Introduction
With a 5-year survival rate of 5%, pancreatic cancer
is one of the most lethal malignancies in the United States
(1,2). The poor prognosis of pancreatic
cancer is due to the failure of early diagnosis for curative
surgical resection combined with adjuvant chemotherapy, the
aggressive biological behavior of the tumor and insensitivity to
most conventional therapies including chemotherapy and radiotherapy
(3). Although a recent study shows
that FOLFIRINOX (combination of fluorouracil, leucovorin,
irinotecan and oxaliplatin) is superior option for patients with
advanced pancreatic cancer and good ECOG (Eastern Cooperative
Oncology Group) performance status, gemcitabine
(difluorodeoxycitidine, dFdC) still remains the first-line standard
drug as a treatment available for metastatic and non-metastatic
with locally advanced pancreatic cancer (4,5);
however, the disease rapidly develops resistance to the drug and no
apparent improvement in overall survival rate over the last decade
(2,6).
The aldehyde dehydrogenase (ALDH) family comprises
evolutionarily conserved 19 isoforms that catalyze oxidization of
aldehydes to carboxylic acids and are localized in the cytoplasm,
mitochondria or nucleus of cells (7). Several lines of evidence suggest that
ALDH activity is a hallmark of cancer stem cells (CSCs) that can be
measured by Aldeflour assay (7).
Since CSCs are known to resistant to various chemotherapies, it is
possible that the resistance to chemotherapeutic agents is due to
the activity of ALDH in CSCs. For example, the expression of
ALDH1A1 or ALDH3A1 is correlated with the resistance of
chemotherapeutics in hematopoietic stem cells, breast cancer
patient samples, or colorectal cancer xenograft tumors (8–10).
The activation of ALDH1A1 was found in stem cell population in
multiple types of cancers including breast, colon, bladder,
pancreatic, head and neck squamous, lung, liver and ovarian cancer
(11–18). In pancreatic cancer patients,
ALDH1A1 expression is also implicated in a stem cell marker and
correlates with worse outcome (19). Recently, we found that the high
level of ALDH1A1 expression is correlated with the resistance to
gemcitabine in MIA PaCa-2/GR comparing with parental MIA PaCa-2/P
cells (20).
Dasatinib is a potent inhibitor of SRC family
kinases and ABL kinases (21,22).
An increasing body of evidence from preclinical and clinical
studies suggests that dasatinib enhanced the antitumor efficacy of
various chemotherapeutic drugs in multiple types of cancers such as
lung, colon, pancreatic, breast, prostate, ovarian, melanoma and
leukemia (23–33). In addition, dasatinib enhanced
antitumor effect of etoposide associated with a decreased
proportion of aldehyde dehydrogenase 1 (ALDH1)-positive cells in
breast cancer MDA-MB-231 and MDA-MB-157 cells (34). The combination treatment of
dasatinib and curcumin also eliminated chemoresistant colon cancer
HCT-116 and HT-29 cell line which show increased expression of CSC
markers as CD133, CD44, CD166 and ALDH1 (35). Although the role of dasatinib in
sensitizing pancreatic cancer cells to gemcitabine was explored
(25,26), the potentially crucial role in the
treatment of pancreatic CSCs has not been investigated.
Herein, we demonstrated the combination effect of
dasatinib and gemcitabine in inhibition of the cell proliferation
and survival of MIA PaCa-2/P and MIA PaCa-2/GR cell lines that are
highly enriched with the level of ALDH1A1 expression. Our results
suggest that the synergistic antitumor effects of
dasatinib/gemcitabine combination are mediated by reducing the
level of ALDH1A1 in ALDH1A1-enriched pancreatic cancer MIA PaCa-2
cells.
Materials and methods
Cell culture and reagents
MIA PaCa-2 cells were purchased from American Type
Culture Collection (ATCC, Manassas, VA, USA). MIA PaCa-2/GR cells
were generated in our laboratory as described (20). The cells were maintained as
described previously (20).
Gemcitabine and dasatinib were purchased from LC Labs (Woburn, MA,
USA) and dissolved in PBS and dimethyl sulfoxide (DMSO),
respectively.
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
assay
A total of 1,500 cells per well were plated in
96-well flat bottom plates and then exposed to test combination
treatment of gemcitabine and dasatinib in various concentrations.
The MTT cell viability assay was performed as described previously
(20). The combination index (CI)
was calculated by using CompuSyn software (ComboSyn, Inc., Paramus,
NJ, USA) and values of CI<1, CI=1, CI>1 indicate synergism,
additive effect, and antagonism, respectively.
Clonogenic assay
MIA PaCa-2/P and/or MIA PaCa-2/GR cells
(2×105 cells) were seeded in 60-mm dishes. Twenty-four
hours after plating, varying concentrations of the drugs, either as
a single agent or in combination, were added to the dishes. After
treatment, cells (500 cells) were re-seeded in 60 mm dishes in
triplicate. After 14 days of incubation, the colonies were stained
and examined as described elsewhere (36,37).
Western blot analysis
Cells were grown to ∼70% confluence and reagents
were added as indicated. Western blot analysis was performed as
described previously (36,37) with the following antibodies:
phospho-SRC (Y416), phospho-STAT3 (T705), and SRC (Cell Signaling
Technology, Inc., Boston, MA, USA), ALDH1A1 (Abcam, Cambridge, UK),
Poly-ADP-ribose-polymerase (PARP; BD Biosciences, Franklin, NJ,
USA), α-tubulin and β-actin (Sigma, St. Louis, MO, USA).
Caspase-3/7 activity assay
Caspase-3/7 activity assay was carried out by using
a Caspase-3/7 Glo assay (Promega, Madison, WI, USA) according to
the manufacturer’s protocol. Cells were treated with either
gemcitabine, dasatinib alone, or combination of both drugs for
indicated concentrations and caspase-3/7 activity was measured from
cell lysates after indicated time of treatment. Luminescence was
measured at 490 nm using VICTOR X multilable plate readers
(Perkin-Elmer Life Sciences, Boston, MA, USA). Relative
luminescence units were determined by calculating luminescence
values from samples as a percentage of values from vehicle-treated
control samples. The experiments were performed in triplicate and
repeated on two separately initiated cultures.
Small interfering RNA (siRNA)
For the RNA interfering experiment, SRC-siRNA,
5’-GUGUCUUAAUACUGUC CUU-3’ and control-siRNA, 5’-GACGAGCGGCACGUG
CACA-3’ were purchased from Bioneer (Daejeon, Korea). SRC-siRNA or
control-siRNA were transfected into MIA PaCa-2/P and MIA PaCa-2/GR
cells using Lipofectamine™ 2000 (Invitrogen, Carlsbad, CA, USA)
according to the manufacturer’s procedure. The transfected cells
were then processed for western blot analysis, caspase-3/7 activity
and MTT cell proliferation assay (20).
Statistical methods
Statistical comparisons were made using the
two-tailed Student’s t-test where appropriate. Results were
considered significant in all experiments at *P<0.05,
**P<0.01 and ***P<0.005. Data were
expressed as the mean ± SD.
Results
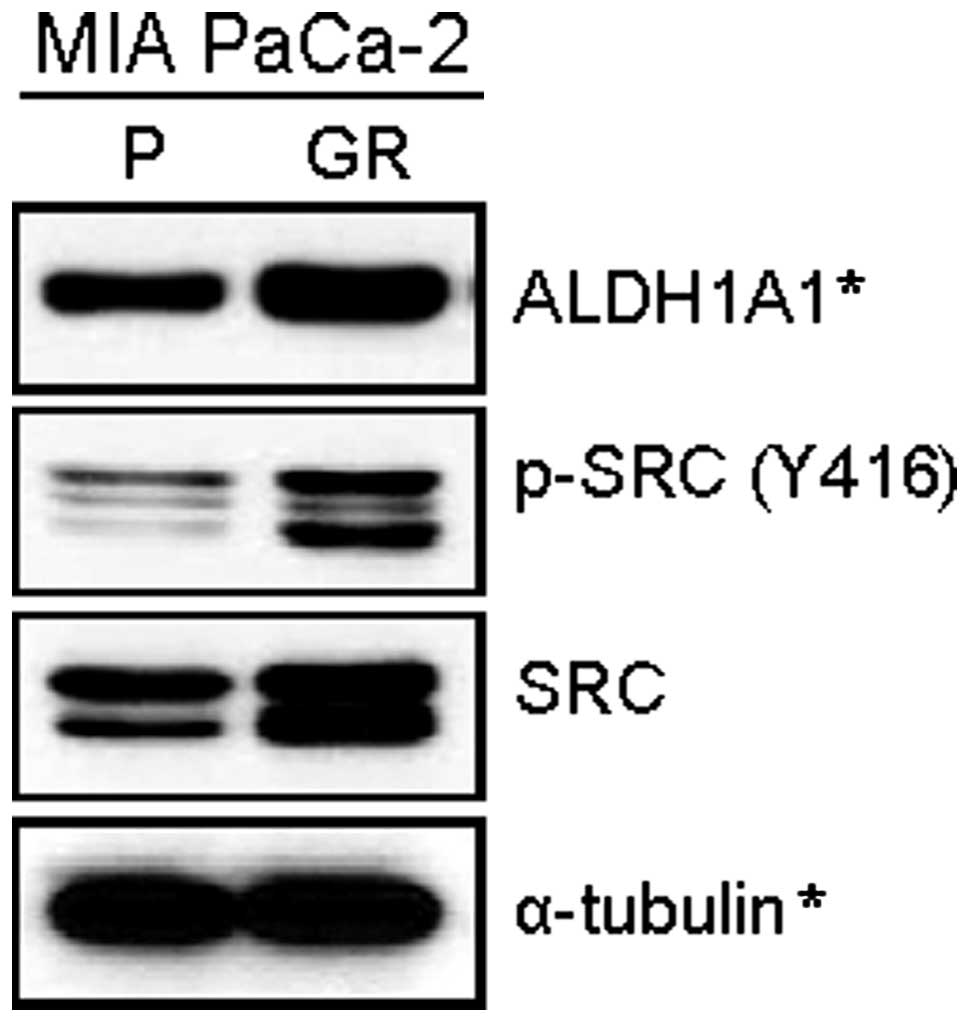
The level of SRC is significantly higher
in MIA PaCa-2/GR cells
Our recent study showed that among various human
pancreatic cancer cell lines, MIA PaCa-2 cells exhibit the highest
level of ALDH1A1 (20), a marker
of tumor-initiating and/or cancer stem cell properties in human
pancreatic cancer. In addition, we also found that the level of
ALDH1A1 expression was higher in MIA PaCa-2/GR cells than MIA
PaCa-2/P cells (20). Given the
potential correlation of SRC with ALDH1A1, we first examined the
level of SRC in both MIA PaCa-2/P and MIA PaCa-2/GR cells. The
western blot analysis revealed that both phosphorylated and total
form of SRC was significantly higher in MIA PaCa-2/GR cells than
MIA PaCa-2/P cells (Fig. 1).
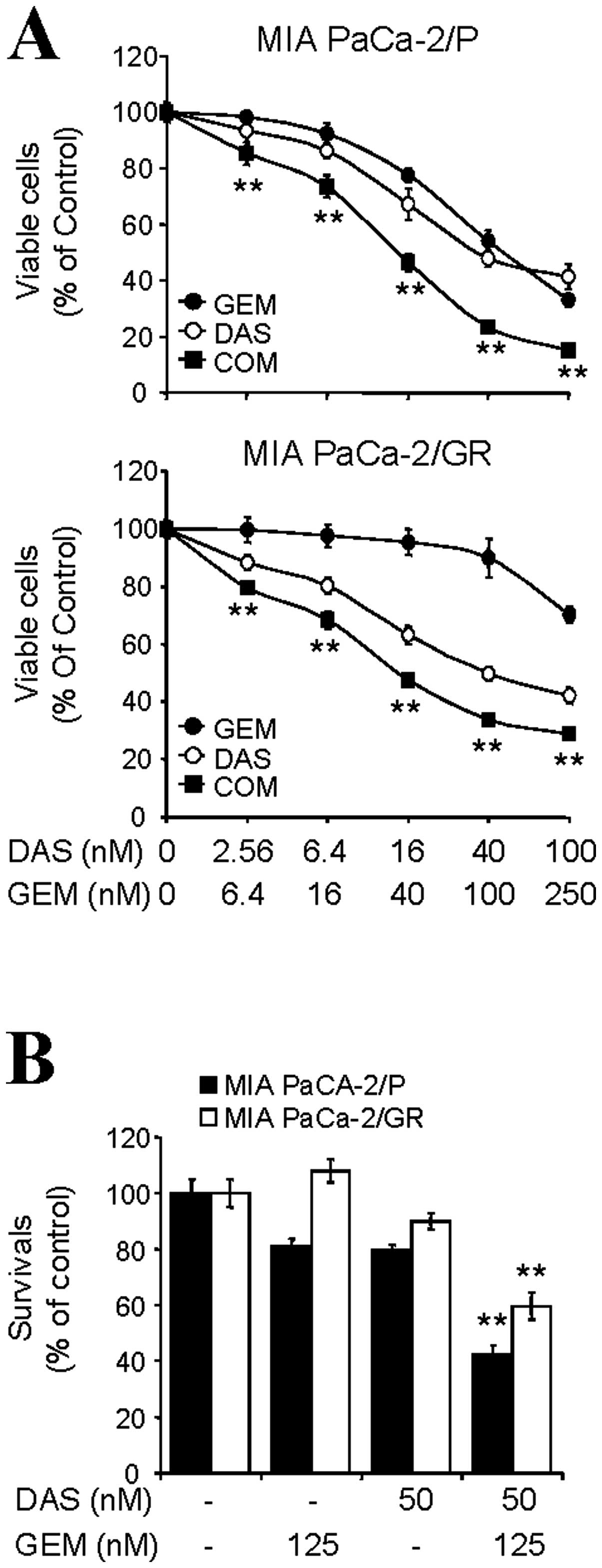
The synergistic antitumor effects by
combination of dasatinib and gemcitabine
In order to investigate the potential beneficial
effect of dasatinib/gemcitabine combination, both cell lines were
treated with dasatinib and gemcitabine for 72 h with fixed molar
ratios of 1:2.5. As shown in Fig.
2A, combination of dasatinib/gemcitabine synergistically
reduced the viable cells in both cell lines. The CI values at
ED50, ED75, and ED90 are 0.67,
0.74 and 0.86 for MIA PaCa-2/P cells and 0.47, 0.57 and 0.79 for
MIA PaCa-2/GR cells, respectively (Table I). In order to determine the
long-term combination effect of dasatinib/gemcitabine, cells were
treated with either dasatinib, gemcitabine or in combination of
both drugs for 24 h and then, cells were continually re-cultured in
fresh media without drug for 14 days. Survived colonies were
calculated as described in Materials and methods and plotted as
percentages of the no treatment control. Results showed that either
gemcitabine or dasatinib as single agent had limited effect on the
survival of these cells. On the contrary, the cell survival was
significantly reduced up to ∼42% in MIA PaCa-2/P and ∼59% in MIA
PaCa-2/GR when the cells were co-treated with dasatinib/
gemcitabine (Fig. 2B). These
results suggest that the combination of dasatinib/gemcitabine
results in a synergistic decrease in the cell proliferation and
survival of ALDH1A1-enriched pancreatic cancer MIA PaCa-2
cells.
 | Table I.Synergistic inhibition of cell
proliferation by combination of dasatinib/gemcitabine in
ALDH1A1-enriched pancreatic cancer MIA PaCa-2 cells.a |
Table I.
Synergistic inhibition of cell
proliferation by combination of dasatinib/gemcitabine in
ALDH1A1-enriched pancreatic cancer MIA PaCa-2 cells.a
|
ED50 |
ED75 |
ED90 |
|---|
| MIA PaCa-2/P | 0.67 | 0.74 | 0.86 |
| MIA PaCa-2/GR | 0.47 | 0.57 | 0.79 |
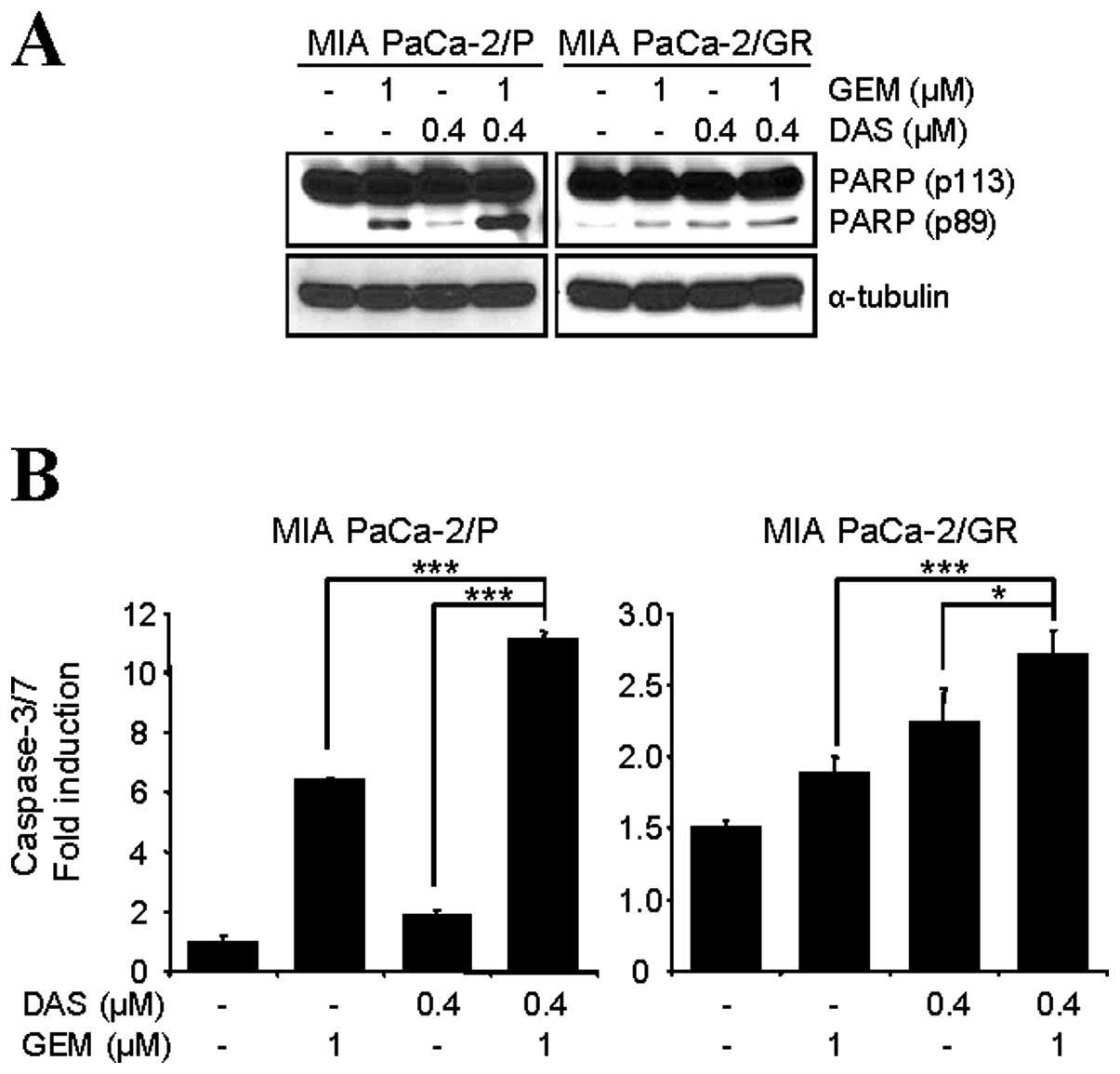
Dasatinib enhances apoptotic cell death
by gemcitabine in MIA PaCa-2 cells
The combination of dasatinib/gemcitabine on the
induction of apoptosis was also investigated. Cells were treated
with either dasatinib (0.4 μM), gemcitabine (1 μM)
alone or in combination of both drugs for 48 h and western blot
analysis was performed to detect apoptotic cell death with a
molecular biomarker of apoptosis, PARP cleavage. Comparing to cells
treated with dasatinib (0.4 μM) or gemcitabine (1 μM)
alone, dasatinib/gemcitabine-treated cells showed a more dramatic
increase of PARP cleavage in both cell lines (Fig. 3A). As expected, the combination of
dasatinib/gemcitabine significantly increased the caspase-3/7
activity in both cell lines (Fig.
3B). Taken together, these results suggest that treatment of
dasatinib significantly enhances gemcitabine-induced apoptosis
through activation of caspase-3/7 and PARP cleavage in both MIA
PaCa-2/P and MIA PaCa-2/GR cell lines.
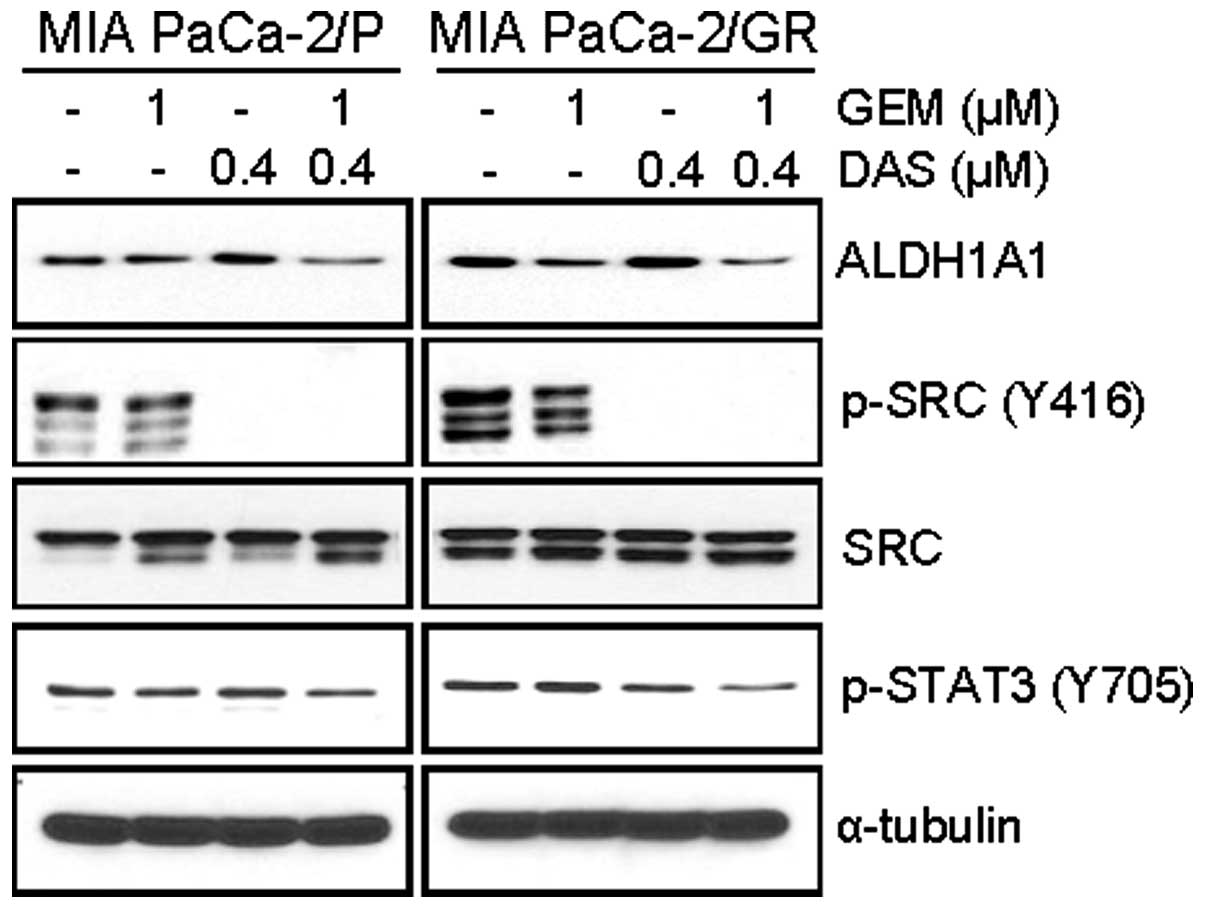
Dasatinib/gemcitabine combination
inhibits the level of ALDH1A1 expression and phospho-SRC
We also evaluated the effect of
dasatinib/gemcitabine combination on ALDH1A1 expression. Treatment
of cells for 48 h with gemcitabine (1 μM) partly reduced the
basal expression of ALDH1A1, while dasatinib (0.4 μM) did
not affect the basal expression of ALDH1A1 (Fig. 4). Importantly, the combination of
dasatinib/ gemcitabine further reduced the level of ALDH1A1
expression in both cell lines (Fig.
4).
Since dasatinib has been reported to decrease
phosphorylation of SRC, FAK, and AKT in a concentration-dependent
manner in either gemcitabine-sensitive (BxPC3) or
gemcitabine-resistant (Panc-1) pancreatic cancer cells (38), we also determined the level of
phospho-SRC in dasatinib/gemcitabine-treated cells. The western
blot analysis showed that combination of dasatinib/gemcitabine did
not affect the dasatinib-mediated suppression of phospho-SRC (Y416)
in these cells (Fig. 4). Under
these conditions, dasatinib alone showed limited inhibitory effect
on the phospho-STAT3 (Y705). However, combination of
dasatinib/gemcitabine inhibited the phosphorylation of STAT3 (Y705)
(Fig. 4).
Knockdown of SRC increases apoptotic cell
death and decreases the level of ALDH1A1 expression by
gemcitabine
The enhanced effect of SRC inhibition on
gemcitabine-induced cell death was further confirmed by
siRNA-mediated knockdown. The cells were transfected with either
control- or SRC-siRNA and further treated with gemcitabine. Under
these conditions, knockdown of SRC by siRNA reduced the level of
phospho-SRC (Y416) and phospho-STAT3 (Y705). Consistent with
dasatinib/gemcitabine combination, combination of SRC-siRNA and
gemcitabine further suppressed the phospho-STAT3 (Y705) in MIA
PaCa-2/P cells (Fig. 5A).
In order to confirm whether inhibition of SRC
enhances sensitivity to gemcitabine, cells pretreated with either
SRC-siRNA or control-siRNA for 48 h were incubated with various
concentrations of gemcitabine for 72 h and cell viability was
determined by MTT assay. The results showed that combination of
SRC-siRNA and gemcitabine was significantly more effective in
reducing the viable cells than control-siRNA and gemcitabine in
both cell lines (data not shown). Furthermore, gemcitabine-induced
PARP cleavage and caspase-3/7 activity were enhanced in these cells
by knockdown of SRC (Fig. 5B and
C). In addition, SRC-knockdown reduced the level of ALDH1A1 in
both cell lines (Fig. 5B). Again,
combination of SRC-siRNA and gemcitabine further decreased the
level of ALDH1A1 expression (Fig.
5B). Taken together, targeting of SRC activity by dasatinib or
siRNA enhanced gemcitabine-induced cell death by inducting
apoptotic cell death and reducing the level of ALDH1A1 expression
in ALDH1A1-enriched pancreatic cancer MIA PaCa-2 cells.
Discussion
In this study, we investigated the effect of
dasatinib on gemcitabine-sensitivity of ALDH1A1-enriched pancreatic
cancer MIA PaCa-2 cells. As results, we found that: i) MIA
PaCa-2/GR cells express significantly higher levels of phospho-SRC
and total SRC as well as ALDH1A1 than MIA PaCa-2/P cells; ii)
combination of dasatinib/gemcitabine reduces the cell proliferation
and survival by induction of apoptotic cell death in both MIA
PaCa-2/P and MIA PaCa-2/ GR cells; iii) dasatinib/gemcitabine
combination inhibits the phosphorylation of SRC (Y416) and STAT3
(Y705) and reduces the level of ALDH1A1; iv) knockdown of SRC by
siRNA enhances gemcitabine-induced apoptotic cell death; and v)
combination of SRC-knockdown with gemcitabine reduced the level of
ALDH1A1 expression. These results strongly support that inhibition
of SRC by dasatinib or siRNA sensitizes ALDH1A1-enriched pancreatic
cancer MIA PaCa-2 cells to gemcitabine.
Failure of standard chemotherapy and radiotherapy to
eliminate pancreatic CSCs is thought to be a key hurdle in the
treatment of pancreatic cancer. CSCs including pancreatic CSCs
possess potential to self-renew and to differentiate into
heterogeneous population of cells within the tumor, and have a high
ability to invade and metastasize (39,40).
It has been reported that pancreatic CSCs are resistant to
gemcitabine and therefore play a significant role in recurrence of
primary pancreatic cancer (41–43).
Pancreatic CSCs are currently identified by the expression of
specific surface and cytoplasmic markers. The potential stem cell
markers such as CD24, CD44 and ESA were reported to be enriched in
pancreatic CSCs (44); and other
markers such as CD133 and ALDH1A1 were also reported to be enriched
in pancreatic CSCs (16,44,45).
Recently, ALDH1A1 has been identified as a potential therapeutic
target (7,46). Notably, inhibition of ALDH1A1 has
been shown to sensitize ALDH1A1-enriched pancreatic cancer MIA
PaCa-2 cells to gemcitabine (20);
in addition, inhibition of ALDH has been also shown to sensitize
ALDH-enriched ovarian and breast cancer cells to chemotherapy and
radiotherapy (18,47).
Taken together, the present study suggests a
potential application of dasatinib/gemcitabine combination to
eliminate the CSC population in the ALDH1A1-enriched pancreatic
cancer MIA PaCa-2 cell lines. This might be particularly of
importance in treatment of pancreatic CSCs which show resistance to
gemcitabine (41–43). Our observation implicates that the
combination of dasatinib/gemcitabine may provide great benefit to
eliminate pancreatic CSCs and inhibit the recurrence of pancreatic
cancer. However, further studies are needed to investigate this
therapeutic strategy in ALDH1A1-positive cells that are isolated by
Aldeflour assay or other CSC marker-specific methods both in
vitro and in vivo animal models.
Acknowledgements
This study was supported by National
Research Foundation of Korea [R31-10069; World Class University
(WCU) program] (Y.S.S.), National Institutes of Health
(1R03CA152530) (I.B.) and the Georgetown University Lombardi
Comprehensive Cancer Center (P30-CA051008) (I.B.).
References
|
1.
|
Hidalgo M: Pancreatic cancer. N Engl J
Med. 362:1605–1617. 2010. View Article : Google Scholar
|
|
2.
|
Long J, Zhang Y, Yu X, Yang J, LeBrun DG,
Chen C, Yao Q and Li M: Overcoming drug resistance in pancreatic
cancer. Expert Opin Ther Targets. 15:817–828. 2011. View Article : Google Scholar
|
|
3.
|
Duffy JP, Eibl G, Reber HA and Hines OJ:
Influence of hypoxia and neoangiogenesis on the growth of
pancreatic cancer. Mol Cancer. 2:122003. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Conroy T, Desseigne F, Ychou M, Bouché O,
Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de
la Fouchardière C, Bennouna J, Bachet JB, Khemissa-Akouz F,
Péré-Vergé D, Delbaldo C, Assenat E, et al: FOLFINOX versus
gemcitabine for metastatic pancreatic cancer. N Engl J Med.
364:1817–1825. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Loehrer PJ Sr, Feng Y, Cardenes H, Wagner
L, Brell JM, Cella D, Flynn P, Ramanathan RK, Crane CH, Alberts SR
and Benson AB III: Gemcitabine alone versus gemcitabine plus
radiotherapy in patients with locally advanced pancreatic cancer:
an Eastern Cooperative Oncology Group trial. J Clin Oncol.
29:4105–4112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Kim MP and Gallick GE: Gemcitabine
resistance in pancreatic cancer: picking the key players. Clin
Cancer Res. 14:1284–1285. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Marcato P, Dean CA, Giacomantonio CA and
Lee PWK: Aldehyde dehydrogenase: its role as a cancer stem cell
marker comes down to the speficic isoform. Cell Cycle.
10:1378–1384. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Dylla SJ, Beviglia L, Park IK, Chartier C,
Raval J, Ngan L, Pickell K, Aguilar J, Lazetic S, Smith-Berdan S,
Clarke MF, Hoey T, Lewicki J and Gurney AL: Colorectal cancer stem
cells are enriched in xenogeneic tumors following chemotherapy.
PLoS One. 18:e24282008. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Magni M, Shammah S, Schiró R, Mellado W,
Dalla-Favera R and Gianni AM: Induction of
cyclophosphamide-resistance by aldehyde-dehydrogenase gene
transfer. Blood. 87:1097–1103. 1998.PubMed/NCBI
|
|
10.
|
Sládek NE, Kollander R, Sreerama L and
Kiang DT: Cellular levels of aldehyde dehydrogeneases (ALDH1A1 and
ALDH3A1) as predictors of therapeutic responses to
cyclophosphamide-based chemotherapy of breast cancer: a
retrospective study. Rational individualization of
oxazaphosphorine-based cancer chemotherapeutic regimens. Cancer
Chemother Pharmacol. 49:309–321. 2002.
|
|
11.
|
Charafe-Jauffret E, Ginestier C, Iovino F,
Tarpin C, Diebel M, Esterni B, Houvenaeghel G, Extra JM, Bertucci
F, Jacquemier J, Xerri L, Dontu G, Stassi G, Xiao Y, Barsky SH,
Birnbaum D, et al: Aldehyde dehydrogenase 1-positive cancer stem
cells mediate metastasis and poor clinical outcome in inflammatory
breast cancer. Clin Cancer Res. 16:45–55. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Huang EH, Hynes MJ, Zhang T, Ginestier C,
Dontu G, Appelman H, Fields JZ, Wicha MS and Boman BM: Aldehyde
dehydrogenase 1 is a marker for normal and malignant human colonic
stem cells (SC) and tracks SC overpopulation during colon
tumorigenesis. Cancer Res. 69:3382–3389. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Su Y, Qui Q, Zhang Z, Jiang Z, Leng Q, Liu
Z, Stass SA and Jiang F: Aldehyde dehydrogenase 1 A1-positive cell
population is enriched in tumor-initiating cells and associated
with progression of bladder cancer. Cancer Epidemiol Biomarkers
Prev. 19:327–337. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Dembinski JL and Krauss S:
Characterization and functional analysis of a slow cycling stem
cell-like subpopulation in pancreas adenocarcinoma. Clin Exp
Metastasis. 26:611–623. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Clay MR, Tabor M, Owen JH, Carey TE,
Bradford CR, Wolf GT, Wicha MS and Prince ME: Single-marker
identification of head and neck squamous cell carcinoma cancer stem
cells with aldehyde dehydrogenase. Head Neck. 32:1195–1201. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Jiang F, Qui Q, Khanna A, Todd NW, Deepak
J, Xing L, Wang H, Liu Z, Su Y, Stass SA and Katz RL: Aldehyde
dehydrogenase 1 is a tumor stem cell-associated marker in lung
cancer. Mol Cancer Res. 7:330–338. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Ma S, Chan KW, Hu L, Lee TK, Wo JY, Ng IO,
Zheng BJ and Guan XY: Identification and characterization of
tumorigenic live cancer stem/progenitor cells. Gastroenterology.
132:2542–2556. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Landen CN Jr, Goodman B, Katre AA, Steg
AD, Nick AM, Stone RL, Miller LD, Mejia PV, Jennings NB, Gershenson
DM, Bast RC Jr, Coleman RL, Lopez-Berestein G and Sood AK:
Targeting aldehyde dehydrogenase cancer stem cells in ovarian
cancer. Mol Cancer Ther. 9:3186–3199. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Rasheed ZA, Yang J, Wang Q, Kowalski J,
Freed I, Murter C, Hong SM, Koorstra JB, Rajeshkumar NV, He X,
Goggins M, Iacobuzio-Donahue C, Berman DM, Laheru D, Jimeno A,
Hidalgo M, Maitra A and Matsui W: Prognostic significance of
tumorigenic cells with mesenchymal features in pancreatic
adenocarcinoma. J Natl Cancer Inst. 102:340–351. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Duong HQ, Hwang JS, Kim HJ, Kang HJ, Seong
YB and Bae I: Aldehyde dehydrogenase 1A1 confers intrinsic and
acquired resistance to gemcitabine in human pancreatic
adenocarcinoma MIA PaCa-2 cells. Int J Oncol. 41:855–861.
2012.PubMed/NCBI
|
|
21.
|
Araujo J and Logothetis C: Dasatinib: a
potent SRC inhibitor in clinical development for the treatment of
solid tumors. Cancer Treat Rev. 36:492–500. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Kim LC, Rix U and Haura EB: Dasatinib in
solid tomors. Expert Opin Investig Drugs. 19:415–425. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Ceppi P, Papotti M, Monica V, Lolanono M,
Saviozzi S, Pautasso M, Novello S, Mussino S, Bracco E, Volante M
and Scagliotti GV: Effects of Src kinase inhibition induced by
dasatinib in non-small cell lung cancer cell lines treated with
cisplatin. Mol Cancer Ther. 8:3066–3074. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Kopetz S, Lesslie DP, Dallas NA, Park SI,
Johnson M, Parikh NU, Kim MP, Abbruzzese JL, Ellis LM, Chandra J
and Gallick GE: Synergistic activity of the SRC family kinase
inhibitor dasatinib and oxaliplatin in colon carcinoma cells is
mediated by oxidative stress. Cancer Res. 69:3842–3849. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Nagaraj NS, Washington MK and Merchant NB:
Combined blockade of Src kinase and epidermal growth factor
receptor with gemcitabine overcomes STAT3-mediated resistance of
inhibition of pancreatic tumor growth. Clin Cancer Res. 17:483–493.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Kim YJ, Hong YB, Cho CH, Seong YS and Bae
I: Exploring protein kinase inhibitors: unveiling gemcitabine
resistance in pancreatic cancer. Pancreas. 41:804–805. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Hong DS, Choe JH, Naing A, Wheler JJ,
Falchook GS, Piha-Paul S, Moulder SL, George GC, Choe JM, Strauss
LC, Gallick GE and Kurzrock R: A phase 1 study of gemcitabine
combinated with dasatinib in patients with advanced solid tumors.
Invest New Drugs. 31:918–926. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Park BJ, Whichard ZL and Corey SJ:
Dasatinib synergizes with both cytotoxic and signal transduction
inhibitors in heterogeneous breast cancer cell lines - lessons for
design of combination targeted therapy. Cancer Lett. 320:104–110.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Somlo G, Atzori F, Strauss LC, Geese WJ,
Specht JM, Gradishar WJ, Rybicki A, Sy O, Vahdal LT and Cortes J:
Dasatinib plus capecitabine for advanced breast cancer: safety and
efficacy in phase I study CA180004. Clin Cancer Res. 19:1884–1893.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Araujo JC, Mathew P, Armstrong AJ, Braud
EL, Posadas E, Lonberg M, Gallick GE, Trudel GC, Paliwal P, Agrawal
S and Logothetic CJ: Dasatinib combined with docetaxel for
castration-resistant prostate cancer: results from a phase 1–2
study. Cancer. 118:63–71. 2012.PubMed/NCBI
|
|
31.
|
Secord AA, Teoh DK, Barry WT, Yu M,
Broadwater G, Havrilesky LJ, lee PS, Berchuck A, Lancaster J and
Wenham RM: A phase I trial of dasatinib, an SRC-family kinase
inhibitor, in combination with paclitaxel and carboplatin in
patients with advanced or recurrent ovarian cancer. Clin Cancer
Res. 18:5489–5498. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Algazi AP, Weber JS, Andrews SC, Urbas P,
Munster PN, DeConti RC, Hwang J, Sondak VK, Messina JL, McCalmont T
and Daud AI: Phase I clinical trial of the Src inhibitor dasatinib
with dacarbazine in metastatic melanoma. Br J Cancer. 106:85–91.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Breccia M, Serrao A, Salaroli A, Loglisci
G, Zacheo I and Alimena G: Dasatinib combined with weekly
administration of vincristine as effective therapy in sudden or
resistant Ph+ lymphoid blast crisis of chronic myeloid leukaemia.
Br J Haematol. 159:612–613. 2012.
|
|
34.
|
Kurebayashi J, Kanomata N, Moriya T,
Kozuka Y, Watanabe M and Sonoo H: Preferential antitumor effect of
the Src inhibitor dasatinib associated with a decreased proportion
of aldehyde dehydrogenase 1-positive cells in breast cancer cells
of the basal B subtype. BMC Cancer. 10:5682010. View Article : Google Scholar
|
|
35.
|
Nautiyal J, Kanwar SS, Yu Y and Majumdar
AP: Combination of dasatinib and curcumin eliminates
chemo-resistant colon cancer cells. J Mol Signal. 6:72011.
View Article : Google Scholar : PubMed/NCBI
|
|
36.
|
Duong HQ, Kim HJ, Kang HJ, Seong YS and
Bae I: ZSTK474, a PI3K inhibitor, suppresses proliferation and
sensitizes human pancreatic adenocarcinoma cells to gemcitabine.
Oncol Rep. 27:182–188. 2012.PubMed/NCBI
|
|
37.
|
Duong HQ, Hong YB, Kim JS, Lee HS, Yi YW,
Kim YJ, Wang A, Zhao W, Cho CH, Seong YS and Bae I: Inhibition of
checkpoint kinase 2 (CHK2) enhances sensitivity of pancreatic
adenocarcinoma cells to gemcitabine. J Cell Mol Med. 17:1261–1270.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
38.
|
Nagaraj NS, Smith JJ, Revetta F,
Washington MK and Merchant NB: Targeted inhibition of SRC kinase
signaling attenuates pancreatic tumorigenesis. Mol Cancer Ther.
9:2322–2332. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Dick JE: Stem cell concepts renew cancer
research. Blood. 112:4793–4807. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40.
|
Wang JC and Dick JE: Cancer stem cells:
lesions from leukemia. Trends Cell Biol. 15:494–501. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
41.
|
Yin T, Wei H, Gou S, Shi P, Yang Z, Zhao G
and Wang C: Cancer stem-like cells enriched in panc-1 spheres
possess increased migration ability and resistance to gemcitabine.
Int J Mol Sci. 12:1595–1604. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
42.
|
Hu G, Li F, Ouyang K, Xie F, Tang X, Wang
K, Han S, Jiang Z, Zhu M, Wen D, Qin X and Zhang L: Intrinsic
gemcitabine resistance in a novel pancreatic cancer cell line is
associated with cancer stem cell-like phenotype. Int J Oncol.
40:798–806. 2012.PubMed/NCBI
|
|
43.
|
Hage C, Rausch V, Giese N, Giese T,
Schonsiegel F, Labsch S, Nwaeburu C, Mattern J, Gladkich J and Herr
I: The novel c-Met inhibitor cabozantinib overcomes gemcitabine
resistance and stem cell signaling in pancreatic cancer. Cell Death
Dis. 4:e6272013. View Article : Google Scholar : PubMed/NCBI
|
|
44.
|
Li C, Heidt DG, Dalerba P, Burant CF,
Zhang L, Adsay V, Wicha M, Clarke MF and Simeone DM: Identification
of pancreatic cancer stem cells. Cancer Res. 67:1030–1037. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
45.
|
Kim MP, Fleming JB, Wang H, Abbruzzese JL,
Choi W, Kopetz S, McConkey DJ, Evans DB and Gallick GE: ALDH
activity selectively defines an enhanced tumor-initiating cell
population relative to CD133 expression in human pancreatic
adenocarcinoma. PLoS One. 6:e206362011. View Article : Google Scholar : PubMed/NCBI
|
|
46.
|
Koppaka V, Thompson DC, Chen Y, Ellermann
M, Nicolaou KC, Juvonen RO, Petersen D, Deitrich RA, Hurley TD and
Vasiliou V: Aldehyde dehydrogenase inhibitors: a comprehensive
review on the pharmacology, mechanism of action, substrate
specificity, and clinical application. Pharmacol Rev. 64:520–539.
2012. View Article : Google Scholar
|
|
47.
|
Croker AK and Allan AL: Inhibition of
aldehyde dehydrogenase (ALDH) activity reduces chemotherapy and
radiation resistance of stem-like ALDHhiCD44+ human
breast cancer cells. Breast Cancer Res Treat. 133:75–87. 2012.
View Article : Google Scholar : PubMed/NCBI
|