Introduction
Lung cancer is the leading cause of cancer-related
death in the developed world (1).
Non-small cell lung cancer (NSCLC) accounts for approximately 80%
of lung cancers, and the prognosis of patients with advanced NSCLC
remains very poor despite advances in treatment (2).
One promising treatment strategy involves the
further subdivision of NSCLC into clinically relevant molecular
subsets according to a classification schema based on specific
so-called oncogenic driver mutations. These mutations occur in
genes that encode signal proteins crucial for cellular
proliferation and survival. Thus, cancer might rely on the
expression of these single oncogenes for survival. This concept is
also called oncogene addiction (3). The identification of epidermal growth
factor receptor (EGFR) mutations as a type of oncogenic
driver mutation in a subset of patients with NSCLC, coupled with
the development of EGFR tyrosine kinase inhibitors
(EGFR-TKIs), has opened new ways to treat this disease (4–7).
Recently, a novel fusion transcript with transforming activity that
is formed by the translocation of echinoderm microtubule-associated
protein-like 4 (EML4) (2p21) and anaplastic lymphoma kinase
(ALK) (2p23) has been described in a subset of NSCLCs
(8). Although patients with
ALK rearrangements respond dramatically to ALK inhibitors,
as is seen in EGFR-TKIs for EGFR-mutated NSCLC, some of them
are resistant to these inhibitors (9–11).
Therefore, additional molecular mechanisms need to be identified to
further improve the response.
Hypoxic cancer cells can be aggressive and exhibit
metastatic phenotypes with lower sensitivity to apoptotic signals.
In addition, hypoxia is involved in the resistance to
chemotherapeutic treatments in several types of tumors, including
EGFR-mutated NSCLC and EGFR-TKIs (12–14).
However, the involvement of hypoxia in the resistance to ALK
inhibitors in NSCLC with an ALK rearrangement remains
unclear. In the present study, we investigated the influence of
hypoxia on the sensitivity to ALK inhibitors in the H3122 NSCLC
cell line with an ALK rearrangement.
Materials and methods
Cell culture and reagent
The H3122 cell line (NSCLC cell line with an
EML4-ALK rearrangement) was maintained in RPMI-1640 medium
with 10% FBS (Sigma-Aldrich, St. Louis, MO, USA). For the normoxic
state, the cell line was maintained in a 5%
CO2-humidified atmosphere at 37°C; for the hypoxic
state, the cell line was maintained in 5% CO2-humidified
0.2% O2 at 37°C. Crizotinib and alectinib (ALK
inhibitors) were purchased from Selleck Chemicals (Houston, TX,
USA).
Growth inhibition assay in vitro
The growth-inhibitory effects of crizotinib and
alectinib were examined using a 3, 4, 5-dimethyl- 2H-tetrazolium
bromide assay (MTT; Sigma-Aldrich), as described previously
(15). The experiment was
performed in triplicate.
Migration assay
The migration assays were performed using Boyden
chamber methods and polycarbonate membranes with an 8-μm pore size
(Chemotaxicell; Kurabo, Osaka, Japan), as previously described
(16). The membranes were coated
with fibronectin on the outer side and were dried for 2 h at room
temperature. The cells (2×104 cells/well) were then
seeded onto the upper chambers with 200 ml of migrating medium
(RPMI containing 0.5% FBS), and the upper chambers were placed into
the lower chambers of 24-well culture dishes containing 600 ml of
RPMI with 10% FBS. After incubation for 48 h under a normoxic or
hypoxic state, the media in the upper chambers were aspirated and
the non-migrated cells on the inner sides of the membranes were
removed using a cotton swab. The cells that had migrated to the
outer side of the membranes were fixed with 4% paraformaldehyde for
10 min, stained with 0.1% crystal violet stain solution for 15 min,
and then counted using a light microscope. The number of migrated
cells was averaged from 5 fields per 1 chamber, and 3 chambers were
used for each experiment. The experiment was performed in
triplicate.
Real-time reverse transcription PCR
(RT-PCR)
One microgram of total RNA from cultured cell lines
was converted to cDNA using the GeneAmp RNA-PCR kit (Applied
Biosystems, Foster City, CA, USA). Real-time PCR was performed
using SYBR Premix Ex Taq and Thermal Cycler Dice (Takara, Shiga,
Japan), as described previously (16). The glyceraldehyde 3-phosphate
dehydrogenase (GAPD, NM_002046) gene was used to normalize the
expression levels in subsequent quantitative analyses. The
experiment was performed in triplicate. To amplify the target genes
encoding E-cadherin, vimentin, fibronectin, and slug
(E-cadherin, VIM, FN1 and SLUG gene), the following
primers were used: E-cadherin-F, TTAAACT CCTGGCCTCAAGCAATC;
E-cadherin-R, TCCTATCTT GGGCAAAGCAACTG; VIM-F,
TGAGTACCGGAGACA GGTGCAG; VIM-R, TAGCAGCTTCAACGGCAAAGTTC;
FN1-F, GGAGCAAATGGCACCGAGATA; FN1-R, GAGCT
GCACATGTCTTGGGAAC; SLUG-F, ATGCATATTCG GACCCACACATTA;
SLUG-R, AGATTTGACCTGTCTGC AAATGCTC; GAPD-F,
GCACCGTCAAGGCTGAGAAC; GAPD-R, ATGGTGGTGAAGACGCCAGT.
Antibody
Antibodies specific for AKT, phospho-AKT, ERK1/2,
phospho-ERK1/2, PARP, cleaved PARP, caspase-3, cleaved caspase-3,
E-cadherin, vimentin, slug, and β-actin were obtained from Cell
Signaling (Beverly, MA, USA). An antibody specific for fibronectin
was obtained from Abcam (Cambridge, UK). An antibody specific for
hypoxia-inducible factor 1α (HIF1α) was obtained from Novus
(Littleton, CO, USA).
Western blot analysis
A western blot analysis was performed as described
previously (15). Briefly,
subconfluent cells were washed with cold phosphate-buffered saline
(PBS) and harvested with Lysis A buffer containing 1% Triton X-100,
20 mM Tris-HCl (pH 7.0), 5 mM EDTA, 50 mM sodium chloride, 10 mM
sodium pyrophosphate, 50 mM sodium fluoride, 1 mM sodium
orthovanadate, and the protease inhibitor mix Complete™ (Roche
Diagnostics, Basel, Switzerland). Wholecell lyses were separated
using SDS-PAGE and were blotted onto a polyvinylidene fluoride
membrane. After blocking with 3% bovine serum albumin in a TBS
buffer (pH 8.0) with 0.1% Tween-20, the membrane was probed with
the primary antibody. After rinsing twice with TBS buffer, the
membrane was incubated with a horseradish peroxidase-conjugated
secondary antibody and washed, followed by visualization using an
ECL detection system and LAS-4000 (GE Healthcare, Buckinghamshire,
UK). When the phosphorylation was evaluated in cells treated with
an inhibitor, the cells were incubated under a normoxic or hypoxic
state for 48 h and the inhibitor was added three hours before the
sample collection.
Short interfering RNA (siRNA)
transfection
Cells were transfected with siRNA for HIF1A
or a non-specific target (scramble) as follows:
GGAAUUAACUCAGUUUGAACUAACU (si-HIF1A) and AAACCUUCAGACGUUAGUUUAUAGA
for a scramble of HIF1A (si-Scr). siRNA transfection was performed
using RNAiMAX (Invitrogen, Carlsbad, CA, USA) according to the
manufacturer’s instructions, as previously described (17), and was allowed to proceed for 48–96
h before the growth-inhibitory test or the collection of the
whole-cell extract. Knockdown was confirmed using western blot
analyses.
Statistical analysis
Continuous variables were analyzed using the
Student’s t-test, and the results were expressed as the average and
standard deviations (SD). The statistical analyses were two-tailed
and were performed using Microsoft Excel (Microsoft, Redmond, WA,
USA). P-values of <0.05 were considered statistically
significant.
Results
Sensitivity to ALK inhibitors under a
normoxic or hypoxic state
To examine the sensitivity of the H3122 cell line to
ALK inhibitors, we performed an MTT assay (Fig. 1A). Under a normoxic state, the 50%
inhibitory concentration (IC50) of crizotinib and
alectinib was 0.096 and 0.033 μM, respectively (Fig. 1B). Under a hypoxic state, however,
the IC50 was 0.75 and 1.30 μM, respectively. These
results indicate that hypoxia induces resistance to ALK inhibitors
in the H3122 cell line.
Effect of hypoxia on AKT and ERK signals
and apoptosis in the H3122 cell line
Next, to examine the effect of hypoxia on the
downstream signal of ALK, we evaluated the phosphorylation of AKT
and ERK under normoxic and hypoxic states. The cells were incubated
under normoxia or hypoxia for 48 h, and the inhibitor was then
added at the indicated concentrations three hours before the sample
collection. The phosphorylation of AKT and ERK was dose-dependently
reduced by crizotinib under a normoxic state. Under hypoxia,
however, crizotinib reduced the phosphorylation to a lesser extent
(Fig. 2A).
Furthermore, to evaluate apoptosis, western blot
analyses for apoptosis-related molecules were performed. The
samples were analyzed 48 h after DMSO (control) or crizotinib (0.1
μM) stimulation under normoxia or hypoxia. Under a normoxic state,
the expressions of both cleaved PARP and cleaved caspase-3 were
elevated by crizotinib, whereas the expressions were not elevated
under hypoxia. These results suggest that the downstream signals
are inactivated by crizotinib to a lesser degree and that
crizotinib-induced apoptosis is inhibited under a hypoxic
state.
EMT of the H3122 cell line is mediated by
hypoxia
To investigate the mechanism of the resistance
induced by hypoxia, the morphologic changes of cells subjected to
hypoxia were observed. The morphology of the cells changed to a
scattered pattern of spindle-shaped cells in a time-dependent
manner (Fig. 3A). Then, to
evaluate the migration ability, a migration assay was performed
using the Boyden chamber method. Under hypoxia, the number of
migrating cells increased significantly, compared with the
situation under normoxia (8.67±3.5 vs. 1.33±1.53/Field,
*P=0.026) (Fig.
3B).
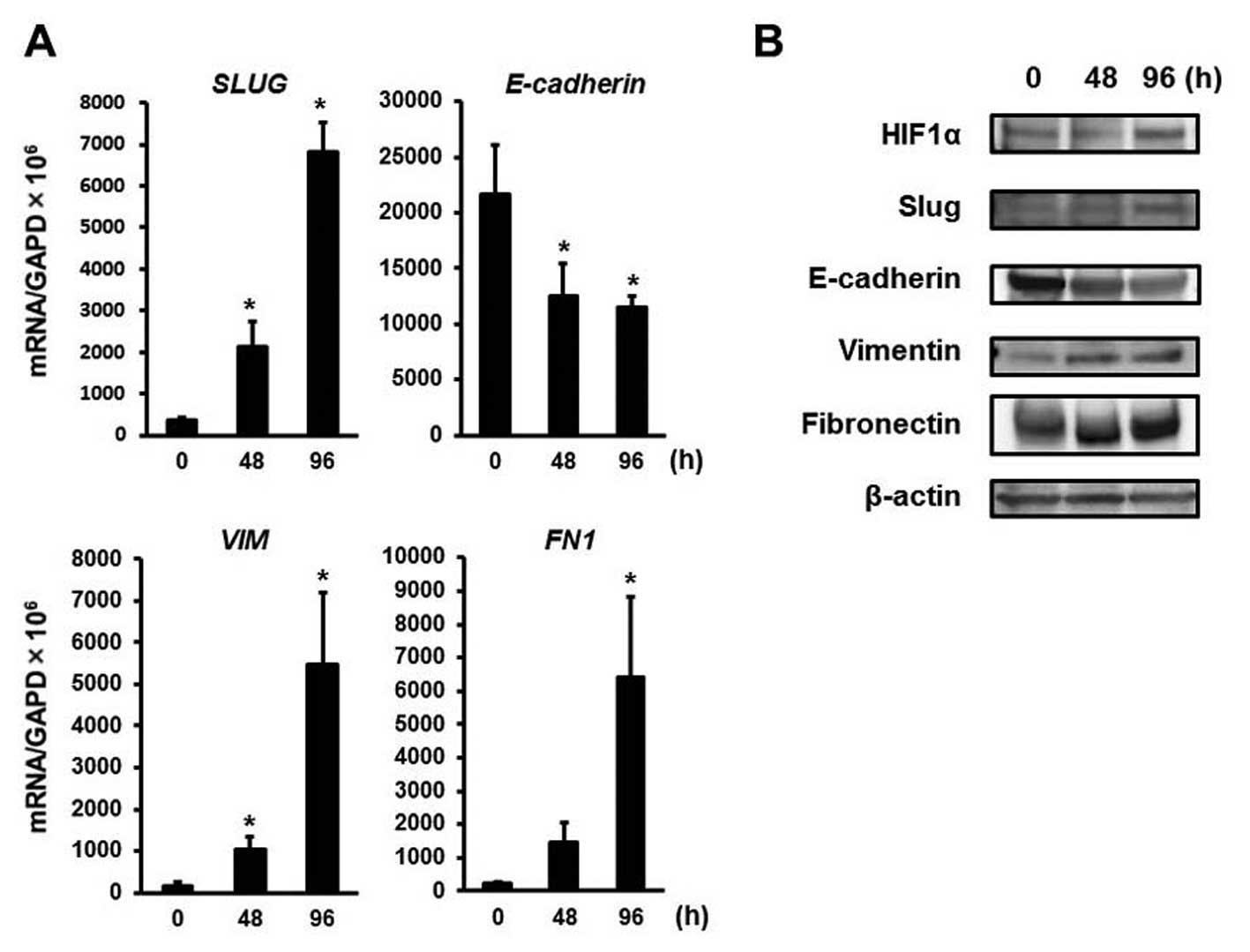
The EMT is characterized by an increase in cell
scattering and an elongation of the cell shape (18,19).
To evaluate whether hypoxia mediates the EMT in the H3122 cell
line, changes in the mRNA expression levels of EMT-related genes
were evaluated using real-time RT-PCR. Hypoxia time-dependently
upregulated SLUG mRNA expression, which is considered to be
a master regulator of the EMT (Fig.
4A). The downregulation of E-cadherin is also known to be a
pivotal cellular event in the EMT (19,20).
E-cadherin mRNA expression was clearly downregulated under
hypoxia (Fig. 4A). The expression
of mesenchymal marker VIM and the FN1 mRNA was also
upregulated (Fig. 4A). Consistent
with the mRNA changes, hypoxia time-dependently upregulated the
protein expression of slug, fibronectin, and vimentin and
downregulated the expression of E-cadherin, along with HIF1α
upregulation, which plays a central role in the hypoxic cellular
responses (21) (Fig. 4B).
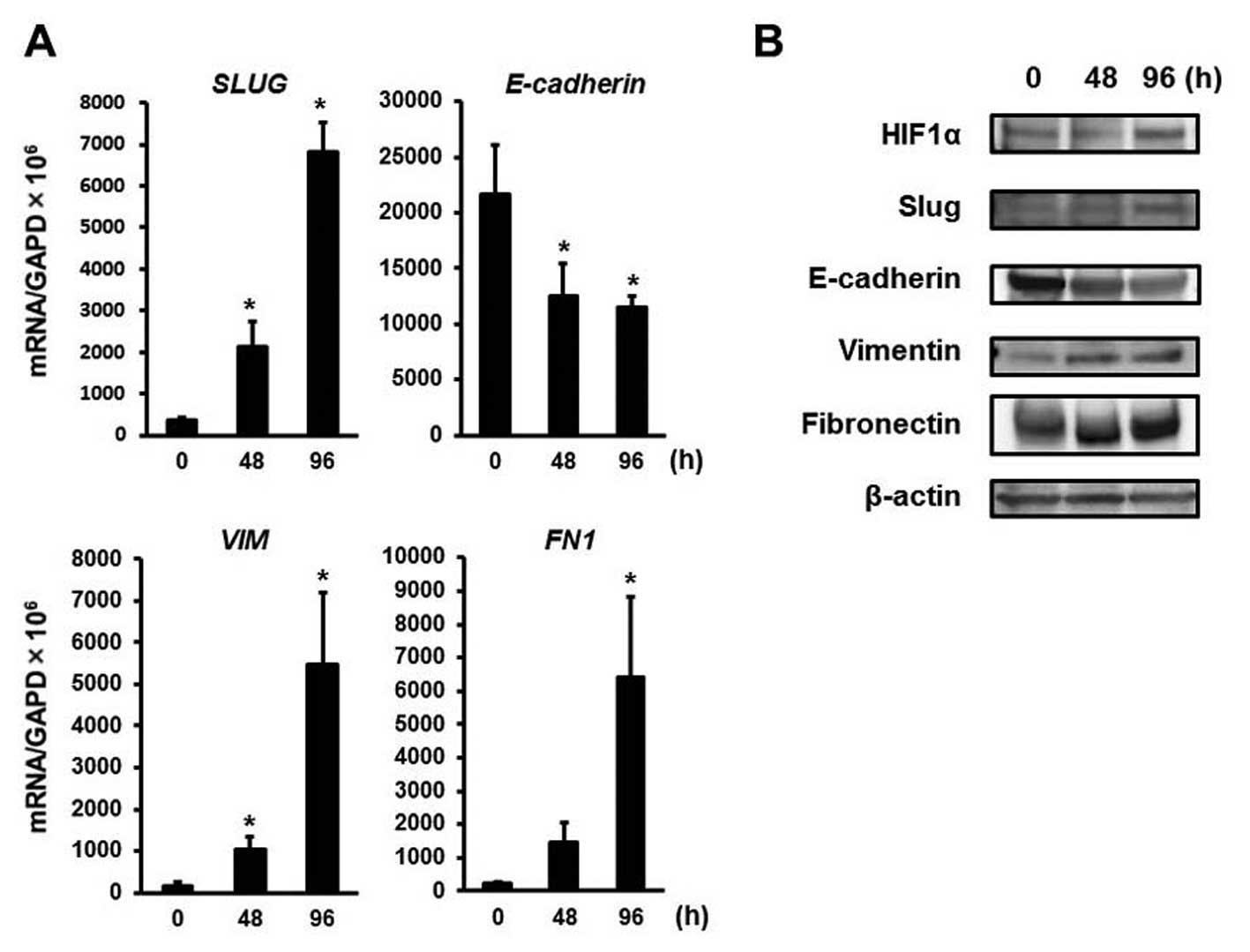 | Figure 4Real-time RT-PCR and western blot
analyses for EMT-related molecules. (A) Real-time RT-PCR for
EMT-related genes. To evaluate whether hypoxia mediates the EMT in
H3122 cells, changes in the mRNA expression levels of EMT-related
genes were evaluated using real-time RT-PCR. The experiment was
performed in triplicate. Hypoxia upregulated SLUG mRNA
expression (48 h, *P=0.030 and 96 h,
*P=0.0053). E-cadherin mRNA expression was
clearly downregulated under hypoxia (48 h, *P=0.035 and
96 h, *P=0.042). The expression of mesenchymal marker
VIM and FN1 mRNA was also upregulated (48 h,
*P=0.025 and *P=0.079, respectively and 96 h,
*P=0.031 and *P=0.044, respectively).
Columns, mean of independent triplicate experiments; error bars,
SD; *P<0.05. (B) Western blot analyses for
EMT-related molecules. Consistent with the mRNA changes, hypoxia
time-dependently upregulated the protein expression of slug,
fibronectin, and vimentin and downregulated the expression of
E-cadherin in the cell line, along with HIF1α upregulation. β-actin
was used as an internal control. |
HIF1A-knockdown effect on hypoxia-induced
EMT and the resistance to ALK inhibitors
As a major transcription factor, HIF1α plays a
central role in hypoxic cellular responses, and this transcription
factor is reportedly related to the EMT (21,22).
HIF1A was knocked down using specific siRNA to investigate
whether it was a key factor in hypoxia-induced EMT and resistance
to ALK inhibitors. HIF1A-knockdown abolished the
hypoxia-induced morphologic changes (si-HIF1A), whereas the
control-siRNA did not (si-Scr) (Fig.
5A). Similarly, HIF1A-knockdown abolished the
hypoxia-induced downregulation of E-cadherin and the upregulation
of slug, vimentin, and fibronectin (Fig. 5B). That is, HIF1A-knockdown
cancelled the hypoxia-induced EMT, resulting in a
mesenchymal-epithelial transition (MET). In addition, the
resistance to crizotinib was abolished by HIF1A-knockdown
(Fig. 5C). These findings indicate
that HIF1α transcriptionally regulates the expressions of
EMT-related molecules during hypoxia and is implicated in
hypoxia-induced resistance to ALK inhibitors in the H3122 cell
line.
 | Figure 5HIF1A-knockdown effect on the
H3122 cell line under hypoxia. To investigate whether HIF1α was a
key factor in hypoxia-induced EMT and resistance to ALK inhibitors,
HIF1A was knocked down using specific siRNA (H3122/si-HIF1A)
or a control (H3122/si-Scr). (A) Morphologic change. Both
H3122/si-HIF1A and H3122/si-Scr cell lines were incubated for 48 h
under a hypoxic state. HIF1A-knockdown abolished the
hypoxia-induced morphologic changes (si-HIF1A), whereas the
control-siRNA did not (si-Scr). Scale bar, 20 μm. (B) Western blot
analyses for EMT-related molecules. Before the sample collection,
both the H3122/si-HIF1A and the H3122/si-Scr cell lines were
incubated for 48 h under hypoxia. HIF1A-knockdown cancelled
the hypoxia-induced downregulation of E-cadherin and the
upregulation of slug, vimentin, and fibronectin. β-actin was used
as an internal control. (C) Growth inhibitory effect of crizotinib.
To examine the sensitivity, we used an MTT assay during a hypoxic
state. The experiment was performed in triplicate. Under hypoxia,
the H3122/si-HIF1A cell line was more sensitive to crizotinib,
compared with the H3122/si-Scr cell line. The graphs, mean of
independent triplicate experiments; error bars, SD. |
Discussion
The EML4-ALK rearrangement has been
identified in 5–10% of NSCLC cases, and ALK inhibitors show marked
antitumor effects in such tumors (8–11).
However, some of these tumors are resistant to inhibitors, and
acquired resistance to ALK inhibitors has already been found to
limit the therapeutic potential of these agents (23–25);
thus, an investigation of the mechanisms underlying such resistance
is warranted. In this study, we found that hypoxia mediated the
resistance to ALK inhibitors in the H3122 NSCLC cell line with an
ALK rearrangement and that the resistance arose from
hypoxia-induced EMT. To the best of our knowledge, this is the
first report to show that hypoxia mediates the resistance to ALK
inhibitors via EMT.
Several reports have discussed resistance to ALK
inhibitors, such as secondary mutations in the ALK tyrosine kinase
domain, the activation of other receptor tyrosine kinases (RTK),
the EMT, and so on (23–27). Second-generation ALK inhibitors
(i.e., alectinib and ceritinib) can be effective against resistant
tumors with secondary mutations, and heat shock protein 90
inhibitors or the inhibition of other RTK signals can also overcome
the resistance (24,25,28,29).
The EMT is a cellular process of morphological change from an
epithelial polarized shape to a mesenchymal fibroblastoid shape, in
addition to accompanying behavioral changes such as enhanced
mobility (18,19). Recently, several studies have
reported that this phenomenon is strongly associated with cancer
cell stemness (30,31) and resistance to drugs such as
EGFR-TKIs (32–34). Our present study showed that
hypoxia-induced EMT was associated with resistance not only to a
first-generation ALK inhibitor, crizotinib, but also to a
second-generation inhibitor, alectinib. Similarly, another study
has demonstrated that the EMT mediates resistance to both first-
and second-generation ALK inhibitors (27). In addition, our study showed that
HIF1A-knockdown, which promoted MET, abolished the
resistance. These findings suggest that EMT is associated with both
first- and second-generation ALK inhibitors in NSCLC with an ALK
rearrangement and that MET can cancel the resistance.
Hypoxic cancer cells can be aggressive and exhibit
metastatic phenotypes with lower sensitivity to apoptotic signals
(12). HIF1α is a key
transcription factor that is induced by hypoxia (21), and it activates the transcription
of genes implicated in tumor angiogenesis, cell survival, and
resistance to chemotherapeutic drugs (12–14).
Similarly, in our present study, activated AKT and ERK signals were
less inhibited by crizotinib, and crizotinib-induced apoptosis was
also inhibited under hypoxia. In addition, it has been reported
that HIF1α stability induced by hypoxia promotes EMT via an
EMT-triggering signal (i.e., TGFB and Notch), inflammation (i.e.,
TNFα, IL-1, and IL-6), and EMT transcriptional factors (i.e.,
twist, snail and slug) (22). In
the present study, slug, which is one of the master regulators of
EMT, was upregulated along with the upregulation of HIF1α during
hypoxia, resulting in EMT and resistance to ALK inhibitors.
HIF1A-knockdown downregulated slug expression, resulting in
MET, which abolished the resistance to ALK inhibitors. Previous
studies have shown that hypoxia mediates the resistance to
EGFR-TKIs in EGFR-mutated NSCLC via an EGFR signal or cancer
cell stemness (13,14). However, our study shows for the
first time, the association between hypoxia-induced EMT and
resistance to ALK inhibitors in NSCLC with an ALK rearrangement.
Indeed, the involvement of EMT in acquired resistance to crizotinib
in a clinically treated patient has been reported, with a tumor
specimen exhibiting a large quantity of necrotic tissue (35). Necrosis is strongly related to
hypoxia; therefore, this finding suggests that hypoxia can induce
EMT. To overcome this resistance, combination with HIF inhibitors
or anti-angiogenic therapies might be a promising strategy, and
further research is needed.
In conclusion, we have found that hypoxia mediates
the resistance to ALK inhibitors in the H3122 NSCLC cell line with
an ALK rearrangement. The resistance comes from
hypoxia-induced EMT, which can be overcome by the inhibition of HIF
or anti-angiogenic therapies. Our findings provide novel insight
into the resistance to ALK inhibitors in NSCLC with an ALK
rearrangement.
Acknowledgements
We thank Mr. Shinji Kurashimo, Mr. Yoshihiro Mine,
Ms. Eiko Honda, Ms. Tomoko Kitayama, and Ms. Ayaka Kurumatani for
their technical assistance. We thank Dr P.A. Jänne (Department of
Medical Oncology, Dana-Farber Cancer Institute, Boston, MA, USA)
for providing the H3122 cell line. This study was supported by the
Third-Term Comprehensive 10-Year Strategy for Cancer Control and
Grant-in Aid from the Japan Society for the Promotion of Science
Fellows.
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar
|
|
2
|
Siegel R, DeSantis C, Virgo K, et al:
Cancer treatment and survivorship statistics, 2012. CA Cancer J
Clin. 62:220–241. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weinstein IB: Cancer. Addiction to
oncogenes - the Achilles heal of cancer. Science. 297:63–64. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Paez JG, Janne PA, Lee JC, et al: EGFR
mutations in lung cancer: correlation with clinical response to
gefitinib therapy. Science. 304:1497–1500. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lynch TJ, Bell DW, Sordella R, et al:
Activating mutations in the epidermal growth factor receptor
underlying responsiveness of non-small-cell lung cancer to
gefitinib. N Engl J Med. 350:2129–2139. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pao W, Miller V, Zakowski M, et al: EGF
receptor gene mutations are common in lung cancers from ‘never
smokers’ and are associated with sensitivity of tumors to gefitinib
and erlotinib. Proc Natl Acad Sci USA. 101:13306–13311. 2004.
|
|
7
|
Mok TS, Wu YL, Thongprasert S, et al:
Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N
Engl J Med. 361:947–957. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Soda M, Choi YL, Enomoto M, et al:
Identification of the transforming EML4-ALK fusion gene in
non-small-cell lung cancer. Nature. 448:561–566. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kwak EL, Bang YJ, Camidge DR, et al:
Anaplastic lymphoma kinase inhibition in non-small-cell lung
cancer. N Engl J Med. 363:1693–170. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shaw AT, Kim DW, Nakagawa K, et al:
Crizotinib versus chemotherapy in advanced ALK-positive lung
cancer. N Engl J Med. 368:2385–2394. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Seto T, Kiura K, Nishio M, et al:
CH5424802 (RO5424802) for patients with ALK-rearranged advanced
non-small-cell lung cancer (AF-001JP study): a single-arm,
open-label, phase 1–2 study. Lancet Oncol. 14:590–598.
2013.PubMed/NCBI
|
|
12
|
Brown JM and Wilson WR: Exploiting tumour
hypoxia in cancer treatment. Nat Rev Cancer. 4:437–447. 2004.
View Article : Google Scholar
|
|
13
|
Minakata K, Takahashi F, Nara T, et al:
Hypoxia induces gefitinib resistance in non-small-cell lung cancer
with both mutant and wild-type epidermal growth factor receptors.
Cancer Sci. 103:1946–1954. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Murakami A, Takahashi F, Nurwidya F, et
al: Hypoxia increases gefitinib-resistant lung cancer stem cells
through the activation of insulin-like growth factor 1 receptor.
PLoS One. 9:e864592014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Arao T, Fukumoto H, Takeda M, Tamura T,
Saijo N and Nishio K: Small in-frame deletion in the epidermal
growth factor receptor as a target for ZD 6474. Cancer Res.
64:9101–9104. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tanaka K, Arao T, Maegawa M, et al: SRPX2
is overexpressed in gastric cancer and promotes cellular migration
and adhesion. Int J Cancer. 124:1072–1080. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kaneda H, Arao T, Tanaka K, et al: FOXQ1
is overexpressed in colorectal cancer and enhances tumorigenicity
and tumor growth. Cancer Res. 70:2053–2063. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee JM, Dedhar S, Kalluri R and Thompson
EW: The epithelial-mesenchymal transition: new insights in
signaling, development, and disease. J Cell Biol. 172:973–981.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
De Craene B and Berx G: Regulatory
networks defining EMT during cancer initiation and progression. Nat
Rev Cancer. 13:97–110. 2013.PubMed/NCBI
|
|
20
|
Wheelock MJ, Shintani Y, Maeda M, Fukumoto
Y and Johnson KR: Cadherin switching. J Cell Sci. 121:727–735.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Harris AL: Hypoxia - a key regulatory
factor in tumour growth. Nat Rev Cancer. 2:38–47. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jiang J, Tang YL and Liang XH: EMT: a new
vision of hypoxia promoting cancer progression. Cancer Biol Ther.
11:714–723. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Choi YL, Soda M, Yamashita Y, et al:
EML4-ALK mutations in lung cancer that confer resistance to ALK
inhibitors. N Engl J Med. 363:1734–1739. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Katayama R, Shaw AT, Khan TM, et al:
Mechanisms of acquired crizotinib resistance in ALK-rearranged lung
cancers. Sci Transl Med. 4:120ra172012.PubMed/NCBI
|
|
25
|
Katayama R, Khan TM, Benes C, et al:
Therapeutic strategies to overcome crizotinib resistance in
non-small cell lung cancers harboring the fusion oncogene EML4-ALK.
Proc Natl Acad Sci USA. 108:7535–7540. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tanizaki J, Okamoto I, Okabe T, et al:
Activation of HER family signaling as a mechanism of acquired
resistance to ALK inhibitors in EML4-ALK-positive non-small cell
lung cancer. Clin Cancer Res. 18:6219–6226. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kim HR, Kim WS, Choi YJ, Choi CM, Rho JK
and Lee JC: Epithelial-mesenchymal transition leads to crizotinib
resistance in H2228 lung cancer cells with EML4-ALK translocation.
Mol Oncol. 7:1093–1102. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sakamoto H, Tsukaguchi T, Hiroshima S, et
al: CH5424802, a selective ALK inhibitor capable of blocking the
resistant gatekeeper mutant. Cancer Cell. 19:679–690. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Friboulet L, Li N, Katayama R, et al: The
ALK inhibitor ceritinib overcomes crizotinib resistance in
non-small cell lung cancer. Cancer Discov. 4:662–673. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chiou SH, Wang ML, Chou YT, et al:
Coexpression of Oct4 and Nanog enhances malignancy in lung
adenocarcinoma by inducing cancer stem cell-like properties and
epithelial-mesenchymal transdifferentiation. Cancer Res.
70:10433–10444. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Scheel C and Weinberg RA: Cancer stem
cells and epithelial-mesenchymal transition: concepts and molecular
links. Semin Cancer Biol. 22:396–403. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rho JK, Choi YJ, Lee JK, et al: Epithelial
to mesenchymal transition derived from repeated exposure to
gefitinib determines the sensitivity to EGFR inhibitors in A549, a
non-small cell lung cancer cell line. Lung Cancer. 63:219–226.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Suda K, Tomizawa K, Fujii M, et al:
Epithelial to mesenchymal transition in an epidermal growth factor
receptor-mutant lung cancer cell line with acquired resistance to
erlotinib. J Thorac Oncol. 6:1152–1161. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sequist LV, Waltman BA, Dias-Santagata D,
et al: Genotypic and histological evolution of lung cancers
acquiring resistance to EGFR inhibitors. Sci Transl Med.
3:75ra262011.PubMed/NCBI
|
|
35
|
Kobayashi Y, Sakao Y, Ito S, et al:
Transformation to sarcomatoid carcinoma in ALK-rearranged
adenocarcinoma, which developed acquired resistance to crizotinib
and received subsequent chemotherapies. J Thorac Oncol. 8:e75–e78.
2013. View Article : Google Scholar
|