Introduction
Hepatocellular carcinoma (HCC) is one of the most
common and frequently occurring tumors worldwide (1). Although the clinical diagnosis and
management of early-stage HCC have improved significantly, HCC
prognosis is still extremely poor (2). Furthermore, advanced HCC is a highly
aggressive tumor with poor or no response to common therapies.
Thus, there is a strong demand for new curative approaches to
advanced HCC.
Metformin is an oral biguanide drug introduced into
clinical practice in the 1950s for the treatment of type 2 diabetes
(3). It lowers hyperglycemia by
inhibiting hepatic glucose production. According to a recent
gastroenterological study, metformin has significant effects on
tumorigenesis (4). For instance,
it has been reported that patients with type 2 diabetes who are
prescribed metformin have a lower risk of pancreatic cancer
compared to patients who do not take metformin (5). In basic investigations, metformin was
shown to inhibit the proliferation of various human cancer cell
types, such as those of the prostate (6), breast (7), colon (8,9),
stomach (10), esophagus (11) and HCC (12). However, the mechanism underlying
the growth suppression of various cancers, including HCC, by
metformin remains relatively unknown.
The relatively recent investigation into miRNAs has
identified a new layer of gene regulation mechanisms. It has become
apparent that aberrant miRNA expression is a common feature of
various human malignancies. In terms of the relationship between
miRNAs and HCC, many studies have shown that specific miRNAs are
expressed aberrantly in malignant HCC cells or tissues compared to
non-malignant hepatocytes and tissues (13–15).
These previous studies have also shown that the modulation of
non-coding RNAs, specifically miRNAs, may act to modulate HCC
formation. However, although miRNAs are becoming increasingly
recognized as regulatory molecules in HCC, their involvement in the
responses to environmental changes, such as exposure to drugs,
remains unknown.
Here we show that me tformin is effective for the
treatment of HCC, and have also studied the expression of cell
cycle-related molecules, tyrosine kinases of receptor type and
angiogenesis molecules to explore the mechanism underlying the
antitumor effect of metformin. In addition, we have identified
miRNAs associated with the antitumor effect of metformin.
Materials and methods
Chemicals
Metformin (1,1-dimethylbiguanide monohydrochloride)
was purchased from Dainippon Sumitomo Pharma (Tokyo, Japan). A Cell
Counting Kit (CCK-8) was purchased from Dojindo Laboratories
(Kumamoto, Japan), and all other chemicals were obtained from Sigma
Chemical (Tokyo, Japan).
Antibodies
In this study, the following antibodies were used:
anti-β-actin monoclonal antibody (Sigma-Aldrich, St. Louis, MO;
A5441, used at 1:3,000), cyclin D1 (Thermo Fisher Scientific,
Waltham, MA; RB-9041, used at 1:1,000), cyclin E (BD Biosciences,
Franklin Lakes, NJ; used at 1:1,000), Cdk6 (Santa Cruz
Biotechnology, Santa Cruz, CA; sc-177, used at 1:1,000), Cdk4 (Cell
Signaling Technology, Danvers, MA; #2906, used at 1:1,000), Cdk2
(Santa Cruz Biotechnology, sc-163, used at 1:2,000), and secondary
horseradish peroxidase-linked anti-mouse and anti-rabbit IgG
antibodies (GE Healthcare UK, Buckinghamshire, UK; used at
1:2,000).
Cell lines and culture
The human HCC cell lines Alex, HLE and Huh7 were
obtained from the Japanese Cancer Research Resources Bank (Tokyo,
Japan). Cells of a normal human liver cell line, Hc-Cells, were
obtained from DS Pharma Biomedical (Osaka, Japan). The human HCC
cells were grown in RPMI-1640 (Gibco Invitrogen, Carlsbad, CA, USA)
and human normal liver cells were grown in a CS-C Complete Medium
Kit R (DS Pharma Biomedical, Osaka, Japan). Both media contained
10% fetal bovine serum (533–69545; Wako, Osaka, Japan) and
penicillin-streptomycin (100 mg/l; Invitrogen, Tokyo, Japan).
Cell proliferation assay
Cell proliferation assays were performed using the
Alex, HLE, and Huh7 cells according to the manufacturer’s
instructions. Cells from each line (1×104) were seeded
into a well of a 96-well plate and cultured in 100 μl of
RPMI-1640 supplemented with 10% FBS. After 24 h seeding cells were
treated by addition of 1 or 5 mM metformin into the culture medium
or were left untreated. At the indicated time points, the medium
was exchanged for 110 μl of RPMI-1640 with the cell lines
reagent (10 μl CCK-8 and 100 μl RPMI-1640), and the
cells were incubated for 2 h. The absorbance was measured for each
well at a wavelength of 450 nm using an auto-microplate reader.
Cell lysate and tissue lysate
The cell lysate assay was performed according to the
methods described in our previous reports (16–18).
All steps were carried out at 4°C. Protein concentrations were
measured using a dye-binding protein assay based on the Bradford
method (19).
Gel electrophoresis and western blot
analysis
Samples were electrophoresed using 10% sodium
dodecyl sulfatepolyacrylamide gels (SDS-PAGE) (18), and the proteins were transferred to
nitrocellulose membranes. The membranes were incubated with primary
antibodies after blocking. Then, the membranes were incubated with
horseradish peroxidaseconjugated secondary antibodies (20). The immunoreactive proteins were
visualized with an enhanced chemiluminescence detection system
(Perkin-Elmer Co., Waltham, MA) on X-ray film.
Flow cytometry analysis
To evaluate the mechanism of growth inhibition by
metformin, the cell cycle profile was analyzed after treatment with
metformin. Huh7 cells (1.0×106 cells in a 6-well plate
dish) were treated with 10 mM metformin or without metformin for
24–72 h. After treatment, the cells were harvested and fixed in 80%
ethanol. The fixed cells were washed with PBS and then stored at
−20°C until flow cytometric analysis was performed. On the day of
analysis, cells were washed and centrifuged using cold PBS,
suspended in 100 μl PBS and 10 μl RNase A solution
(250 μg/ml) and incubated for 30 min at 37°C. Then, 110
μl propidium iodide (PI) stain (100 μg/ml) was added
to each tube, and the tubes were incubated at 4°C for at least 30
min prior to analysis.
Flow cytometric analysis was performed using a
Cytomics FC 500 flow cytometer (Beckman Coulter, Brea, CA)
appointed with an argon laser (488 nm). The percentages of cells in
different phases of the cell cycle were analyzed by using FlowJo
software (Tree Star, Ashland, OR). All experiments were performed
in triplicate to assess for consistency of response.
Xenograft model analysis
Animal experiments were performed according to the
guidelines of the Committee on Experimental Animals of Kagawa
University and use of animals by National Cancer Research Institute
(NCRI) (21). We purchased 30 male
athymic mice (BALB/c-nu/nu; 8 weeks old; 20–25 g) from Japan SLC
(Hamamatsu, Japan). The animals were maintained under specific
pathogen-free conditions using a laminar airflow rack and had
continuous free access to sterilized food (gamma-ray-irradiated
food, CL-2; Clea Japan, Tokyo, Japan) and autoclaved water. Each
mouse was subcutaneously inoculated with Huh7 cells
(5×106 cells/animal) in the flank region. After the
xenografts were identifiable as a mass of more than 6 mm in maximal
diameter in all recipients, the animals were randomly assigned to
three groups. The metformin-treated group was injected 5 times a
week intraperitoneally (i.p.) at 1 mg/body or 2 mg/body per day for
2 weeks. The control group was administered only PBS (n=10) for 2
weeks. After the initiation of the metformin administration, the
tumor growth was monitored by the same investigators (H.M. and
T.M.), and the tumorigenesis of HCC was monitored everyday. Tumor
size was measured weekly by measuring the two greatest
perpendicular tumor dimensions. To examine the significance of the
differences between growth curves in this study, all the
measurements of tumor volume for each growth curve from the start
of the treatment to the end, typically about 30 observations, were
analyzed by one-way analysis of variance (ANOVA). The tumor volume
was calculated as follows: tumor volume (mm3) = [tumor
length (mm) × tumor width (mm)2]/2 (22). All animals were sacrificed on day
14 after treatment. All animals were alive during the
observation.
Antibody arrays of phosphorylated
receptor tyrosine kinase (p-RTK)
The RayBio™ Human Phospho Array Kit (cat. no. ARY
001) was purchased from RayBiotech Inc. (Norcross, GA). The assay
for the p-RTK array was performed according to the manufacturer’s
instructions. Briefly, p-RTK array membranes were blocked with 5%
BSA/TBS (0.01 M Tris-HCl, pH 7.6) for 1 h. The membranes were then
incubated with 2 ml of lysate prepared from cell lines or tumorous
tissues after normalization with equal amounts of protein. After
extensive washing with TBS including 0.1% v/v Tween-20 (3 washings
of 10 min each), and TBS alone (2 washings of 10 min each) to
remove unbound materials, the membranes were incubated with
anti-phospho-tyrosine-HRP antibody for 2 h at room temperature. The
unbound HRP antibody was washed out with TBS including 0.1%
Tween-20. Finally, each array membrane was exposed to X-ray film
using a chemiluminescence detection system (Perkin-Elmer Co.).
Antibody array for angiogenesis
To assess whether molecules important in
angiogenesis are regulated by the antitumor effect of metformin,
the RayBio Human Angiogenesis Antibody Array (RayBiotech Inc.) was
used according to the protocol. This method is a dot-blot-based
assay which enables detection and comparison of 19 different
angiogenesis-specific cytokines. Briefly, angiogenesis protein
array membranes were blocked with 5% BSA/TBS (0.01 M Tris-HCl, pH
7.6) for 1 h. The membranes were then incubated with 2 ml of lysate
prepared from tumor tissues after normalization with equal amounts
of protein. After extensive washing with TBS including 0.1% v/v
Tween-20 (3 washings of 5 min each) to remove unbound materials,
the membranes were incubated with HRP angiogenesis antibody for 2 h
at room temperature. Unbound HRP antibody was washed out with TBS
including 0.1% Tween-20. Finally, each array membrane was exposed
to X-ray film using a chemiluminescence detection system
(Perkin-Elmer Co.).
Densitometric analysis
The densitometric densities of p-EGFR and p-IGF-1R
in the cell lines and p-EGFR, Mer and angiogenin in tumorous tissue
were visualized in black and white, respectively. The densities of
p-EGFR, p-IGF-1R and Mer obtained from the membrane array were
analyzed by means of a Kodak Image Station (Kodak, Tokyo,
Japan).
Analysis of miRNA microarray
The samples of cancer cell lines were processed for
total RNA extraction with an miRNeasy mini kit (Qiagen, Hilden,
Germany) according to the manufacturer’s instructions. RNA samples
typically showed A260/280 ratios of between 1.9 and 2.1, as
determined using an Agilent 2100 Bioanalyzer (Agilent Technologies,
Santa Clara, CA). After RNA measurement with an RNA 6000 Nano kit
(Agilent Technologies), the samples were labeled using a miRCURY
Hy3/Hy5 Power labeling kit and were hybridized on a human miRNA
Oligo chip (v.14.0; Toray Industries, Tokyo, Japan). Scanning was
performed with the 3D-Gene Scanner 3000 (Toray Industries). 3D-Gene
extraction version 1.2 software (Toray Industries) was used to read
the raw intensity of the image. To determine the change in miRNA
expression between metformin-treated and control samples, the raw
data were analyzed via GeneSpringGX v 10.0 (Agilent Technologies).
Samples were first normalized relative to 28sRNA and baseline
corrected to the median of all samples. Replicate data were
consolidated into two groups: those from metformin-treated animals
and those from control animals, and were organized by using the
hierarchical clustering and analysis of variance (ANOVA) functions
in the GeneSpring software. Hierarchical clustering was done by
using the clustering function (condition tree) and Euclidean
correlation as a distance metric. Two-way ANOVA analysis and
asymptotic p-value computation without any error correction on the
samples were performed to search for the miRNAs that varied most
prominently across the different groups. The p-value cutoff was set
to 0.05. Only changes >50% on at least one of the time points
for each sample were considered significant. All the analyzed data
were scaled by global normalization. The statistical significance
of differentially expressed miRNAs was analyzed by Student’s
t-test. All our micoroarray data in this study were submited as a
complete data set to the NCBI Gene Expression Omnibus (GEO), no.
44204 (http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?token=ljglzioeieoqijc&acc=GSE44204).
Results
Metformin inhibits the proliferation of
human HCC cell lines
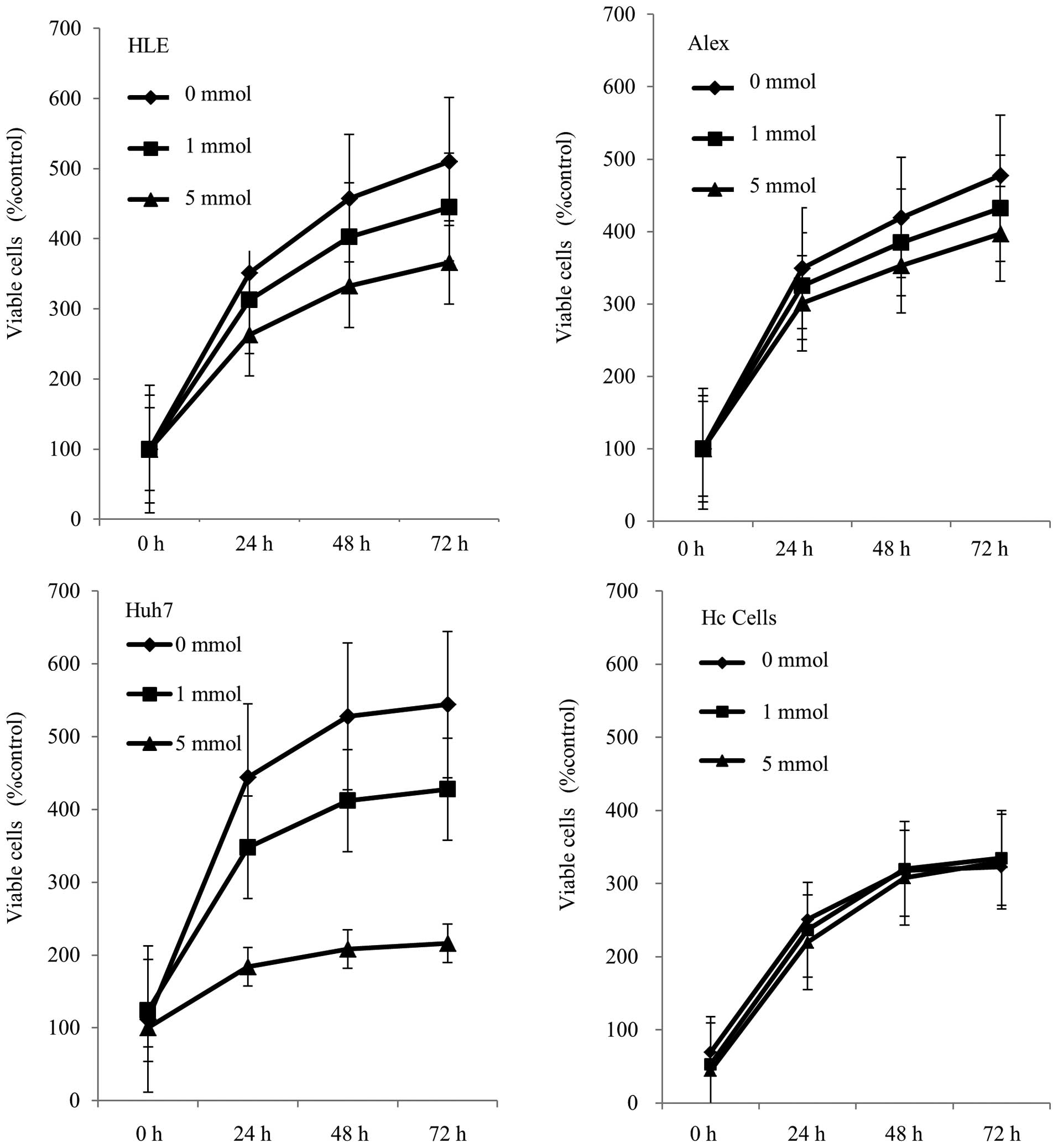
To evaluate the effect of the cell growth of
metformin on human HCC cells in vitro, we examined
metformin’s effect on proliferation in three HCC cell lines,
namely, Alex, HLE and Huh7. Cells were grown in 10% fetal bovine
serum (FBS) and treated with 1 or 5 mM metformin, or without
metformin as a control. To discern the direct relationship between
the decrease in cell viability and the inhibition of cell
proliferation, we followed the course of proliferation over 3 days
after the addition of metformin. Metformin (0, 1 and 5 mM) led to a
decrease in cell proliferation in a dose- and time-dependent manner
in all three cell lines (Fig. 1),
with the reduction being especially prominent in Huh7. On the other
hand, metformin did not suppress the proliferation of normal
hepatocytes. Thus the results showed that metformin inhibited the
proliferation of HCC cells, but not the proliferation of normal
hepatocytes (Hc cells).
Effects of metformin on cell cycle
regulatory proteins in Huh7
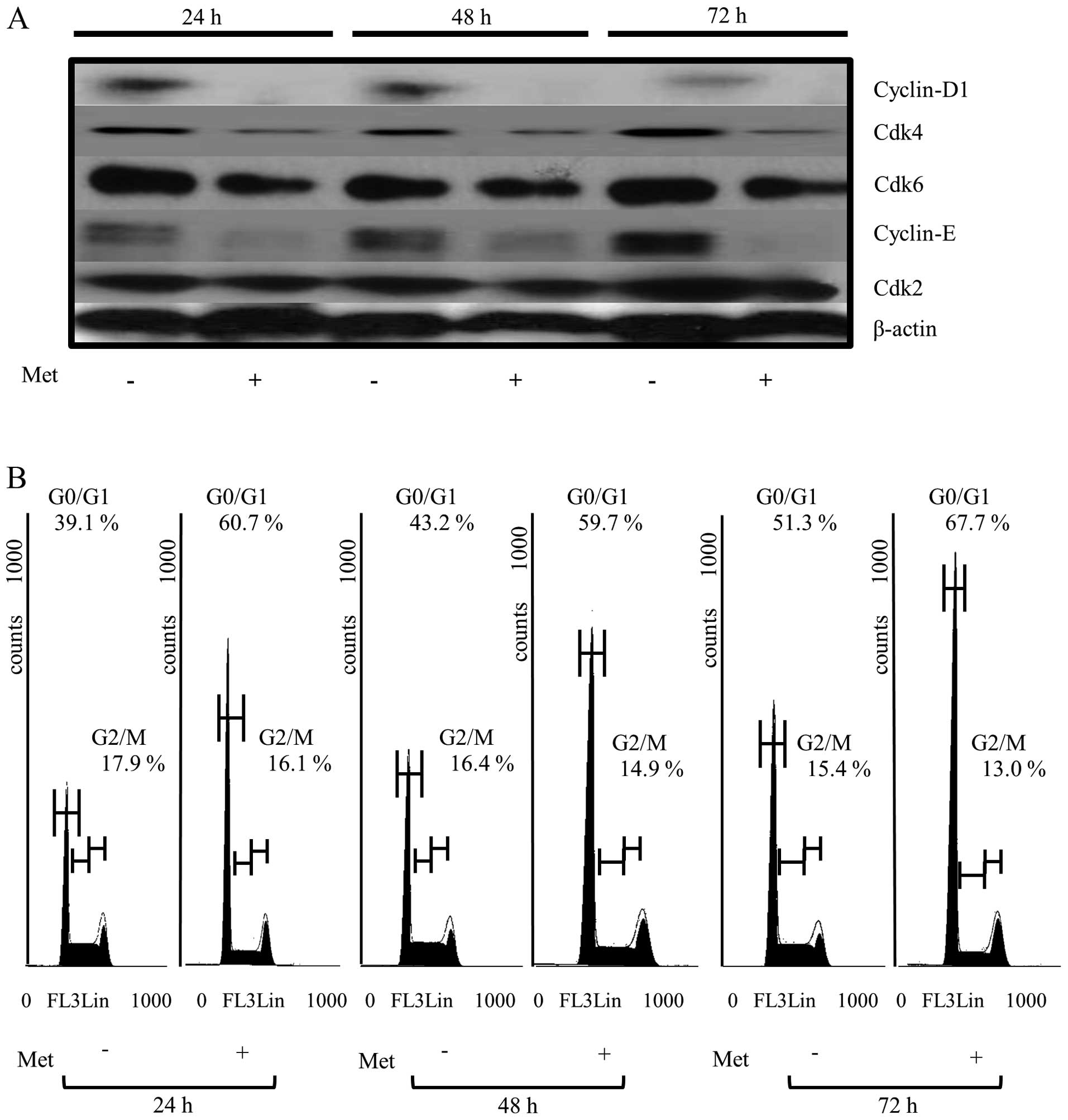
To study whether or not metformin affects the cell
cycle in Huh7 cells, we examined the expression of various cell
cycle-related molecules in Huh7 cells with and without metformin
treatment using western blot analysis. The samples were cells
treated with 10 mM metformin or left untreated for 24–72 h. The
most remarkable changes were the loss of cyclin D1, Cdk4 and cyclin
E, a key protein implicated in the transition of the G0/G1 phase.
In short, the cyclin D1, Cdk4 and cyclin E levels had already
declined rapidly at 24 h after the addition of metformin, and were
no longer detectable at 24 h (Fig.
2A).
As shown in Fig.
2A, we also studied the expression of two other cell
cycle-related proteins, Cdk6 and Cdk2, implicated in the G0/G1
transition. The results showed that the catalytic subunit of cyclin
E, Cdk2 and the catalytic subunit of cyclin D1, Cdk6 were almost
unchanged at all time points after the addition of metformin
(Fig. 2A). Similar things occurred
in other cancer cell lines, such as Alex and HLE (data not shown).
As an internal control, the amount of β-actin was also measured and
was almost the same in each sample (Fig. 2A).
Next, to further investigate the inhibition of Huh7
cell proliferation in the presence of metformin, the cell cycle
progression was examined using flow cytometry. We treated
proliferating Huh7 cells with 10 mM metformin for different
durations. After the addition of 10 mM metformin, an increasing
number of cells started to accumulate in G0/G1, 60.7% after 24 h,
59.7% after 48 h and 67.7% by 72 h (Fig. 2B). In parallel, after the addition
of 10 mM metformin, we observed reductions in the percentage of
cells in the S phase and G2/M phase. These data suggest that
metformin inhibits the cell cycle progression from G0/G1 into S
phase, resulting in G1 cell cycle arrest.
Metformin inhibits tumor proliferation in
vivo
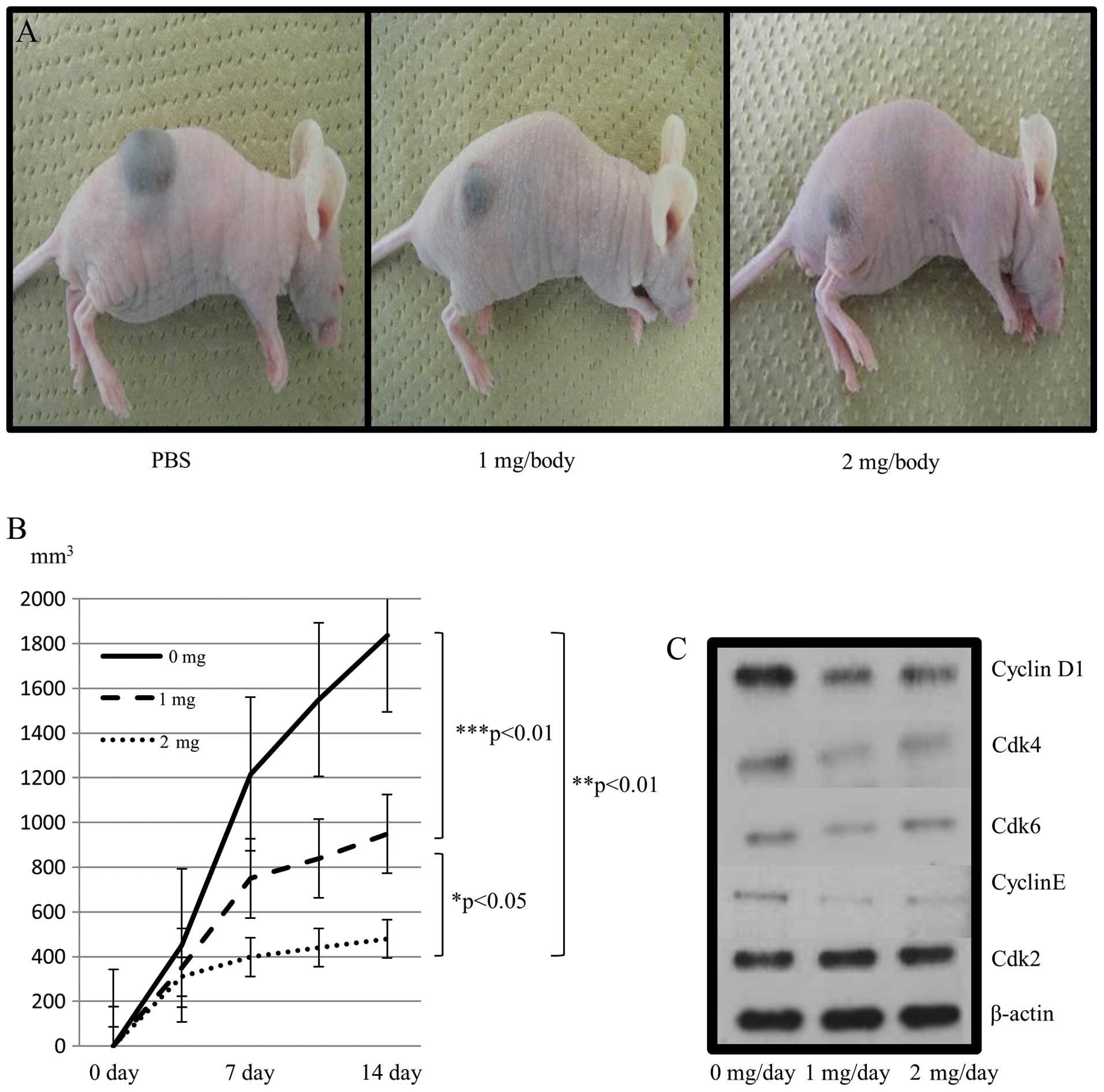
In order to determine whether metformin could affect
tumor growth in vivo, metformin was injected daily
intraperitoneally (i.p.) at 1 or 2 mg per day in xenografted mice.
Animals in the control group received i.p. administration of the
vehicle (PBS). As shown in Fig. 3A and
B, animals in the control group developed rapidly-growing
subcutaneous HCC. On the basis of the integrated values of the
tumor growth curves, i.p. administration of metformin led to a
substantial inhibition of tumor growth, by 25% (1 mg/day) and 52%
(2 mg/day) (Fig. 3A and B). These
growth rates were significantly above those of the control (both
p<0.01, respectively). In addition, 2 mg metformin treatment
significantly inhibited tumor growth compared with that in 1 mg
metformin-treated mice (p<0.05). All animals remained alive
throughout the experiment, and metformin exhibited no apparent
changes in mice and did not affect their weight (data not
shown).
To determine whether metformin also affected cell
cycle-regulatory protein levels in vivo, we performed a
western blot analysis in tumorous tissues obtained from the
xenograft experiments. Metformin (1–2 mg dose) reduced the levels
of cell cycle-related molecules (cyclin D1, Cdk4, cyclin E) in
treated tumors compared with controls (Fig. 3C). However, the expressions of Cdk2
and Cdk6 in tumorous tissue remained unchanged. These data were
similar to the results of the in vitro observation (Fig. 2A). In summary, in the in
vivo study, as in the in vitro study, metformin
decreased tumor growth by reducing cell cycle-regulatory protein
levels, especially in cyclin D1, Cdk4 and cyclin E, resulting in G1
cell cycle arrest.
Differences in phosphorylated-receptor
tyrosine kinases (p-RTKs) between metformin-treated and control
samples in vitro and in vivo
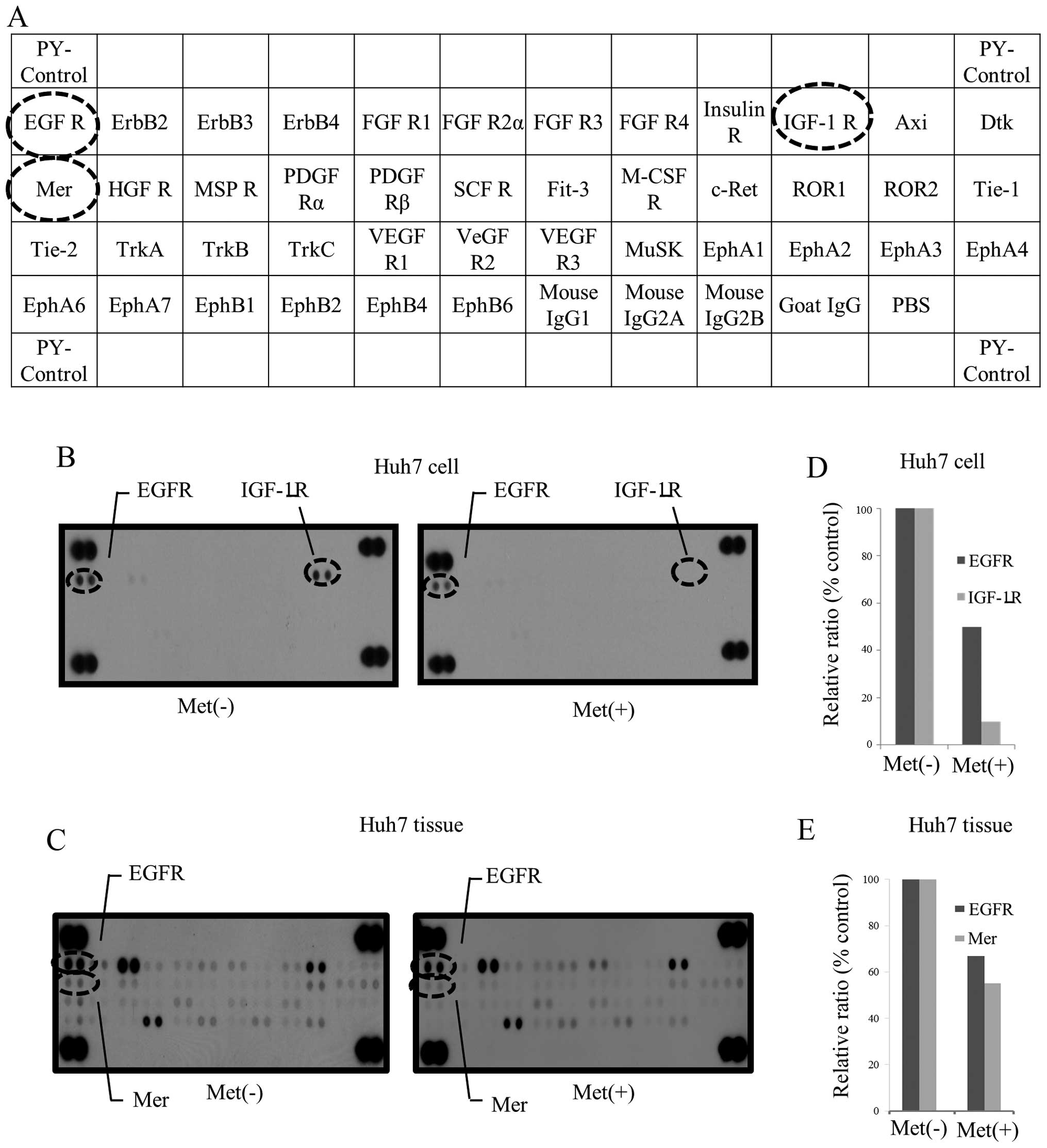
We used a phosphorylated-RTK array system to
identify the key RTKs associated with the antitumor effect of
metformin. By using an antibody array (Fig. 4A), we simultaneously screened the
expressions of 42 different activated RTKs in Huh7 cells and
tumorous tissues with or without metformin. In the in vitro
study, the expressions of phosphorylated-epidermal growth factor
(p-EGFR) and phosphorylated-insulin-like growth factor-1 receptor
(p-IGF-1R) in Huh7 cells were reduced by treatment with metformin
(Fig. 4B), while in the in
vivo study, the levels of p-EGFR and Mer in tumorous tissues
(Fig. 4C) were reduced by the
treatment with metformin. The densitometric ratios of the p-EGFR
and p-IGF-1R spots of the metformin-treated cell lines to the
non-treated cell lines were 51 and 12%, respectively (Fig. 4D). In addition, the ratios of
p-EGFR and Mer of the metformin-treated tumorous tissue to the
non-treated tissue were 67 and 55%, respectively (Fig. 4E).
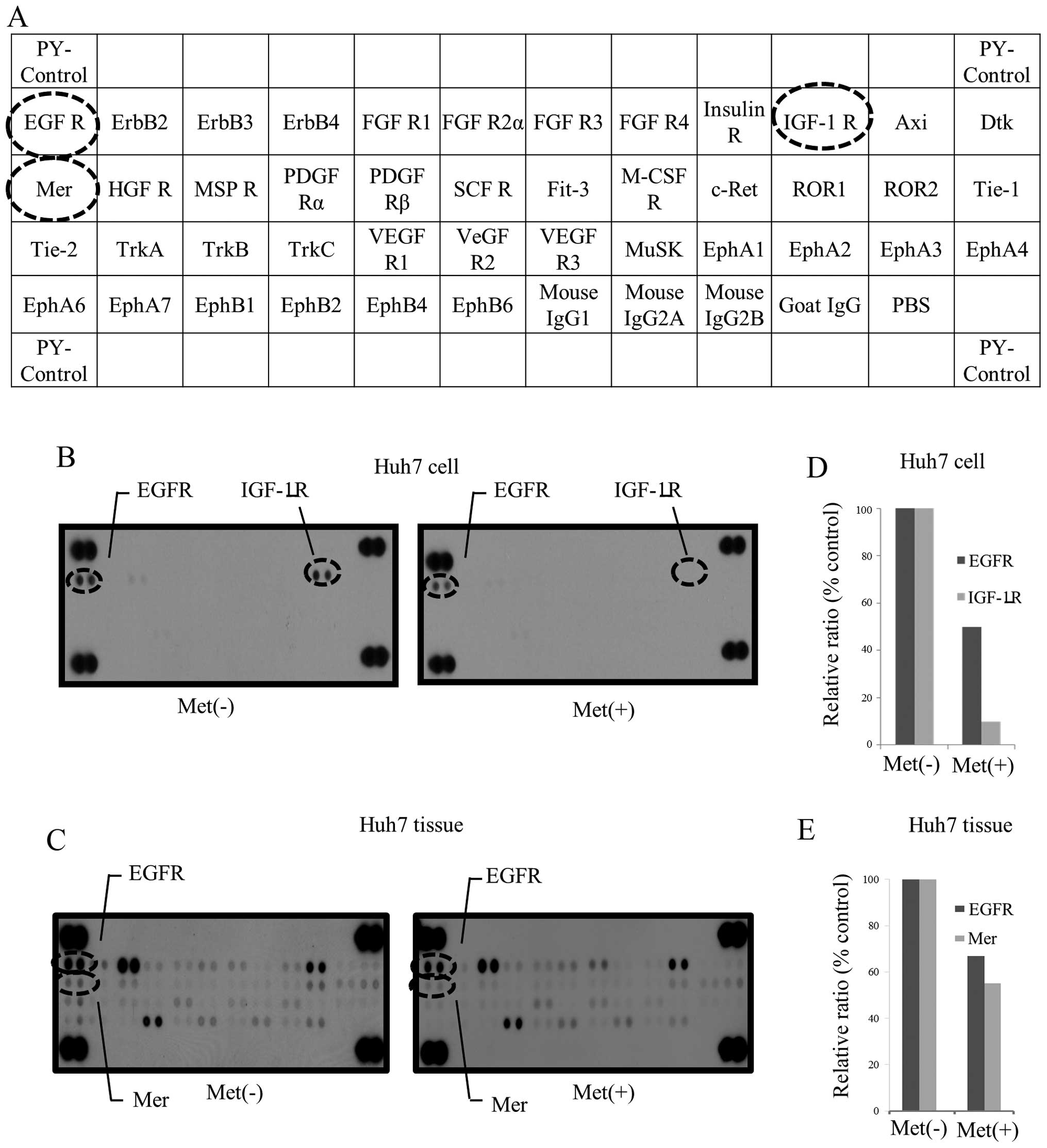 | Figure 4.(A) Template showing the location of
tyrosine kinase antibody spotted onto the RayBio Human Phospho
Array Kit. PY-Control, phospho-tyrosine positive control; EGFR,
epidermal growth factor receptor; ErbB2, v-erb-b2 erythroblastic
leukemia viral oncogene homolog 2; ErbB3, v-erb-b2 erythroblastic
leukemia viral oncogene homolog 3; ErbB4, v-erb-a erythroblastic
leukemia viral oncogene homolog 4; FGFR, fibroblast growth factor
receptor; Insulin R, insulin receptor; IGF-1R, insulin-like growth
factor I receptor; Axl, Axl receptor tyrosine kinase; Dtk,
developmental receptor tyrosine kinase; Mer, tyrosine-protein
kinase Mer; HGFR, hepatocyte growth factor receptor; MSPR,
macrophage stimulatory protein receptor; PDGFR, platelet-derived
growth factor receptor; SCFR, stem-cell factor receptor; Flt-3,
Fms-like tyrosine kinase 3; M-CSFR, macrophage colony-stimulating
factor receptor; c-Ret, receptor tyrosine kinase c-ret; ROR,
receptor tyrosine kinase-like orphan receptor; Tie, tyrosine kinase
with immunoglobulin-like and EGF-like domains; TrkA, neurotrophic
tyrosine kinase, receptor, type 1; TrkB, neurotrophic tyrosine
kinase, receptor, type 2; TrkC, neurotrophic tyrosine kinase,
receptor, type 3; VEGFR, vascular endothelial growth factor
receptor; MuSK, muscle, skeletal, receptor tyrosine kinase; Eph,
Eph receptor; PBS, phosphate-buffered saline. (B and C)
Representative expression of various p-RTKs in HCC cell lines and
tumors with or without metformin treatment. The reduced expression
levels of p-EGFR and p-IGF-1R were detected in metformin-treated
cell lines and the reduced p-EGFR and p-Mer were detacted in the
tumorous tissues obtained from xenograft animal treated with
metformin. (D) The densitometric ratios of the p-EGFR and p-IGF-1R
spots of the metformin-treated cell line to the non-treated one
were 50.1 and 7.8%, respectively. (E) The ratios of the p-EGFR and
p-Mer spots of metformin-treated tumorous tissue to the non-treated
tumorous tissue were 55.2 and 67.1%, respectively. |
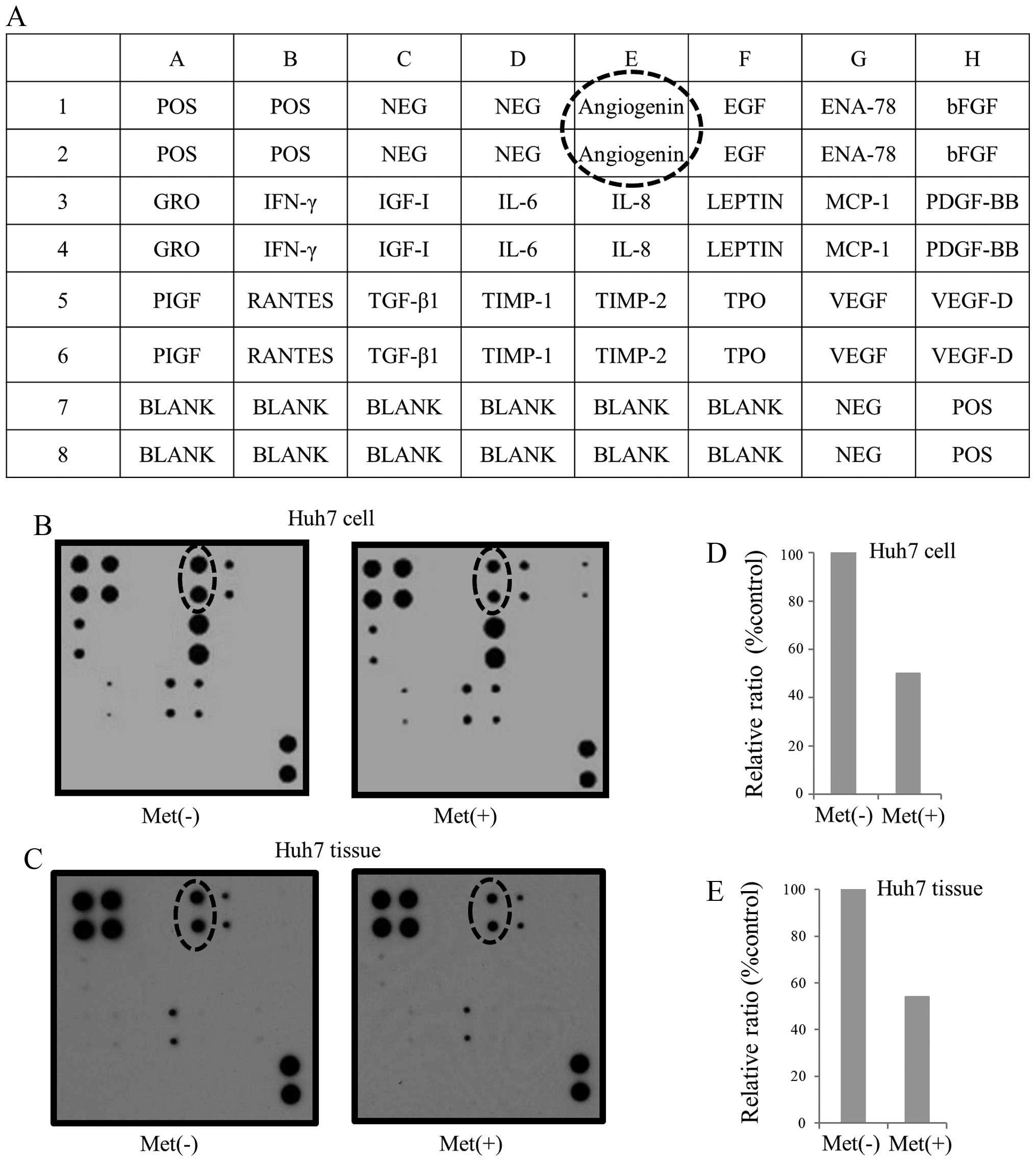
Differences in angiogenesis in vitro and
in vivo with and without metformin
We used an angiogenesis array system to identify the
key angiogenesis-related molecules associated with the antitumor
effect of metformin. The antibody array (Fig. 5A) allowed us to simultaneously
screen the expressions of 20 different angiogenesis molecules in
Huh7 cells (Fig. 5B) and tumor
tissues (Fig. 5C) with or without
metformin. Among the 20 angiogenesis molecules screened, angiogenin
was reduced in in vitro and in vivo study with
metformin treatment. The densitometric densities on angiogenin in
cell line and tumorous tissue were visualized in black and white,
respectively. The densitometric ratios of the angiogenin spots from
metformin-treated cell line and tumorous tissues to those of cell
line and tumorous tissues not treated with metformin were 51%
(Fig. 5D) and 54% (Fig. 5E).
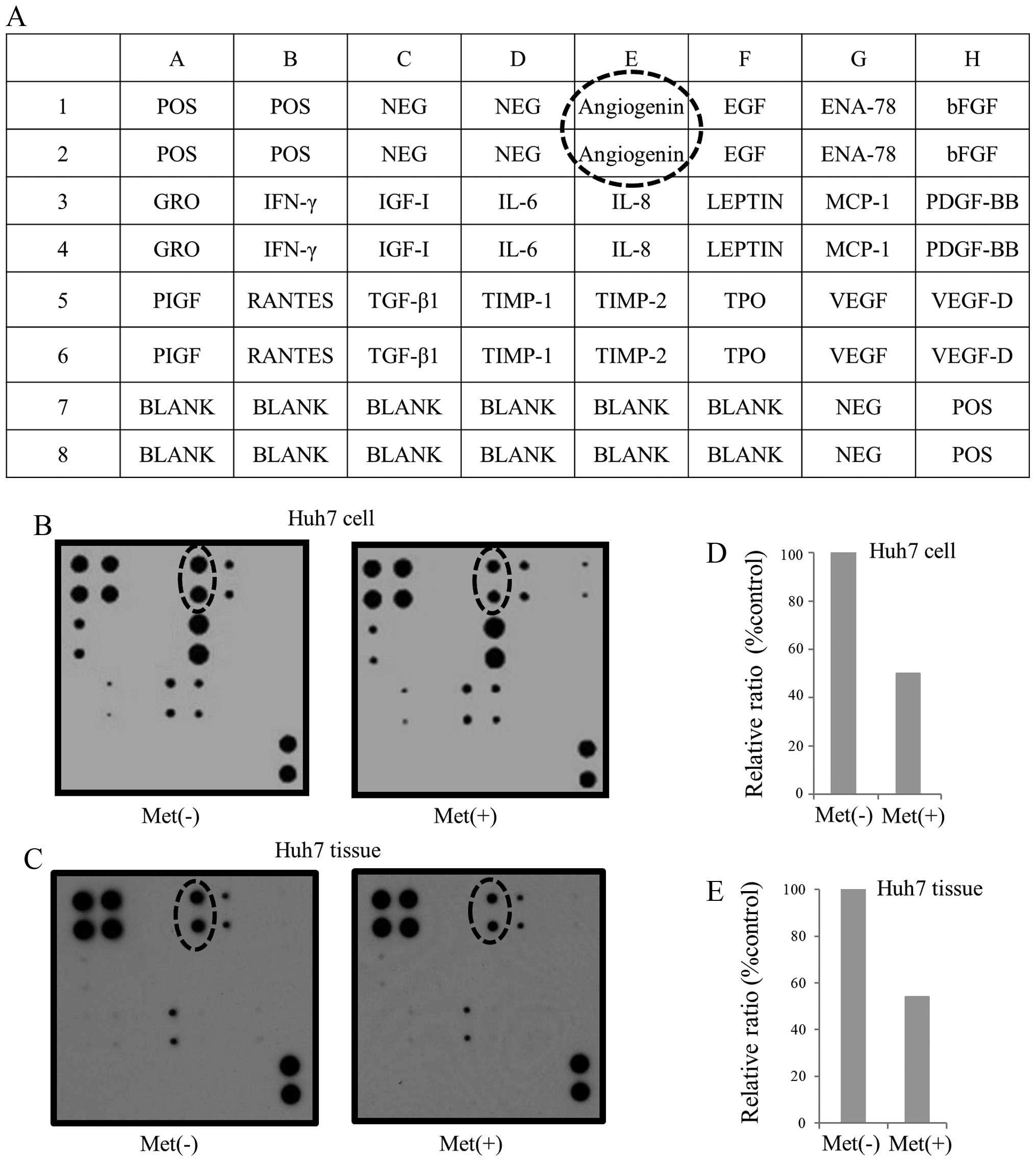 | Figure 5.(A) Template showing the location of
angiogenesis antibody spotted onto the RayBio human angiogenesis
antibody array kit. Pos, positive control; NEG, negative control;
Angiogenin, angiogenin; EGF, endothelial growth factor; ENA-78,
epithelial neutrophil-activating protein 78; bFGF, basic fibroblast
growth factor; GRO, growth related oncogene; IFN-γ, interferon γ;
IGF-1, insulin-like growth factor-I; IL-6, interleukin-6; IL-8,
interleukin-8; LEPTIN, leptin; MCP-1, monocyte chemotactic
protein-1; PDGF-BB, platelet-derived growth factor BB; PIGF, PIGF,
placental growth factor; RANTES, regulated upon activation normal T
cell expressed and presumably secreted; TGF-β1, transforming growth
factor-β1; TIMP-1, tissue inhibitor of metalloproteinase-1; TIMP-2,
tissue inhibitor of metalloproteinase-2; Thrombopoietin; VEGF,
vascular endothelial growth factor; VEGF-D, vascular endothelial
growth factor-D; BLANK, blank. (B and C) Representative expression
of various angiogenic molecules in Huh7 cell lines and tumors with
or without metformin treatment, respectively. A reduction in
angiogenin was detected in metformin-treated cell lines and tumors.
(D) The densitometric ratio of the angiogenin spots of the
metformin-treated cell line to the non-treated one was 52.1%. (E)
The ratio of the angiogenin of tumorous tissue of nude mice with
metformin-treatment to non-treated tissue was 54.0%. |
Differences in miRNA expression between
the metformin-treated and control cell lines
Using a custom microarray platform, we analyzed the
expression levels of 985 human miRNA probes in the cell lines
treated with metformin and the control cell line. As shown in
Table I, when the expression of
miRNAs was studied in Huh7 cells treated with 10 mM metformin and
without metformin in vitro, 33 of 985 miRNAs were
significantly upregulated in Huh7 cells at 72 h after metformin
treatment (Table I), while 18 of
985 miRNAs downregulated (Table
II).
 | Table I.Statistical results and chromosomal
of miRNAs upregulated in Huh7 cells treated with metformin. |
Table I.
Statistical results and chromosomal
of miRNAs upregulated in Huh7 cells treated with metformin.
| miRNAs | Fold (treated/non
-treated) mean ± SD | P-value | Chromosomal
localization |
|---|
| hsa-miR-1304 | 2.29±0.75 | 0.0307 | 15q21.2 |
| hsa-miR-1270 | 2.24±0.91 | 0.0095 | 19 |
| hsa-miR-324-5p | 1.98±0.69 | 0.0228 | 17p13.1 |
|
hsa-miR-125a-5p | 1.95±0.12 | 0.0096 | 19q13.41 |
| hsa-miR-23a | 1.87±0.08 | 0.0055 | 19p13.13 |
| hsa-let-7a | 1.82±0.34 | 0.0099 | 9q22.32 |
| hsa-miR-3143 | 1.81±0.36 | 0.0411 | 6 |
|
hsa-miR-3607-5p | 1.78±0.26 | 0.0034 | 5 |
| hsa-miR-1178 | 1.76±0.20 | 0.0204 | 12q24.23 |
| hsa-miR-181a | 1.75±0.24 | 0.0047 | 1q32.1 |
| hsa-miR-99b | 1.74±0.13 | 0.0099 | 19q13.41 |
| hsa-miR-142-3p | 1.74±0.42 | 0.0147 | 17q22 |
| hsa-let-7e | 1.74±0.18 | 0.0066 | 19q13.41 |
| hsa-miR-27a | 1.72±0.19 | 0.0061 | 19p13.13 |
| hsa-miR-502-5p | 1.69±0.37 | 0.0248 | Xp11.23 |
| hsa-miR-23b | 1.68±0.40 | 0.0229 | 9q22.32 |
| hsa-miR-563 | 1.67±0.44 | 0.0156 | 3p25.1 |
| hsa-miR-181d | 1.65±0.11 | 0.0363 | 19q13.13 |
| hsa-miR-29a | 1.64±0.36 | 0.0443 | 7q32.3 |
| hsa-miR-612 | 1.64±0.17 | 0.0346 | 11q13.1 |
| hsa-miR-551b | 1.64±0.40 | 0.0368 | 3q26.2 |
|
hsa-miR-3616-3p | 1.63±0.20 | 0.0095 | 20 |
| hsa-miR-34a | 1.58±0.17 | 0.0162 | 1p36.22 |
| hsa-miR-185 | 1.56±0.21 | 0.0152 | 22q11.21 |
| hsa-miR-613 | 1.54±0.16 | 0.0193 | 12p13.1 |
| hsa-miR-378 | 1.54±0.06 | 0.0007 | 5q32 |
| hsa-miR-21* | 1.53±0.36 | 0.0259 | 17q23.1 |
| hsa-miR-181b | 1.51±0.24 | 0.0221 | 1q32.1 |
| hsa-miR-26a | 1.51±0.25 | 0.0083 | 3q22.2 |
| hsa-miR-3649 | 1.51±0.22 | 0.0488 | 12 |
| hsa-miR-455-3p | 1.51±0.04 | 0.0045 | 9q32 |
| hsa-miR-449a | 1.5±0.33 | 0.0263 | 5q11.2 |
| hsa-miR-24 | 1.5±0.03 | 0.0094 | 9q22.32 |
 | Table II.Statistical results and chromosomal
of miRNAs downregulated in Huh7 cells treated with metformin. |
Table II.
Statistical results and chromosomal
of miRNAs downregulated in Huh7 cells treated with metformin.
| miRNAs | Fold
(treated/non-treated) mean ± SD | P-value | Chromosomal
localization |
|---|
| hsa-miR-518f | 0.35±0.07 | 0.0485 | 19q13.42 |
| hsa-miR-1180 | 0.42±0.20 | 0.0460 | 17 |
| hsa-miR-3686 | 0.43±0.14 | 0.0372 | 8 |
| hsa-miR-217 | 0.48±0.23 | 0.0494 | 2p16.1 |
| hsa-miR-553 | 0.49±0.12 | 0.0031 | 1p21.2 |
| hsa-miR-4296 | 0.53±0.12 | 0.0225 | 10 |
|
hsa-miR-3689a-5p | 0.54±0.21 | 0.0391 | 9 |
| hsa-miR-4295 | 0.55±0.09 | 0.0200 | 10 |
| hsa-miR-1203 | 0.58±0.05 | 0.0111 | 17 |
| hsa-miR-302b | 0.59±0.07 | 0.0327 | 4q25 |
| hsa-miR-943 | 0.60±0.16 | 0.0443 | 4p16.3 |
| hsa-miR-551b* | 0.61±0.14 | 0.0066 | 3q26.2 |
|
hsa-miR-3663-5p | 0.65±0.12 | 0.0220 | 10 |
| hsa-miR-1307 | 0.72±0.05 | 0.0110 | 10 |
| hsa-miR-130b | 0.74±0.02 | 0.0283 | 22 |
| hsa-miR-1227 | 0.76±0.11 | 0.0411 | 19 |
| hsa-miR-658 | 0.79±0.07 | 0.0157 | 22q13.1 |
| hsa-miR-126* | 0.87±0.07 | 0.0312 | 9q34.3 |
Unsupervised hierarchical clustering analysis, using
Pearson’s correlation, showed that cell lines treated with
metformin clustered together and separately from the untreated cell
lines (Fig. 6). These subsets of
119 microRNAs in cell lines exhibited >1.5-fold alterations in
expression levels between the metformin-treated and control
groups.
Discussion
HCC is the sixth most common malignancy and the
third most common cause of cancer-related death worldwide (1). Conventional chemotherapy does not
provide significant clinical benefits or prolonged survival for
patients with advanced HCC (23).
Therefore, it is necessary to identify new therapies for the
treatment of HCC.
The role of the anti-diabetic drug metformin in
glucose and fatty acid metabolism is very well known (20,22).
Recent data suggest that metformin was shown to protect from cancer
and inhibit the proliferation of various human cancer cell types,
such as those of the prostate (6),
breast (7), colon (8,9),
stomach (10), and esophagus
(11) and HCC (12). However, the antitumor mechanism of
metformin in various cancers, including hepatocellular carcinoma
(HCC), has not been fully clarified. Here we show that metformin
inhibits the growth of HCC cells and tumorigenesis in vitro and in
vivo. In addition, we have identified miRNAs, receptor-type
tyrosine kinase and angiogenesis molecules associated with the
antitumor effect of metformin in HCC.
In the present study, metformin led to a strong,
dose-dependent inhibition of cell proliferation in all HCC cell
lines. However, to our surprise, metformin did not inhibit the
proliferation of normal hepatocytes. These data suggest that
metformin exhibits an anti-proliferation effect on HCC cells, but
does not have an anti-proliferation effect on normal hepatocytes.
These results suggest that metformin would be very effective for
HCC treatment, since it specifically suppressed the proliferation
in cancer cells, but not in normal cells.
In previous reports, downregulation of cyclin D1 in
response to metformin has been demonstrated in various cancer cell
lines (8,9). We have also reported that cyclin D1
was reduced in gastric cancer cells treated with metformin in
vitro. In the present study, we have also shown that the major
cell cycle regulators (cyclin D1, Cdk4 and cyclin E) could be
intracellular targets of the metformin-mediated anti-proliferative
effect in HCC. To be sure, flow cytometry also revealed that
metformin arrested HCC cells at the G0/G1 phase in
vitro.
An in vivo experiment using subcutaneous
HCC-bearing athymic nude mice also demonstrated that metformin
markedly suppressed the growth of HCC, and the expression levels of
numerous cell cycle-related molecules (cyclin D1, Cdk4, cyclin E)
were found to be reduced by treatment with metformin, indicating
that metformin may inhibit the expression of cell cycle-related
molecules. These data suggest that the antitumor effect of
metformin may be related to the role of G1 arrest of HCC cells.
Our in vitro study was performed using a
higher dose of metformin than the human therapeutic concentration
(6 to 30 μM). This has been a previously raised criticism of
similar work in other cancer cell types, such as the prostate
(6), breast (7), colon (8,9),
stomach (10), and esophagus
(11) and HCC (12). However, it is important to consider
that cells in culture are grown under hyperglycemic conditions
(24). Tissue culture media alone
contains high concentrations of glucose, and 5–10% fetal bovine
serum is typically added, resulting in excessive growth
stimulation. This may explain why the doses of metformin required
to realize the antitumor effects in a cell culture system are
higher than those used in diabetic patients.
Metformin leads to changes in various protein
phosphorylation. In the present study, we have shown that metformin
reduced the activation of the EGFR, IGF-1R and Mer in vitro
and/or in vivo. In regard to p-EGFR and p-IGF-1R, some
studies (1,2), including a report by our group
(23), have also reported that
metformin reduced the expression of p-EGFR and p-IGF-1R in breast
(24), pancreas (26) and gastric cancer (10,25).
However, to date, there have been no reports in which metformin
inhibited Mer activation. The upregulation of Mer is detected in
various cancers (27,28). Mer prevents apoptosis without
stimulating proliferation (28),
whereas it increases without inhibiting apoptosis (29). The mechanism of metformin’s
anti-proliferation effect in cancer cells may occur through
inactivation of Mer. In addition, our studies suggest that
metformin may reduce the expression levels of p-EGFR, p-IGFR and
p-Mer in many cancers, including HCC and their molecules may become
the new target factor of the treatment in HCC. In addition, the
pathway of EGFR and IGF-1R plays a role in controlling cell cycle
events. EGFR and IGF-R1 are upregulated by many proteins involved
in cell cycle progression, such as cyclin D1 and Cdk4. Therefore,
metformin blocked the cell cycle in G0/G1 in vitro and in
vivo through the reduction of the activity of EGFR and
IGF-1R.
In the present study, metformin was found to reduce
only angiogenin out of 20 angiogenesis-related proteins in an
analysis using a protein array. Angiogenin is not only related to
angiogenesis, but also possesses the ability to promote cell growth
(30). In addition, some previous
reports (31) have shown that
enhanced expression of angiogenin is associated with the
progression of HCC. These data suggest that the antitumor effect of
metformin may be due to a reduction of angiogenin.
To identify miRNAs associated with the antitumor
effect of metformin, we used a miRNA expression array and measured
the variations in miRNA profiles in HCC cell lines in culture
treated with metformin compared to those not treated with
metformin. The cluster analyses we performed clearly demonstrated
that metformin treatment affects the extent of miRNA expression in
cultured cells. In the analyses, we selected sets of miRNAs for
which the expression levels were altered significantly before and
after metformin treatment. We identified 51 miRNAs differentially
expressed (33 upregulated and 18 downregulated) in culture. These
miRNAs are meaningful candidates to gauge the effectiveness of
metformin treatment and to provide clues to the molecular basis of
metformin’s anticancer effects, particularly when mediated with
miRNAs.
We found that members of the let-7 family (let-7a,
let-7b and let-7e) are upregulated in cultured cells treated with
metformin. The human let-7 family contains 13 members and is widely
recognized as a class of miRNAs producing a tumor-suppressing
effect (32). Consistent with this
event, downregulation of let-7 family members has been reported in
many cancers, such as lung (33),
breast (34), colorectal cancer
(35), melanoma (36), gastric cancer (10) and HCC (37). The let-7 family acts as a tumor
suppressor by binding its target oncogenes, including Ras (38), HMGA2 (39) and c-Myc (40). Therefore, the downregulated let-7
plays an important role in the development of various cancers,
including HCC. Collectively, these findings suggest that the
suppression of cancer cell proliferation by metformin may be at
least partly due to the upregulation of let-7a, let-7b and
let-7e.
In the present study, metformin treatment resulted
in altered expression of a surprising number of diverse miRNAs. The
miRNAs upregulated in HCC cells treated with metformin included
miRNAs that are overexpressed in HCC, such as miR-23a, miR-27A,
miR-34a, miR-21, miR-24 and miR-324-5p, and miRNAs that are reduced
in HCC, such as miR-7a, miR-7b and miR-7e, miR-23b, miR-29a,
miR-26a, miR-81a, miR-142-3p and miR-378 (41,42).
We speculate that the former group of miRNAs may be involved in
survival responses that are altered in malignant cells, whereas the
latter group may reflect the general cellular responses to
death-inducing stimuli. However, additional detailed studies will
be needed to assess whether or not each miRNA reflects a cause or a
consequence of exposure to metformin treatment.
In conclusion, our results revealed that metformin
inhibits human HCC cell proliferation and tumor growth, possibly by
suppressing the cell cycle-related molecules via alteration of
miRNAs. Metformin is a drug widely used for the treatment of type 2
diabetes with limited side-effects. Therefore, metformin may become
a novel and effective therapy for the treatment and long-term
management of HCC, providing additional benefits at low cost.
Abbreviations
Abbreviations:
|
miRNA
|
microRNA
|
|
Cdk
|
cyclin-dependent kinase;
|
|
PBS
|
phosphate-buffered saline;
|
|
HCC
|
hepatocellular carcinoma
|
References
|
1.
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar
|
|
2.
|
Venook AP, Papandreou C, Furuse J and de
Guevara LL: The incidence and epidemiology of hepatocellular
carcinoma: A global and regional perspective. Oncologist. 15:5–13.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Witters LA: The blooming of the French
lilac. J Clin Invest. 108:1105–1107. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Barriere G, Tartary M and Rigaud M:
Metformin: A rising star to fight the epithelial mesenchymal
transition in oncology. Anticancer Agents Med Chem. 13:333–340.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Lee MS, Hsu CC, Wahlqvist ML, Tsai HN,
Chang YH and Huang YC: Type 2 diabetes increases and metformin
reduces total, colorectal, liver and pancreatic cancer incidences
in taiwanese: A representative population prospective cohort study
of 800,000 individuals. BMC Cancer. 11:202011. View Article : Google Scholar
|
|
6.
|
Ben Sahra I, Laurent K, Loubat A, et al:
The antidiabetic drug metformin exerts an antitumoral effect in
vitro and in vivo through a decrease of cyclin D1 level. Oncogene.
27:3576–3586. 2008.PubMed/NCBI
|
|
7.
|
Brown KA, Hunger NI, Docanto M and Simpson
ER: Metformin inhibits aromatase expression in human breast adipose
stromal cells via stimulation of AMP-activated protein kinase.
Breast Cancer Res Treat. 123:591–596. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Hosono K, Endo H, Takahashi H, et al:
Metformin suppresses azoxymethane-induced colorectal aberrant crypt
foci by activating AMP-activated protein kinase. Mol Carcinog.
49:662–671. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Zhou XZ, Xue YM, Zhu B and Sha JP: Effects
of metformin on proliferation of human colon carcinoma cell line
SW-480. Nan Fang Yi Ke Da Xue Xue Bao. 30:1935–1938. 2010.(In
Chinese).
|
|
10.
|
Kato K, Gong J, Iwama H, et al: The
antidiabetic drug metformin inhibits gastric cancer cell
proliferation in vitro and in vivo. Mol Cancer Ther. 11:549–560.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Kobayashi M, Kato K, Iwama H, et al:
Antitumor effect of metformin in esophageal cancer: In vitro
study. Int J Oncol. 42:517–524. 2012.PubMed/NCBI
|
|
12.
|
Qu Z, Zhang Y, Liao M, Chen Y, Zhao J and
Pan Y: In vitro and in vivo antitumoral action of metformin on
hepatocellular carcinoma. Hepatol Res. 42:922–933. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Landgraf P, Rusu M, Sheridan R, et al: A
mammalian microRNA expression atlas based on small RNA library
sequencing. Cell. 129:1401–1414. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Ji J, Yamashita T, Budhu A, et al:
Identification of microRNA-181 by genome-wide screening as a
critical player in EpCAM-positive hepatic cancer stem cells.
Hepatology. 50:472–480. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Callegari E, Elamin BK, Giannone F, et al:
Liver tumorigenicity promoted by microRNA-221 in a mouse transgenic
model. Hepatology. 56:1025–1033. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Masaki T, Shiratori Y, Rengifo W, et al:
Hepatocellular carcinoma cell cycle: Study of long-evans cinnamon
rats. Hepatology. 32:711–720. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Masaki T, Shiratori Y, Rengifo W, et al:
Cyclins and cyclin-dependent kinases: Comparative study of
hepatocellular carcinoma versus cirrhosis. Hepatology. 37:534–543.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Masaki T, Tokuda M, Yoshida S, et al:
Comparison study of the expressions of myristoylated alanine-rich C
kinase substrate in hepatocellular carcinoma, liver cirrhosis,
chronic hepatitis, and normal liver. Int J Oncol. 26:661–671.
2005.
|
|
19.
|
Bradford MM: A rapid and sensitive method
for the quantitation of microgram quantities of protein utilizing
the principle of protein-dye binding. Anal Biochem. 72:248–254.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Towbin H, Staehelin T and Gordon J:
Electrophoretic transfer of proteins from polyacrylamide gels to
nitrocellulose sheets: Procedure and some applications. Proc Natl
Acad Sci USA. 76:4350–4354. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Workman P, Aboagye EO, Balkwill F, et al:
Guidelines for welfare and use of animals in cancer research. Br J
Cancer. 102:1555–1577. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
D’Incalci M, Colombo T, Ubezio P, et al:
The combination of yondelis and cisplatin is synergistic against
human tumor xenografts. Eur J Cancer. 39:1920–1926. 2003.
|
|
23.
|
Masaki T, Morishita A, Kurokohchi K and
Kuriyama S: Multidisciplinary treatment of patients with
hepatocellular carcinoma. Expert Rev Anticancer Ther. 6:1377–1384.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Liu B, Fan Z, Edgerton SM, Deng XS,
Alimova IN, Lind SE and Thor AD: Metformin induces unique
biological and molecular responses in triple negative breast cancer
cells. Cell Cycle. 8:2031–2040. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Gong J, Morishita A, Kurokohchi K, et al:
Use of protein array to investigate receptor tyrosine kinases
activated in gastric cancer. Int J Oncol. 36:101–106.
2010.PubMed/NCBI
|
|
26.
|
Wang LW, Li ZS, Zou DW, Jin ZD, Gao J and
Xu GM: Metformin induces apoptosis of pancreatic cancer cells.
World J Gastroenterol. 14:7192–7198. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Verma A, Warner SL, Vankayalapati H,
Bearss DJ and Sharma S: Targeting Axl and Mer kinases in cancer.
Mol Cancer Ther. 10:1763–1773. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Guttridge KL, Luft JC, Dawson TL,
Kozlowska E, Mahajan NP, Varnum B and Earp HS: Mer receptor
tyrosine kinase signaling: Prevention of apoptosis and alteration
of cytoskeletal architecture without stimulation or proliferation.
J Biol Chem. 277:24057–24066. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Sainaghi PP, Castello L, Bergamasco L,
Galletti M, Bellosta P and Avanzi GC: Gas6 induces proliferation in
prostate carcinoma cell lines expressing the axl receptor. J Cell
Physiol. 204:36–44. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Li S and Hu GF: Angiogenin-mediated rRNA
transcription in cancer and neurodegeneration. Int J Biochem Mol
Biol. 1:26–35. 2010.
|
|
31.
|
Hisai H, Kato J, Kobune M, et al:
Increased expression of angiogenin in hepatocellular carcinoma in
correlation with tumor vascularity. Clin Cancer Res. 9:4852–4859.
2003.PubMed/NCBI
|
|
32.
|
Boyerinas B, Park SM, Hau A, Murmann AE
and Peter ME: The role of let-7 in cell differentiation and cancer.
Endocr Relat Cancer. 17:F19–F36. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Takamizawa J, Konishi H, Yanagisawa K, et
al: Reduced expression of the let-7 microRNAs in human lung cancers
in association with shortened postoperative survival. Cancer Res.
64:3753–3756. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
Yu F, Yao H, Zhu P, et al: Let-7 regulates
self renewal and tumorigenicity of breast cancer cells. Cell.
131:1109–1123. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35.
|
Akao Y, Nakagawa Y and Naoe T: Let-7
microRNA functions as a potential growth suppressor in human colon
cancer cells. Biol Pharm Bull. 29:903–906. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36.
|
Fu TY, Chang CC, Lin CT, Lai CH, Peng SY,
Ko YJ and Tang PC: Let-7b-mediated suppression of basigin
expression and metastasis in mouse melanoma cells. Exp Cell Res.
317:445–451. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Zhu XM, Wu LJ, Xu J, Yang R and Wu FS:
Let-7c microRNA expression and clinical significance in
hepatocellular carcinoma. J Int Med Res. 39:2323–2329. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
38.
|
Johnson SM, Grosshans H, Shingara J, et
al: RAS is regulated by the let-7 microRNA family. Cell.
120:635–647. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Lee YS and Dutta A: The tumor suppressor
microRNA let-7 represses the HMGA2 oncogene. Genes Dev.
21:1025–1030. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40.
|
Osada H and Takahashi T: Let-7 and
miR-17-92: Small-sized major players in lung cancer development.
Cancer Sci. 102:9–17. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41.
|
Haybaeck J, Zeller N and Heikenwalder M:
The parallel universe: MicroRNAs and their role in chronic
hepatitis, liver tissue damage and hepatocarcinogenesis. Swiss Med
Wkly. 141:w132872011.PubMed/NCBI
|
|
42.
|
Borel F, Konstantinova P and Jansen PL:
Diagnostic and therapeutic potential of miRNA signatures in
patients with hepatocellular carcinoma. J Hepatol. 56:1371–1383.
2012. View Article : Google Scholar : PubMed/NCBI
|