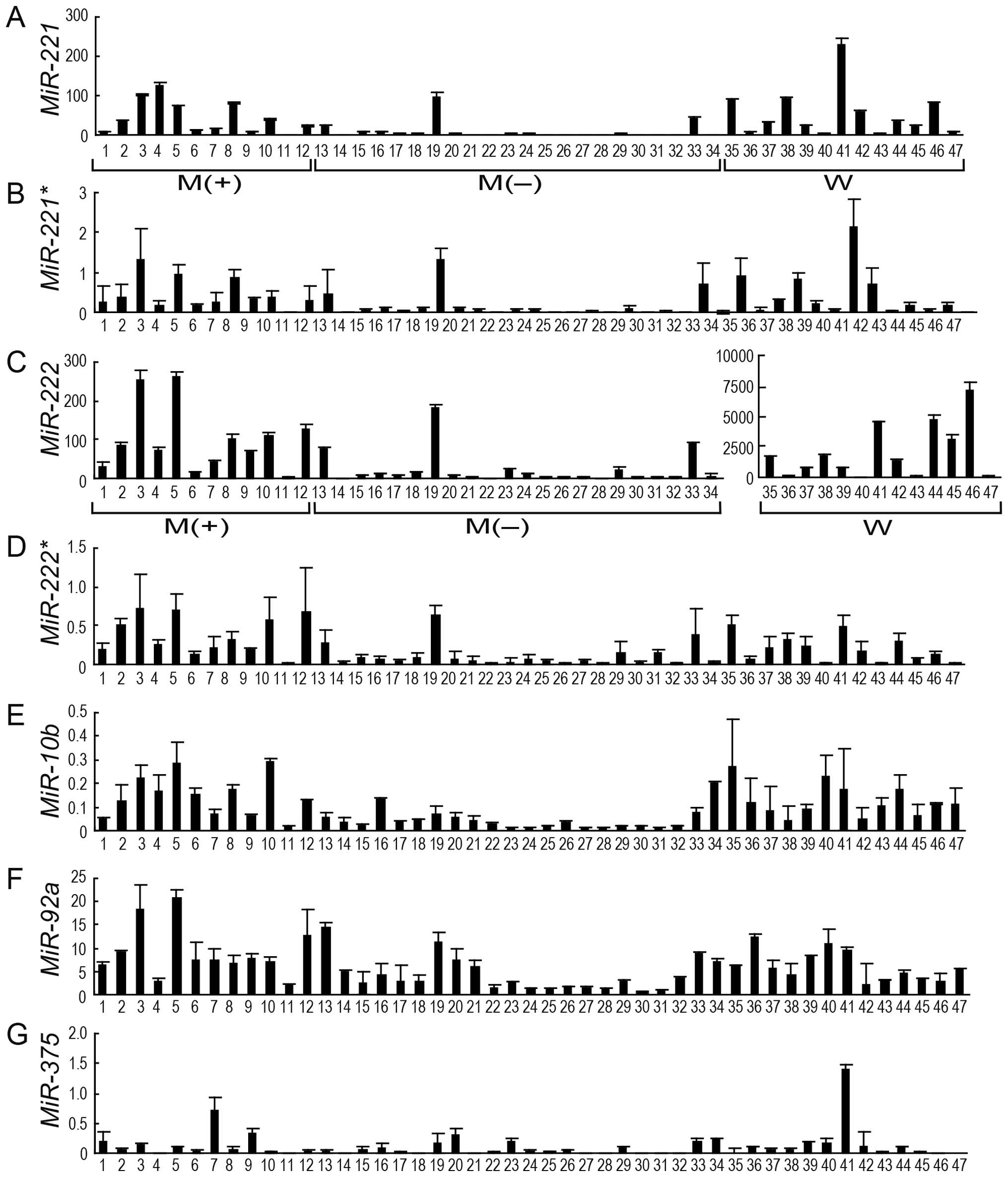
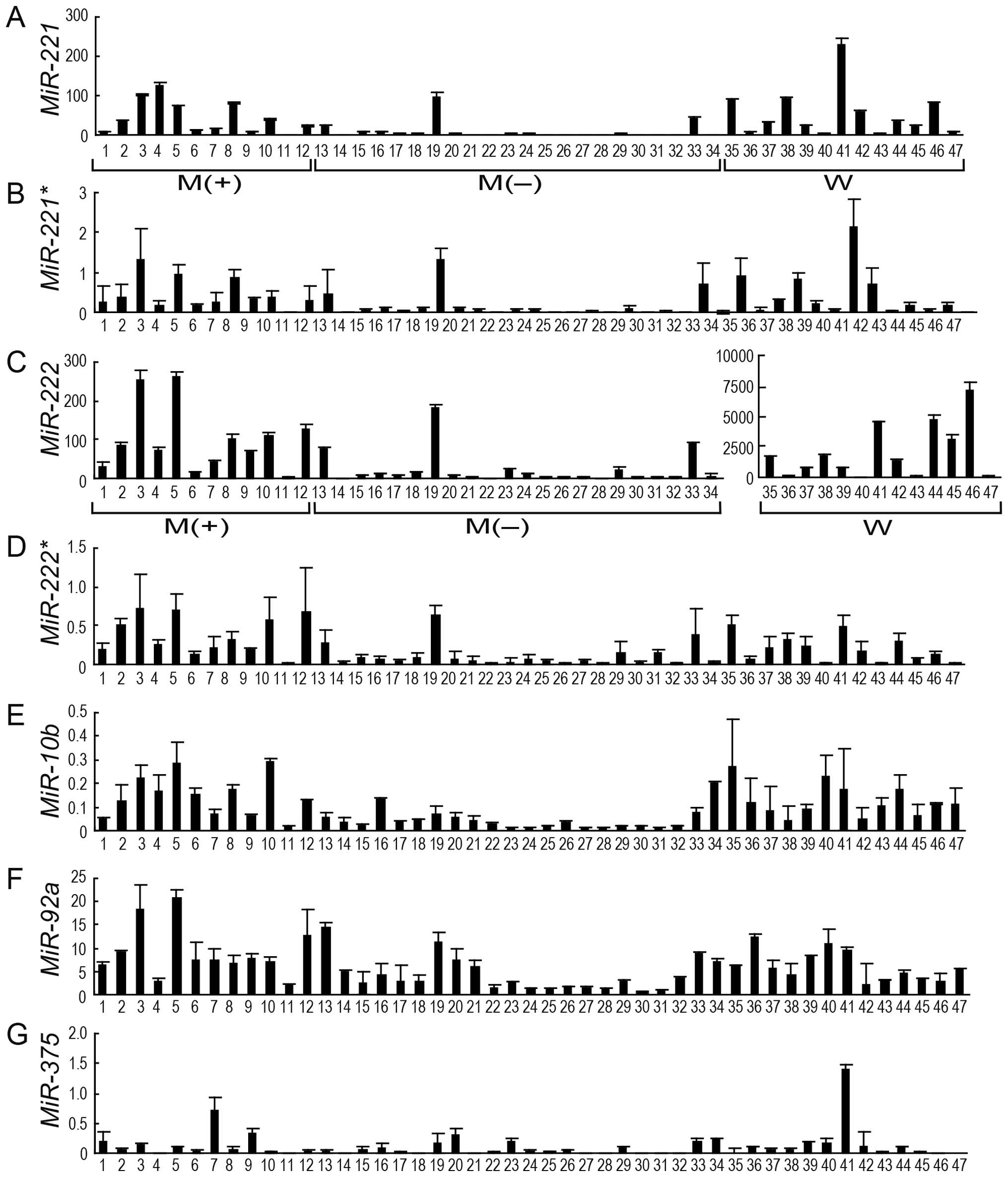 | Figure 2Histogram illustration showing the
expression levels of miR-221, miR-221*,
miR-222, miR-222*, miR-10b, miR-92a and
miR-375 in 47 samples of FTC. The expression levels of these
miRNAs [(A) miR-221, (B) miR-221*, (C)
miR-222, (D) miR-222*, (E) miR-10b,
(F) miR-92a and (G) miR-375] in samples
laser-microdissected from metastatic MI-FTC [M(+); nos. 1–12],
non-metastatic MI-FTC [M(−); nos. 13–34] and WI-FTC (W; nos.
35–47). The expression levels of these miRNAs were absolutely
quantified and shown as the values normalized for the expression
level of RNU44 in each sample; miRNA
(amol/μl)/RNU44 (amol/μl). The data are
presented as the mean ± SD. |
Furthermore, we investigated the expression levels
of these miRNAs in WI-FTC samples to assess whether the miRNA
expression patterns in metastatic MI-FTC were similar to those in
WI-FTC that has distant metastasis and worse prognosis.
Quantitative PCR analysis revealed that miR-221,
miR-222, miR-10b and were significantly upregulated
in WI-FTC tissues compared to M(−) tissues (p=0.001, p<0.001 and
p=0.002, respectively) (Fig. 1).
The p-values for miR-221*,
miR-222* and miR-92a were 0.070, 0.299 and
0.197, respectively. It should be noted that the expression pattern
of upregulation of miR-221/222 cluster and miR-10b in
metastatic MI-FTC was substantially similar to that of WI-FTC
(Fig. 1).
In addition, we also examined the expression levels
of miR-888 and miR-891a, in individual FTC samples by
real-time PCR, these downregulated miRNAs were not significantly
downregulated in M(+) samples compared to M(−) samples (data not
shown).
Evaluation of the prognostic values of
miRNAs in MI-FTC
A logistic regression analysis was conducted to
evaluate the prognostic values of miRNAs in the prediction of
MI-FTC metastasis. As seen in Table
IV, only variables that were significant in univariate analyses
were used in a multivariate model. MiR-222 was excluded as
an independent variable since the value of VIF for miR-222
was 18.332, indicating serious multicollinearity. The dependent
variables were M(+) and M(−); independent variables considered in
the model were age, vascular invasion and four miRNAs
(miR-221, miR-222*, miR-10b and
miR-92a). Forced-entry binary logistic regression was used
to predict the metastasis after the initial MI-FTC operation. A
test of the full model against a constant only model was
statistically significant, indicating that the prognostic variables
as a set reliably distinguished between M(+) and M(−) groups
(χ2=25.552, p<0.001 with df=6). Prediction success
overall was 85.3% [86.4% for M(−) and 83.3% for M(+)]. The Wald
criterion demonstrated that only miR-10b made a significant
contribution to prognosis [OR for a 1 standard deviation (SD)]
increase 19.756, 95% CI 1.433–272.355, p=0.026). ORs, 95% CIs and
p-values are summarized in Table
V. These data imply that miR-10b has potential as a
prognostic factor for MI-FTC.
 | Table VPrognostic factors for prediction of
MI-FTC metastasis. |
Table V
Prognostic factors for prediction of
MI-FTC metastasis.
| Prognostic
factor | P-value | OR (per SD
increase) | 95% CI |
|---|
| miR-10b | 0.026 | 19.759 | 1.433–272.355 |
| miR-92a | 0.695 | 0.495 | 0.015–16.592 |
| miR-221 | 0.706 | 0.674 | 0.087–5.232 |
|
miR-222* | 0.508 | 2.960 | 0.119–73.725 |
| Vascular
invasion | 0.110 | 12.650 | 0.564–283.580 |
| Age | 0.129 | 1.091 | 0.975–1.220 |
| Constant | 0.045 | 0.002 | |
Discussion
In this study, we performed a comprehensive analysis
of miRNA expression in MI-FTC and found that miRNAs comprising the
miR-221/222 cluster, miR-10b and miR-92a were
significantly upregulated in metastatic MI-FTC. We used FFPE
samples obtained from surgical operations for LMD analysis. Stocks
of pathologic samples, such as FFPE specimens, are of great
advantage in the design of clinical studies. Protein markers in
FFPE tissues are generally stable provided that they are stored
appropriately; thus, they can be detected by means of various
immunohistological staining methods as well as mass spectrometry
analysis. Conversely, RNAs are believed to be relatively unstable
in FFPE samples and Xi et al indeed showed that the
detectable levels of mRNA transcripts in freshly frozen samples and
FFPE samples are poorly correlated (18). This could be explained in part by
the fragmentation of mRNAs in FFPE samples; cellular RNAs were
demonstrated to survive fixation and embedding procedures and RNA
extraction as relatively short (<300-bp) fragments (19). Furthermore, RNAs in FFPE samples
undergo some chemical modifications, which in turn facilitates
fragmentation and interferes with enzymatic reactions such as RT
(20,21). In contrast, small RNAs such as
miRNAs have been demonstrated to be more stable, emerging as
suitable molecules for the molecular characterization of FFPE
samples (18). In addition, active
miRNAs are present intracellularly as a complex with an RNA-induced
silencing complex, which possibly protects miRNAs from degradation.
Application of the LMD technique makes FFPE samples even more
advantageous in selective regions, e.g., carcinoma regions. No
prior study has been conducted using LMD for the molecular analysis
of FTC. To our knowledge, this is the first study to achieve the
comprehensive analysis of miRNA expression in MI-FTC using LMD.
The miR-221/222 cluster consists of four
miRNAs: miR-221, miR-221*, miR-222
and miR-222*. miR-221 and miR-222
were also previously reported to be upregulated miRNAs in PTC
(12–14). In addition, miR-221 and
miR-222 were identified as upregulated in FTC (22). Thus, these miRNAs appear to be
closely linked with the pathogenesis of both PTC and FTC. In
contrast, miR-221* and miR-222*
have been considered to be minor miRNAs and the expression of these
miRNAs in thyroid tumors has not been well studied. Judging from
the Ct values in our array analysis, however,
miR-222* was expressed at considerable levels in
FTC and this miRNA, as well as those of miR-221 and
miR-222, were dysregulated in metastatic MI-FTC compared to
non-metastatic MI-FTC (Table III).
Takano et al screened differentially expressed mRNAs in FTC
and follicular adenoma and found the decreased expression of
trefoil factor 3 mRNA to be a marker of FTCs (23). Foukakis et al generated the
mRNA expression profiles by PCR-based quantification followed by
logistic regression analysis and attempted to identify
transcriptional markers of malignancy in FTC (24). However, no mRNAs that distinguish
between metastatic and non-metastatic MI-FTCs have been reported so
far. Interestingly, Lu et al reported that miRNA profiles
are highly informative for the classification of poorly
differentiated tumors, the classification of which was inaccurate
by mRNA profiles (25). Likewise,
our findings suggest that miRNA profiles allow us to classify
MI-FTC into metastatic and non-metastatic groups, which have not
been previously distinguished, in terms of molecular pathology.
Molecular pathology examinations of miRNAs for the metastatic
potency of MI-FTC using FFPE surgical samples from the initial
operation should lead to recommendations for patients to strictly
monitor metastatic signs at intervals and if necessary undergo
additional operations (completion total thyroidectomy) and
radioiodine ablation therapy.
What functions do these miRNAs have? Recent studies
have reported that miR-221 and miR-222 regulate cell
growth and cell cycle progression by targeting cyclin-dependent
kinase inhibitor 1B (CDKN1B) and cyclin-dependent kinase
inhibitor 1C (CDKN1C) in several cancer cell lines (26–30).
This miRNA-mediated cell cycle regulation was also reported for PTC
(12,31). Considering that both FTC and PTC
are differentiated thyroid carcinomas originating from a common
cell type (the follicular cell), the upregulation of miR-221
and miR-222 in MI-FTC may lead to dysregulated cell cycle
progression by targeting CDKN1B and CDKN1C and
facilitates its hematogenous metastasis to lung and bone. Another
possibility is that the miR-221 gene family is involved in
metastatic processes by affecting cell migration and/or invasion.
In silico target prediction analysis revealed that these
miRNAs possibly target genes associated with matrix degradation.
For example, TargetScan 5.1 (www.targetscan.org/; Accessed May 10, 2011), a
representative target prediction program, predicts that both
miR-221 and miR-222 putatively target the mRNAs for
tissue inhibitor of metalloproteinase (TIMP)-2 and TIMP-3,
endogenous inhibitors of metalloproteinases (MMPs) such as MMP-2
and -9. Because these MMPs degrade matrices, particularly basement
membranes, to facilitate cancer cell invasion, miR-221 and
miR-222 possibly enhance cancer metastasis by downregulating
MMP inhibitors. MiR-10b has also been reported to have
malignancy and metastatic behavior; miR-10b is upregulated
in several cancer types (32–36).
Ma et al revealed that miR-10b initiates tumor
invasion and metastasis in cancer cells (32). In breast cancer cells, the
upregulation of miR-10b suppresses a direct target
Homeobox D10 (HOXD10), leading to induction of a
pro-metastatic gene, ras homolog gene family, member
C(32). Sun et al
demonstrated that in glioma cells, miR-10b promotes cancer
invasion by modulating tumor invasion factors MMP-14 and uPAR
expression via HOXD10(37).
It is likely that miR-10b acts as a promoter of metastasis
in breast cancer cells (38).
Upregulation of miR-92a, a miR-17-92a cluster-derived
miRNA, has also been reported in various cancers (39–45).
Recent report suggests a mechanism by which miR-92a promotes
metastasis (46). Considering
these metastasis-related miRNAs were upregulated in FTCs containing
metastatic MI-FTC and WI-FTC, the dysregulation of these miRNAs
could be closely related to the molecular mechanisms of metastasis
in FTCs. Further studies will be necessary to elucidate the
functions of the miR-221/222 cluster, miR-10b and
miR-92a in MI-FTC, especially, involvement in the molecular
pathogenesis of MI-FTC metastasis. In addition, controversy exists
involving the diagnostic criteria of well-differentiated thyroid
carcinomas (FTC and PTC). Mete and Asa recently reported that the
application of rigid criteria of vascular invasion (exclusion of
cases with vascular pseudoinvasion) provided a clinically relevant
prediction of distant metastasis in patients with PTC (47). It also remains to be investigated
whether the levels of miRNA expression correlate with angioinvasion
in well-differentiated thyroid carcinomas re-evaluated by the new
criteria based on true vascular invasion.
The most remarkable point of the present study is
that it was designed as a retrospective study to identify miRNAs
dysregulated in metastatic MI-FTC over non-metastatic MI-FTC, in
which we managed to collect specimens from patients who underwent
≥10 years of follow-up after the initial operation. Note that such
a comparative analysis has not been previously achieved because of
the difficulty in collecting FFPE samples and information from
patients with non-meta-static MI-FTC who have undergone
postoperative follow-up for such a long period. Logistic regression
analysis further supports the clinical significance of our findings
for surgical therapy in MI-FTC. However, the present and previous
studies on thyroid carcinoma constituted a relatively small
proportion of metastatic MI-FTC (23,24,48,49)
since metastatic MI-FTC is a relatively rare form of thyroid
cancer. The number of metastatic MI-FTC cases (in the total number
of MI-FTC cases) employed in the studies by Takano et
al(23), Foukakis et
al(24), Asari et
al(48) and Sugino et
al(49) was 1 case (15 cases),
4 cases (31 cases), 12 cases (127 cases) and 20 cases (111 cases),
respectively. In the present study, the number of metastatic MI-FTC
(in the total number of MI-FTC) is 12 out of 34 cases. It also
remains to be investigated whether the dysregulated miRNAs serve as
surrogate endpoint biomarkers for MI-FTC. Therefore, a large
multi-center case-control study of MI-FTC with a longer follow-up
period is necessary for evaluation the clinical significance of the
miRNAs identified in this study.
If patients are treated curatively, FTC and PTC
exhibit essentially identical 10-year cause-specific survival rates
(5,50–52).
In terms of diagnosis, PTC is readily diagnosed by fine-needle
aspiration cytology (FNAC). Conversely, FTC, especially MI-FTC, is
difficult to diagnose preoperatively by any modality, including
FNAC, because its routine cytological features are similar to those
of follicular adenoma (5,53). Ideally, the preoperative prediction
of the metastatic prognosis of MI-FTC, which could be achieved by
detecting miRNAs in FNAC samples, should be possible because the
upregulation of miR-221 and miR-222 has been recently
demonstrated in PTC from FNAC samples (14). However, further studies are needed
regarding the clinical applications for MI-FTC.
In conclusion, our miRNA analysis in FFPE samples
using LMD has provided important information regarding the
molecular pathology and novel therapeutic strategies for MI-FTC. In
this study, we found for the first time that the expression of
miRNAs belonging to the miR-221/222 cluster, miR-10b
and miR-92a were significantly upregulated in meta-static
MI-FTC. We conclude that miR-10b shows potential as a
prognostic factor for MI-FTC at an initial operation stage.
Acknowledgements
We thank Shinji Morita and Miyoko
Higuchi at Kuma Hospital and Takuji Kosuge and Yoshimi Hinohara at
Nippon Medical School for providing expert technical assistance.
This study was supported by Grants-in-Aids for Scientific Research
and Private University Strategic Research Foundation Support
Program (2008–2012) from the Ministry of Education, Culture,
Sports, Science and Technology/Japan Society for the Promotion of
Science, Japan.
References
|
1
|
Vinay K, Abul KA, Nelson F and Richard M:
Robbins: Basic Pathology. 8th edition. Saunders; Philadelphia, PA:
2007
|
|
2
|
LiVolsi VA: Pathology of thyroid disease.
Thyroid Disease: Endocrinology, Surgery, Nuclear Medicine and
Radiotherapy. Falk SA: Lippincott-Raven; Philadelphia, PA: pp.
127–175. 1997
|
|
3
|
DeLellis RA and Williams ED: Thyroid and
parathyroid tumours. World Health Organization Classification of
Tumours. Pathology and Genetics. Tumours of Endocrine Organs.
DeLellis RA, Lloyd RV, Heitz PU and Eng C: IARC Press; Lyon: pp.
51–56. 2004
|
|
4
|
Sobrinho-Simoes M, Albores-Saavedra J and
Tallini G: Poorly dirrerentiated carcinoma. World Health
Organization Classification of Tumours. Pathology and Genetics.
Tumours of Endocrine Organs. DeLellis RA, Lloyd RV, Heitz PU and
Eng C: IARC Press; Lyon: pp. 73–76. 2004
|
|
5
|
Ito Y, Hirokawa M, Higashiyama T, Takamura
Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K and Miyauchi A:
Prognosis and prognostic factors of follicular carcinoma in Japan:
importance of postoperative pathological examination. World J Surg.
31:1417–1424. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bartel DP: MicroRNAs: genomics,
biogenesis, mechanism and function. Cell. 116:281–297. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen CZ: MicroRNAs as oncogenes and tumor
suppressors. N Engl J Med. 353:1768–1771. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Iorio MV, Ferracin M, Liu CG, Veronese A,
Spizzo R, Sabbioni S, Magri E, Pedriali M, Fabbri M, Campiglio M,
Menard S, Palazzo JP, Rosenberg A, Musiani P, Volinia S, Nenci I,
Calin GA, Querzoli P, Neqrini M and Croce CM: MicroRNA gene
expression deregulation in human breast cancer. Cancer Res.
65:7065–7070. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Murakami Y, Yasuda T, Saigo K, Urashima T,
Toyoda H, Okanoue T and Shimotohno K: Comprehensive analysis of
microRNA expression patterns in hepatocellular carcinoma and
non-tumorous tissues. Oncogene. 25:2537–2545. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Calin GA, Ferracin M, Cimmino A, Di Leva
G, Shimizu M, Wojcik SE, Iorio MV, Visone R, Sever NI, Fabbri M,
Iuliano R, Palumbo T, Pichiorri F, Roldo C, Garzon R, Sevignani C,
Rassenti L, Alder H, Volnia S, Liu CG, Kipps TJ, Negrini M and
Croce CM: A microRNA signature associated with prognosis and
progression in chronic lymphocytic leukemia. N Engl J Med.
353:1793–1801. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yanaihara N, Caplen N, Bowman E, Seike M,
Kumamoto K, Yi M, Stephens RM, Okamoto A, Yokota J, Tanaka T, Calin
GA, Liu CG, Croce CM and Harris CC: Unique microRNA molecular
profiles in lung cancer diagnosis and prognosis. Cancer Cell.
9:189–198. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Visone R, Russo L, Pallante P, De Martino
I, Ferraro A, Leone V, Borbone E, Petrocca F, Alder H, Croce CM and
Fusco A: MicroRNAs(miR)-221 and miR-222, both overexpressed in
human thyroid papillary carcinomas, regulate p27Kip1
protein levels and cell cycle. Endocr Relat Cancer. 14:791–798.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pallante P, Visone R, Croce CM and Fusco
A: Deregulation of microRNA expression in follicular cell-derived
human thyroid carcinomas. Endocr Relat Cancer. 17:F91–F104. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mazeh H, Mizrahi I, Halle D, Ilyayev N,
Stojadinovic A, Trink B, Mitrani-Rosenbaum S, Roistacher M, Ariel
I, Eid A, Freund HR and Nissan A: Development of a microRNA-based
molecular assay for the detection of papillary thyroid carcinoma in
aspiration biopsy samples. Thyroid. 21:111–118. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hair JF Jr, Anderson RE, Tatham RL and
Black WC: Multivariate Data Analysis with Readings. 4th edition.
Prentice-Hall; Englewood Cliffs: 1995
|
|
16
|
Cohen J, Cohen P, West SG and Aiken LS:
Applied Multiple Regression/Correlation Analysis for the Behavioral
Sciences. 3rd edition. Lawrence Erlbaum Associates; Mahwah, NJ:
2003
|
|
17
|
Guthrie JL, Seah C, Brown S, Tang P,
Jamieson F and Drews SJ: Use of Bordetella pertussis BP3385 to
establish a cutoff value for an IS481-targeted real-time PCR assay.
J Clin Microbiol. 46:3798–3799. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xi Y, Nakajima G, Gavin E, Morris CG, Kudo
K, Hayashi K and Ju J: Systematic analysis of microRNA expression
of RNA extracted from fresh frozen and formalin-fixed
paraffin-embedded samples. RNA. 13:1668–1674. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cronin M, Pho M, Dutta D, Stephans JC,
Shak S, Kiefer MC, Esteban JM and Baker JB: Measurement of gene
expression in archival paraffin-embedded tissues: development and
performance of a 92-gene reverse transcriptase-polymerase chain
reaction assay. Am J Pathol. 164:35–42. 2004. View Article : Google Scholar
|
|
20
|
Masuda N, Ohnishi T, Kawamoto S, Monden M
and Okubo K: Analysis of chemical modification of RNA from
formalin-fixed samples and optimization of molecular biology
applications for such samples. Nucleic Acids Res. 27:4436–4443.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Srinivasan M, Sedmak D and Jewell S:
Effect of fixatives and tissue processing on the content and
integrity of nucleic acids. Am J Pathol. 161:1961–1971. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nikiforova MN, Tseng GC, Steward D, Diorio
D and Nikiforov YE: MicroRNA expression profiling of thyroid
tumors: biological significance and diagnostic utility. J Clin
Endocrinol Metab. 93:1600–1608. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takano T, Miyauchi A, Yoshida H, Kuma k
and Amino N: High-throughput differential screening of mRNAs by
serial analysis of gene expression: decreased expression of trefoil
factor 3 mRNA in thyroid follicular carcinomas. Br J Cancer.
90:1600–1605. 2004. View Article : Google Scholar
|
|
24
|
Foukakis T, Gusnanto A, Au AY, Höög A, Lui
WO, Larsson C, Wallin G and Zedenius J: A PCR-based expression
signature of malignancy in follicular thyroid tumors. Endocr Relat
Cancer. 14:381–391. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lu J, Getz G, Miska EA, Alvarz-Saavedra E,
Lamb J, Peck D, Sweet-Cordero A, Ebert BL, Mak RH, Ferrando AA,
Downing JR, Jacks T, Horvitz HR and Golub TR: MicroRNA expression
profiles classify human cancers. Nature. 435:834–838. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Galardi S, Mercatelli N, Giorda E,
Massalini S, Frajese GV, Ciafere SA and Farace MG: miR-221 and
miR-222 expression affects the proliferation potential of human
prostate carcinoma cell lines by targeting p27Kip1. J
Biol Chem. 282:23716–23724. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Miller TE, Ghoshal K, Ramaswamy B, Roy S,
Datta J, Shapiro CL, Jacob S and Majumder S: MicroRNA-221/222
confers tamoxifen resistance in breast cancer by targeting
p27Kip1. J Biol Chem. 283:29897–29903. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang C, Han L, Zhag A, Yang W, Zhou X, Pu
P, Du Y, Zeng H and Kang C: Global changes of mRNA expression
reveals an increased activity of the interferon-induced signal
transducer and activator of transcription (STAT) pathway by
repression of miR-221/222 in glioblastoma U251 cells. Int J Oncol.
36:1503–1512. 2010.
|
|
29
|
Le Sage C, Nagel R, Egan DA, Schrier M,
Mesman E, Mangiola A, Anile C, Maira G, Mercatelli N, Ciafre SA,
Farace MG and Agami R: Regulation of the p27(Kip1) tumor suppressor
by miR-221 and miR-222 promotes cancer cell proliferation. EMBO J.
26:3699–3708. 2007.PubMed/NCBI
|
|
30
|
Fornari F, Gramantieri L, Ferracin M,
Veronese A, Sabbiori S, Calin GA, Grazi GL, Giovannini C, Croce CM,
Bolondi L and Negrini M: MiR-221 controls CDKN1C/p57 and CDKN1B/p27
expression in human hepatocellular carcinoma. Oncogene.
27:5651–5661. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
He H, Jazdzewski K, Li W, Liyanarachchi S,
Nagy R, Volinia S, Calin GA, Liu CG, Franssila K, Suster S, Kloos
RT, Croce CM and de la Chapelle A: The role of microRNA genes in
papillary thyroid carcinoma. Proc Natl Acad Sci USA.
102:19075–19080. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ma L, Teruya-Feldstein J and Weinberg RA:
Tumour invasion and metastasis initiated by microRNA-10b in breast
cancer. Nature. 449:682–688. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tan HX, Wang Q, Chen LZ, Huang XH, Chen
JS, Fu XH, Cao LQ, Chen XL, Li W and Zhang LJ: MicroRNA-9 reduces
cell invasion and E-cadherin secretion in SK-Hep-1 cell. Med Oncol.
27:654–660. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bloomston M, Frankel WL, Petrocca F,
Volinia S, Alder H, Hagan JP, Liu CG, Bhatt D, Taccioli C and Croce
CM: MicroRNA expression patterns to differentiate pancreatic
adenocarcinoma from normal pancreas and chronic pancreatitis. JAMA.
297:1901–1908. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ciafre SA, Galardi S, Mangiola A, Ferracin
M, Liu CG, Sabatino G, Negrini M, Maira G, Croce CM and Farace MG:
Extensive modulation of a set of microRNAs in primary glioblastoma.
Biochem Biophys Res Commun. 334:1351–1358. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Huse JT, Brennan C, Hambardzumyan D, Wee
B, Pena J, Rouhanifard SH, Sohn-Lee C, le Sage C, Agami R, Tuschl T
and Holland EC: The PTEN-regulating microRNA miR-26a is amplified
in high-grade glioma and facilitates gliomagenesis in vivo. Genes
Dev. 23:1327–1337. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sun L, Yan W, Wang Y, Sun G, Luo H, Zhang
J, Wang X, You Y, Yang Z and Liu N: MicroRNA-10b induces glioma
cell invasion by modulating MMP-14 and uPAR expression via HOXD10.
Brain Res. 1389:9–18. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ma L and Weinberg RA: Micromanagers of
malignancy: role of microRNAs in regulating metastasis. Trends
Genet. 24:448–456. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ota A, Tagawa H, Karnan S, Tsuzuki S,
Karpas A, Kira S, Yoshida Y and Seto M: Identification and
characterization of a novel gene, C13orf25, as a target for
13q31-q32 amplification in malignant lymphoma. Cancer Res.
64:3087–3095. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hayashita Y, Osada H, Tatematsu Y, Yamada
H, Yanagisawa K, Tomida S, Yatabe Y, Kawahara K, Sekido Y and
Takahashi T: A polycistronic microRNA cluster, miR-17-92, is
overexpressed in human lung cancers and enhances cell
proliferation. Cancer Res. 65:9628–9632. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Monzo M, Navarro A, Bandres E, Artells R,
Moreno I, Gel B, Ibeas R, Moreno J, Martinez F, Diaz T, Martinez A,
Balagué O and Garcia-Foncillas J: Overlapping expression of
microRNAs in human embryonic colon and colorectal cancer. Cell Res.
18:823–833. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Diosdado B, van de Wiel MA, Terhaar Sive
Droste JS, Mongera S, Postma C, Meijerink W J, Carvalho B and
Meijer GA: MiR-17-92 cluster is associated with 13q gain and c-myc
expression during colorectal adenoma to adenocarcinoma progression.
Br J Cancer. 101:707–714. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Connolly E, Melegari M, Landgraf P,
Tchaikovskaya T, Tennant BC, Slagle BL, Rogler LE, Zavolan M,
Tuschl T and Rogler CE: Elevated expression of the miR-17-92
polycistron and miR-21 in hepadnavirus-associated hepatocellular
carcinoma contributes to the malignant phenotype. Am J Pathol.
173:856–864. 2008. View Article : Google Scholar
|
|
44
|
Chen HC, Chen GH, Chen Y H, Liao WL, Liu
CY, Chang KP, Chang YS and Chen SJ: MicroRNA deregulation and
pathway alterations in nasopharyngeal carcinoma. Br J Cancer.
100:1002–1011. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Takakura S, Mitsutake N, Nakashima M,
Namba H, Saenko VA, Rogounovitch TI, Nakazawa Y, Hayashi T, Ohtsuru
A and Yamashita S: Oncogenic role of miR-17-92 cluster in
anaplastic thyroid cancer cells. Cancer Sci. 99:147–154. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chen ZL, Zhao XH, Wang JW, Li BZ, Wang Z,
Sun J, Tan FW, Ding DP, Xu XH, Zhou F, Tan XG, Hang J, Shi SS, Feng
XL and He J: microRNA-92a promotes lymph node metastasis of human
esophageal squamous cell carcinoma via E-cadherin. J Biol Chem.
25:10725–10734. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Mete O and Asa SL: Pathological definition
and clinical significance of vascular invasion in thyroid
carcinomas of follicular epithelial derivation. Mod Pathol.
24:1545–1552. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Asari R, Koperek O, Scheuba C, Riss P,
Kaserer K, Hoffmann M and Niederle B: Follicular thyroid carcinoma
in an iodine-replete endemic goiter region: a prospectively
collected, retrospectively analyzed clinical trial. Ann Surg.
249:1023–1031. 2009. View Article : Google Scholar
|
|
49
|
Sugino K and Ito K, Nagahama M, Kitagawa
W, Shibuya H, Ohkuwa K, Yano Y, Uruno T, Akaishi J, Kameyama K and
Ito K: Prognosis and prognostic factors for distant metastases and
tumor mortality in follicular thyroid carcinoma. Thyroid.
21:751–757. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Mazzaferri EL and Jhiang SM: Long-term
impact of initial surgical and medical therapy on papillary and
follicular thyroid cancer. Am J Med. 97:418–428. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
van Heerden JA, Hay ID, Goellner JR,
Salomao D, Ebersold JR, Bergstralh EJ and Grant CS: Follicular
thyroid carcinoma with capsular invasion alone: a nonthreatening
malignancy. Surgery. 112:1130–1138. 1992.PubMed/NCBI
|
|
52
|
Thompson LD, Wieneke JA, Paal E, Frommelt
RA, Adair CF and Heffess CS: A clinicopathologic study of minimally
invasive follicular carcinoma of the thyroid gland with a review of
the English literature. Cancer. 91:505–524. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Mazafferi EL and Kloos RT: Carcinoma of
follicular epithelium: radioiodine and other treatments and
outcomes. The Thyroid. Braverman LE and Utiger RD: Lippincott
Williams & Wilkins; Philadelphia, PA: pp. 934–966. 2005
|