1. Introduction
Breast cancer (BC) is a global health problem and
one of the principal causes of female morbidity and mortality
(1–3). Its distribution (incidence,
prevalence) and the economic burden it imposes on national health
services make it a major public health concern both in developed
and developing countries (4).
BC is the most common neoplasm affecting women aged
<45 years and is even more prevalent in the 45–65-year age
group. BC is the main cause of female death from cancer
worldwide.
In 2008 ~1.4 million new BC diagnoses were made
throughout the world and 446,000 women died of BC; in the same year
incidence in EU Member States (EU28) was ~450,000 new cases with
140,000 deaths, accounting for a mean incidence rate of 70.7 and a
mean mortality rate of 16.7 per 100,000 women (world
age-standardized rate, ASR-W) (5).
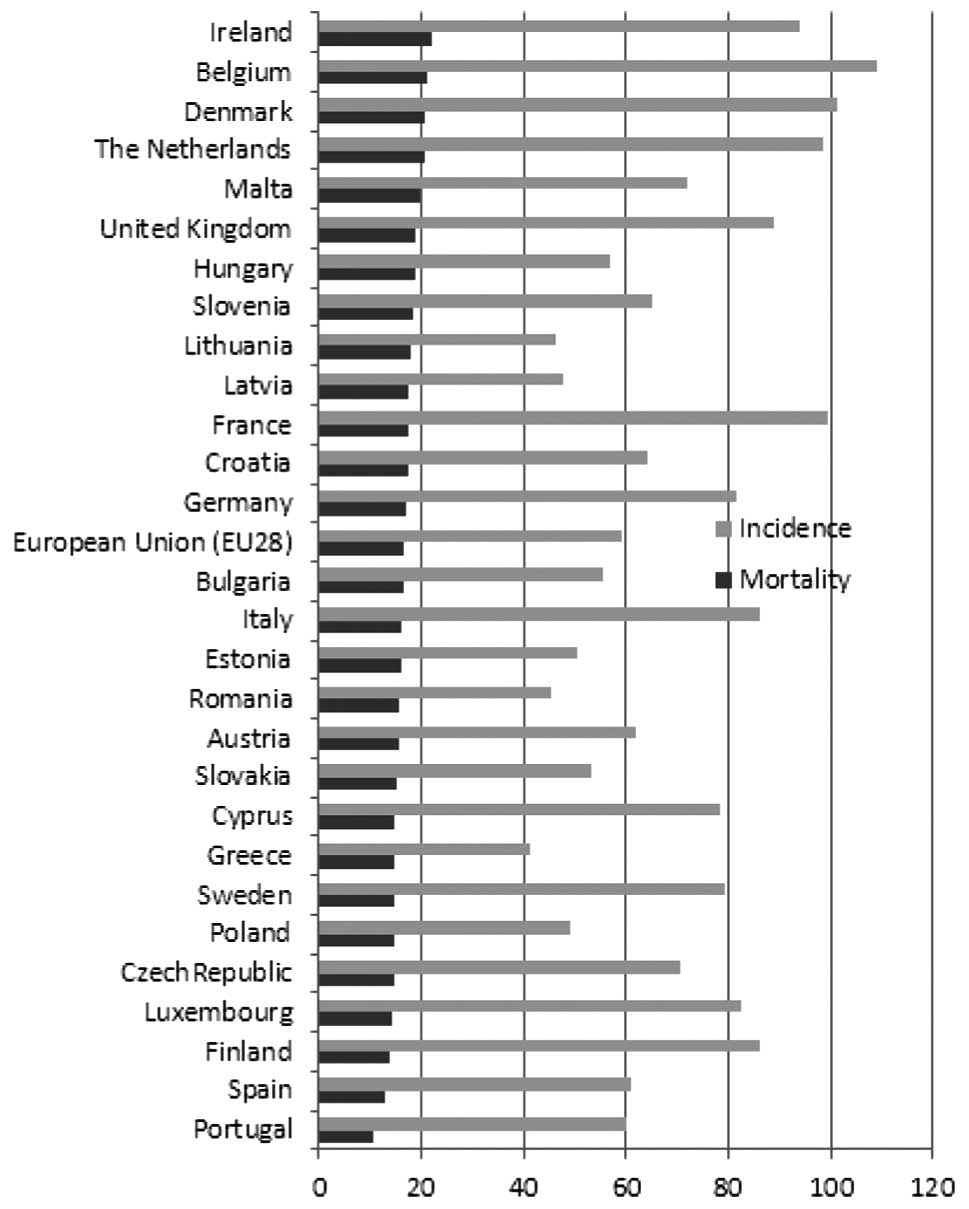
Different incidence, mortality and survival rates
are due to different risk factors, availability of organized
screening programmes, and access to effective treatment (1). Despite the fact that mortality tends
to be higher in less prosperous countries (Fig. 1) (6), the incidence of BC in Western Europe
is among the highest in the world (5) and BC prevention is a major public
health goal also in the EU.
Retrospective studies of death causes among females
over the past 30 years based on World Health Organization data in
the majority of European countries have reported a variety of
situations with considerable changes in BC mortality rates,
including a ~40% reduction in Ireland and a 17% increase in
Romania. The most developed North-Western European countries all
experienced reductions, while increments were recorded in Central
European States (Table I). The
highest reductions involved women aged <50 years also in areas
lacking active screening programmes; reductions were less striking
among 50- to 69-year olds, and a greater variability, even
including strong increments, was found among women older than 70
years (7–10).
 | Table IBreast cancer standardized mortality
and incidence rates in European Union Member States and changes in
mortality rates from 1989 to 2006. |
Table I
Breast cancer standardized mortality
and incidence rates in European Union Member States and changes in
mortality rates from 1989 to 2006.
| Member state | Mortality
ratea | Incidence
ratea | Change in mortality
% |
|---|
| Austria | 15.4 | 62.1 | −26.8 (7) |
| Belgium | 21.0 | 109.2 | −24.6 (12) |
| Bulgaria | 16.5 | 55.5 | −0.8 (7) |
| Croatia | 17.6 | 64.0 | −0.3 (41) |
| Cyprus | 14.9 | 78.4 | NA |
| Czech Republic | 14.5 | 70.8 | NA |
| Denmark | 20.8 | 101.1 | −17.8 (7) |
| Estonia | 15.9 | 50.2 | −20.8 (7) |
| European Union
(EU28) | 16.7 | 63.1 | +9.6 (7) |
| Finland | 13.7 | 86.1 | −11.7 (7) |
| France | 17.6 | 99.7 | −10.7 (7) |
| Germany | 16.9 | 81.8 | −21.3 (53) |
| Greece | 14.9 | 41.4 | +1.4 (7) |
| Hungary | 18.6 | 56.8 | −11.4 (7) |
| Ireland | 21.8 | 93.9 | −26.7 (12) |
| Italy | 16.1 | 86.3 | −22.8 (7) |
| Latvia | 17.6 | 47.9 | +11.4 (7) |
| Lithuania | 17.8 | 46.4 | −0.7 (7) |
| Luxembourg | 14.2 | 82.3 | −34.1 (7) |
| Malta | 19.6 | 72.2 | NA |
| Poland | 14.7 | 48.9 | −25.0 (12) |
| Portugal | 10.7 | 60.0 | −5.9 (7) |
| Romania | 15.6 | 45.4 | +17.8 (7) |
| Slovakia | 15.1 | 53.4 | +16.6 (7) |
| Slovenia | 18.4 | 64.9 | −1.5 (7) |
| Spain | 12.9 | 61.0 | −16.1 (7) |
| Sweden | 14.8 | 79.4 | −26.8 (7) |
| The
Netherlands | 20.5 | 98.5 | −16.8 (12) |
| United Kingdom | 18.6 | 89.1 | −29.6/−35 (46) |
An increased BC incidence and a peak in the 1980s in
all countries was followed by a reduction in BC mortality both in
countries adopting screening programmes and in those lacking them,
probably due to advances in surgical techniques and treatments in
all countries (11,12) (Table
I).
The favourable effects of organized screening are
however well established. A number of trials have shown large
reductions in mortality (13–17)
that in a study carried out in the Netherlands actually reached 70%
(18); despite some possible
biases in showing the mortality reduction, all have consistently
demonstrated the effectiveness of screening in reducing BC
mortality (19).
In 2003 the European Council recommended the
implementation of cancer screening programmes based on European
best-practice guidelines (20).
According to the International Agency for Cancer
Research, participants in organized screening programmes, where
50–69-year-old women are invited to undergo mammography at 2-year
intervals, are 35% less likely to die from BC (21). According to a more recent review of
methodologically more stringent studies the probable impact of EU28
screening programmes on women invited to screen is a 26% reduction
in mortality (95% confidence interval, CI, 13–36 %) at 6–11-year
follow-up (22).
Despite widespread agreement among EU Member States
on the important role of population-based (PB) screening in
controlling cancer, the 2007 EU report reviewing compliance with
Council recommendations found that several states still had no BC
screening programme. We review the progress of EU28 screening
programmes as of March 2014.
2. Screening techniques
Clinical breast examination (CBE) is the basic
physical examination of the breast, especially in symptomatic
women. In the French programme it is an integral part of
first-level screening (23),
guiding in its performance and interpretation. Albeit carried out
by experienced professionals integration with other tests is
required in presence of suspicious finding or sign.
Mammography is the sole screening method recognized
by the European Commission for women aged 50–69 years. It is the
morphological method enabling examination of the breast in its
entirety and offering the highest sensitivity also for early-stage
tumours, especially in women with predominantly dense breasts. Its
specificity is affected by breast density and reporting
technique.
A review of the European literature examining the
impact of mammographic screening on BC mortality found a reduction
of 25–31% among invited women and of 38–48% among those who
actually screened (24). According
to the authors the reason for the debate on BC screening is the
adoption of analytical methods unsuitable to capture the real
effects of screening.
An independent British study confirmed these data
and found an ~20% reduction in BC mortality among women subjected
to screening, with ~1% overdiagnosis (25). However further analysis of the data
led the authors to state that overdiagnosis rates cannot be
quantified with precision. Views on how to evaluate the risk of
overdiagnosis differ, resulting in estimates that can range from 0
to 50% depending on the method used (26).
Overdiagnosis has been attracting growing interest;
the issue is closely related to the availability of sensitive
diagnostic tests and to the high probability of detecting
slow-growing or non-aggressive lesions. It is a useful parameter to
assess the impact of screening on overall female health and is
evaluated by comparing tumour incidence in women screened for a
given period and in women who have never been screened.
An Italian study based on cancer registry data
assessed the effect of BC screening on the reduction of diagnoses
of highly invasive lesions. Organized programmes that had been
active for several years were associated with a significant, stable
reduction in the incidence of pT4 lesions and with an increase in
pT2 lesions starting in the 3rd-4th year of the programme, with an
incidence rate ratio that decreased from 0.81 (95% CI, 0.75–0.88)
to 0.71 (95% CI, 0.64–0.79) in the 7th-8th year (27).
Finally, a large number of diagnostic centres have
adopted digital mammography, which has improved diagnosis and
enables better scan management and storage. The image is shown in
real time on high-resolution monitors and is later archived in
electronic image filing systems. The adoption of digital
mammography in 2007 rapidly resulted in a doubling of referral
rates in the Netherlands screening programme (28); moreover, the improved equipment
sensitivity resulted in a reduction in false-positives.
Computer-assisted techniques combined with digital mammography also
enhance lesion detection (29).
3. Breast cancer screening: spontaneous or
organized?
In 2003 the European Commission recommended PB
screening for women aged 50–69 years; in 2007 programmes based on
Council indications were active or were being organized in 22
states.
Alternatives to organized screening, proposed with a
view to achieving earlier diagnosis, encourage self-referral to
breast units interconnected on line, also with a view to monitoring
the quality of examinations. These models exploit and improve
existing diagnostic resources and facilities and aim at tailoring
diagnostic and clinical protocols to the risk profile and clinical
condition of each subject; moreover they are useful in settings
where it is difficult to use classic screening methods with
individual invitations. However, several national and European
experiences indicate that screening by invitation achieves high
levels of coverage more rapidly and that the cost of organized
programmes is more limited (30–33).
4. The situation in EU28
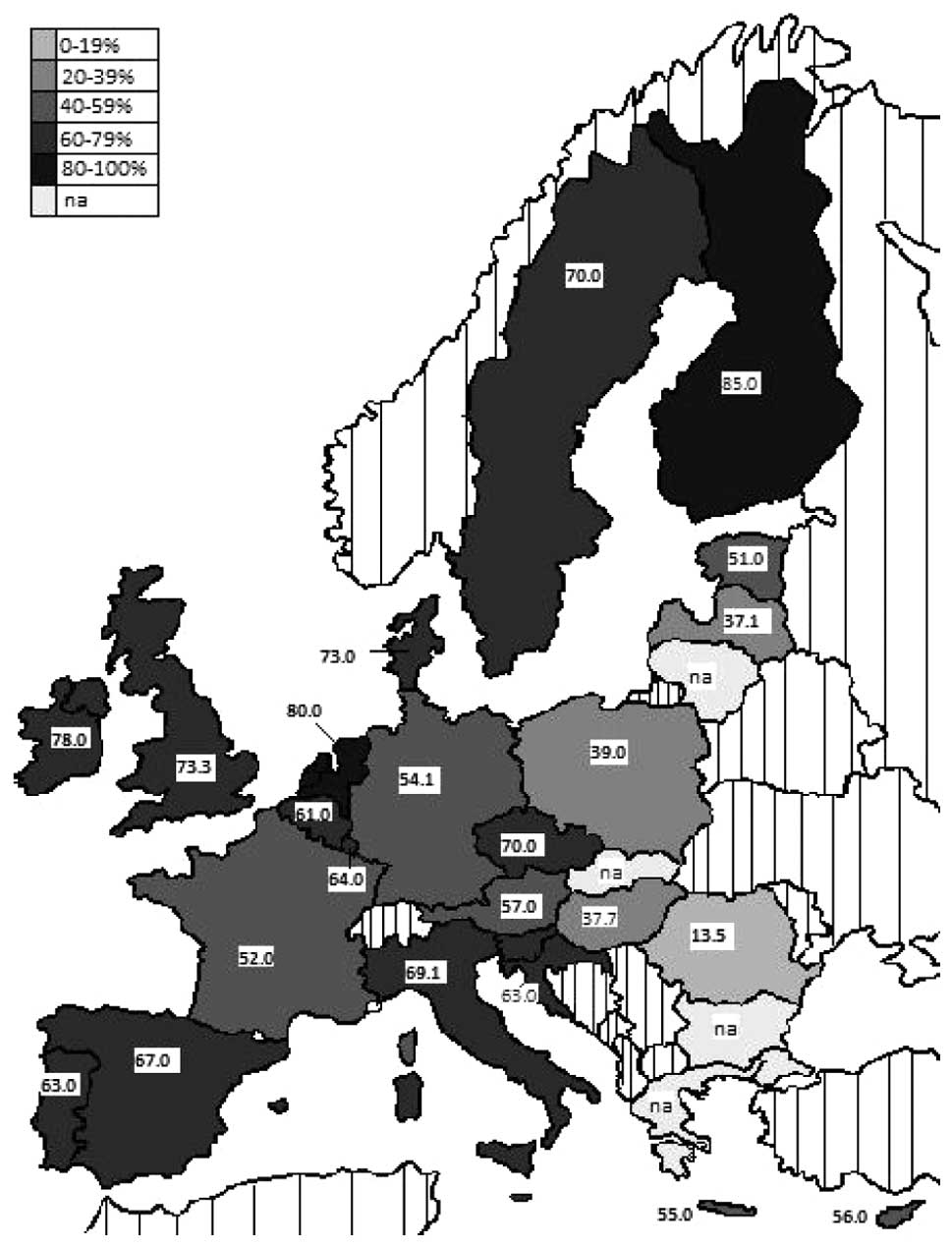
The current situation of screening programmes in
EU28 is described below and reported in Table II and shown in Fig. 2. The present study is based on the
most recent data available from PubMed-indexed journals, the
websites of the Health ministries of each member state, and the
websites of national cancer observatories; failing these sources,
information was sought in scientific journals published in the
local language.
 | Table IIDistribution of cancer screening
programmes in EU28 as of March 2014. |
Table II
Distribution of cancer screening
programmes in EU28 as of March 2014.
| Region/member
state | Programme type and
extension | Screening method in
use | Views | Double | Screening interval
reading (years) | Age of target
population | Programme start
date | Natw coverage | Attendance in 2010
(%) (46) |
|---|
| Austria | NPB | Natw | Fm | 2 | No | 2 | >40 | 1974 | - | NA |
| PB | Rega | Dm | 2 | | 1/2 | 40–59/60–69 | 2007 | 2008 | 57.0 (35) |
| Belgium | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 2001 | - | 61.0 (12) |
| Bulgaria | NPB | Local | Fm | - | - | - | 45–69 | 2011 | - | NA |
| Croatia | PB | Natw | Fm Dm | 2 | Yes | 2 | 50–69 | - | 2006 | 63.0 |
| Cyprus | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 2003 | 2006 | 56.0 (43) |
| Czech Republic | NPB | Natw | Fm Dm | 2 | Yes | 2 | 45–69 | 2002 | 2007 | 70.0 (46) |
| Denmark | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 1991 | 2010 | 73.0 |
| Estonia | PB | Natw | Dm | - | - | 2 | 50–65 | 2002 | 2007 | 51.0 |
| Finland | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 1987 | 1989 | 85.0 |
| France | PB | Natw | Fm Dm CBE | 2 | Yes | 2 | 50/74 | 1989 | 2004 | 52.0 |
| Germany | PB | Natw | Fm Dm | 2 | Yes | 2 | 50–69 | 2005 | 2009 | 54.1 |
| Greece | NPB | Pilot | Fm | 2 | - | 1/2 | 40–50/64 | - | - | NA |
| Hungary | PB | Natw | Fm | 2 | Yes | 2 | 45–65 | 2002 | - | 53.5 (55) |
| Ireland | PB | Natw | Dm | 2 | Yes | 2 | 50–64 | 2000 | 2008 | 78.0 (12) |
| Italy | PB | Natw | Fm Dm | 2 | Yes | 2 | 50–69 (74) | 1990 | 2007 | 69.1 |
| Latvia | PB | Natw | Fm Dm | 2 | No | 2 | 50–69 | 2008 | 2009 | 37.1 |
| Lithuania | PB | Natw | Fm | 2 | Yes | 2 | 50–69 | 2005 | - | NA |
| Luxembourg | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 1992 | 1992 | 64.0 |
| Malta | PB | Natw | Dm | 2 | - | 3 | 50–59 | 2008 | 2009 | 55.0 (46) |
| The
Netherlands | PB | Natw | Dm | 2 (1) | Yes | 2 | 50–74 | 1988 | 1997 | 80.0 |
| Poland | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 2006 | 2007 | 39.0 |
| Portugal | PB | Natw | Dm | 2 | Yes | 2 | 45–69 | 1990 | 2005 | 63.0 |
| Romania | NPB | Local | Fm | 2 | No | (3) (2) 1 | 40+ | - | - | 13.5 (46) |
| Slovakia | NPB | - | - | - | - | 2 | 40+ | - | - | NA |
| Slovenia | PB | Natw | Dm | 2 | Yes | 2 | 50–69 | 2008 | - | 75 |
| Spain | PB | Natw | Fm Dm | 2 | Yes | 2 | (45) 50–69 | 1990 | 2009 | 67.0 |
| Sweden | PB | Natw | Fm Dm | 2 | Yes | (1.5) 2 | 40 (50)–(69)
74 | 1986 | 1996 | 70.0 |
| United Kingdom | PB | Natw | Fm Dm | 2 | No | 3 | 50–(64) 70 | 1988 | 1995 | 73.3 |
In 1974 Austria was the first EU Member State to
implement a BC screening programme. Screening remains opportunistic
in most of the country, with mammography offered to all women
>40 years old (34). In Tyrol
an organized PB programme offering a yearly mammogram to women with
healthcare insurance aged 40–49 years and biannual examination to
those aged 60–69 years has been active since 2007; it does not
envisage double reading of mammograms (35).
With 147.5 cases per 100,000 women, Belgium has the
highest BC incidence in the world (36). Its organized screening programme
offers mammograms every 2 years to women aged 50–69 years. However,
opportunistic screening is quite widespread, and ~80% of diagnostic
mammographic examinations are believed to be related to spontaneous
screening. Moreover 85% of examinations are combined with
ultrasound (US) scanning performed on the same day; this may
indicate that especially in Wallonia and in Brussels US is used as
a screening method. This in turn may account for the large number
of second-line examinations (biopsy and fine needle aspiration)
performed each year (37).
Attendance is ~61% according to a 2010 survey (38).
Bulgaria has no active national programme. BC
prevention is entrusted to a private association, the Centre for
Protection of Rights in Health Care, which since 2011 has been
conducting screening examinations with mobile units throughout the
country. The local authorities in the municipalities visited are in
charge of making appointments for women aged 40–60years who wish to
be examined (39).
In 2006 Croatia set up an organized screening
programme offering biannual mammograms at various sites (public
hospitals, universities, private facilities) (40,41).
A recent quality audit of sample mammograms highlighted severe
problems in breast positioning and lesion detection that had the
potential to affect screening effectiveness and that could be
addressed by improving personnel training and operative strategies
(42).
Cyprus set up its first pilot programme in Nicosia
in 2003; the programme was extended nationwide in 2006 (43). It is a centralized PB screening
programme that is offered to women aged 50–69 years. The Health
Ministry website contains information on the shift to digital
mammography (44).
The Czech Republic does not have a centralized PB
screening programme. Physicians and gynaecologists advise women
aged 45–69 to undergo a free examination; in 2010 the upper age
limit was removed. Mammograms are taken with traditional or digital
machines (45). The results are
archived in a national database that is accessible online
(www.svod.cz) and allows monitoring BC trends at both
the national and regional level, also providing several reference
parameters. Screening adhesion is high (46).
For many years screening programmes have been in
place in few areas of Denmark, Copenhagen (1991) and Fyn (1993)
being the first areas to be served. Nationwide coverage was
achieved in 2010. Mammograms are offered to women aged 50–69 years
(47). For a long time the first
round offered two views and the second a single view; the two views
have subsequently been extended to the second round. The reduction
in mortality found in areas offering screening (12) has raised controversy because
similar rates seem to be found in areas not offering it (47,48).
Estonia made a large effort since it implemented a
BC screening programme in 2002. At first the target population was
limited to 45–59 year olds with healthcare coverage, but since 2007
mammograms are offered to all 50–65-year-olds. Digital mammography
was introduced in 2006 (49). The
+9.6% mortality rate (12) needs
careful assessment by comparison with a study reporting a rate of
+25.5% in 1990–2002 (50).
In Finland BC screening is managed by local
authorities, who are responsible for the activation, delivery and
quality assessment of services, which can be provided autonomously
or be outsourced from public or private bodies. The central
government evaluates service quality through a team of experts.
According to the Health and Social Services Ministry website
(51) participation in 2009 was
84% compared with the OECD mean of 62%.
In France women aged 50–74 are offered mammograms
every 2 years followed by CBE. Screening is by invitation; digital
mammography was introduced in 2008. France is the first EU country
by volume of yearly screening mammograms (52).
In Germany a number of pilot projects were followed
in 2005 by activation of the national programme. The national
centre invites women aged 50–69 years to screen every 2 years
(53).
Greece has the lowest BC incidence in EU28 but a
rising mortality rate. Screening is exclusively opportunistic and
attendance is unknown (54). Some
sporadic pilot projects have been active since the 1990s.
In Hungary the organized programme, implemented in
2002, is paralleled by strong spontaneous screening. Although
adhesion to the organized programme is on the rise (53.5% in 2005),
>350,000 women use non-organized screening (55).
Ireland introduced screening in 2000 and slowly
extended it nationwide. The target population is the 50–69-year age
group; the examination is offered every 2 years. Digital
mammography was adopted nationwide in 2008. The use of mobile units
is widespread (56).
In Italy PB screening began in 1990; nationwide
coverage was attained in 2007. The target population is generally
aged 50–69 years, but in some regions it includes 45-year-olds and
in others women aged ≤74 years are also invited. The mean rate of
adhesion to the various programmes is 60.5%. Spontaneous screening
is not easy to quantify, but a 2010 survey (project PASSI) found
that 61% of women aged 40–49 years had undergone at least one
preventive mammogram (57).
Latvia activated screening for BC and uterine cancer
in 2009. The management of invitations is centralized and is based
on the population registry. The equipment is generally analogical
but some facilities have digital machines. Participation, poor at
first, is slowly rising: at the end of October 2013 it was 37%. The
Health Ministry website (58)
provides updated information on the activity of mobile units and
attendance rates.
Lithuania activated a screening programme in 2005
but could not implement it nationwide due to lack of facilities and
specialized personnel. No information is available on its progress
(59). The mortality rate does not
seem to have changed over the last 20 years.
Luxembourg adopted a programme with centralized
management of invitations and reminders in 1992 (60). In 2001 it began to adopt digital
equipment to archive images and enable double reading also remotely
(61).
In Malta screening was implemented in 2009. The
Health Ministry provides all the necessary information on the
project but it may have planned poorly, because Malta boosts one of
the worst records in terms of the number of mammograms taken within
national screening programmes (5%); in contrast private centres,
which 50% of the population have visited at least once, are quite
busy (46).
In the Netherlands screening began in 1989. Women
aged 50–69 years are screened at 2-year intervals and those aged
≤74 years were added in 1998. Two views are taken in the first
round and a single view thereafter. Nationwide adoption of digital
mammography was completed in 2010 (28).
In 2007 Poland set up a centralized PB programme
offering digital mammograms to women aged 50–69 years at 2-year
intervals, except those undergoing follow-up (62). Radiologists at all levels use
computer-assisted techniques to improve diagnostic performances
(63).
Portugal implemented its first region-based
screening programme in 1990; nationwide screening was achieved in
2005. The Health Ministry aims at 60% coverage by 2016 (64). The programme offers digital
mammography to women aged 45–69 years, also with mobile units.
In Romania, which has no screening programme, not
for profit organizations help the government increase cancer
awareness and prevention and provide healthcare and screening on
request. The Romanian Cancer Society (65) recommends screening mammograms at
3-year intervals from age 40 years, biannual examination between 45
and 50 and yearly screening thereafter.
In 2008 Slovakia began to organize a BC screening
programme that has not yet been activated. Even though prevention
is merely opportunistic, 80% of women have been examined at least
once in their life (46).
In Slovenia the PB DORA screening programme,
introduced in 2008, has been geared to achieve nationwide coverage
over a few years. Women aged 50–69 years are invited to screen at
mobile units or at the Ljubljana cancer centre. The response has
been very good, exceeding a participation rate of 75% after the
third screening round (66).
Spain introduced a BC screening programme in Navarre
in 1990 and achieve national coverage in 2009. Digital mammography
is spreading. The target population (aged 50–69 or 45–69 years in
different programmes) is invited to screen at 2-year intervals
(67).
Sweden has one of the first programmes introduced in
Europe, but exhibits considerable organizational variability.
Biannual mammograms are generally offered to women aged 50–69
years, but in >60% of the country women aged 40–49 years are
also invited to test every 18 months; in about half of the country
70–74-year-olds are also offered a biannual mammogram.
The UK has different PB programmes in England,
Wales, Scotland and Northern Ireland, with testing usually offered
at 3-year intervals. In Northern Ireland the screening programme,
introduced in 1990, was initially aimed at 50–64-year-olds but was
extended to 70-year-olds in 2004. In Scotland the target population
is aged 50–70 years. The shift to digital mammography is ongoing.
Wales activated its programme in 1989 (50–70-year-olds). It adopted
digital mammography in 2011. In England the shift is nearly
complete (68). Here a trial begun
in 2010 is assessing the value of extending BC screening to
47–73-years-olds (69). Mortality
in 1989–2006 fell by 35% in England and Wales, by 30% in Scotland
and by 29% in Northern Ireland (12).
5. Discussion
BC is probably a heterogeneous group of diseases
with distinct natural histories. The notion that cancer progresses
inexorably from atypia to carcinoma in situ, invasive
carcinoma and then metastasis is no longer tenable (70–74).
Early diagnosis of abnormalities is increasingly
important to gain a greater understanding of the risk of
progression of the individual lesions and of the disease in
general. Crucial issues for screening programmes involve the
management of such abnormalities to improve survival and the
interval between examinations (21). We review the epidemiological
scenario of BC, active screening programmes, and changes in EU28
mortality rates.
The introduction of a cancer screening programme
entails an increased rate of diagnoses; any changes to a screening
programme that has been active for some years may also have an
impact on incidence. For instance, the introduction of digital
mammography in the Netherlands led to a strong increase in BC
diagnosis but has not so far affected mortality. The mortality data
tend to be more stable over time, and their change is related to a
variety of disease-related factors. Examination of BC mortality
rate changes shows that reductions also occurred in countries that
set up a screening programme after 2006. This is explained by the
survival-enhancing effect of more effective diagnostic methods,
surgical techniques and treatments (11).
Overall, screening programmes offer the advantage of
early lesion detection, enabling their management before
progression and worsening.
Adhesion to BC screening, like participation in
colorectal tumour screening (75),
is still among the weaknesses of the programmes adopted by several
EU28 countries.
The target rate of participation of 75% is not
achieved several states. Poor knowledge of the disease and of the
attendant risk (76) as well as
organizational barriers (e.g., test hours coinciding with work
hours; the need for reaching facilities far away from one’s
residence) may significantly limit participation, especially in
less prosperous countries. This situation does not meet one of the
main criteria of screening programmes, their ethics, since all
women should have equal access to cancer screening and to quality
treatment and post-treatment care irrespective of place of
residence, social standing, job and education. Yet marked
disparities are currently found among member states, regions and
even hospitals in the same area.
In this light the 2008 Commission Report focuses on
the implementation of Council recommendations by aiming at reducing
disparities among states by promoting the sharing of the best
experiences and abilities gained. To do this, capillary diffusion
of appropriate information systems capable of evaluating cancer
trends in the population, like cancer registries, is required. Such
tools are highly cost-effective, since important information on
cancer diagnosis/treatment is provided at small cost to the
healthcare service, enabling identification and management of any
weaknesses, especially in problems areas and programmes. Full
exchange and circulation of information among member states would
enable the system to be completed and EU collaboration to
flourish.
6. Conclusions
Even though the European scenario currently requires
a curb on public spending, the various national health services
should guarantee screening access and participation to the largest
possible number of subjects, also considering that adhesion is a
weakness of many programmes. Awareness campaigns and training of
healthcare providers may be a good and economical starting point to
improve the knowledge of disease risk and enhance screening
compliance also in the short term; at the same time the cancer
registries system would allow monitoring the effectiveness of the
fight against cancer also in the light of the fact that population
ageing entails a constant increase in the incidence of these
diseases.
References
|
1
|
Althuis MD, Dozier JM, Anderson WF, Devesa
SS and Brinton LA: Global trends in breast cancer incidence and
mortality 1973–1997. Int J Epidemiol. 34:405–412. 2005.PubMed/NCBI
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
3
|
Hortobagyi GN, de la Salazar GJ, Pritchard
K, et al: The global breast cancer burden: variations in
epidemiology and survival. Clin Breast Cancer. 6:391–401. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Forbes JF: The incidence of breast cancer:
the global burden, public health considerations. Semin Oncol.
24(Suppl 1): S1-20–S1-35. 1997.PubMed/NCBI
|
|
5
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: GLOBOCAN 2008: Cancer Incidence and
Mortality Worldwide IARC Cancerbase No, 10. International Agency
for Research on Cancer; Lyon: 2010
|
|
6
|
Khatib OMN: Guidelines for the Early
Detection and Screening of Breast Cancer. EMRO Technical
Publications Series, 30. WHO World Health Organization; Cairo:
2006
|
|
7
|
Autier P1, Boniol M, La Vecchia C, Vatten
L, Gavin A, Héry C and Heanue M: Disparities in breast cancer
mortality trends between 30 European countries: retrospective trend
analysis of WHO mortality database. BMJ. 341:c36202010. View Article : Google Scholar
|
|
8
|
Bosetti C, Bertuccio P, Malvezzi M, et al:
Cancer mortality in Europe, 2005–2009 and an overview of trends
since 1980. Ann Oncol. 24:2657–2671. 2013.
|
|
9
|
Levi F, Bosetti C, Lucchini F, Negri E and
La Vecchia C: Monitoring the decrease in breast cancer mortality in
Europe. Eur J Cancer Prev. 14:497–502. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tyczynski JE, Plesko I, Aareleid T, et al:
Breast cancer mortality patterns and time trends in 10 new EU
member states: mortality declining in young women, but still
increasing in the elderly. Int J Cancer. 112:1056–1064. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Botha JL, Bray F, Sankila R and Parkin DM:
Breast cancer incidence and mortality trends in 16 European
countries. Eur J Cancer. 39:1718–1729. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Autier P, Boniol M, Gavin A and Vatten LJ:
Breast cancer mortality in neighbouring European countries with
different levels of screening but similar access to treatment:
trend analysis of WHO mortality database. BMJ. 343:d44112011.
View Article : Google Scholar
|
|
13
|
Fielder HM, Warwick J, Brook D, et al: A
case-control study to estimate the impact on breast cancer death of
the breast screening programme in Wales. J Med Screen. 11:194–198.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Allgood PC, Warwick J, Warren RM, Day NE
and Duffy SW: A case-control study of the impact of the East
Anglian breast screening programme on breast cancer mortality. Br J
Cancer. 98:206–209. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gabe R, Tryggvadóttir L, Sigfússon BF,
Olafsdóttir GH, Sigurdsson K and Duffy SW: A case-control study to
estimate the impact of the Icelandic population-based mammography
screening program on breast cancer death. Acta Radiol. 48:948–955.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Puliti D, Miccinesi G, Collina N, et al:
Effectiveness of service screening: a case control study to assess
breast cancer mortality reduction. Br J Cancer. 99:423–427. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Roder D, Houssami N, Farshid G, et al:
Population screening and intensity of screening are associated with
reduced breast cancer mortality: evidence of efficacy of
mammography screening in Australia. Breast Cancer Res Treat.
108:409–416. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Paap E, Holland R, den Heeten GJ, et al: A
remarkable reduction of breast cancer deaths in screened versus
unscreened women: a case-referent study. Cancer Causes Control.
21:1569–1573. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Puliti D and Zappa M: Breast cancer
screening: are we seeing the benefit? BMC Med. 10:1062012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
L 327/34 Council Recommendation of 2
December 2003 on cancer screening (2003/878/EC). Official Journal
of the European Union. European Union; Brussels: pp.
L327/34–L327/37. 16–12. 2003
|
|
21
|
Vainio H and Bianchini F: IARC Handbooks
of Cancer Prevention Volume 7 Breast Cancer Screening. IARC Press,
International Agency for Research on Cancer; Lyon: 2002
|
|
22
|
Njor S, Nyström L, Moss S, et al: Breast
cancer mortality in mammographic screening in Europe: a review of
incidence-based mortality studies. J Med Screen. 19(Suppl 1):
S33–S41. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
International Cancer Screening Network;
Atlanta: Breast Cancer Screening Programs in 26 ICSN Countries,
2012: Organization, Policies, and Program Reach. http://appliedresearch.cancer.gov/icsn/breast/screening.html.
Accessed Nov 23 2013
|
|
24
|
Broeders M, Moss S, Nyström L, et al: The
impact of mammographic screening on breast cancer mortality in
Europe: a review of observational studies. J Med Screen. 19(Suppl
1): 14–25. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Marmot MG, Altman DG, Cameron DA, Dewar
JA, Thompson SG and Wilcox M: The benefits and harms of breast
cancer screening: an independent review. Lancet. 380:1778–1786.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Marmot MG, Altman DG, Cameron DA, Dewar
JA, Thompson SG and Wilcox M: The benefits and harms of breast
cancer screening: an independent review. Br J Cancer.
108:2205–2240. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Foca F, Mancini S, Bucchi L, et al:
Decreasing incidence of late-stage breast cancer after the
introduction of organized mammography screening in Italy. Cancer.
119:2022–2028. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Timmers JM, den Heeten GJ, Adang EM, Otten
JD, Verbeek AL and Broeders MJ: Dutch digital breast cancer
screening: implications for breast cancer care. Eur J Public
Health. 22:925–929. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Houssami N, Lord SJ and Ciatto S: Breast
cancer screening: emerging role of new imaging techniques as
adjuncts to mammography. Med J Aust. 190:493–497. 2009.PubMed/NCBI
|
|
30
|
Beemsterboer PM, de Koning HJ, Warmerdam
PG, et al: Prediction of the effects and costs of breast-cancer
screening in Germany. Int J Cancer. 58:623–628. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
De Koning H: Breast cancer screening;
cost-effective in practice? Eur J Radiol. 33:32–37. 2000.PubMed/NCBI
|
|
32
|
Hakama M, Pukkala E, Heikkilä M and Kallio
M: Effectiveness of the public health policy for breast cancer
screening in Finland: population based cohort study. BMJ.
314:864–867. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hakama M, Pukkala E, Söderman B and Day N:
Implementation of screening as a public health policy: issues in
design and evaluation. J Med Screen. 6:209–216. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vutuc C, Waldhoer T and Haidinger G:
Breast cancer trends: opportunistic screening in Austria versus
controlled screening in Finland and Sweden. Eur J Cancer Prev.
15:343–346. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Oberaigner W, Daniaux M, Geiger-Gritsch S,
Knapp R, Siebert U and Buchberger W: Introduction of organised
mammography screening in Tyrol: results following first year of
complete rollout. BMC Public Health. 11:6732011.PubMed/NCBI
|
|
36
|
Ferlay J, Steliarova-Foucher E,
Lortet-Tieulent J, et al: Cancer incidence and mortality patterns
in Europe: estimates for 40 countries in 2012. Eur J Cancer.
49:1374–1403. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Verleye L, Desomer A, Gailly J and Robays
J: Dépistage du cancer du sein: comment identifier les femmes
exposées à un risque accru - Quelles techniques d’imagerie
utiliser? Good Clinical Practice (GCP), . Bruxelles: Centre fédéral
d’expertise des soins de santé (KCE). KCE Reports 172B
D/2011/10273/91. 2011
|
|
38
|
Hermesse J: Résultats de 6 ans de dépistag
eorganisé du cancer du sein en Belgique. [Internet] Communiqué par
l’Agence intermutualiste. Education Santé. 261:november. 2010, pp.
5–6, http://www.educationsante.be/es/imprarticle.php?id=1309.
Accessed Oct 18, 2013
|
|
39
|
Center for Protection of Rights in Health
Care (CZPZ). Sophia (Bulgary): Screening examinations for breast
cancer. http://www.czpz.org/index.php?option=com_content&view=category&id=50&Itemid=107&lang=en.
Accessed Nov 24, 2013
|
|
40
|
Tesic V, Kolaric B, Znaor A, Kuna SK and
Brkljacic B: Mammographic density and estimation of breast cancer
risk in intermediate risk population. Breast J. 19:71–78. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kelava I, Tomičić K, Kokić M, et al:
Breast and gynecological cancers in Croatia, 1988–2008. Croat Med
J. 53:100–108. 2012.
|
|
42
|
Brnić Z, Blašković D, Klasić B, et al:
Image quality of mammography in Croatian nationwide screening
program: comparison between various types of facilities. Eur J
Radiol. 81:e478–e485. 2012.PubMed/NCBI
|
|
43
|
Hadjisavvas A, Loizidou MA, Middleton N,
et al: An investigation of breast cancer risk factors in Cyprus: a
case control study. BMC Cancer. 10:1–10. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ministry of Health Cyprus. Cyprus: breast
cancer screening. http://www.moh.gov.cy.
Accessed Oct 15, 2013
|
|
45
|
Majek O, Danes J, Skovajsova M, et al:
Breast cancer screening in the Czech Republic: time trends in
performance indicators during the first seven years of the
organised programme. BMC Public Health. 11:2882011.PubMed/NCBI
|
|
46
|
Eurostat Breast Cancer. Eurostat screening
statistics. http://epp.eurostat.ec.europa.eu/statistics_explained/index.php/Breast_cancer_screening_statistics.
Accessed 25 Oct, 2013
|
|
47
|
Domingo L, Jacobsen KK, von Euler-Chelpin
M, et al: Seventeen-years overview of breast cancer inside and
outside screening in Denmark. Acta Oncol. 52:48–56. 2013.PubMed/NCBI
|
|
48
|
Jørgensen KJ, Zahl PH and Gøtzsche PC:
Breast cancer mortality in organised mammography screening in
Denmark: comparative study. BMJ. 340:c12412010.PubMed/NCBI
|
|
49
|
Matsalu M; Ministry of Health Estonia.
Crossing borders in breast cancer screening. First International
Symposium; October 28 & 29 - 2010; Amsterdam. The Netherland.
http://www.breastcancerscreening.eu/images/stories/PDF's/101029_05_Presentation_Estonia_Meeli_Matsalu_Symposium_Crossing_borders.pdf.
Accessed Sep 17, 2013
|
|
50
|
Héry C, Ferlay J, Boniol M and Autier P:
Quantification of changes in breast cancer incidence and mortality
since 1990 in 35 countries with Caucasian-majority populations. Ann
Oncol. 19:1187–1194. 2008.PubMed/NCBI
|
|
51
|
Ministry of Health Finland. Breast Cancer
screening. Finland: http://www.stm.fi/sosiaali_ja_terveyspalvelut/terveyspalvelut/seulonnat.
Accessed Oct 16, 2013
|
|
52
|
Séradour B: Breast cancer screening in
France: an overview in 2009. Rev Prat. 60:191–199. 2010.(In
French).
|
|
53
|
Biesheuvel C, Weigel S and Heindel W:
Mammography screening: evidence, history and current practice in
Germany and other European countries. Breast Care (Basel).
6:104–109. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Tsakiroglou M, Bakalis M, Valasoulis G,
Paschopoulos M, Koliopoulos G and Paraskevaidis E: Women’s
knowledge and utilization of gynecological cancer prevention
services in the Northwest of Greece. Eur J Gynaecol Oncol.
32:178–181. 2011.
|
|
55
|
Boncz I, Sebestyén A, Pintér I, Battyány I
and Ember I: The effect of an organized, nationwide breast cancer
screening programme on non-organized mammography activities. J Med
Screen. 15:14–17. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Minister for Health and Children Ireland.
National Cancer Screening Service. http://www.cancerscreening.ie/.
Accessed Mar, 2014
|
|
57
|
Zorzi M, Fedato C, Grazzini G, et al:
Screening for colorectal cancer in Italy, 2010 survey. Epidemiol
Prev. 36(Suppl 1): 55–77. 2012.
|
|
58
|
Ministry of Health Latvia. Breast cancer
screening. http://www.vmnvd.gov.lv/lv/aktualitates.
Accessed Nov 10, 2013
|
|
59
|
Breast Cancer Screening Germany 11/17/2006
in European-Hospital. http://www.european-hospital.com/en/article/743-Breast_cancer_screening.html.
Accessed Oct 12, 2013
|
|
60
|
Autier P, Shannoun F, Scharpantgen A, et
al: A breast cancer screening programme operating in a liberal
health care system: the Luxembourg Mammography Programme,
1992–1997. Int J Cancer. 97:828–832. 2002.PubMed/NCBI
|
|
61
|
Shannoun F, Schanck JM, Scharpantgen A,
Wagnon MC, Ben Daoud M and Back C: Organisational aspects of
mammography screening in digital settings: first experiences of
Luxembourg. Radiat Prot Dosimetry. 129:195–198. 2008. View Article : Google Scholar
|
|
62
|
Szynglarewicz B, Matkowski R, Kasprzak P,
et al: The effectiveness of population-based breast cancer
screening programme. Pol Merkur Lekarski. 26:117–120. 2009.(In
Polish).
|
|
63
|
Cancer.gov. Atlanta: International Cancer
Screening Network; Policies on Number of Views, Double-Reading, and
Computer Aided Detection for Breast Cancer Screening Programs in 26
ICSN Countries. 2012, http://appliedresearch.cancer.gov/icsn/breast/policies.reading.html.
Accessed Oct 23, 2013
|
|
64
|
Ministry of Health Portugal. Breast cancer
screening. http://www.portaldasaude.pt/portal/conteudos/a+saude+em+portugal/noticias/rastreio+estremoz+14.htm.
Accessed Dec 11, 2013
|
|
65
|
Oncologic Society Romania. Breast cancer
screening. http://www.srccjro.org/.
Accessed Dec 20, 2013
|
|
66
|
Dora Project. Breast cancer screening
Slovenia. http://www.dpor.si/en/?page_id=97.
Accessed Dec 18, 2013
|
|
67
|
Ascunce N, Salas D, Zubizarreta R, et al:
Cancer screening in Spain. Ann Oncol. 21(Suppl 3): iii43–51. 2010.
View Article : Google Scholar
|
|
68
|
Pubblic Health England: NHS. Breast cancer
screening programme. http://www.cancerscreening.nhs.uk/breastscreen/digital-mammography.html.
Accessed Dec 16, 2013
|
|
69
|
Moser K, Sellars S, Wheaton M, et al:
Extending the age range for breast screening in England: pilot
study to assess the feasibility and acceptability of randomization.
J Med Screen. 18:96–102. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Buerger H, Otterbach F, Simon R, Schäfer
KL, Poremba C and Diallo R: Different genetic pathways in the
evolution of invasive breast cancer are associated with distinct
morphological subtypes. J Pathol. 189:521–526. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Buerger H, Schmidt H, Beckmann A, Zänker
KS, Boecker W and Brandt B: Genetic characterisation of invasive
breast cancer: a comparison of CGH and PCR based multiplex
microsatellite analysis. J Clin Pathol. 54:836–840. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Kao J, Salari K, Bocanegra M, et al:
Molecular profiling of breast cancer cell lines defines relevant
tumor models and provides a resource for cancer gene discovery.
PLoS One. 4:e61462009.PubMed/NCBI
|
|
73
|
Prat A, Parker JS, Karginova O, et al:
Phenotypic and molecular characterization of the claudin-low
intrinsic subtype of breast cancer. Breast Cancer Res. 12:R682010.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Banegas MP, Tao L, Altekruse S, et al:
Heterogeneity of breast cancer subtypes and survival among Hispanic
women with invasive breast cancer in California. Breast Cancer Res
Treat. 144:625–634. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Altobelli E, Lattanzi A, Paduano R,
Varassi G and di Orio F: Colorectal cancer prevention in Europe:
burden of disease and status of screening programs. Prev Med.
62C:132–141. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
James TM, Greiner KA, Ellerbeck EF, Feng C
and Ahluwalia JS: Disparities in colorectal cancer screening: a
guideline-based analysis of adherence. Ethn Dis. 16:228–233.
2006.PubMed/NCBI
|