Introduction
Pancreatic cancer is the 4th leading cause of cancer
deaths in the United States (1).
Conventional therapies such as surgery, radiation, chemotherapy or
a combination of these fail to substantially alter the course of
pancreatic cancer, and the prognosis for these patients remains
extremely poor with a 5-year survival of only 5% (1) and a median survival of <6 months
that has remained unchanged for the last three decades (2,3). The
long-term goal of our research is to develop an effective strategy
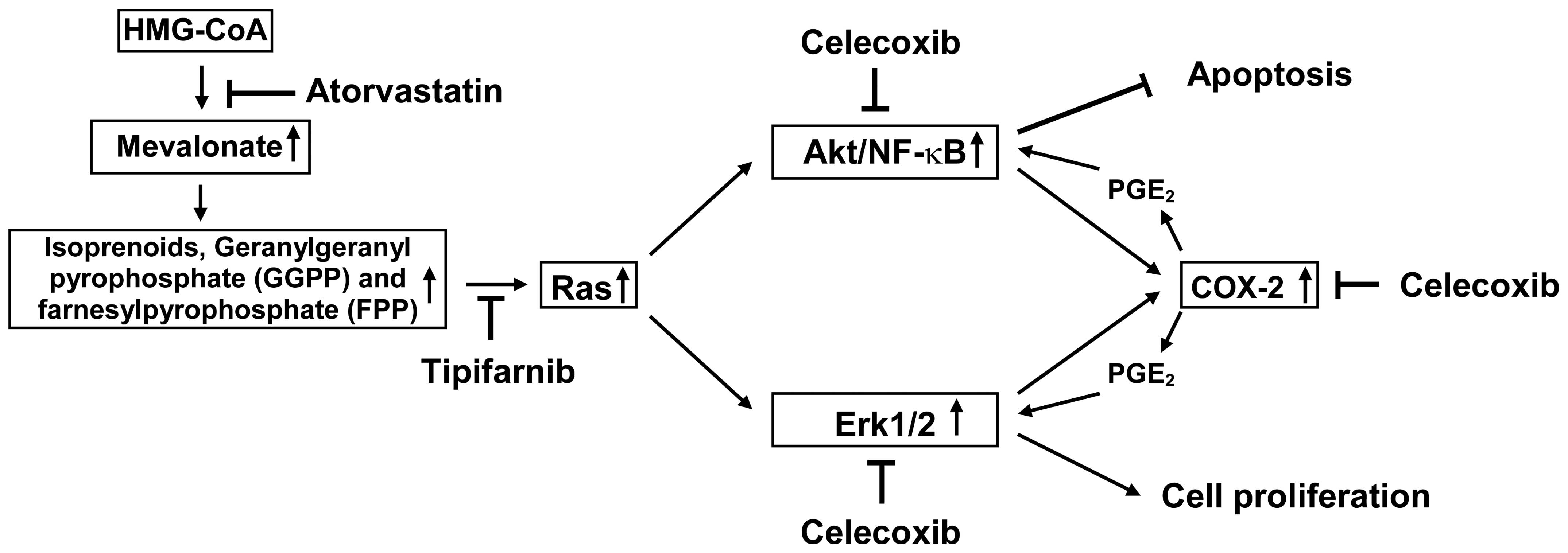
for inhibiting the progression and growth of pancreatic cancer. Ras
mutation and overexpression of cyclooxygenase-2 (COX-2) are present
in the majority of pancreatic cancer patients (2–5). Ras
mutation results in constitutive activation of Erk1/2 and PI3K/Akt
pathways leading to increased cell proliferation and decreased
apoptosis in pancreatic cancer cells (6). Overexpression of COX-2 results in
increased production of prostaglandins and also the activation of
Erk1/2 and Akt (7,8). An approach for inhibiting the
progression and growth of pancreatic cancer is the simultaneous use
of agents that inhibit the function of both Ras and COX-2. A
combination of these agents may synergize to suppress pancreatic
cancer growth and stimulate apoptosis. We hypothesize that
simultaneous inhibition of HMG-CoA reductase with atorvastatin
(Lipitor), inhibition of farnesyl transferase with tipifarnib
(Zarnestra) and inhibition of COX-2 with celecoxib (Celebrex) will
synergistically inhibit downstream readouts of activated ras and
elevated COX-2 (activated Akt/NFκB and activated Erk1/2) thereby
inhibiting proliferation and stimulating apoptosis. This hypothesis
is illustrated in Fig. 1. The
drugs chosen for this study are relatively non-toxic, work by
different mechanisms and can readily be utilized for a clinical
trial. Atorvastatin and celecoxib are in broad clinical use and
tipifarnib is a farnesyl transferase inhibitor that has been
extensively tested in clinical trials (9–12).
To the best of our knowledge the simultaneous targeting of Ras and
COX-2 pathways in pancreatic cancer growth is novel.
To test our hypothesis that simultaneous inhibition
of the Ras and COX-2 pathways will potently inhibit the growth and
induce apoptosis in pancreatic cancer cells in vitro and
in vivo, we investigated the effects of atorvastatin,
celecoxib and tipifarnib alone or in combination on the growth and
apoptosis of human pancreatic cancer Panc-1 cells cultured in
vitro or grown as xenograft tumors in SCID mice. We found that
treatment of Panc-1 cells with a combination of atorvastatin,
celecoxib and tipifarnib had a stronger inhibitory effect on
proliferation and a stronger stimulatory effect on apoptosis than
any of the drugs alone or for any combination of two drugs. We also
found that treatment of tumor-bearing SCID mice with a combination
of atorvastatin, celecoxib and tipifarnib had a stronger inhibitory
effect on the growth of Panc-1 tumors in these mice than for any of
the three drugs alone or for any combination of two drugs.
Materials and methods
Cell culture and reagents
Panc-1 cells were obtained from Dr Pamela Crowell
(Indiana University - Purdue University Indianapolis, Indianapolis,
IN). Luciferase-expressing Panc-1 cells were obtained from Dr
Bharart Aggarwal (The University of Texas M.D. Anderson Cancer
Center, Houston, TX). Atorvastatin and celecoxib were provided by
the National Cancer Institute’s Repository. Tipifarnib was provided
by Johnson & Johnson Pharmaceutical Research and Development
(Raritan, NJ). Propylene glycol, polysorbate 80, benzyl alcohol,
ethanol and DMSO were purchased from Sigma (St. Louis, MO).
Matrigel was obtained from BD Biosciences (Bedford, MA). Dulbecco’s
modified Eagle’s medium (DMEM) tissue culture medium,
penicillin-streptomycin, L-glutamine and fetal bovine serum (FBS)
were from Gibco (Grand Island, NY). Panc-1 cells were maintained in
DMEM culture medium containing 10% FBS that was supplemented with
penicillin (100 U/ml)-streptomycin (100 μg/ml) and
L-glutamine (300 μg/ml). Cultured cells were grown at 37°C
in a humidified atmosphere of 5% CO2 and were passaged
twice a week. Panc-1 cells were initially seeded at a density of
0.2×105 cells/ml in 35-mm tissue culture dishes (2
ml/dish) for assays of proliferation and apoptosis, and seeded at a
density of 1×105 cells/ml of medium in 100 mm culture
dishes (10 ml/dish) for the western blot analysis. Atorvastatin,
celecoxib and tipifarnib were dissolved in DMSO and the final
concentration of DMSO in all experiments was 0.2%.
Determination of the number of viable
cells
The number of viable cells after each treatment was
determined using a hemacytometer under a light microscope (Nikon
Optiphot, Nikon, Tokyo, Japan). Cell viability was determined by
the trypan blue exclusion assay, which was done by mixing 80
μl of cell suspension and 20 μl of 0.4% trypan blue
solution for 2 min. Blue cells were counted as dead cells and the
cells that did not absorb dye were counted as live cells.
Morphological assessment of apoptotic
cells
Apoptosis was determined by morphological assessment
in cells stained with propidium iodide (13). Briefly, cytospin slides were
prepared after each experiment and cells were fixed with
acetone/methanol (1:1) for 10 min at room temperature, followed by
10 min with propidium iodide staining (1 μg/ml in PBS) and
analyzed using a fluorescence microscope (Nikon Eclipse TE200,
Nikon). Apoptotic cells were identified by classical morphological
features including nuclear condensation, cell shrinkage, and
formation of apoptotic bodies (13). At least 200 cells were counted in
each sample and the percentage of apoptotic cells is presented.
Western blot analysis
After treatment, Panc-1 cells were washed with
ice-cold PBS and lysed with 800 μl of lysis buffer (10 mM
Tris-HCl, pH 7.4, 50 mM sodium chloride, 30 mM sodium
pyrophosphate, 50 mM sodium fluoride, 100 μM sodium
orthovandate, 2 mM iodoacetic acid, 5 mM ZnCl2, 1 mM
phenylmethylsulfonyl fluoride and 0.5% Triton X-100). The
homogenates were centrifuged at 12,000 x g for 15 min at 4°C. The
protein concentration of whole cell lysates was determined with a
Bio-Rad protein assay kit (Bio-Rad, Hercules, CA). Equal amounts
(20 μg) of protein were then resolved on a 10% Criterion
Precast Gel (Bio-Rad) and transferred to a PVDF membrane. The
membrane was then probed with anti-phosphorylated Erk1/2 and Akt
primary antibodies (Cell Signaling Technology, Beverly, MA). After
hybridization with primary antibody, the membrane was washed with
Tris-buffered saline three times, then incubated with secondary
antibodies conjugated with infrared-dye (Cell Signaling Technology)
and washed with Tris-buffered saline three times. Labeled proteins
were visualized using the Odyssey infrared imaging system (LI-COR
Biosciences, Lincoln, NE). The extent of protein loading was
determined by blotting for β-actin.
Subcutaneous and orthotopic xenograft
Panc-1 tumors in immunodeficient mice
Female severe combined immunodeficient (SCID) mice
(6–7 weeks old) were obtained from Taconic Farms Inc (Germantown,
NY). The animals were housed in sterile filter-capped microisolator
cages and provided with sterilized food and water. For subcutaneous
xenograft tumors, pancreatic cancer Panc-1 cells (2×106
cells/0.1 ml/mouse) suspended in 50% Matrigel (Collaborative
Research, Bedford, MA) in DMEM medium were injected subcutaneously
into the right flank of the mice. After 4–6 weeks, mice with Panc-1
tumors (0.6–1.0 cm wide and 0.6–1.0 cm long) were injected with
vehicle (5 μl/g body weight), atorvastatin (2 μg/g),
celecoxib (2 μg/g), tipifarnib (0.8 μg/g),
atorvastatin (2 μg/g) + celecoxib (2 μg/g),
atorvastatin (2 μg/g) + tipifarnib (0.8 μg/g),
celecoxib (2 μg/g) + tipifarnib (0.8 μg/g) or
atorvastatin (2 μg/g) + celecoxib (2 μg/g) +
tipifarnib (0.8 μg/g) once a day for 30 days. In all
experiments, animals in the different experimental groups received
the same amount of vehicle (5 μl/g body weight) which
consisted of propylene glycol, polysorbate 80, benzyl alcohol,
ethanol and water (40:0.5:1:10:48.5) (14). Tumor size (length x width) and body
weight were measured every third day. For the orthotopic xenograft
experiment, luciferase-expressing Panc-1 cells (15) harvested from subconfluent cultures
were injected into the pancreas of female SCID mice. In this
procedure, mice were anesthetized with ketamine-xylazine solution,
a small left abdominal flank incision was made, and Panc-1 cells
(1×106) in 100 μl DMEM medium were injected into
the subcapsular region of the pancreas using a 27-gauge needle. To
prevent leakage, a cotton swab was held for 1 min over the site of
injection. The abdominal wound was closed with wound clips
(Braintree Scientific, Inc., Braintree, MA). Three weeks after
injection of tumor cells, the mice were randomized into two groups
based on the IVIS imaging. The control group received i.p.
injections with vehicle (5 μl/g body weight) and the
combination treatment group received i.p. injections with
atorvastatin (2 μg/g) + celecoxib (2 μg/g) +
tipifarnib (0.8 μg/g) once a day for 28 days. Each group had
4 mice. For the IVIS imaging, the mice were anesthetized with
isoflurane and injected i.p. with luciferin. The mice were then
placed into the imaging chamber of the IVIS imaging system (Xenogen
Corporation, San Diego, CA) and a bioluminescence image was taken.
All animal experiments were carried out under an Institutional
Animal Care and Use Committee (IACUC)-approved protocol.
Statistical analyses
The analyses of percentage of initial tumor size
were based on a repeated measurement model (16). The treatment effects were assessed
by comparing the rates of change over time between treatment groups
(i.e. comparing the slopes and/or quadratic trends between
treatment groups). Heterogeneous autoregressive correlation
structure was used to account for the within-mice correlation. The
analysis of variance (ANOVA) model with Tukey-Kramer adjustment
(17) was used for the comparison
of tumor size and body weight among different treatment groups at
the end of the treatment.
Results
Effects of atorvastatin, celecoxib and
tipifarnib on the growth and apoptosis of cultured Panc-1
cells
Dose-response studies on the effects of
atorvastatin, celecoxib or tipifarnib on the growth and apoptosis
of cultured Panc-1 cells using our previously utilized methodology
(13,14,18)
are shown in Fig. 2. The
concentration of atorvastatin, celecoxib or tipifarnib alone to
achieve 50% inhibition of the growth of Panc-1 cells was 5, 8 and
0.5 μM, respectively (Fig.
2A) whereas a combination of the three drugs at 1, 1 and 0.1
μM, respectively, also inhibited Panc-1 growth by ∼50%
(Table I). Treatment of Panc-1
cells with a combination of the 3 drugs had a stronger inhibitory
effect on proliferation and a stronger stimulatory effect on
apoptosis than the individual drugs alone or for any combination of
two drugs (Table I).
 | Table I.Effects of atorvastatin, celecoxib
and tipifarnib alone or in combination on the growth and apoptosis
of Panc-1 cells. |
Table I.
Effects of atorvastatin, celecoxib
and tipifarnib alone or in combination on the growth and apoptosis
of Panc-1 cells.
| Treatment | Viable cells (% of
control) | Apoptosis (% of
cells) |
|---|
| Control | 100 | 1.5±0.5 |
| Atorvastatin (1
μM) | 91.1±2.3 | 4.3±0.5 |
| Celecoxib (1
μM) | 93.4±1.6 | 3.8±0.6 |
| Tipifarnib (0.1
μM) | 90.3±1.1 | 5.6±0.4 |
| Atorvastatin (1
μM) + celecoxib (1 μM) | 79.7±6.9 | 8.8±1.1 |
| Atorvastatin (1
μM) + tipifarnib (0.1 μM) | 80.0±2.3 | 6.7±0.2 |
| Celecoxib (1
μM) + tipifarnib (0.1 μM) | 83.7±2.8 | 6.3±0.8 |
| Atorvastatin (1
μM) + celecoxib (1 μM) + tipifarnib (0.1
μM) | 49.9±5.2 | 20.5±3.1 |
Effects of atorvastatin, celecoxib and
tipifarnib on the levels of activated Akt and Erk1/2 in cultured
Panc-1 cells
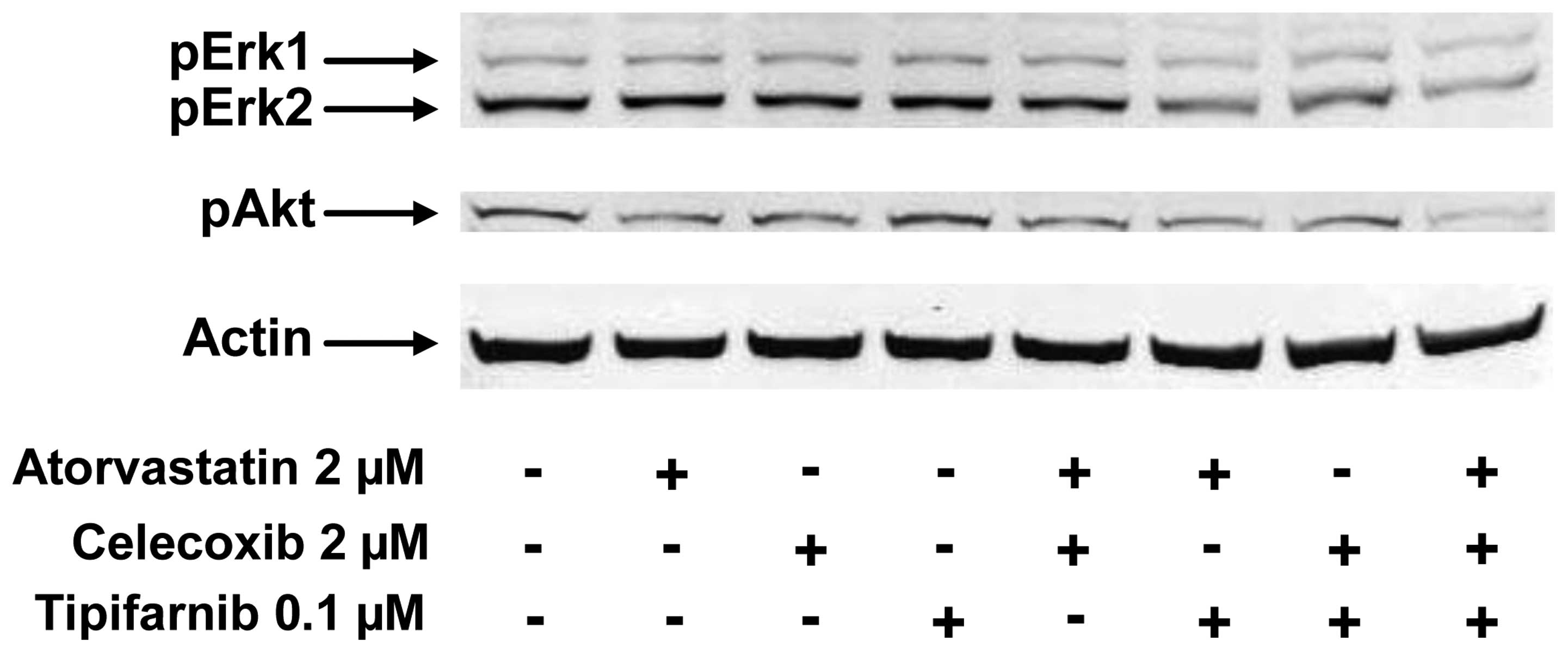
The levels of activated Akt and Erk1/2 in Panc-1
cells were evaluated by western blot analysis using
anti-phospho-Akt (pAkt) and anti-phospho-Erk1/2 (pErk1/2)
antibodies (both from Cell Signaling Technology). In these
experiments, Panc-1 cells were treated with atorvastatin (2
μM), celecoxib (2 μM) or tipifarnib (0.1 μM)
alone or in combination for 24 h and analyzed by western blot
analysis. As shown in Fig. 3,
treatment of Panc-1 cells with each drug alone or any combination
of two drugs for 24 h had little or no effect on the level of pAkt
in the cells, but the combination of atorvastatin, celecoxib and
tipifarnib caused a strong decrease in the level of pAkt (Fig. 3). Treatment of Panc-1 cells with
each drug alone or with a combination of atorvastatin and celecoxib
had little or no effect on the level of pErk1/2 in the cells
(Fig. 3). Treatment of Panc-1
cells with atorvastatin + tipifarnib or celecoxib + tipifarnib
resulted in modestly decreased pErk1/2 in the cells while a
combination of atorvastatin, celecoxib and tipifarnib caused a much
stronger decrease in pErk1/2 (Fig.
3).
Effects of i.p. injections of
atorvastatin, celecoxib and tipifarnib alone or in combination on
the growth of Panc-1 xenograft tumors in immunodeficient mice
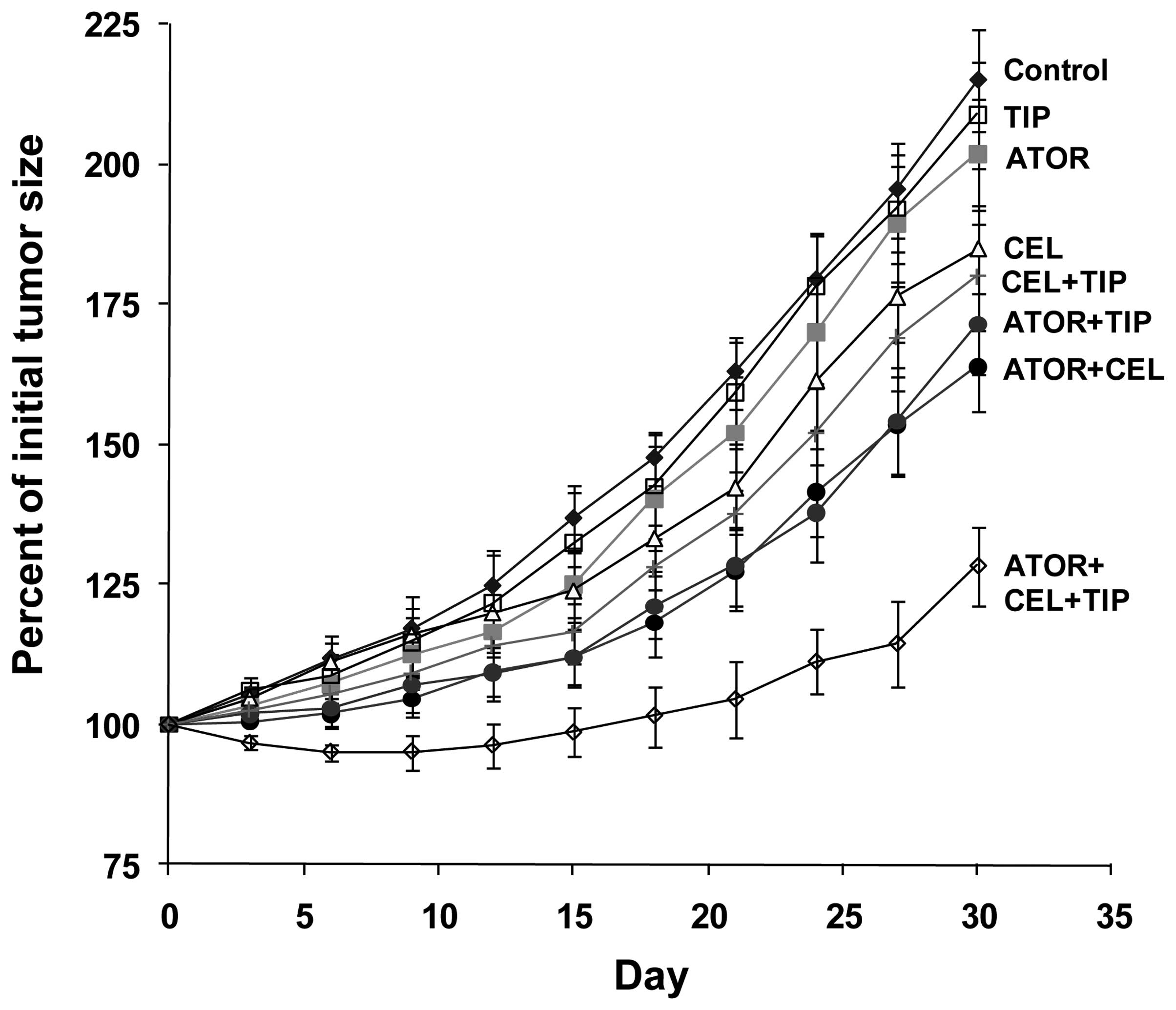
Female SCID mice with subcutaneous Panc-1 tumors
measuring 0.5–1.0 cm in length and 0.5–1.0 cm in width were
injected i.p. with celecoxib (2 μg/g body weight/day),
atorvastatin (2 μg/g body weight/day) or tipifarnib (0.8
μg/g body weight/day) alone or in combination. The
combination of celecoxib, atorvastatin and tipifarnib had a strong
inhibitory effect on tumor growth, whereas injection of tipifarnib
or atorvastatin alone was inactive and celecoxib alone or celecoxib
plus tipifarnib had only a small inhibitory effect on tumor growth,
and administration of atorvastatin plus celecoxib or atorvastatin
plus tipifarnib had a moderate inhibitory effect on tumor growth
(Fig. 4). Quadratic trends of
tumor growth were similar for all groups. The linear trends in
tumor growth for all the treatment groups were significantly
different from the vehicle control group (p≤0.0021) except for the
atorvastatin group and tipifarnib group. The linear trends for the
atorvastatin group and tipifarnib group were not significantly
different from the control (p-values were 0.1294 and 0.4996,
respectively). The linear trend in tumor growth for the
atorvastatin + celecoxib + tipifarnib group was significantly
different from that for any other group (p≤0.0034). The strong
inhibitory effect of the administration of a combination of
atorvastatin, celecoxib and tipifarnib on tumor growth lasted for
∼4 weeks followed by a partial restoration of tumor growth
(Fig. 4). At the end of the study
when the animals were sacrificed, the mean ± SE for the percent of
initial body weight was 92.2±2.0% for the vehicle treated control
group, 92.9±2.3% for the atorvastatin group, 87.8±2.5% for the
celecoxib group, 90.7±1.3% for the tipifarnib group, 90.0±2.1% for
the atorvastatin + celecoxib group, 86.3±2.7% for the atorvastatin
+ tipifarnib group, 90.9±1.4% for the celecoxib + tipifarnib group
and 89.3±1.9% for the atorvastatin + celecoxib + tipifarnib group.
Statistical analysis using ANOVA with the Tukey-Kramer multiple
comparison test showed that the difference in the percent of
initial body weight between the control group and any of the
treatment groups was not statistically significant (p>0.05).
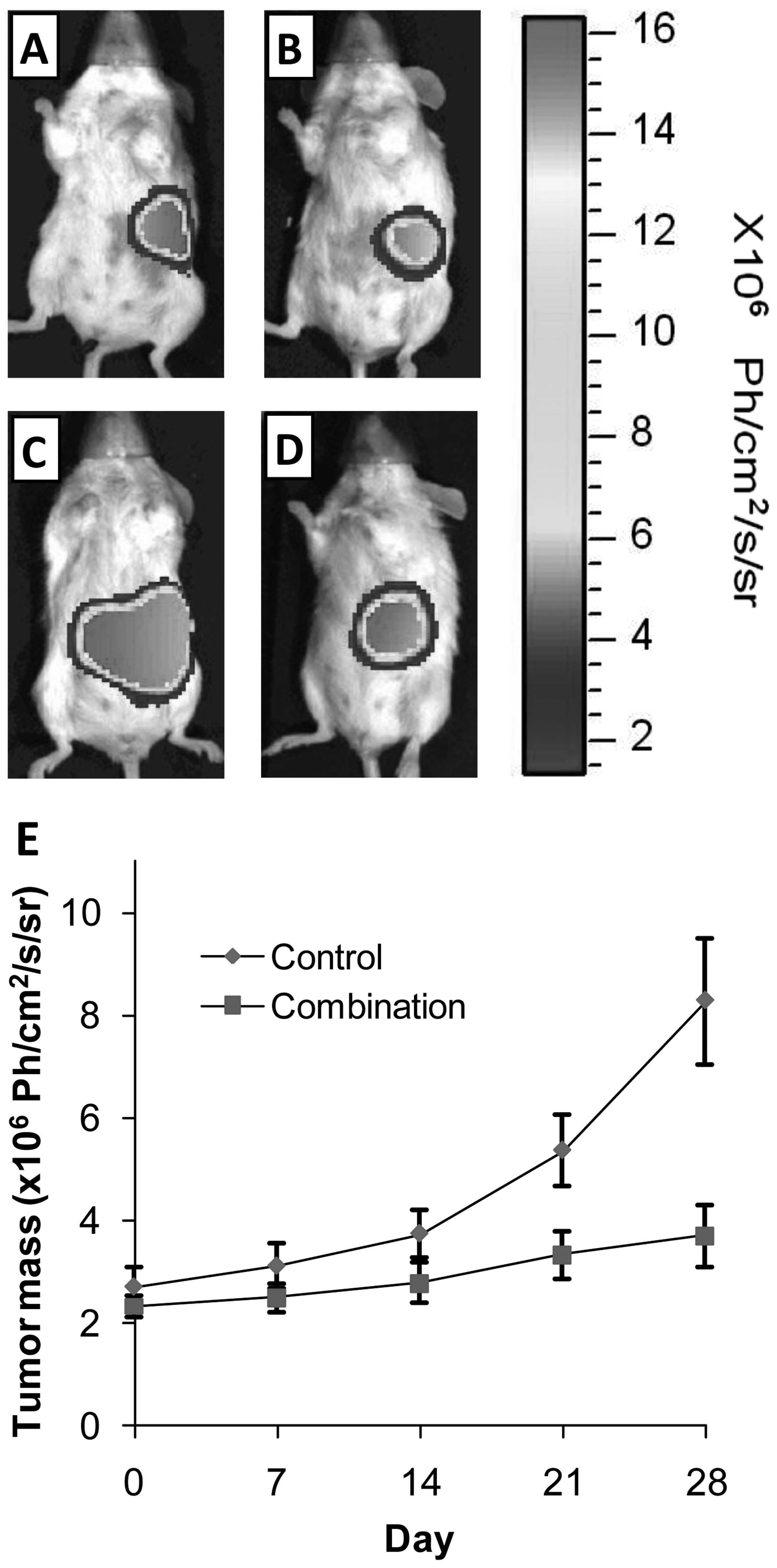
In an additional experiment, we determined the
effect of atorvastatin, celecoxib and tipifarnib in combination on
the growth of orthotopic Panc-1 xenograft tumors in SCID mice. As
shown in Fig. 5, treatment of the
mice with daily i.p. injections of atorvastatin (2 μg/g body
weight/day) + celecoxib (2 μg/g body weight/day) +
tipifarnib (0.8 μg/g body weight/day) strongly inhibited the
growth of orthotopic Panc-1 xenograft tumors for the duration of
the 28-day study. Statistical analysis using the Student’s t-test
showed that the difference in tumor size between the control group
and the combination treatment group at the end of the study was
statistically significant (p<0.01). The difference in the
percent of initial body weight between the control group and the
combination treatment group was not statistically significant
(Student’s t-test; p>0.05).
Discussion
In the present study, we showed that daily i.p.
injections of SCID mice with atorvastatin, celecoxib and tipifarnib
in combination had a stronger inhibitory effect on the growth of
Panc-1 xenograft tumors than atorvastatin, celecoxib or tipifarnib
used alone or for any combination of two drugs (Fig. 4). Although the triple drug
combination had a strong inhibitory effect on tumor growth, there
was no effect on body weight. We also found that atorvastatin,
celecoxib and tipifarnib in combination inhibited the growth,
induced apoptosis and decreased phosphorylation of Akt and Erk1/2
in cultured Panc-1 cells (Figs. 2
and 3). To the best of our
knowledge, this is the first report on the combined inhibitory
effect of atorvastatin, celecoxib and tipifarnib on the growth of
pancreatic cancer cells cultured in vitro or grown as
xenograft tumors in immunodeficient mice.
Tipifarnib is a selective non-peptidomimetic
inhibitor of farnesyltransferase. Preclinical studies demonstrated
that tipifarnib competitively inhibits farnesylation of K-ras
peptides at nanomolar concentrations. Tipifarnib also inhibits
proliferation of pancreatic cancer cells cultured in vitro
and grown as xenograft tumors in immunodeficient mice (19). However, the results of clinical
studies showed that tipifarnib did not exhibit single-agent
antitumor activity in patients with previously untreated metastatic
pancreatic cancer (12,20,21).
A possible explanation for these negative results of clinical
trials is that Ras can be geranylgeranylated, an alternative
lipidation that can substitute for farnesylation (22), and this reaction may not be
inhibited by farnesyltransferase inhibitors. Therefore, agents such
as 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) reductase inhibitors
that can reduce both geranylgeranyl pyrophosphate (GGPP) and
farnesylpyrophosphate (FPP) may enhance the effectiveness of
tipifarnib. Atorvastatin is a member of the statin family of drugs
that inhibit HMG-CoA reductase, a rate limiting enzyme in
cholesterol biosynthesis, and this drug is used clinically as a
safe and effective agent for the control of hypercholesterolemia
(23). HMG-CoA reductase
inhibition leads to reduced synthesis of isoprenoids, GGPP and FPP
(24,25). In the present study, we found that
a combination of atorvastatin and tipifarnib decreased the level of
pErk1/2 while atorvastatin or tipifarnib alone had little or no
effect on the level of pErk1/2. Although further studies are needed
to determine the inhibitory effect of atorvastatin and tipifarnib
on activation of Ras protein, our results indicated that a
combination of these two drugs more potently inhibited the Ras
down-stream effector Erk1/2 than either drug alone.
Celecoxib, a selective COX-2 inhibitor, has been
shown previously to inhibit the growth of human pancreatic cancer
cell lines (26,27). Recent studies showed that celecoxib
inhibited angiogenesis, tumor growth and metastasis in pancreatic
xenograft tumors (28,29), and celecoxib also inhibited
pancreas cancer formation in a COX-2 overexpressing mouse (30). Although treatment with celecoxib
alone did not influence tumor growth in tumor-bearing mice
(30), the possibility that a
combination of celecoxib, atorvastatin and tipifarnib will inhibit
pancreas tumor growth in this genetic model of pancreas cancer has
not yet been explored. The present study provides evidence that the
combination of celecoxib, atorvastatin and tipifarnib have a strong
inhibitory effect on the growth of both subcutaneous and orthotopic
Panc-1 xenograft tumors in SCID mice.
Although loss of effectiveness of the triple drug
combination after 4 weeks of inhibition of tumor growth is
suggested by the last data point in Fig. 4, no loss of effectiveness was
observed during a 4 week treatment interval in a second study with
an orthotopic pancreas tumor model (Fig. 5). Additional studies are needed to
strengthen data on a possible loss of effectiveness of the triple
drug combination on tumor growth with continued therapy beyond 4
weeks. The possible loss of effectiveness of drug treatment after 4
weeks of therapy could be because chronic drug treatment (or
vehicle) stimulated metabolic inactivation of the drugs (enzyme
induction) or because the tumor cells became intrinsically
resistant to drug administration. In a separate study in male SCID
mice, feeding a combination of celecoxib (0.05% in diet) and
atorvastatin (0.02% in diet) for 2 weeks resulted in substantially
lower serum levels of atorvastatin and its metabolites than in the
serum of mice fed atorvastatin alone (unpublished observations).
These results suggest that increasing the dose of atorvastatin
after 2–3 weeks of treatment may prevent the loss of effectiveness
at late time intervals. Additional studies are needed to determine
whether treating the mice with atorvastatin, celecoxib and
tipifarnib stimulates the hepatic metabolism of these drugs to
inactive products or whether tumor cells become intrinsically
resistant to drug treatment. The strong inhibitory effect of a
combination of atorvastatin, celecoxib and tipifarnib (relatively
non-toxic drugs) on the growth of pancreas tumors provide a
rationale for a clinical trial to determine the effectiveness of
the simultaneous administration of atorvastatin, celecoxib and
tipifarnib possibly in combination with gemcitabine on the growth
of pancreas tumors in pancreas cancer patients or to determine
whether the triple drug combination will prevent the recurrence of
pancreas cancer in patients who have undergone surgery by the
Whipple procedure to remove their pancreas cancer. It is well-known
that patients who have had surgical removal of their pancreas tumor
by the Whipple procedure have a high risk for recurrence of
pancreas cancer (31,32).
Acknowledgements
The present study was supported by
funds from the Chinese National Science Foundation Grants 81272452
and 21272043, and the Rutgers Cancer Institute of New Jersey grant
CCSG P30-CA072720 RSD. The authors thank Ms. Florence Florek and
Annette Dionisio for their excellent help in the preparation of
this manuscript.
References
|
1.
|
Jemal A, Siegel R, Ward E, et al: Cancer
Statistics 2009. CA Cancer J Clin. 59:225–249. 2009. View Article : Google Scholar
|
|
2.
|
Almoguera C, Shibata D, Forrester K, et
al: Most human carcinomas of the exocrine pancreas contain mutant
c-K-ras genes. Cell. 53:549–554. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Kokawa A, Kondo H, Gotoda T, et al:
Increased expression of cyclooxygenase-2 in human pancreatic
neoplasms and potential for chemoprevention by cyclooxygenase
inhibitors. Cancer. 91:333–338. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Tucker ON, Dannenberg AJ, Yang EK, et al:
Cyclooxygenase-2 expression is upregulated in human pancreatic
cancer. Cancer Res. 59:987–990. 1999.PubMed/NCBI
|
|
5.
|
Okami J, Yamamoto H, Fujiwara Y, et al:
Overexpression of COX-2 in carcinoma of the pancreas. Clin Cancer
Res. 5:2018–2024. 1999.PubMed/NCBI
|
|
6.
|
Osada M, Tolkacheva T, Li W, et al:
Differential roles of Akt, Rac, and Ral in R-Ras-mediated cellular
transformation, adhesion, and survival. Mol Cell Biol.
19:6333–6344. 1999.
|
|
7.
|
Krysan K, Reckamp KL, Dalwadi H, et al:
Prostaglandin E2 activates mitogen-activated protein kinase/Erk
pathway signaling and cell proliferation in non-small cell lung
cancer cells in an epidermal growth factor receptor-independent
manner. Cancer Res. 65:6275–6281. 2005. View Article : Google Scholar
|
|
8.
|
Han W and Ca T: Cyclooxygenase-2-derived
prostaglandin E2 promotes human cholangiocarcinoma cell growth and
invasion through EP1 receptor-mediated activation of the epidermal
growth factor receptor and Akt. J Biol Chem. 280:24053–24063. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Sparano JA, Moulder S, Kazi A, et al:
Phase II trial of tipifarnib plus neoadjuvant
doxorubicin-cyclophosphamide in patients with clinical stage
IIB-IIIC breast cancer. Clin Cancer Res. 15:2942–2948. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Lancet JE, Gojo I, Gotlib J, et al: A
phase 2 study of the farnesyltransferase inhibitor tipifarnib in
poor-risk and elderly patients with previously untreated acute
myelogenous leukemia. Blood. 109:1387–1394. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Moller I, Blum S, Gattermann N, Haas R,
Habersang U and Kuendgen A: Repeated responses of an elderly
patient with high-risk myelodysplastic syndrome to sequential
therapy with tipifarnib, 5-azacitidine, and dectabine. Ann Hematol.
88:1141–1144. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Van Cutsem E, van de Velde H, Karasek P,
et al: Phase III trial of gemcitabine plus tipifarnib compared with
gemcitabine plus placebo in advanced pancreatic cancer. J Clin
Oncol. 22:1430–1438. 2004.PubMed/NCBI
|
|
13.
|
Hansson A, Marin YE, Suh J, et al:
Enhancement of TPA-induced growth inhibition and apoptosis in
myeloid leukemia cells by BAY 11-7082 an NF-κB inhibitor. Int J
Oncol. 27:941–948. 2005.PubMed/NCBI
|
|
14.
|
Zheng X, Chang RL, Cui XX, et al:
Inhibitory effect of 12-O-tetradecanoylphorbol-13-acetate alone or
in combination with all-trans-retinoic acid on the growth of LNCaP
prostate tumors in immunodeficient mice. Cancer Res. 64:1811–1820.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Kunnumakkara AB, Krishnan S, Diagaradjane
P, Gelovani J and Aggarwal BB: Curcumin potentiates antitumor
activity of gemcitabine in an orthotopic model of pancreatic cancer
through suppression of proliferation, angiogenesis, and inhibition
of nuclear factor-kappaB-regulated gene products. Cancer Res.
67:3853–3861. 2007. View Article : Google Scholar
|
|
16.
|
Bakeman A: Recommended effect size
statistics for repeated measures designs. Behav Res Methods.
37:379–384. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Stoline MR: The status of multiple
comparisons, simultaneous estimation of all pairwise comparisons in
one-way ANOVA designs. Am Stat. 35:134–141. 1981.
|
|
18.
|
Zheng X, Chang RL, Cui XX, et al: Effects
of 12-O-tetradecanoylphorbol-13-acetate (TPA) in combination with
paclitaxel (Taxol) on prostate cancer LNCaP cells cultured in vitro
or grown as xenograft tumors in immunodeficient mice. Clin Cancer
Res. 12:3444–3451. 2006. View Article : Google Scholar
|
|
19.
|
End DW, Smets G, Todd AV, et al:
Characterization of the antitumor effects of the selective farnesyl
protein transferase inhibitor R115777 in vivo and in vitro. Cancer
Res. 61:131–137. 2001.PubMed/NCBI
|
|
20.
|
Macdonald JS, McCoy S, Whitehead RP, et
al: A phase II study of farnesyl transferase inhibitor R115777 in
pancreatic cancer: a Southwest Oncology Group (SWOG 9924) study.
Invest New Drugs. 23:485–487. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Cohen SJ, Ho L, Ranganathan S, et al:
Phase II and pharmaco-dynamic study of the farnesyltransferase
inhibitor R115777 as initial therapy in patients with metastatic
pancreatic adenocarcinoma. J Clin Oncol. 21:1301–1306. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Sun J, Ohkanda J, Coppola D, et al:
Geranylgeranyltransferase I inhibitor GGTI-2154 induces breast
carcinoma apoptosis and tumor regression in H-Ras transgenic mice.
Cancer Res. 63:8922–8929. 2003.PubMed/NCBI
|
|
23.
|
Malinowski JM: Atorvastatin, a
hydroxymethylglutarylcoenzyme A reductase inhibitor. Am J Health
Syst Pharm. 55:2253–2303. 1998.PubMed/NCBI
|
|
24.
|
Goldstein JL and Brown MS: Regulation of
the mevalonate pathway. Nature. 343:425–430. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Wiemer AJ and Wiemer DF: The intermediate
enzymes of isoprenoid metabolism as anticancer targets. Anticancer
Agents Med Chem. 9:526–542. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Ding XZ, Hennig R and Adrian TE:
Lipoxygenase and cyclooxygenase metabolism: new insights in
treatment and chemoprevention of pancreatic cancer. Mol Cancer.
2:10–16. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
El-Rayes BF, Ali S, Sarkar FH and Philip
PA: Cyclooxygenase-2-dependent and -independent effects of
celecoxib in pancreatic cancer cell lines. Mol Cancer Ther.
3:1421–1426. 2004.PubMed/NCBI
|
|
28.
|
Raut CP, Nawrocki S, Lashinger LM, et al:
Celecoxib inhibits angiogenesis by inducing endothelial cell
apoptosis in human pancreatic tumor xenografts. Cancer Biol Ther.
3:1217–1224. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Wei D, Wang L, He Y, Xiong HQ, Abbruzzese
JL and Xie K: Celecoxib inhibits vascular endothelial growth factor
expression in and reduces angiogenesis and metastasis of human
pancreatic cancer via suppression of Sp1 transcription factor
activity. Cancer Res. 64:2030–2038. 2004. View Article : Google Scholar
|
|
30.
|
Gregor JI, Kilian M, Heukamp I, et al:
Effects of selective COX-2 and 5-LOX inhibition on prostaglandin
and leukotriene synthesis in ductal pancreatic cancer in Syrian
hamster. Prostaglandins Leukot Essent Fatty Acids. 2:226–232.
2005.PubMed/NCBI
|
|
31.
|
Colby JK, Klein RD, McArthur MJ, et al:
Progressive meta-plastic and dysplastic changes in mouse pancreas
induced by cyclooxygenase-2 overexpression. Neoplasia. 10:782–796.
2008.PubMed/NCBI
|
|
32.
|
Glasgow RE and Mulvihill SJ: Pancreas.
Surgery, Basic Science and Clinical Evidence. Norton JA, Barie PS,
Bollinger RR, et al: 2nd edition. Springer; New York, NY: pp.
875–909. 2008
|