Cutaneous melanoma, is a form of aggressive cancer
that develops from melanocytes. It is most common in people between
30 and 60 years of age. The highest incidence rates occurs in
white-skinned peoples living at low latitudes (1). Accordingly, the association between
sun exposure and melanoma have been explored. An important risk
factor for melanoma is UV irradiation upon sun exposure (2). Indication of a direct UV mutagenic
effect in melanoma development remains controversial as the
nucleotide exchange detected in the B-RAF gene (T/A) is not
classically linked to UV mutagenesis signature attributable to
cytidine to thymidine (C→T) transitions. As suggested, it is
possible that B-RAF mutations could arise from error prone
replication of UV-damaged DNA (3).
Melanoma is a heterogeneous disease that presents different genetic
alterations and variety of histologic subtypes (4). B-RAF mutations were commonly
detected in cutaneous melanomas arising from intermittent
sun-exposed sites (5).
Accordingly, we have, recently, identified a higher frequency of
B-RAFV600E mutation in melanoma of the trunk from
indoor workers compared to outdoor workers, suggesting that this
mutation may be associated with an intermittent exposure to the
sun, as usually the trunk is a sun-protected body site (6).
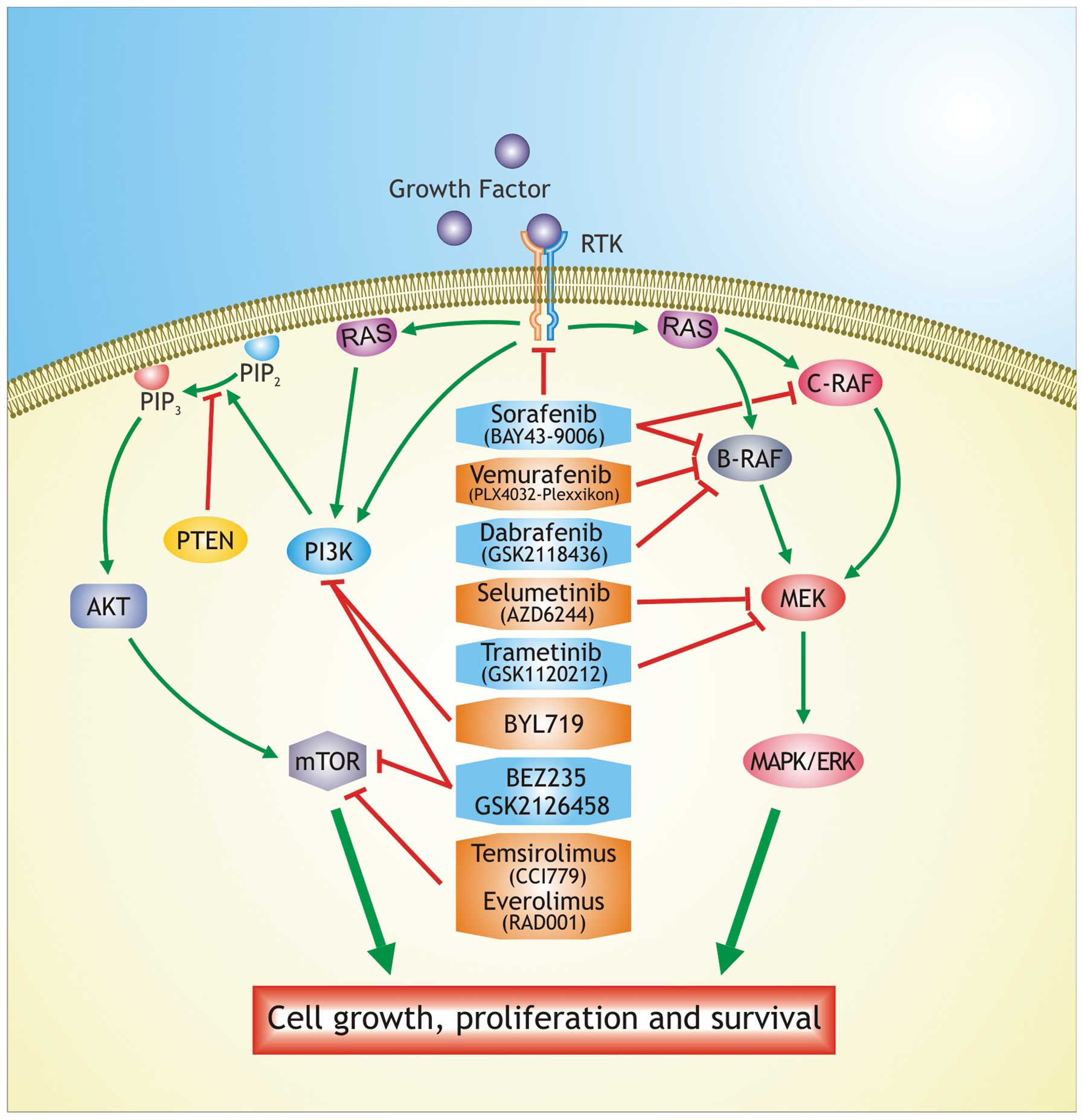
Melanomas exhibit mutations in the Ras/Raf/mitogen
activated protein kinase (MAPK) pathway. Over 50% of melanomas
harbor activating mutations in B-RAF gene
(B-RAFV600E) (7,8),
known to play a key role in proliferation and survival of melanoma
cells through activation of the MAPK pathway (9). Furthermore, this mutation causes
constitutive activation of the kinase as well as insensitivity to
negative feedback mechanism (10).
B-RAFV600E, B-RAFV600K,
B-RAFV600R and B-RAFV600D
mutations were detected at the frequency from 6 to 3% (7). Knowledge on the deregulation of MAPK
and P3K pathways in different cancer types, including melanoma, has
led to the development of specific inhibitors of their key
components (11–14) (Fig.
1).
A list of current clinical trials for melanoma is
available on the NCI Web site (http://www.cancer.gov/clinicaltrials). For stage IV
(TNM) melanoma we found a total of 281 ongoing clinical trials.
Most of these studies are evaluating whether any benefits are
observed after treatment with novel combination therapies or
tailored therapies compared to standard treatments. In Table I the MAPK/AKT inhibitors with their
targets are summarized. The prognosis for melanoma patients at
early stage of the disease is 90% survival by surgical treatment.
In contrast, the prognosis for advanced melanoma is restricted due
to the development of drug resistance after treatment with
chemotherapeutic agents (15).
This review is focused on the clinical application for the
treatment of melanoma with MAPK and AKT inhibitors and other novel
therapies. Mechanisms of resistance for each therapy are also
discussed.
Sorafenib (BAY43-9006, Nexavar, Bayer
Pharmaceuticals Corp., West Haven, CT, USA) is a potent
multi-kinase inhibitor that targets also the receptor tyrosine
kinase-associated angiogenesis (VEGFR-2, VEGFR-3, PDGF-β) and tumor
progression (c-KIT, FLT-3) (16,17).
Sorafenib was initially developed as an inhibitor of the RAF
serine/threonine kinases and administered orally in combination
with carboplatin and taxol in patients with lung cancer (10).
The study of this inhibitor in xenograft models
showed that sorafenib inhibited tumor cell proliferation and/or
endothelial cell mediated tumor angiogenesis in several forms of
human cancer (18). Sorafenib
administered as monotherapy has a manageable side effect profile in
phase I/II/III studies (19–21)
and the most common toxic effects are hand-foot skin reaction
(HFS), rash and diarrhoea (22).
Sorafenib is effective in the treatment of a small percentage of
melanomas that carry mutations G469E and D594G in B-RAF gene
expressing constitutively ERK1/2, low levels of MEK. However, it
did not show significant benefit in melanoma patients harboring
B-RAFV600E mutation (23). It was suggested that a receptor
kinase upstream of Ras/Raf/MEK/ERK cascade may be targeted by
sorafenib (24). This inhibitor
may be administered in combination with an inhibitor of MEK in the
treatment of more aggressive forms of melanoma. It may target the
VEGF and other membrane receptors expressed in cancer cells,
whereas the MEK inhibitor blocks the cascade which is abnormally
activated by B-RAF (25).
The sorafenib dose (400 mg b.i.d) is administered in combination
with standard chemotherapy, such as dacarbazine, in patients with
advanced melanoma because it has few side effects as a single
agent, indeed the response rate was 21% with a median time from
treatment initiation of 2.3 months (26). Although this combination does not
cause toxic effects and shows antitumor activity, it is not applied
in clinical practice because selective inhibitors of B-RAF
are more effective in the treatment of malignant melanoma (27).
Vemurafenib (Zelboraf, Plexxikon/Roche) was approved
first by the FDA in USA, in August 2011, for the treatment of
patients with metastatic melanoma with B-RAFV600E
mutation and then in Europe (15).
Vemurafenib (PLX4032) is a potent oral drug that inhibits the
kinase domain of the most common mutation of B-RAF
(B-RAFV600E), decreasing cell proliferation
through the phosphorylation of ERK and cyclin D1 (28,29),
but it does not have antitumor effects against cells with
B-RAFWT (30,31).
The pharmacodynamic analysis reported that the
activity of vemurafenib was characterized as exposure-dependent
tumor response corresponding with percentage of inhibition of MEK
and ERK phosphorylation. Additionally, the relationship between
dose exposure and response suggests that melanoma regression was
found to correlate with >90% inhibition of ERK phosphorylation
(32).
Dabrafenib (GSK2118436) is a reversible
ATP-competitive inhibitor that selectively inhibits B-RAF.
It is similar to vemurafenib concerning the mechanism of action,
pharmacodynamics, timing of responses and development of
resistance, but it presents a shorter half-life (44). Dabrafenib is efficient in about
50–70% of patients with B-RAFV600E or
B-RAFV600K mutations (45,46).
A phase I/II study of dabrafenib established a dose
of 150 mg twice daily and reported positive responses in about 50%
of the patients with advanced melanoma and a median
progression-free survival of 6-3 months (47). The most common cutaneous side
effects were hyperkeratosis, papillomas and palmar-plantar
erythrodysaesthesia; other side effects were pyrexia, fatigue,
headache and arthralgia, which together necessitated dose
reductions (48).
In a phase III study, comparing dabrafenib vs.
dacarbazine, it has been demonstrated that the response rates were
53 vs. 19% and PFS 5.3 vs. 2.7, although the trial allowed
crossover and was not powered to detect an overall survival benefit
(49,50). The low rate of survival benefit was
partly due to the obligatory crossover to dabrafenib at progression
in patients randomly assigned to dacarbazine (29).
MEK proteins belong to a family of enzymes, that
selectively phosphorylate serine/threonine and tyrosine residues
within the activation loop of their specific MAP kinase substrates.
MEK1 and MEK2 display a similar structural organization, are
closely related and they participate in the Ras/Raf/MEK/ERK signal
transduction cascade (51,52).
Several MEK inhibitors have been tested in clinical
trials. Selumetinib (AZD6244), is an oral small molecule that
inhibits MEK1/2 and has been tested clinically in a randomize phase
II trial in patients with B-RAF mutated melanoma (53). In a phase III study, only
trametinib (known as GSK1120212 or JTP-74057), a selective oral
inhibitor of MEK1 and 2, has been demonstrated to have impact on
clinical efficacy (54,55). Trametenib causes a block of the
protein MEK, and is correlated with improved PFS in patients
carrying B-RAFV600E/K mutations (56).
Previous studies showed that trametinib inhibits
cell growth by the inhibition of pERK 1/2, inducing cell cycle
arrest in cell lines with mutant B-RAF and RAS. This
shows its potent antitumor activity when administered daily for 14
days (57–59). In a phase III trial (METRIC),
trametinib was compared with dacarbazine in patients with
B-RAF mutations (60),
observing an improvement in median survival of 81 vs. 67% and PFS
of 4.8 vs. 1.5 months, with an objective response rate about 25%
(61). Administration of
trametinib, as monotherapy, results in a low activity in patients
previously treated with B-RAF inhibitors. Resistance to B-RAF
inhibitors may be also associated with resistance to MEK
inhibitors. In patients treated with trametinib the most common
toxic effects included skin rash, diarrhea, edema, hypertension and
fatigue (62). Trametinib compared
with chemotherapy showed a significant improvement in
progression-free and overall survival in patients with advanced
and/or metastatic melanoma (60).
PI3K/AKT/mTOR pathway is one of the most frequently
dysregulated pathway in human cancer. The most frequent causes of
changes in this pathway include mutation or increased gene copy
numbers of PIK3CA or other PI3K isoforms, loss of expression
of the pathway suppressors (for example, PTEN) or hyperactivation
of RTKs through receptor overexpression or activating mutations
(63–66). Hot spot mutations of the
PIK3CA gene include E542K, E545K and H1047R.
These mutations are oncogenic per se, as they can induce the
generation of tumors in several preclinical models without other
molecular aberrations (67–69).
The PI3K/AKT/mTOR and RAS/RAF/MEK/ERK pathways
interact at multiple points, resulting in cross-activation,
cross-inhibition, pathway convergence and these observations have
driven the development of small molecule inhibitors that target
various nodes of both pathways (70).
Recent studies have revealed that PI3K signalling is
deregulated in a high proportion of melanomas (11). Indeed, PTEN is deleted and
the downstream AKT gene is amplified in about 45% of
melanomas. These alterations cause an overexpression of AKT3, an
isoform of AKT (71). Increased
phospho-AKT expression in melanoma is associated with tumor
progression and shorter survival (72). The study of genomic alterations in
primary melanomas showed that tumors with B-RAF mutations
had few copies of PTEN, suggesting that dual activation of
the PI3K-AKT and MAPK pathways are important events in melanoma
development (73).
The research on PI3K inhibitors is expanding in
order to find more selective compounds, such as isoform-specific
PI3K inhibitors (74).
Advanced studies led to the development of
inhibitors of PI3K which selectively target only the catalytic
sites (75). The new PI3Ka
isoform-specific inhibitors gave an effective response in cell
lines that present PIK3CA mutations (76,77).
In addition, one of these compounds, BYL719, has revealed that
besides PIK3CA mutations, the presence of PI3KCA
amplification correlated with higher drug sensitivity, while
B-RAF and PTEN mutations were correlated with
resistance (74).
New therapeutic approaches involve the use of
immunotherapy for the treatment of cancer. Immunotherapy is based
on increasing the immune defenses to eliminate the cancer cells to
gain chemotherapeutic effect, and aiming to arrest the cell cycle
inducing apoptosis (81).
Immunotherapy may be used for tumors because they
express tumor associated antigens (82,83);
melanoma lesions often contain a high number of infiltrative
T-cells specific to melanocyte tumor-associated antigens such as
MART1, gp100 and tyrosinase (84).
An approach to eliminate the melanoma cells is to increase the
natural function of these cytotoxic T lymphocytes (CTL) (85).
Cytotoxic T lymphocyte-associated antigen 4 (CTLA-4)
is an immunoglobin-like molecule found primarily on CD4+
or CD8+ T lymphocytes and high levels of CTLA-4 are also
important in maintaining certain subsets of T-regulatory cells.
CTLA-4 is an ‘immune checkpoint’ that downregulates pathways of
T-cell activation and prevents autoimmunity, for this purpose it
has become an attractive target for immunotherapy (86).
The first immunotherapy to be approved by the Food
and Drug Administration (FDA) for treatment of advanced melanoma
was interleukin-2 (IL-2) but, like dacarbazine, response rates were
low even at high-doses of treatment (87). Its use in clinical practice is
limited by the severe toxic side-effects (88–90).
Ipilimumab is a recombinant, human monoclonal
antibody that binds to CTLA-4 and blocks the interaction of CTLA-4
with its ligands, CD80 and CD86. This immunotherapeutic augments
the antitumor T-cell response resulting in uncontrolled T-cell
proliferation and for this reason is associated with a substantial
risk of immune-related adverse reactions (91,92).
Ipilimumab acts by an indirect mechanism through T-cell mediated
antitumor immune responses. The most common severe immune-mediated
adverse reactions are enterocolitis, hepatitis, dermatitis,
neuropathy and endocrinopathy; these reactions can occur both
during the treatment, or weeks or months after discontinuation of
treatment (93,94).
Ipilimumab was approved, as monotherapy at 3 mg/kg,
in the European Union in 2011 for pretreated adult patients with
advanced (unresectable or metastatic) melanoma and in the United
States for both first- and second-line treatment for advanced
melanoma (95,96). In a clinical study, untreated
patients with advanced melanoma received a higher dose of
ipilimumab with or without dacarbazine or dacarbazine plus placebo.
Patients treated with dacarbazine and ipilimumab showed a
significant increase of the overall survival rate compared with
those treated with dacarbazine plus placebo (29). The treatment with ipilimumab in
advanced melanoma patients was also considered in concomitance with
the experimental vaccine glycoprotein 100 (gp100) (97). Patients with advanced melanoma
stage III or IV were included in this study. Pre-treated patients
were randomized for the administration of ipilimumab alone or in
combination with gp100 or gp100 alone. It was shown that the
combination with ipilimumab and gp100 did not improve survival when
compared with ipilimumab alone, suggesting that ipilimumab remains
the treatment with most efficacy for advanced melanoma (98).
Besides ipilimumab, also nivolumab, a monoclonal
antibody directed against the PD-1 receptor or its ligand (PD-L1)
has been reported (97). PD-1
receptor acts as an inhibitory receptor of T cells similar to
CTLA-4. In an initial phase I study of a monoclonal antibody
binding the PD-1 receptor, in patients previously treated, tumor
responses were recorded in 26 of 94 (28%) (99). Nivolumab has been administered as
monotherapy; most recent data suggest that nivolumab and ipilimumab
can be administered concomitantly with a manageable safety profile
(100). Immunotherapy is becoming
an important support to melanoma treatment (101).
Resistance to therapeutic agents, both chemical or
biological agents, remains the main problem in the management of
the therapy in melanoma. Combination of B-RAF inhibitors with MEK
inhibitors has been evaluated to improve the disease-free survival.
This combination reduces the skin toxicities and may also enhance
the antitumoral effects by synergistically suppressing ERK pathways
activity (102).
In patients who have developed resistance to
vemurafenib, the combination of dabrafenib and trametinib showed
76% of clinical response compared with that obtained with the
treatment of dabrafenib as single agent (54%) (41).
In a phase I/II trial, the combination of dabrafenib
and trametinib was effective in patients with
B-RAFV600E mutated metastatic melanoma and
numerous clinical trials are in progress to test other combinations
of B-RAF and MEK inhibitors (103,104). In a phase I study the
effectiveness of vemurafenib was tested in combination with an
inhibitor of MEK showing a tumor reduction in melanoma patients,
while in a phase III trial vemurafenib alone was compared with
vemurafenib in combination with MEK inhibitor (36). Several clinical studies are still
evaluating the combination of PI3K and MEK inhibitors in a variety
of cancers. This combined therapy may be able to overcome the
resistance mechanisms leading to apoptosis. These combinations
appear well tolerated and can be administered as therapeutic doses
(80).
The approval of ipilimumab represents a further
treatment option for melanoma patients. The National Comprehensive
Cancer Network (NCCN) now lists ipilimumab and vemurafenib among
the small number of preferred systemic regimens for treating
advanced and metastatic melanoma (105). The combination of vemurafenib
with immunotherapy could overcome the resistance mechanisms because
immunotherapy drugs have low response rates but relatively long
durations of response in a large subset of responding patients, by
contrast, B-RAF inhibitors have high initial response rates but
rarely produce long-term durable responses (95,106). Ipilimumab targets the tumors
indirectly by activation of the immune system therefore it is
likely to be efficacious in melanoma patients with and without the
B-RAFV600E mutation (100).
Some clinical trials have shown that MAPK pathway
inhibition with a selective inhibitor of
B-RAFV600E increase expression of
melanoma-derived antigens by the tumor and increased the
recognition of melanoma cells by antigen-specific T cells and,
selective inhibition did not have deleterious effects on T cell
proliferation or function (100,107).
B-RAF inhibitor treatment led to increased number of
tumor infiltrating lymphocytes in tumor biopsies obtained 10–14
days after treatment initiation. This increase was associated with
a reduction in tumor size and an increase in necrosis in
on-treatment biopsies (108,109).
These results suggested that at least a subset of
patients might be able to receive treatment with curative intent
with interleukin-2 or ipilimumab without compromising their ability
to benefit from B-RAF inhibitor treatment if they fail to achieve a
durable response (106).
Studies that combine B-RAF inhibitors with
immunotherapy are in progress and offer opportunities to further
improve outcomes for patients with advanced B-RAF V600E mutant
melanoma.
Finally, the effects of the new nitric oxide (NO)
donating compound (S,R)-3-phenyl-4,5-dihydro-5-isoxazole acetic
acid-nitric oxide (GIT-27NO) on the A375 human melanoma cell line
were investigated by our group. The capacity of GIT-27NO to induce
p53-mediated apoptosis in A375 melanoma cells suggests that
GIT-27NO may have a potential therapeutic use in the clinical
setting (110,111).
Cancer research is converging on understanding the
roles of signal transduction pathways in drug resistance and
sensitivity. Targeting various effectors of these pathways with
pharmacologic inhibitors may arrest melanoma cell proliferation.
This review pays attention on the clinical application of both
Raf/MEK/ERK and PI3K/AKT/mTOR pathway inhibitors as novel treatment
strategy for melanoma. Furthermore, we described how alterations of
molecular pathways, involved in melanoma development, interact with
each other resulting in response to therapy and/or chemoresistance.
The use of MAPK and AKT inhibitors for the treatment of melanoma
indicates that the response rate of these new molecular targeted
agents is higher compared to the standard chemotherapy. However,
additional studies are needed to better define the mechanisms of
resistance to these novel biological therapies.
|
1
|
Bataille V, Winnett A, Sasieni P, Newton
Bishop JA and Cuzick J: Exposure to the sun and sunbeds and the
risk of cutaneous melanoma in the UK: a case-control study. Eur J
Cancer. 40:429–435. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hodis E, Watson IR, Kryukov GV, Arold ST,
Imielinski M, Theurillat JP, Nickerson E, Auclair D, Li L, Place C,
Dicara D, Ramos AH, Lawrence MS, Cibulskis K, Sivachenko A, Voet D,
Saksena G, Stransky N, Onofrio RC, Winckler W, Ardlie K, Wagle N,
Wargo J, Chong K, Morton DL, Stemke-Hale K, Chen G, Noble M,
Meyerson M, Ladbury JE, Davies MA, Gershenwald JE, Wagner SN, Hoon
DS, Schadendorf D, Lander ES, Gabriel SB, Getz G, Garraway LA and
Chin L: A landscape of driver mutations in melanoma. Cell.
150:251–263. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Thomas NE, Berwick M and Cordeiro-Stone M:
Could BRAF mutations in melanocytic lesions arise from DNA damage
induced by ultraviolet radiation? J Invest Dermatol. 126:1693–1696.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Thomas NE, Edmiston SN, Alexander A,
Millikan RC, Groben PA, Hao H, Tolbert D, Berwick M, Busam K, Begg
CB, Mattingly D, Ollila DW, Tse CK, Hummer A, Lee-Taylor J and
Conway K: Number of nevi and early-life ambient UV exposure are
associated with BRAF-mutant melanoma. Cancer Epidemiol Biomarkers
Prev. 16:991–997. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Venesio T, Chiorino G, Balsamo A, Zaccagna
A, Petti C, Scatolini M, Pisacane A, Sarotto I, Picciotto F and
Risio M: In melanocytic lesions the fraction of
BRAFV600Ealleles is associated with sun exposure but
unrelated to ERK phosphorylation. Mod Pathol. 21:716–726.
2008.PubMed/NCBI
|
|
6
|
Candido S, Rapisarda V, Marconi A,
Malaponte G, Bevelacqua V, Gangemi P, Scalisi A, McCubrey JA,
Maestro R, Spandidos DA, Fenga C and Libra M: Analysis of the
B-RAFV600Emutation in cutaneous melanoma patients
with occupational sun exposure. Oncol Rep. 31:1079–1082. 2014.
|
|
7
|
Davies H, Bignell GR, Cox C, Stephens P,
Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W,
Davis N, Dicks E, Ewing R, Floyd Y, Gray K, Hall S, Hawes R, Hughes
J, Kosmidou V, Menzies A, Mould C, Parker A, Stevens C, Watt S,
Hooper S, Wilson R, Jayatilake H, Gusterson BA, Cooper C, Shipley
J, Hargrave D, Pritchard-Jones K, Maitland N, Chenevix-Trench G,
Riggins GJ, Bigner DD, Palmieri G, Cossu A, Flanagan A, Nicholson
A, Ho JW, Leung SY, Yuen ST, Weber BL, Seigler HF, Darrow TL,
Paterson H, Marais R, Marshall CJ, Wooster R, Stratton MR and
Futreal PA: Mutations of the BRAF gene in human cancer. Nature.
417:949–954. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Libra M, Malaponte G, Navolanic PM,
Gangemi P, Bevelacqua V, Proietti L, Bruni B, Stivala F, Mazzarino
MC, Travali S and McCubrey JA: Analysis of BRAF mutation in primary
and metastatic melanoma. Cell Cycle. 4:1382–1384. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Garnett MJ and Marais R: Guilty as
charged: B-RAF is a human oncogene. Cancer Cell. 6:313–319. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ascierto PA, Kirkwood JM, Grob J, Simeone
E, Grimaldi AM, Maio M, Palmieri G, Testori A, Marincola FM and
Mozzillo N: The role of BRAF V600 mutation in melanoma. J Transl
Med. 10:852012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen B, Tardell C, Higgins B, Packman K,
Boylan JF and Niu H: BRAFV600E negatively regulates the AKT pathway
in melanoma cell lines. PLoS One. 7:e425982012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vredeveld LC, Possik PA, Smit MA, Meissl
K, Michaloglou C, Horlings HM, Ajouaou A, Kortman PC, Dankort D,
McMahon M, Mooi WJ and Peeper DS: Abrogation of BRAFV600E-induced
senescence by PI3K pathway activation contributes to
melanomagenesis. Genes Dev. 26:1055–1069. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lipkin G: Plasticity of the cancer cell:
implications for epigenetic control of melanoma and other
malignancies. J Invest Dermatol. 128:2152–2155. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Villanueva J, Adina V, Lee JT,
Somasundaram R, Fukunaga-Kalabis M, Cipolla AK, Wubbenhorst B, Xu
X, Gimotty PA, Kee D, Santiago-Walker AE, Letrero R, D’Andrea K,
Pushparajan A, Hayden JE, Kimberly BD, Laquerre S, McArthur GA,
Sosman JA, Nathanson KL and Herlyn M: Acquired resistance to BRAF
inhibitors mediated by a RAF kinase switch in melanoma can be
overcome by co-targeting MEK and IGF-1R/PI3K. Cancer Cell.
18:683–695. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Viola JR, Rafael DF, Wagner E, Besch R and
Hindawi MO: Gene therapy for advanced melanoma: selective targeting
and therapeutic nucleic acids. J Drug Deliv. 2013:8973482013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wilhelm SM, Adnane L, Newell P, Villanueva
A, Llovet JM and Lynch M: Preclinical overview of sorafenib, a
multikinase inhibitor that targets both Raf and VEGF and PDGF
receptor tyrosine kinase signaling. Mol Cancer Ther. 7:3129–3140.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karasarides M, Chiloeches A, Hayward R,
Niculescu-Duvaz D, Scanlon I, Friedlos F, Ogilvie L, Hedley D,
Martin J, Marshall CJ, Springer CJ and Marais R: B-RAF is a
therapeutic target in melanoma. Oncogene. 23:6292–6298. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wilhelm SM, Carter C, Tang L, Wilkie D,
McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, Cao Y,
Shujath J, Gawlak S, Eveleigh D, Rowley BL, Adnane L, Lynch M,
Auclair D, Taylor I, Gedrich R, Voznesensky A, Riedl B, Post LE,
Bollag G and Trail PA: BAY 43-9006 exhibits broad spectrum oral
antitumor activity and targets the RAF/MEK/ERK pathway and receptor
tyrosine kinases involved in tumor progression and angiogenesis.
Cancer Res. 64:7099–7109. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Strumberg D, Awada A, Piccart P, Hirte H,
Moore M, Clark J, Lenz HJ, Lathia C, Schwartz B and Humphrey R:
Final report of the phase I clinical program of the novel raf
kinase inhibitor BAY 43-9006 in patients with refractory solid
tumors. J Clin Oncol. 22:2032003.
|
|
20
|
Strumberg D: Preclinical and clinical
development of the oral multikinase inhibitor sorafenib in cancer
treatment. Drugs Today. 41:773–784. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Awada A, Hendlisz A, Gil T, Bartholomeus
S, Mano M, de Valeriola D, Strumberg D, Brendel E, Haase CG,
Schwartz B and Piccart M: Phase I safety and pharmacokinetics of
BAY 43-9006 administered for 21 days on/7 days off in patients with
advanced, refractory solid tumours. Br J Cancer. 92:1855–1861.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Eisen T, Ahmad T, Flaherty KT, Gore M,
Kaye S, Marais R, Gibbens I, Hackett S, James M, Schuchter LM,
Nathanson KL, Xia C, Simantov R, Schwartz B, Poulin-Costello M,
O’Dwyer PJ and Ratain MJ: Sorafenib in advanced melanoma: a Phase
II randomised discontinuation trial analysis. Br J Cancer.
95:581–586. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chakraborty R, Wieland CN and Comfere N:
Molecular targeted therapies in metastatic melanoma. Pharmgenomics
Pers Med. 6:49–56. 2013.PubMed/NCBI
|
|
24
|
McCubrey JA, Steelman LS, Chappell WH,
Abrams SL, Montalto G, Cervello M, Nicoletti F, Fagone P, Malaponte
G, Mazzarino MC, Candido S, Libra M, Bäsecke J, Mijatovic S,
Maksimovic-Ivanic D, Milella M, Tafuri A, Cocco L, Evangelisti C,
Chiarini F and Martelli AM: Mutations and deregulation of
Ras/Raf/MEK/ERK and PI3K/PTEN/Akt/mTOR cascades which alter therapy
response. Oncotarget. 3:954–987. 2012.PubMed/NCBI
|
|
25
|
McCubrey JA, Steelman LS, Chappell WH,
Abrams SL, Franklin RA, Montalto G, Cervello M, Libra M, Candido S,
Malaponte G, Mazzarino MC, Fagone P, Nicoletti F, Bäsecke J,
Mijatovic S, Maksimovic-Ivanic D, Milella M, Tafuri A, Chiarini F,
Evangelisti C, Cocco L and Martelli AM: Ras/Raf/MEK/ERK and
PI3K/PTEN/Akt/mTOR cascade inhibitors: how mutations can result in
therapy resistance and how to overcome resistance. Oncotarget.
3:1068–1111. 2012.PubMed/NCBI
|
|
26
|
Pecuchet N, Lebbe C, Mir O, Billemont B,
Blanchet B, Franck N, Viguier M, Coriat R, Tod M, Avril MF and
Goldwasser F: Sorafenib in advanced melanoma: a critical role for
pharmacokinetics? Br J Cancer. 107:455–461. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Eisen T, Marais R, Affolter A, Lorigan P,
Robert C, Corrie P, Ottensmeier C, Chevreau C, Chao D, Nathan PD,
Jouary T, Harries M, Negrier S, Montegriffo E, Ahmad T, Gibbens I,
James MG, Strauss UP, Prendergast S and Gore ME: Sorafenib and
dacarbazine as first-line therapy for advanced melanoma: phase I
and open-label phase II studies. Br J Cancer. 105:353–359. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tsai J, Lee JT, Wang W, Zhang J, Cho H,
Mamo S, Bremer R, Gillette S, Kong J, Haass NK, Sproesser K, Li L,
Smalley KS, Fong D, Zhu YL, Marimuthu A, Nguyen H, Lam B, Liu J,
Cheung I, Rice J, Suzuki Y, Luu C, Settachatgul C, Shellooe R,
Cantwell J, Kim SH, Schlessinger J, Zhang KY, West BL, Powell B,
Habets G, Zhang C, Ibrahim PN, Hirth P, Artis DR, Herlyn M and
Bollag G: Discovery of a selective inhibitor of oncogenic B-Raf
kinase with potent antimelanoma activity. Proc Natl Acad Sci USA.
105:3041–3046. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jang S and Atkins MB: Which drug, and
when, for patients with BRAF-mutant melanoma? Lancet Oncol.
14:60–69. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chapman PB, Hauschild A, Robert C, Haanen
JB, Ascierto P, Larkin J, Dummer R, Garbe C, Testori A, Maio M,
Hogg D, Lorigan P, Lebbe C, Jouary T, Schadendorf D, Ribas A, O’Day
SJ, Sosman JA, Kirkwood JM, Eggermont AM, Dreno B, Nolop K, Li J,
Nelson B, Hou J, Lee RJ, Flaherty KT and McArthur GA: Improved
survival with vemurafenib in melanoma with BRAF V600E mutation. N
Engl J Med. 364:2507–2516. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Joseph EW, Pratilas CA, Poulikakos PI,
Tadi M, Wang W, Taylor BS, Halilovic E, Persaud Y, Xing F, Viale A,
Tsai J, Chapman PB, Bollag G, Solit DB and Rosen N: The RAF
inhibitor PLX4032 inhibits ERK signaling and tumor cell
proliferation in a V600E BRAF-selective manner. Proc Natl Acad Sci
USA. 107:14903–14908. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bollag G, Hirth P, Tsai J, Zhang J,
Ibrahim PN, Cho H, Spevak W, Zhang C, Zhang Y, Habets G, Burton EA,
Wong B, Tsang G, West BL, Powell B, Shellooe R, Marimuthu A, Nguyen
H, Zhang KY, Artis DR, Schlessinger J, Su F, Higgins B, Iyer R,
D’Andrea K, Koehler A, Stumm M, Lin PS, Lee RJ, Grippo J, Puzanov
I, Kim KB, Ribas A, McArthur GA, Sosman JA, Chapman PB, Flaherty
KT, Xu X, Nathanson KL and Nolop K: Clinical efficacy of a RAF
inhibitor needs broad target blockade in BRAF-mutant melanoma.
Nature. 467:596–599. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sosman JA, Kim KB, Schuchter L, Gonzalez
R, Pavlick AC, Weber JS, McArthur GA, Hutson TE, Moschos SJ,
Flaherty KT, Hersey P, Kefford R, Lawrence D, Puzanov I, Lewis KD,
Amaravadi RK, Chmielowski B, Lawrence HJ, Shyr Y, Ye F, Li J, Nolop
KB, Lee RJ, Joe AK and Ribas A: Survival in BRAF V600-mutant
advanced melanoma treated with vemurafenib. N Engl J Med.
366:707–714. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Oberholzer PA, Kee D, Dziunycz P, Sucker
A, Kamsukom N, Jones R, Roden C, Chalk CJ, Ardlie K, Palescandolo
E, Piris A, MacConaill LE, Robert C, Hofbauer GF, McArthur GA,
Schadendorf D and Garraway LA: RAS mutations are associated with
the development of cutaneous squamous cell tumors in patients
treated with RAF inhibitors. J Clin Oncol. 30:316–321. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Su F, Viros A, Milagre C, Trunzer K,
Bollag G, Spleiss O, Reis-Filho JS, Kong X, Koya RC, Flaherty KT,
Chapman PB, Kim MJ, Hayward R, Martin M, Yang H, Wang Q, Hilton H,
Hang JS, Noe J, Lambros M, Geyer F, Dhomen N, Niculescu-Duvaz I,
Zambon A, Niculescu-Duvaz D, Preece N, Robert L, Otte NJ, Mok S,
Kee D, Ma Y, Zhang C, Habets G, Burton EA, Wong B, Nguyen H, Kockx
M, Andries L, Lestini B, Nolop KB, Lee RJ, Joe AK, Troy JL,
Gonzalez R, Hutson TE, Puzanov I, Chmielowski B, Springer CJ,
McArthur GA, Sosman JA, Lo RS, Ribas A and Marais R: RAS mutations
in cutaneous squamous-cell carcinomas in patients treated with BRAF
inhibitors. N Engl J Med. 366:207–215. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Flaherty KT, Puzanov I, Kim KB, Ribas A,
McArthur GA, Sosman JA, O’Dwyer PJ, Lee RJ, Grippo JF, Nolop K and
Chapman PB: Inhibition of mutated, activated BRAF in metastatic
melanoma. N Engl J Med. 363:809–819. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Corcoran RB, Settleman J and Engelman JA:
Potential therapeutic strategies to overcome acquired resistance to
BRAF or MEK inhibitors in BRAF mutant cancers. Oncotarget.
2:336–346. 2011.PubMed/NCBI
|
|
38
|
McCubrey JA, Steelman LS, Kempf CR,
Chappell WH, Abrams SL, Stivala F, Malaponte G, Nicoletti F, Libra
M, Basecke J, Maksimovic-Ivanic D, Mijatovic S, Montalto G,
Cervello M, Cocco L and Martelli AM: Therapeutic resistance
resulting from mutations in Raf/MEK/ERK and PI3K/PTEN/Akt/mTOR
signaling pathways. J Cell Physiol. 226:2762–2781. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shao Y and Aplin AE: Akt3-mediated
resistance to apoptosis in B-RAF-targeted melanoma cells. Cancer
Res. 70:6670–6681. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Emery CM, Vijayendrana KG, Zipserc MC,
Sawyera AM, Niua L, Kima JJ, Hattona C, Choprad R, Oberholzera PA,
Karpovac MB, MacConailla LE, Zhangf J, Grayf NS, Sellersd WR,
Dummerc R and Garrawaya LA: MEK1 mutations confer resistance to MEK
and B-RAF inhibition. Proc Natl Acad Sci USA. 106:20411–20416.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Greger JG, Eastman SD, Zhang V, Bleam MR,
Hughes AM, Smitheman KN, Dickerson SH, Laquerre SG, Liu L and
Gilmer TM: Combinations of BRAF, MEK, and PI3K/mTOR inhibitors
overcome acquired resistance to the BRAF inhibitor GSK2118436
dabrafenib, mediated by NRAS or MEK mutations. Mol Cancer Ther.
11:909–920. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Aplin AE, Kaplan FM and Shao Y: Mechanisms
of resistance to RAF inhibitors in melanoma. J Invest Dermatol.
131:1817–1820. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Trunzer K, Pavlick AC, Schuchter L,
Gonzalez R, McArthur GA, Hutson TE, Moschos SJ, Flaherty KT, Kim
KB, Weber JS, Hersey P, Long GV, Lawrence D, Ott PA, Amaravadi RK,
Lewis KD, Puzanov I, Lo Roger S, Koehler A, Kockx M, Spleiss O,
Schell-Steven A, Gilbert HN, Cockey L, Bollag G, Lee RJ, Joe AK,
Sosman JA and Ribas A: Pharmacodynamic effects and mechanisms of
resistance to vemurafenib in patients with metastatic melanoma. J
Clin Oncol. 31:1767–1774. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hauschild A, Grob J, Demidov LV, Jouary T,
Gutzmer R, Millward M, Rutkowski P, Blank CU, Miller WH Jr,
Kaempgen E, Martín-Algarra S, Karaszewska B, Mauch C,
Chiarion-Sileni V, Martin A, Swann S, Haney P, Mirakhur B, Guckert
ME, Goodman V and Chapman PB: Dabrafenib in BRAF-mutated metastatic
melanoma: a multicentre, open-label, phase 3 randomised controlled
trial. Lancet. 380:358–365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Long GV, Trefzer U, Davies MA, Kefford RF,
Ascierto PA, Chapman PB, Puzanov I, Hauschild A, Robert C, Algazi
A, Mortier L, Tawbi H, Wilhelm T, Zimmer L, Switzky J, Swann S,
Martin A, Guckert M, Goodman V, Streit M, Kirkwood JM and
Schadendorf D: Dabrafenib in patients with Val600Glu or Val600Lys
BRAF-mutant melanoma metastatic to the brain (BREAK-MB): a
multicentre, open-label, phase 2 trial. Lancet Oncol. 13:1087–1095.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ascierto PA, Minor D, Ribas A, Lebbe C,
O’Hagan A, Arya N, Guckert M, Schadendorf D, Kefford RF, Grob J,
Hamid O, Amaravadi R, Simeone E, Wilhelm T, Kim KB, Long GV, Martin
A, Mazumdar J, Goodman VL and Trefzer U: Phase II trial (BREAK-2)
of the BRAF inhibitor dabrafenib (GSK2118436) in patients with
metastatic melanoma. J Clin Oncol. 31:3205–3211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Falchook GS, Long GV, Kurzrock R, Kim KB,
Arkenau TH, Brown MP, Hamid O, Infante JR, Millward M, Pavlick AC,
O’Day SJ, Blackman SC, Curtis CM, Lebowitz P, Ma B, Ouellet D and
Kefford RF: Dabrafenib in patients with melanoma, untreated brain
metastases, and other solid tumours: a phase 1 dose-escalation
trial. Lancet. 379:1893–1901. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Trefzer U, Minor D, Ribas A, Lebbe C,
Siegfried A, Arya N, Guckert M, Schadendorf D, Kefford R, Grob JJ,
Hamid O, Amaravadi R, Simeone E, Wilhelm T, Kim K, Goodman V and
Ascierto PA: BREAK-2: a Phase IIA trial of the selective BRAF
kinase inhibitor GSK2118436 in patients with BRAF mutation-positive
(V600E/K) metastatic melanoma. Pigm Cell Melanoma R.
24:10202011.
|
|
49
|
Gray-Schopfer V, Wellbrock C and Marais R:
Melanoma biology and new targeted therapy. Nature. 445:851–857.
2007. View Article : Google Scholar
|
|
50
|
Johnson DB and Sosman JA: Update on the
targeted therapy of melanoma. Curr Treat Options Oncol. 14:280–292.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Chang L and Karin M: Mammalian MAP kinase
signalling cascades. Nature. 410:37–40. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Thompson N and Lyons J: Recent progress in
targeting the Raf/MEK/ERK pathway with inhibitors in cancer drug
discovery. Curr Opin Pharmacol. 5:350–356. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Catalanotti F, Solit DB, Pulitzer MP,
Berger MF, Scott SN, Iyriboz T, Lacouture ME, Panageas KS, Wolchok
JD, Carvajal RD, Schwartz GK, Rosen N and Chapman PB: Phase II
trial of MEK inhibitor selumetinib (AZD6244, ARRY-142886) in
patients with BRAFV600E/K-mutated melanoma. Clin Cancer Res.
19:2257–2264. 2013. View Article : Google Scholar
|
|
54
|
Flaherty KT, Robert C, Hersey P, Nathan P,
Garbe C, Milhem M, Demidov LV, Hassel JC, Rutkowski P, Mohr P,
Dummer R, Trefzer U, Larkin JM, Utikal J, Dreno B, Nyakas M,
Middleton MR, Becker JC, Casey M, Sherman LJ, Wu FS, Ouellet D,
Martin AM, Patel K and Schadendorf D: Improved survival with MEK
inhibition in BRAF-mutated melanoma. N Engl J Med. 367:107–114.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Byron SA, Loch DC, Wellens CL, Wortmann A,
Wu J, Wang J, Nomoto K and Pollock PM: Sensitivity to the MEK
inhibitor E6201 in melanoma cells is associated with mutant BRAF
and wildtype PTEN status. Mol Cancer. 11:752012. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Falchook GS, Lewis KD, Infante JR, Gordon
MS, Vogelzang NJ, De Marini DJ, Sun P, Moy C, Szabo SA, Roadcap LT,
Peddareddigari VG, Lebowitz PF, Le NT, Burris HA III, Messersmith
WA, O’Dwyer PJ, Kim KB, Flaherty K, Bendell JC, Gonzalez R,
Kurzrock R and Fecher LA: Activity of the oral MEK inhibitor
trametinib in patients with advanced melanoma: a phase 1
dose-escalation trial. Lancet Oncol. 13:782–789. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Yamaguchi T, Kakefuda R, Tajima N, Sowa Y
and Sakai T: Antitumor activities of JTP-74057 (GSK1120212), a
novel MEK1/2 inhibitor, on colorectal cancer cell lines in
vitro and in vivo. Int J Oncol. 39:23–31.
2011.PubMed/NCBI
|
|
58
|
Gilmartin AG, Bleam MR, Groy A, Moss KG,
Minthorn EA, Kulkarni SG, Rominger CM, Erskine S, Fisher KE, Yang
J, Zappacosta F, Annan R, Sutton D and Laquerre SG: GSK1120212
(JTP-74057) is an inhibitor of MEK activity and activation with
favorable pharmacokinetic properties for sustained in vivo pathway
inhibition. Clin Cancer Res. 17:989–1000. 2011. View Article : Google Scholar
|
|
59
|
Akinleye A, Furqan M, Mukhi N, Ravella P
and Liu D: MEK and the inhibitors: from bench to bedside. J Hematol
Oncol. 6:272013. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Robert C, Flaherty KT, Hersey P, Nathan P,
Garbe C, Milhem MM, Demidov LV, Hassel JC, Rutkowski P, Mohr P,
Dummer R, Trefzer U, Larkin JMG, Utikal J, Casey M, Sherman LJ,
Crist WA, Wu FS, Patel K and Schadendorf D: METRIC phase III study:
efficacy of trametinib (T), a potent and selective MEK inhibitor
(MEKi), in progression-free survival (PFS) and overall survival
(OS), compared with chemotherapy (C) in patients (pts) with BRAF
V600E/K mutant advanced or metastatic melanoma (MM). J Clin Oncol.
30(Suppl): abs. LBA8509. 2012.
|
|
61
|
Klinac D, Gray ES, Millward M and Ziman M:
Advances in personalized targeted treatment of metastatic melanoma
and non-invasive tumor monitoring. Front Oncol. 3:542013.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kim KB, Lewis K, Pavlick A, Infante JR,
Ribas A, Sosman JA, Fecher LA, Millward M, McArthur GA, Hwu P,
Gonzalez R, Ott PA, Long G, Gardner OS, Ouellet D, Xu Y, De Marini
DJ, Le N, Patel K and Kefford R: A phase II study of the MEK1/MEK2
inhibitor GSK1120212 in metastatic BRAF-V600E or K mutant cutaneous
melanoma patients previously treated with or without a BRAF
inhibitor. International Melanoma Congress. Pigment Cell Res.
24:990–1075. 2011.
|
|
63
|
Ikenoue T, Kanai F, Hikiba Y, Obata T,
Tanaka Y, Imamura J, Ohta M, Jazag A, Guleng B, Tateishi K, Asaoka
Y, Matsumura M, Kawabe T and Omata M: Functional analysis of PIK3CA
gene mutations in human colorectal cancer. Cancer Res.
65:4562–4567. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Isakoff SJ, Engelman JA, Irie HY, Luo J,
Brachmann SM, Pearline RV, Cantley LC and Brugge JS: Breast
cancer-associated PIK3CA mutations are oncogenic in mammary
epithelial cells. Cancer Res. 65:10992–11000. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zhao JJ, Liu Z, Wang L, Shin E, Loda MF
and Roberts TM: The oncogenic properties of mutant p110alpha and
p110beta phosphatidylinositol 3-kinases in human mammary epithelial
cells. Proc Natl Acad Sci USA. 102:18443–18448. 2005. View Article : Google Scholar
|
|
66
|
Janku F, Wheler JJ, Naing A, Stepanek VM,
Falchook GS, Fu S, Garrido-Laguna I, Tsimberidou AM, Piha-Paul SA,
Moulder SL, Lee JJ, Luthra R, David SH and Kurzrock R: PIK3CA
mutations in advanced cancers: characteristics and outcomes.
Oncotarget. 3:1566–1575. 2012.PubMed/NCBI
|
|
67
|
Zhao L and Vogt PK: Class I PI3K in
oncogenic cellular transformation. Oncogene. 27:5486–5496. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Ligresti G, Militello L, Steelman LS,
Cavallaro A, Basile F, Nicoletti F, Stivala F, McCubrey JA and
Libra M: PIK3CA mutations in human solid tumors. Role in
sensitivity to various therapeutic approaches. Cell Cycle.
8:1352–1358. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Hafsi S, Pezzino FM, Candido S, Ligresti
G, Spandidos DA, Soua Z, McCubrey JA, Travali S and Libra M: Gene
alterations in the PI3K/PTEN/AKT pathway as a mechanism of
drug-resistance. Int J Oncol. 40:639–644. 2011.PubMed/NCBI
|
|
70
|
Mendoza MC, Er EE and Blenis J: The
Ras-ERK and PI3KmTOR pathways: cross-talk and compensation. Trends
Biochem Sci. 36:320–328. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Stahl JM, Sharma A, Cheung M, Zimmerman M,
Cheng JQ, Bosenberg MW, Kester M, Sandirasegarane L and Robertson
GP: Deregulated Akt3 activity promotes development of malignant
melanoma. Cancer Res. 64:7002–7010. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Meier F, Schittek B, Busch S, Garbe C,
Smalley K, Satyamoorthy K, Li G and Herlyn M: The RAS/RAF/MEK/ERK
and PI3K/AKT signaling pathways present molecular targets for the
effective treatment of advanced melanoma. Front Biosci.
10:2986–3001. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
73
|
Russo AE, Torrisi E, Bevelacqua Y,
Perrotta R, Libra M, McCubrey JA, Spandidos DA, Stivala F and
Malaponte G: Melanoma: molecular pathogenesis and emerging target
therapies (Review). Int J Oncol. 34:1481–1489. 2009.PubMed/NCBI
|
|
74
|
Brana I and Siu LL: Clinical development
of phosphatidylinositol 3-kinase inhibitors for cancer treatment.
BMC Med. 10:1612012. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ogita S and Lorusso P: Targeting
phosphatidylinositol 3 kinase (PI3K)-Akt beyond rapalogs. Target
Oncol. 6:103–117. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Huang A, Fritsch C, Wilson C, Reddy A, Liu
M, Lehar J, Quadt C, Hofmann F and Schlegel R: Single agent
activity of PIK3CA inhibitor BYL719 in a broad cancer cell line
panel. Proceedings of the 103rd Annual Meeting of the American
Association for Cancer Research; Chicago, IL, Philadelphia, PA. Am
Assoc Cancer Res. abs. 3749. 2012
|
|
77
|
Jessen K, Kessler L, Kucharski J, Guo X,
Staunton J, Janes M, Elia M, Banerjee U, Lan L, Wang S, Stewart J,
Luzader A, Darjania L, Li L, Chan K, Martin M, Ren P, Rommel C and
Liu Y: A potent and selective PI3K inhibitor, INK1117, targets
human cancers harboring oncogenic PIK3CA mutations. In:
AACR-NCI-EORTC International Conference: Molecular Targets and
Cancer Therapeutics; San Francisco, CA, Philadelphia, PA. Am Assoc
Cancer Res. 10. abs. A171. 2011
|
|
78
|
Britten CD: PI3K and MEK inhibitor
combinations: examining the evidence in selected tumor types.
Cancer Chemother Pharmacol. 71:1395–1409. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Liu P, Cheng H, Roberts TM and Zhao JJ:
Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev
Drug Discov. 8:627–644. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Markman B, Dienstmann R and Tabernero J:
Targeting the PI3K/Akt/mTOR pathway - beyond rapalogs. Oncotarget.
1:530–543. 2010.PubMed/NCBI
|
|
81
|
Mansh M: Ipilimumab and cancer
immunotherapy: a new hope for advanced stage melanoma. Yale J Biol
Med. 84:381–389. 2011.PubMed/NCBI
|
|
82
|
Sondak VK, Smalley KS, Kudchadkar R,
Grippon S and Kirkpatrick P: Ipilimumab. Nat Rev Drug Discov.
10:411–412. 2011. View Article : Google Scholar
|
|
83
|
Fellner C: Ipilimumab (Yervoy) prolongs
survival in advanced melanoma. Drug Forecast. 37:503–530.
2012.PubMed/NCBI
|
|
84
|
Tjin EP, Konijnenberg D, Krebbers G, Mallo
H, Drijfhout JW, Franken KL, van der Horst CM, Bos JD, Nieweg OE,
Kroon BB, Haanen JB, Melief CJ, Vyth-Dreese FA and Luiten RM: T
cell immune function in tumor, skin, and peripheral blood of
advance stage melanoma patients: implications for immunotherapy.
Clin Cancer Res. 17:5736–5747. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Levings MK, Sangregorio R and Roncarolo
MG: Human cd25(+)cd4(+) t regulatory cells suppress naive and
memory T cell proliferation and can be expanded in vitro without
loss of function. J Exp Med. 193:1295–1302. 2001.
|
|
86
|
Melero I, Hervas-Stubbs S, Glennie M,
Pardoll DM and Chen L: Immunostimulatory monoclonal antibodies for
cancer therapy. Nat Rev Cancer. 7:95–106. 2007. View Article : Google Scholar
|
|
87
|
Agarwala SS: Current systemic therapy for
metastatic melanoma. Expert Rev Anticancer Ther. 9:587–595. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Kirkwood JM, Tarhini AA, Panelli MC,
Moschos SJ, Zarour HM, Butterfield LH and Gogas HJ: Next generation
of immunotherapy for melanoma. J Clin Oncol. 26:3445–3455. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Antony GK and Dudek AZ: Interleukin 2 in
cancer therapy. Curr Med Chem. 17:3297–3302. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Chmielowski B: Ipilimumab: a
first-in-class T-cell potentiator for metastatic melanoma. J Skin
Cancer. 2013:4238292013. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Hodi FS, O’Day SJ, McDermott DF, Weber RW,
Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel
JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM,
Linette GP, Hogg D, Ottensmeier CH, Lebbé C, Peschel C, Quirt I,
Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos
A and Urba WJ: Improved survival with ipilimumab in patients with
metastatic melanoma. N Engl J Med. 363:211–223. 2010.PubMed/NCBI
|
|
92
|
Robert C and Ghiringhelli F: What is the
role of cytotoxic T lymphocyte-associated antigen 4 blockade in
patients with metastatic melanoma? Oncologist. 14:848–861.
2009.PubMed/NCBI
|
|
93
|
Hwu P: Treating cancer by targeting the
immune system. N Engl J Med. 363:779–781. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Wolchok JD, Neyns B, Linette G, Negrier S,
Lutzky J, Thomas L, Waterfield W, Schadendorf D, Smylie M, Guthrie
T Jr, Grob JJ, Chesney J, Chin K, Chen K, Hoos A, O’Day SJ and
Lebbé C: Ipilimumab monotherapy in patients with pretreated
advanced melanoma: a randomised, double-blind, multicentre, phase
2, dose-ranging study. Lancet Oncol. 11:155–164. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lipson EJ and Drake CG: Ipilimumab: an
anti-CTLA-4 antibody for metastatic melanoma. Clin Cancer Res.
17:6958–6962. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Di Giacomo AM, Calabrò L, Danielli R,
Fonsatti E, Bertocci E, Pesce I, Fazio C, Cutaia O, Giannarelli D,
Miracco C, Biagioli M, Altomonte M and Maio M: Long-term survival
and immunological parameters in metastatic melanoma patients who
responded to ipilimumab 10 mg/kg within an expanded access
programme. Cancer Immunol Immunother. 62:1021–1028. 2013.PubMed/NCBI
|
|
97
|
Feng Y, Roy A, Masson E, Chen T, Humphrey
R and Weber JS: Exposure-response relationships of the efficacy and
safety of ipilimumab in patients with advanced melanoma. Clin
Cancer Res. 19:3977–3986. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Melero I, Grimaldi AM, Perez-Gracia JL and
Ascierto PA: Clinical development of immunostimulatory monoclonal
antibodies and opportunities for combination. Clin Cancer Res.
19:997–1008. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Topalian SL, Hodi FS, Brahmer JR,
Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD,
Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L,
Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM,
McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D,
Kollia GD, Gupta A, Wigginton JM and Sznol M: Safety, activity, and
immune correlates of anti-PD-1 antibody in cancer. N Engl J Med.
366:2443–2454. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Shahabi V, Whitney G, Hamid O, Schmidt H,
Chasalow SD, Alaparthy S and Jackson JR: Assessment of association
between BRAF-V600E mutation status in melanomas and clinical
response to ipilimumab. Cancer Immunol Immunother. 61:733–737.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Davar D, Tarhini AA and Kirkwood JM:
Adjuvant immunotherapy of melanoma and development of new
approaches using the neoadjuvant approach. Clin Dermatol.
31:237–250. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Lo RS: Combinatorial therapies to overcome
B-RAF inhibitor resistance in melanomas. Pharmacogenomics.
13:125–128. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Infante JR, Falchook GS, Lawrence DP,
Weber JS, Kefford RF, Bendell JC, Kurzrock R, Shapiro G, Kudchadkar
RR, Long GV, Burris HA, Kim KB, Clements A, Peng S, Yi B, Allred
AJ, Ouellet D, Patel K, Lebowitz PF and Flaherty KT: Phase I/II
study to assess safety, pharmacokinetics, and efficacy of the oral
MEK 1/2 inhibitor GSK1120212 (GSK212) dosed in combination with the
oral BRAF inhibitor GSK2118436 (GSK436). J Clin Oncol. 29(Suppl):
abs. CRA8503. 2011.
|
|
104
|
Weber JS, Flaherty KT, Infante JR,
Falchook GS, Kefford R, Daud A, Hamid O, Gonzalez R, Kudchadkar RR,
Lawrence DP, Burris HA, Long GV, Algazi AP, Lewis KD, Kim KB,
Puzanov I, Sun P, Little SM, Patel K and Sosman JA: Updated safety
and efficacy results from a phase I/II study of the oral BRAF
inhibitor dabrafenib (GSK2118436) combined with the oral MEK 1/2
inhibitor trametinib (GSK1120212) in patients with BRAFi-naïve
metastatic melanoma. J Clin Oncol. 30(Suppl): abs. 8510. 2012.
|
|
105
|
Curti BD and Urba WJ: Integrating new
therapies in the treatment of advanced melanoma. PhD Current
Treatment Options in Oncology. Skin Cancer. 13:327–339.
2012.PubMed/NCBI
|
|
106
|
Ascierto PA, Simeone E, Giannarelli D,
Grimaldi AM, Romano A and Mozzillo N: Sequencing of BRAF inhibitors
and ipilimumab in patients with metastatic melanoma: a possible
algorithm for clinical use. J Transl Med. 10:1072012. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Comin-Anduix B, Chodon T, Sazegar H,
Matsunaga D, Mock S, Jalil J, Escuin-Ordinas H, Chmielowski B, Koya
RC and Ribas A: The oncogenic BRAF kinase inhibitor PLX4032/RG7204
does not affect the viability or function of human lymphocytes
across a wide range of concentrations. Clin Cancer Res.
16:6040–6048. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Wargo JA, Cogdill A, Dang P, Gupta R,
Piris A, Boni A, Garber HR, Ott H, Newton LP, Flaherty KT, Lawrence
DP, Tsao H and Fisher DE: Treatment with a selective inhibitor of
BRAFV600E increases melanocyte antigen expression and CD8 T cell
infiltrate in tumors of patients with metastatic melanoma. Cancer
Res. 71:abs. 95. 2011. View Article : Google Scholar
|
|
109
|
Wilmott JS, Long GV, Howle JR, Haydu LE,
Sharma RN, Thompson JF, Kefford RF, Hersey P and Scolyer RA:
Selective BRAF inhibitors induce marked T-cell infiltration into
human metastatic melanoma. Clin Cancer Res. 18:1386–1394. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Mijatovic S, Maksimovic-Ivanica D, Mojic
M, Malaponte G, Libra M, Cardile V, Miljkovic D, Harhaji L,
Dabideen D, Cheng KF, Bevelacqua Y, Donia M, Garotta G, Al-Abed Y,
Stosic-Grujicic S and Nicoletti F: Novel nitric oxide-donating
compound (S,R)-3-phenyl-4,5-dihydro-5-isoxazole acetic acid-nitric
oxide (GIT-27NO) induces p53 mediated apoptosis in human A375
melanoma cells. Nitric Oxide. 19:177–183. 2008. View Article : Google Scholar
|
|
111
|
Donia M, Mangano K, Fagone P, De Pasquale
R, Dinotta F, Coco M, Padron J, Al-Abed Y, Lombardo GA,
Maksimovic-Ivanic D, Mijatovic S, Zocca M, Perciavalle V,
Stosic-Grujicic S and Nicoletti F: Unique antineoplastic profile of
Saquinavir-NO, a novel NO-derivative of the protease inhibitor
Saquinavir, on the in vitro and in vivo tumor
formation of A375 human melanoma cells. Oncol Rep. 28:682–688.
2012.PubMed/NCBI
|