Introduction
Targeting of cancer-associated abnormalities with
specific drugs is a promising strategy in treatment of disseminated
malignancies. The epidermal growth factor receptor (EGFR) is a
transmembrane tyrosine kinase receptor that regulates cell
proliferation and survival, but is abnormally expressed and/or
activated in many epithelial tumours (1,2).
EGFR is a target for several anticancer therapeutics, such as
tyrosine kinase inhibitors gefitinib and erlotinib and monoclonal
antibodies cetuximab and panitumumab (3).
High level of EGFR expression is associated with
poor prognosis in a number of cancers, such as head and neck
squamous cell carcinoma (HNSCC) (4), breast (5) and non-small-cell lung cancer (NSCLC)
(6). High EGFR expression predicts
resistance to neoadjuvant therapy with anthracyclines and taxanes
in triple-negative breast cancer (7) and relapse of HNSCC after radiotherapy
(8). Overexpression of EGFR can be
used for stratification of patients with advanced NSCLC to
gefitinib (9,10) and to first-line chemotherapy in
combination with cetuximab (11).
Patients with a high expression of EGFR in NSCLC might also benefit
from the addition of cetuximab to chemoradiotherapy, but cetuximab
might be detrimental for patients with low EGFR expression
(12). Patients with high EGFR
expression in HNSCC may benefit from hyperfractionated accelerated
radiotherapy (13). Thus,
detection of high EGFR expression levels in malignant tumours may
provide important prognostic and predictive information influencing
management of the patients.
Currently, EGFR expression level is determined using
analyses of biopsy material. However, the biopsy-based methods are
invasive and associated with morbidity. Therefore, a limited number
of biopsy samples are usually taken. Furthermore, the EGFR
expression might change over time due to genetic instability of the
cancer and/or in response to therapy (14). An appreciable discrepancy in EGFR
expression in primary tumours and corresponding metastases has been
documented in colorectal cancer (15,16)
and NSCLC (17,18). There is an unmet clinical need to
establish a methodology enabling non-invasive repeatable assessment
of EGFR expression during course of disease.
Radionuclide molecular imaging with EGFR-specific
agents might be a way to provide repetitive non-invasive assessment
of target expression level. Goldenberg and co-workers (19) have demonstrated that the
111In-labeled anti-EGFR antibody 225 (murine predecessor
of cetuximab) accumulates in human cancer xenografts in mice
proportionally to the EGFR-expression. A clinical study confirmed
that 111In-225 can visualize EGFR-expressing tumours in
patients (20). The cited study
also identified the major obstacle for EGFR visualization in
vivo, which is the expression of the receptors in multiple
normal tissues, foremost in the liver. However, the authors have
shown that increasing the injected antibody dose saturates
receptors in normal tissues but not in tumours making imaging
possible. Still, there are general issues with antibody-based
imaging agents, such as a long residence time in circulation and
slow penetration into tumours. This results in low tumour-to-blood
ratios, translating into low contrast and therefore, a low
sensitivity of imaging. Positron-emission tomography (PET) provides
better resolution and sensitivity than single photon emission
computed tomography (SPECT). Therefore, labelling of anti-EGFR
antibodies with long-lived positron emitting radionuclides
64Cu (T1/2=12.7 h) (21,22),
86Y (T1/2=14.7 h) (23,24),
and 89Zr (T1/2=78.4 h) (25,26)
has been evaluated. While 64Cu and
86Y-labelled antibodies have shown promising results in
murine models at 24–48 h, the half-life of these nuclides is too
short for clinical translation. The use of the more long-lived
89Zr is probably the only viable option in clinical
settings. Still, it would be desirable to have higher contrast than
antibodies could provide even if PET is used for imaging.
An alternative to antibodies is the use of a
radiolabelled natural ligand of EGFR, epidermal growth factor (EGF)
(27–30). This small (6 kDa) protein has much
more rapid extravasation rate than bulky (150 kDa) antibodies.
Small size results also in a rapid clearance of unbound imaging
agent via the kidneys, which is a precondition for high contrast
imaging. Railly and co-workers (28) have demonstrated that
111In-EGF provides higher tumour-to-blood ratio than
anti-EGFR antibody labelled with the same nuclide. The major issue
with the use of EGF as an imaging agent is its strong agonistic
action causing nausea, vomiting and hypotension at higher injected
doses (27). An ideal agent for
EGFR imaging should be as small as EGF but without agonistic
properties upon binding to the receptor.
Affibody molecules constitute a rather new class of
imaging agents that meet the requirements of small size and absence
of agonistic action (31).
Affibody molecules are engineered scaffold protein binders, which
are originally based on a domain of protein A (32). The use of molecular display
techniques enables selection of high-affinity affibody binders to
variety of molecular targets (31,32).
Due to the small size (7 kDa) and high affinity (low nanomolar or
subnanomolar level), affibody molecules is a very promising format
of targeting proteins for radionuclide molecular imaging (33,34).
In the clinic, affibody molecules have demonstrated feasibility of
imaging of HER2-expressing breast cancer metastases with high
specificity and sensitivity (35).
Earlier, we have reported development of high-affinity anti-EGFR
affibody molecules for the use in radionuclide imaging (36–38).
These studies resulted in development of the ZEGFR:2377 affibody
molecule that has equal affinity to human and murine EGFR (38). This makes mouse models relevant for
preclinical evaluations. In preclinical studies,
111In-DOTA-ZEGFR:2377 provided a tumour-to-blood ratio
exceeding the tumour-to-blood ratios of any anti-EGFR monoclonal
antibody. However, the use of the radionuclide 111In
requires SPECT for imaging. As PET imaging provides better
sensitivity of diagnostics, development of an affibody-based agent
labelled with a positron emitting nuclide would be desirable.
Previous studies (38) have shown that
111In-DOTA-ZEGFR:2377 provides the highest
tumour-to-blood ratio and therefore the best sensitivity at 24 h
after injection. Hence, the use of short-lived positron emitting
nuclides, such as 18F (T1/2=109.8 min) or
68Ga (T1/2=67.6 min), for labelling of
ZEGFR:2377 would be suboptimal. The use of a more long-lived
positron emitter would be desirable. Earlier studies have
demonstrated that the use of radiometal labels for anti-EGFR
affibody provide better contrast than the use of radiohalogens
(37), which excludes the
positron-emitting halogen 124I (T1/2=109.8
min) as a label. Therefore, a long-lived positron emitter, such as
89Zr (T1/2=78.4 h) would be a better choice
for labelling of ZEGFR:2377.
The goal of the presesnt study was to evaluate a
89Zr-labelled anti-EGFR ZEGFR:2377 affibody molecule for
imaging of EGFR expression in human xenografts in mice and to
compare imaging properties of 89Zr ZEGFR:2377 with
properties of anti-EGFR antibody 89Zr-cetuximab.
Materials and methods
Material
Zirconium-89 (solution in 1 M oxalic acid) was
purchased from Perkin-Elmer (Waltham, MA, USA).
Statistics
Data on cellular uptake and biodistribution were
analyzed by unpaired, two-tailed t-test using GraphPad Prism
(version 4.00 for Windows GraphPad Software) in order to determine
significant differences (P<0.05).
Preparation of targeting conjugates
Anti-EGFR ZEGFR:2377 affibody molecule having a
single C-terminal cysteine was produced as previously described
(38).
For labelling with 89Zr, ZEGFR:2377 was
conjugated to a maleimido derivative of deferoxamine (DFO) chelator
(Macrocyclics, Dallas, TX, USA). To reduce spontaneously formed
intermolecular disulphide bonds, affibody molecules were treated
with dithiothreitol (DTT; E. Merck, Darmstadt, Germany). Affibody
molecules (2 ml, 2.3 mg/ml in PBS) were mixed with 100 μl 1 M
Tris-HCl buffer, pH 8.0, and 63 μl DTT solution (0.5 M in water).
The mixture was incubated at 40°C for 30 min. The reduced affibody
molecules were then purified and the buffer was changed using a
disposable PD-10 column (GE Healthcare, Uppsala, Sweden)
pre-equilibrated with 0.2 M ammonium acetate, pH 5.5. The
DFO-to-ZEGFR:2377 ratio was optimized to obtain conjugate in high
yield. To do this, a 2-, 3-, 5- and 8-fold molar excess of DFO
(0.0337 μmole/μl DMSO) was added to the ZEGFR:2377 (0.5 mg in 0.72
ml 0.1 M ammonium acetate buffer, pH 5.5) under gentle shaking, and
incubated for 30 min at 40°C. Unconjugated molecules and excess
chelators were separated from the DFO-conjugated affibody molecules
on a semi-preparative RP-HPLC column (Zorbax 300SB-C18 9.4×250 mm,
5 μm particle size; Agilent Technologies, Palo Alto, CA, USA) using
a gradient from 35–60% B for 18 min at a flow rate of 0.5 ml/min
(A: 0.1% trifluoroacetic acid in water, B: 0.1% trifluoroacetic
acid in acetonitrile). The analysis was performed using
high-performance liquid chromatography and on-line mass
spectrometry (HPLC-MS) using an Agilent 1100 LC/MSD system equipped
with electrospray ionization and single quadrupole (Agilent
Technologies). The analysis was performed using a Zorbax 300SB-C18
2.1×150 mm, 3.5 μm column. Agilent ChemStation Rev. B.02.01
software (Agilent Technologies) was used for analysis and
evaluation of HPLC data. The purified conjugate (further designated
as DFO-ZEGFR:2377) was freeze-dried.
Cetuximab was conjugated with
p-isothiocyanatobenzyl-desferrioxamine (Df-Bz-NCS) as
previously described (39). The
conjugate was purified using a NAP-5 size-exclusion column
equilibrated with PBS.
Radiolabeling
DFO-ZEGFR:2377 was labelled with 89Zr
using a modified method published by Vosjan and co-workers
(39). A solution of
89Zr (67 μl, 30–40 MBq) was mixed with 30.2 μl 2 M
Na2CO3, and the mixture was incubated for 3
min. Thereafter, 100 μl 0.5 M HEPES buffer, pH 7.1 was added
followed by DFO-ZEGFR:2377 (50 μg dissolved in 240 μl ammonium
acetate, pH 5.5) and 234.5 μl 0.5 M HEPES, pH 7.1. The mixture was
incubated for 60 min at room temperature. The final purification of
89Zr-DFO-ZEGFR:2377 was performed using a NAP-5
size-exclusion column equilibrated with PBS.
For labelling of DFO-cetuximab, a solution of
89Zr (7 μl, 4 MBq) was mixed with 3 μl 2 M
Na2CO3, the mixture was incubated for 3 min
and 10 μl 0.5 M HEPES buffer, pH 7.1 was added. DFO-cetuximab (100
μg dissolved in 60 μl ammonium acetate, pH 5.5) and 60 μl 0.5 M
HEPES, pH 7.1, were added and the mixture was incubated for 90
min.
Radio-instant thin layer chromatography (radio-ITLC)
was used to measure yield, purity and stability of radiolabelled
conjugates. ITLC strips (150–771 Dark Green Tec-Control
Chromatography strips; Biodex Medical Systems, Shirley, NY, USA)
were eluted with 0.2 M citric acid, pH 2.0. An SDS-PAGE analysis
was performed [NuPAGE 4–12% Bis-Tris Gel in MES buffer ( both from
Invitrogen AB Foster City, CA, USA), 200 V constant] to
cross-validate the ITLC.
Stability of 89Zr-DFO-ZEGFR:2377 was
measured in PBS and murine blood plasma up to 24 h. For blood
stability studies, freshly labelled 89Zr-DFO-ZEGFR:2377
(10 μl) was diluted in a serum sample (240 μl) to a concentration
similar to the concentration in blood at the time of injection.
In vitro studies
In vitro binding and cellular processing
studies were performed using EGFR-expressing A431 epidermoid
carcinoma cell line (ATCC; purchased via LGC Promochem, Borås,
Sweden). Binding specificity and cellular processing of
89Zr-DFO-ZEGFR:2377 were evaluated according to methods
previously described (40). To
determine binding specificity, A431 cells (3 cell culture dishes)
were incubated for 1 h at 37°C with 10 nM
89Zr-DFO-ZEGFR:2377. Two sets of control dishes were
pre-treated with 100-fold molar excess of either non-labelled
ZEGFR:2377 or cetuximab 5 min before adding 10 nM
89Zr-DFO-ZEGFR:2377 and incubated at the same
conditions. After 1-h incubation, the incubation media were
collected, the cells were detached using trypsin and collected.
Radioactivity in cells and incubation media was measured, and
percentage of cell-bound radioactivity was measured. Binding
specificity of 89Zr-DFO-cetuximab was evaluated in the
same way.
To determine internalization rate, A431 cells were
incubated with 10 nM 89Zr-DFO-ZEGFR:2377 at 37°C in a
humidified incubator. At 1, 2, 4, 8 and 24 h after incubation
start, internalized and membrane-bound radioactivity in a set of
three dishes was determined by the acid wash method, as previously
described (40). Briefly, the
incubation medium was collected, cells were washed by an ice-cold
medium and treated with 4 M urea solution in a 0.1 M glycine
buffer, pH 2.5, for 5 min on ice. The buffer was collected, the
cells were additionally washed with the buffer and the acidic
fractions were pooled. Thereafter, the cells were lysed by a
treatment with 1 M sodium hydroxide solution (0.5 h at 37°C) for at
least 0.5 h. The basic solution containing cell debris with
internalized radioactivity was collected. Dishes were additionally
washed with sodium hydroxide and alkaline fractions were pooled.
Radioactivity of the fractions was measured. Radioactivity in
acidic fractions represented membrane-bound tracer, and
radioactivity of alkaline fraction presented internalized
tracer.
Kinetics of 89Zr-DFO-ZEGFR:2377 binding
to and dissociation from living A431 cells was measured by using
LigandTracer Yellow instrument (Ridgeview Instruments AB, Vänge,
Sweden). The data were analyzed using InteractionMap software
(Ridgeview Diagnostics AB, Uppsala, Sweden) to calculate
association rate, dissociation rate and dissociation constant at
equilibrium as previously described (41).
Animal studies
The animal experiments were planned and performed in
accordance with the national regulation on laboratory animals'
protection and were approved by the Ethics Committee for Animal
Research in Uppsala. Euthanasia was performed under Ropmpun/Ketalar
anesthesia, and all efforts were made to minimize suffering. Female
outbred BALB/c nu/nu mice were purchased from Taconic M&B a/S
(Ry, Denmark). At the time of the experiment, the average animal
weight was 19±1 g. EGFR-expressing xenografts were established by
subcutaneous injection of 107 A431 cells in the right
hind leg. The tumours were grown for 12–14 days before the
experiment. The animals were randomized into groups of four.
For biodistribution measurements, three group of
mice were intravenously injected with
89Zr-DFO-ZEGFR:2377 (20 kBq in 100 μl PBS per mouse).
The injected protein dose was adjusted to 40 μg per mouse by
non-labelled affibody molecule. One group was euthanized at 3 and
another at 24 h after injection, and distribution of radioactivity
was measured. To confirm the EGFR specificity of in vivo
targeting, the receptors in one group of mice were pre-saturated by
injection of 400 μg of non-labelled ZEGFR:2377 40 min before
injection of 89Zr-DFO-ZEGFR:2377. Biodistribution in
this group of mice was measured at 3 h after injection. For
comparison, one group of mice was injected with
89Zr-DFO-cetuximab (30 kBq/50 μg in 100 μl PBS per
mouse) and the biodistribution was measured at 48 h after injected.
After euthanasia, blood and organ samples were collected and
weighed, and their radioactivity was measured. Tissue uptake (decay
corrected) was calculated as percent of injected dose per gram (%
ID/g).
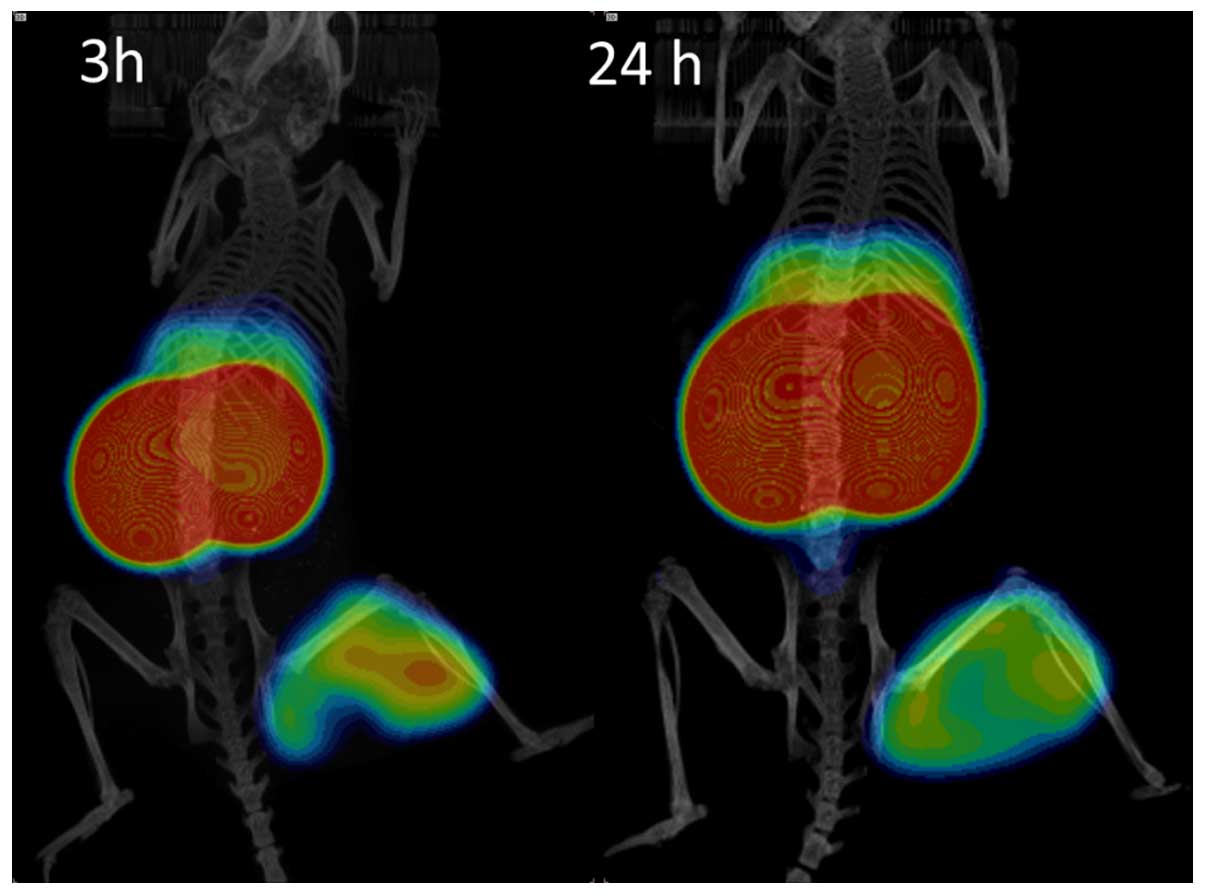
Whole body positron emission tomography
(PET)/computed tomography (CT) scans of the mice injected with
89Zr-DFO-Z2377 (45 μg, 4.6 MBq) were performed in
Triumph™ tri-modality system (TriFoil Imaging, Inc., Northridge,
CA, USA) at 3 and 24 h p.i. The animals were sacrificed by
CO2 asphyxiation immediately before being placed in the
camera. The urinary bladder was excised post-mortem due to its
proximity to tumor xenografts and kidneys. The PET scans were
conducted for 30 min followed by CT examination at the following
parameters: field of view (FOV), 8 cm; magnification, 1.48; one
frame and 512 projections for 2.13 min. CT raw files were
reconstructed by filter back projection (FBP). PET data were
reconstructed into a static image using OSEM-3D (20 iterations).
The scatter and attenuation correction were performed using their
respective CT data. PET and CT files were analyzed using PMOD
v3.508 (PMOD Technologies Ltd., Zurich, Switzerland). Coronal
PET-CT images are presented as maximum intensity projections (MIP)
in RGB color scale.
Results
Preparation of targeting conjugates
Increase of chelator-to-protein molar ratio from 3:1
to 5:1 improved the conjugation yield from 81 to 93%. Further
increase of the chelator-to-protein molar ratio to 8:1 did not
improve the conjugation (yield of 93%). Semipreparative HPLC
enabled efficient separation of DFO-ZEGFR:2377 from unconjugated
ZEGFR:2377. HPLC analysis demonstrated that the purity of
DFO-ZEGFR:2377 was >95%. The mass spectrometry analysis showed
an excellent agreement between the molecular mass of DFO-ZEGFR:2377
with the theoretical value (expected 8102.8 Da, observed 8103
Da).
Radiolabelling
Labelling of DFO-ZEGFR:2377 with 89Zr
provided yield of 99±1%. Purification using a disposable NAP-5
size-exclusion column provided purity of 100%. The identity of
conjugates was confirmed by radio-SDS-PAGE. There was no measurable
release of 89Zr from 89Zr-DFO-ZEGFR:2377
during incubation in PBS (Table
I). A minimum release (<3%) was observed in murine blood
plasma after incubation for 24 h.
 | Table IStability of
89Zr-DFO-ZEGFR:2377 in PBS and murine blood plasma. |
Table I
Stability of
89Zr-DFO-ZEGFR:2377 in PBS and murine blood plasma.
| Protein-associated
radioactivity, % |
|---|
|
|
|---|
| 1 h | 2 h | 4 h | 24 h |
|---|
| PBS | 100±0 | 100±0 | 100±0 | 100±0 |
| Plasma | 100±0 | 100±0 | 100±0 | 98.5±1.5 |
In vitro studies
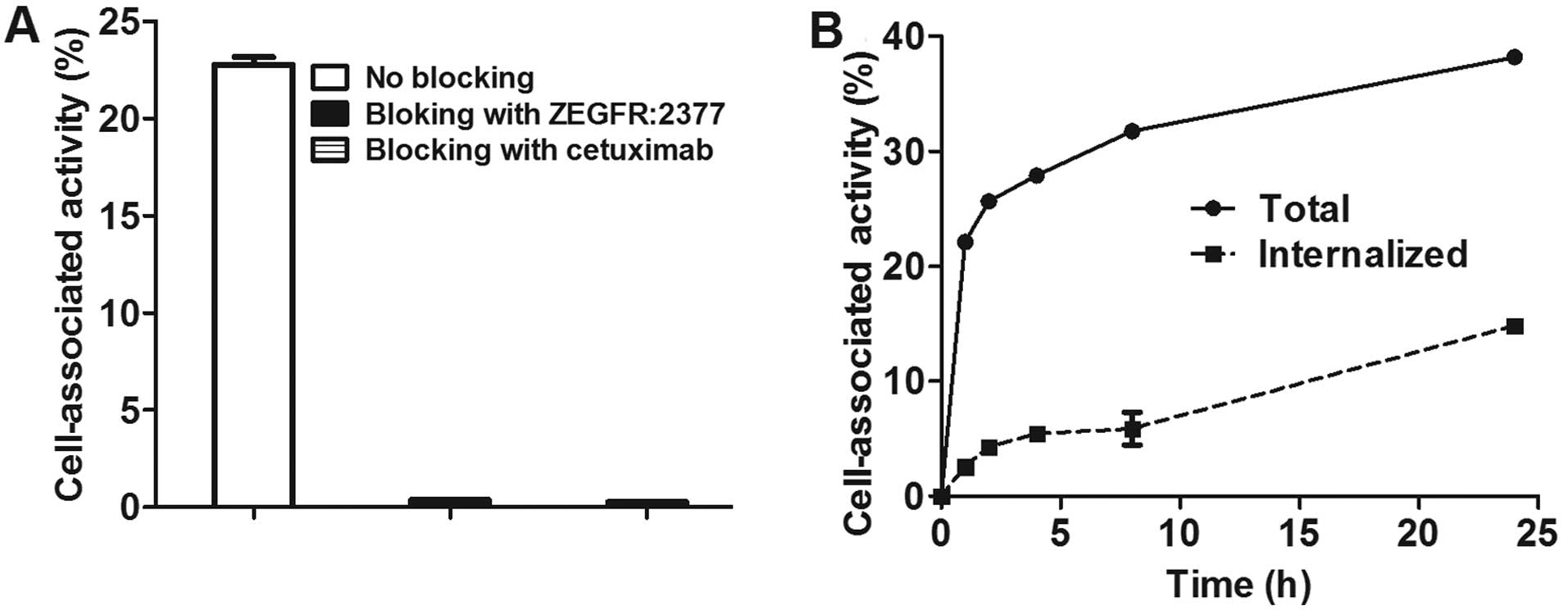
Data concerning specificity of
89Zr-DFO-ZEGFR:2377 binding to EGFR-expressing A431
cells are presented in Fig. 1A.
Pre-saturation of EGFR on A431 cells with an excess of both
non-labeled ZEGFR:2377 and cetuximab caused a highly significant
(P<1×10−5) reduction of
89Zr-DFO-ZEGFR:2377 binding to the cells.
This demonstrates saturability of binding and proves that the
binding of the conjugate to EGFR-expressing cells is
receptor-mediated. Similarly, specificity of
89Zr-DFO-cetuximab binding to A431 cells was confirmed
(data not shown).
Data concerning cellular processing of
89Zr-DFO-ZEGFR:2377 are presented in Fig. 1B. The internalization of
89Zr-DFO-ZEGFR:2377 by A431 cells was relatively slow.
The internalized fraction was ~20% after 4-h incubation and ~40%
after 24 h.
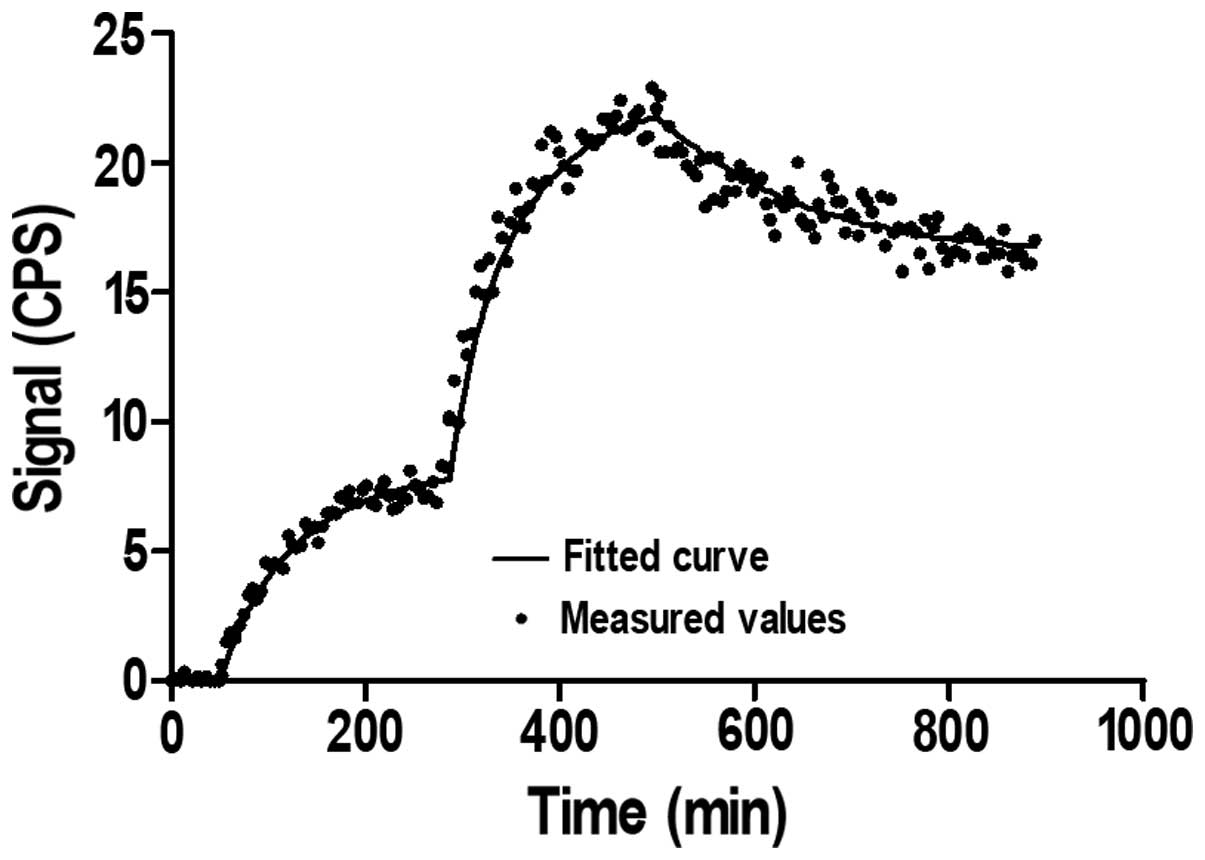
A representative LigandTracer sensorgram of
89Zr-DFO-ZEGFR:2377 binding to and dissociation from
living A431 cells is presented in Fig.
2. The interaction of 89Zr-DFO-ZEGFR:2377 was
characterized by rapid binding (association rate of
1.95±0.45×105 1/Mxs) and slow dissociation (dissociation
rate of 3.3±1.2×10−5 1/s). This provided a very high
affinity. The dissociation constant (KD) of
89Zr-labelled DFO-ZEGFR:2377 interaction with A431 cells
was 160±60 pM.
Animal studies
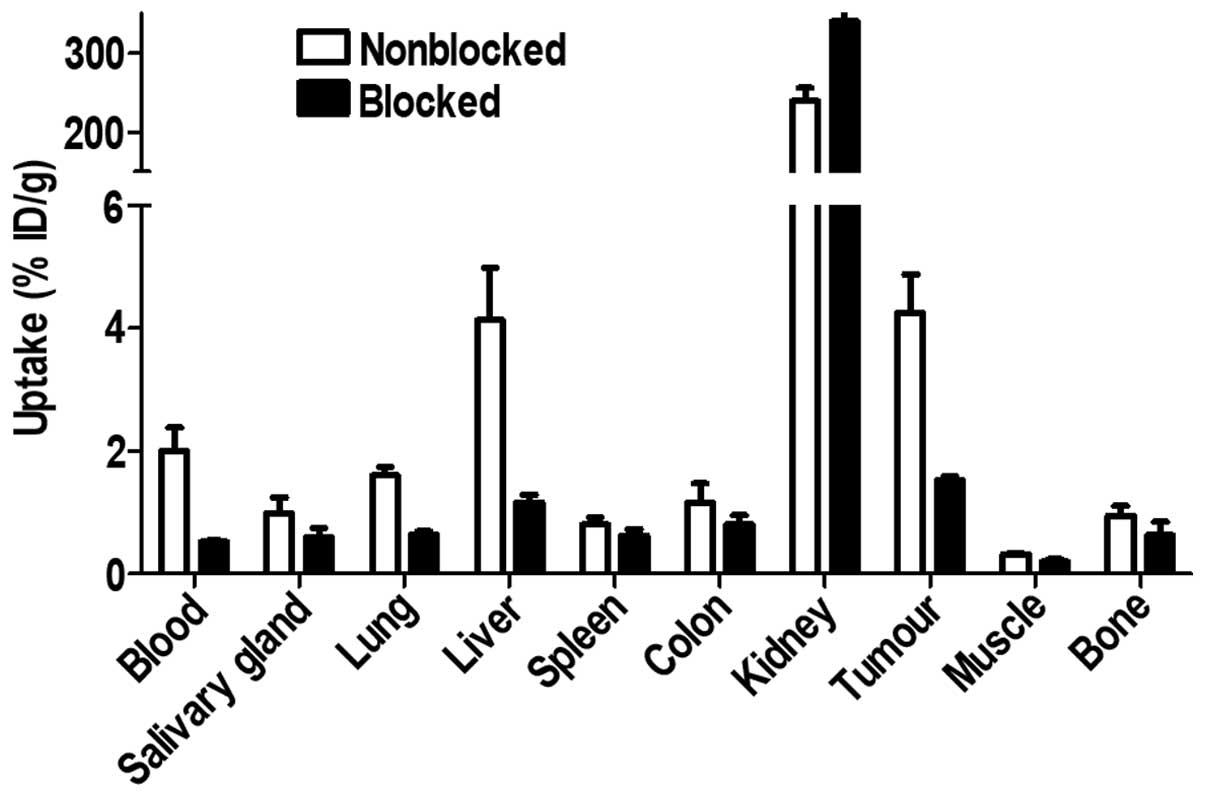
The results of an in vivo specificity test
are presented in Fig. 3.
Pre-saturation of EGFR with a large excess of non-labelled affibody
molecule caused a significant (P<0.0005) reduction in tumour
uptake. Radioactivity uptake was also significantly (P<0.05)
reduced in EGFR-expressing tissues, such as liver, salivary gland
and lung. There was also a significant reduction of uptake in blood
and muscle. Radioactivity uptake in kidneys was increased in the
blocked group.
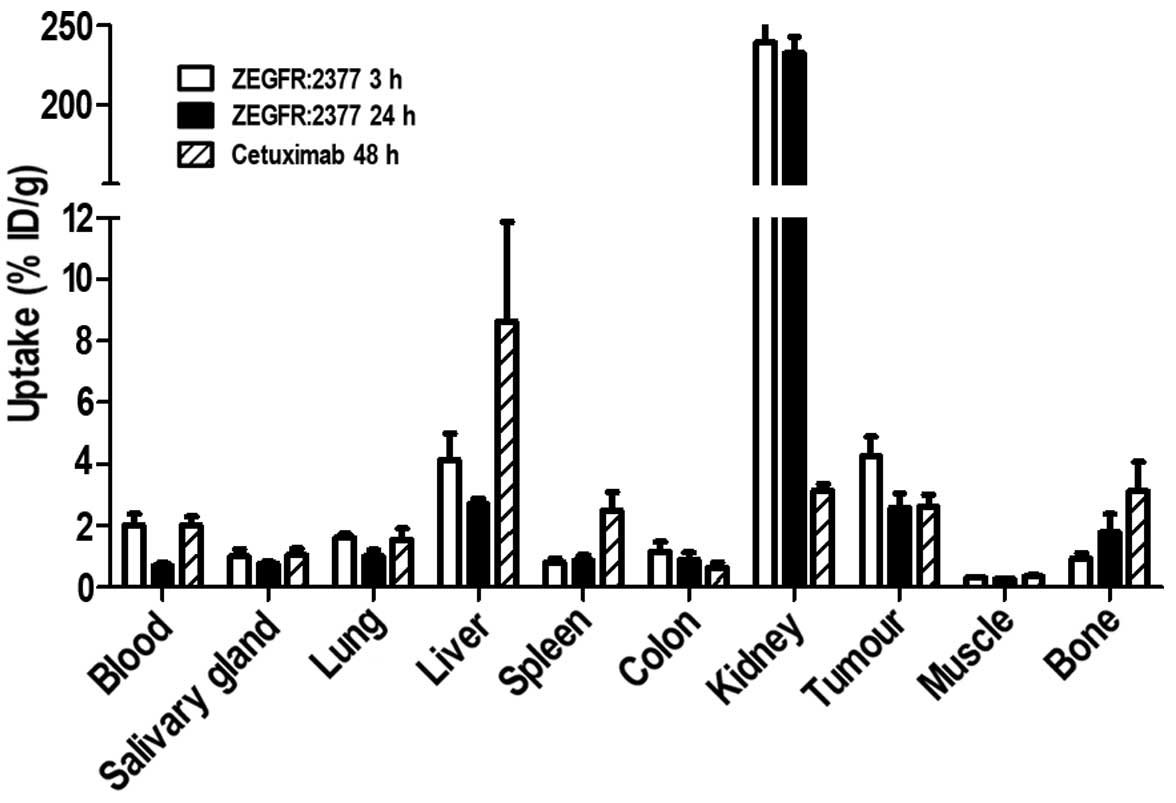
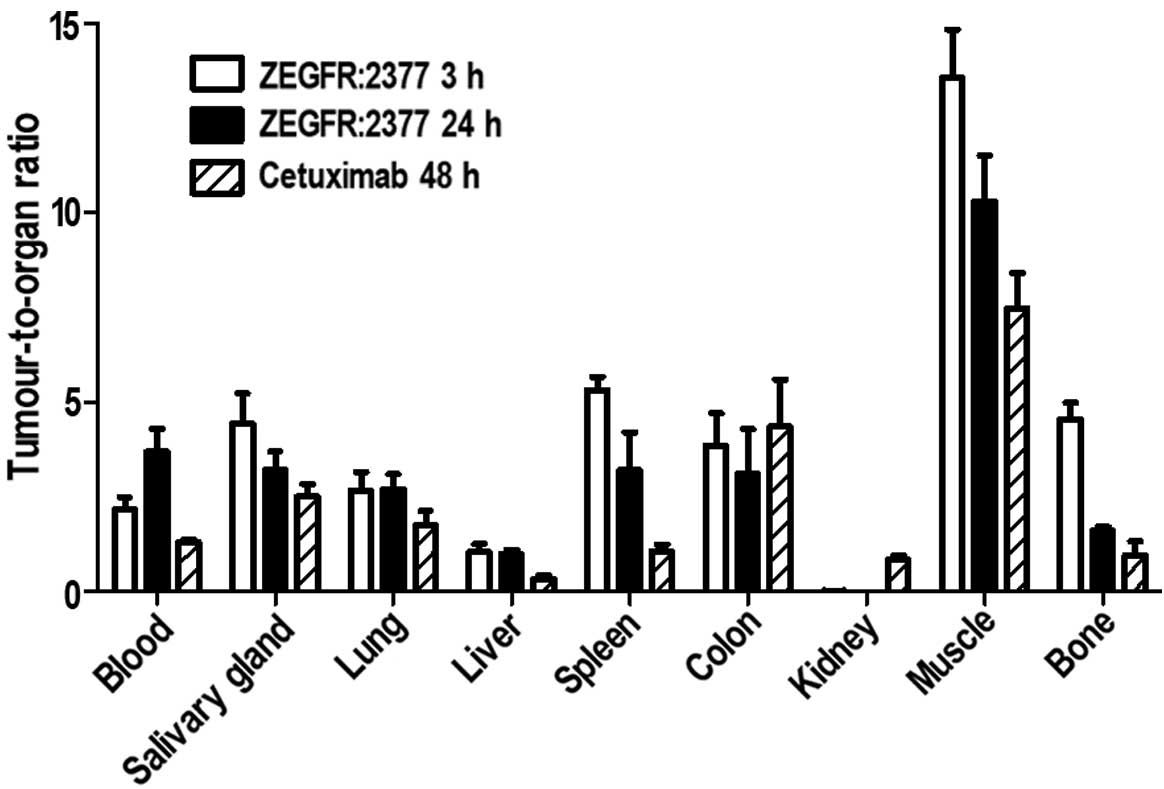
Comparison of 89Zr-DFO-ZEGFR:2377
biodistribution at 3 and 24 h and 89Zr-DFO-cetuximab
biodistribution in nude mice bearing EGFR-expressing xenografts is
presented in Fig. 4.
89Zr-DFO-ZEGFR:2377 demonstrated relatively rapid blood
clearance. Already at 3 h after injection, the blood concentration
was 2.0±0.4% ID/g. Low radioactivity uptake in gastrointestinal
tract (2.5±0.4% ID pre-whole sample, including content) suggested
that hepatobiliary exertion played a minor role in clearance of
89Zr-DFO-ZEGFR:2377. On the contrary, the high kidney
uptake suggested that 89Zr-DFO-ZEGFR:2377 underwent a
rapid glomerular filtration followed by renal re-absorption, which
is typical for affibody molecules. The tumour uptake (4.3±0.6%
ID/g) exceeded the uptake in other organs and tissues except for
liver (4.1±0.9% ID/g) and kidneys. At 24 h after injection, the
blood concentration of 89Zr-DFO-ZEGFR:2377 decreased
nearly 3-fold, from 2.0±0.3% ID/g to 0.70±0.07% ID/g. There was no
significant decrease of uptake in salivary gland, spleen, colon,
and kidney between 3 and 24 h after injection. There was
significant (P<0.05) decrease of 89Zr uptake in the
tumour, or in lung, liver and muscle. The 89Zr uptake in
bone increased at 24 h.
Biodistribution of 89Zr-DFO-cetuximab was
measured at 48 h after injection, i.e. an optimal time-point for
imaging using radiolabelled monoclonal antibodies. At this
time-point, the tumour uptake of 89Zr-DFO-cetuximab was
at the same level as uptake of 89Zr-DFO-ZEGFR:2377 at 24
h after injection. However, uptake of 89Zr-DFO-cetuximab
was significantly higher in blood, salivary gland, lung, liver,
spleen and muscles. The use of monoclonal antibody provided
significantly lower uptake in kidneys.
Tumour-to-organ ratios for 89Zr-labelled
tracers, which determine contrast and therefore sensitivity of
imaging, are presented in Fig. 5.
At both time-points, 89Zr-DFO-ZEGFR:2377 provided
significantly higher tumour-to-organ ratios than
89Zr-DFO-cetuximab except from the tumour-to-kidney
ratio and, at 4 h after injection, the tumour-to-salivary gland
ratio. At 24 h after injection, the tumour-to-blood ratio for
89Zr-DFO-ZEGFR:2377 (3.7±0.6) was 1.7-fold higher than
at 3 h after injection. At the same time, tumour-to-muscle ratio
was reduced 1.3-fold, tumour-to-bone ratio 2.8-fold and
tumour-to-spleen ratio 1.4-fold. There was no significant
difference in tumour-to-organ ratios for other tissues.
MicroPET imaging of EGFR expression in mice bearing
A431 xenografts using 89Zr-DFO-ZEGFR:2377 is presented
in Fig. 6. The images were in a
good agreement with the biodis-tribution data. The highest
concentration of radioactivity was in kidneys. Liver showed also a
prominent uptake of radioactivity. Tumours on right hind legs were
clearly visualized. The tumour uptake was at the same level as in
the liver (somewhat higher at 3 h after injection) and noticeably
higher than uptake in any other tissue. The image at 3 h provided
somewhat better contrast towards bones.
Discussion
PET as an imaging modality has traditionally been
associated with applications using radiolabelled small molecules as
imaging agents and protein-based imaging agents were typically
applied in SPECT imaging. However, the intrinsic advantages of PET,
such as higher sensitivity, better resolution and superior
quantification accuracy caused an increased interest in the
labelling of proteinaceous imaging probes with positron-emitting
nuclides and their use for PET imaging (42). The short-lived positron-emitting
nuclides, such as 18F (T1/2=109.8 min) or
68Ga (T1/2=67.6 min), are perfect labels for
small peptides providing high contrast already a few hours after
injection (42). These nuclides
have been successfully used for labelling of e.g. anti-HER2 and
anti-PDGFR affibody molecules (43–45).
However, anti-EGFR affibody molecules have unusually slow blood
clearance. This might be associated with their slow internalisation
after binding to EGFR in normal tissues (38). Clearance from blood causes
dissociation of the reversibly bound tracer from EGFR-expressing
tissues and its release back to blood circulation. Thus, the
tumour-to-blood ratio for 18F-labelled anti-EGFR
ZEGFR:1907 affibody molecules was around 2 within the time window
for this short-lived nuclide, although three different labelling
approaches were tested (46,47).
The low tumour-to-blood ratio translates into low overall contrast
and compromises sensitivity of imaging diagnostics. Previous
studies have shown that the tumour-to-blood ratio for
111In-DOTA-ZEGFR:2377 affibody molecule is significantly
higher at 24 than at 4 h after injection. However, next-day-imaging
requires a more long-lived positron-emitting label.
Radionuclide 89Zr seems suitable for
labelling of affibody molecules for PET imaging on the next day
after injection. This nuclide has been successfully used for
labelling of several antibodies for preclinical (25,26,48,49)
and clinical (50,51) PET imaging. Derivatives of
deferoxamine (DFO) chelator provide attachment of 89Zr
to targeting proteins under mild conditions (room temperature,
neutral pH) with adequate stability (52). 89Zr is currently
commercially available.
In this study, a maleimido derivative of DFO was
site-specifically conjugated to a unique cysteine at the C-terminus
of ZEGFR:2377 affibody molecules, providing a homogeneous
conjugate. DFO-ZEGFR:2377 was efficiently labelled with
89Zr. The conjugate was stable both in PBS and in murine
plasma during incubation up to 24 h (Table I). The
89Zr-DFO-ZEGFR:2377 affibody tracer demonstrated
specific binding to EGFR-expressing cells (Fig. 1) and high affinity (160±60 pM, as
measured by LigandTracer). The slow internalization of
89Zr-DFO-ZEGFR:2377 by A431 cells (Fig. 1) was consistent with earlier
findings for 111In-DOTA-ZEGFR:2377 (38). In vivo,
89Zr-DFO-ZEGFR:2377 bound specifically to
EGFR-expressing xenografts and EGFR-expressing murine organs at 3 h
after injection (Fig. 3).
Saturation of uptake in normal tissues resulted in lower release of
the conjugate back to circulation, which resulted in lower
concentration of radioactivity in blood and muscles (Fig. 3). In addition, non-bound
89Zr-DFO-ZEGFR:2377 was cleared from blood and
re-absorbed in the kidneys, which resulted in higher kidney uptake
after blocking (Fig. 3). The
increased uptake in the kidneys upon blocking suggests that the
renal uptake of 89Zr-DFO-ZEGFR:2377 is not
EGFR-mediated. Most likely, the renal re-absorptions of
89Zr-DFO-ZEGFR:2377 is mediated by one of the ‘scavenger
receptor’ systems that is responsible for recovery of proteins from
primary urine (53). Although the
high renal re-absorption is a common feature of affibody molecules
(34), its exact mechanism is
still not known. It has to be noted that the high renal uptake does
not prevent visualization of tumours in close vicinity of the
kidneys. For example, a HER2-expressing adrenal metastasis has been
clearly visualized by the anti-HER2 111In-ABY-025
affibody molecule during a clinical study (35), although the renal uptake of this
tracer was as high as the uptake of 89Zr-DFO-ZEGFR:2377
in preclinical studies (54).
At 24 h after injection, the uptake of
89Zr-DFO-ZEGFR:2377 in tumours and majority of tissues
was reduced compared to uptake at 3 h (Fig. 4). The only exception was bone,
where the uptake of 89Zr was higher at 24 h after
injection. This is consistent with the data for
89Zr-labelled antibodies, which also demonstrated
increase of the bone uptake at later time-points (48,52).
This might be an indication of release of the radionuclide from the
conjugate in vivo (52). As
89Zr-DFO-ZEGFR:2377 was stable in the blood plasma ex
vivo (Table I), we can suppose
that the release takes place during catabolism in excretory organs
and EGFR-expressing tissues. As the decrease of tumour uptake was
slower than blood clearance, the tumour-to-blood ratio
significantly (P<0.05) increased from 2.2±0.3 to 3.7±0.6,
leading to increased overall imaging contrast. The EGFR-expressing
xenografts were clearly visualized at both 3 and 24 h after
injection (Fig. 6).
For comparison, we investigated targeting of
EGFR-expressing xenografts using 89Zr-labelled anti-EGFR
antibody cetuximab. The biodistribution of
89Zr-DFO-cetuximab was measured at 48 h after injection
because the literature data (25)
suggest that this time-point is optimal for imaging of A431
xenografts, as there was neither significant increase of tumour
uptake nor decrease of blood concentration at later time-points.
Our data were in a good agreement with the data published by Aerts
and co-workers (25) as the
difference was within the measurement accuracy. At the optimal
time-point, the tumour uptake of 89Zr-DFO-cetuximab
(2.6±0.4% ID/g) was at the same level as uptake of
89Zr-DFO-ZEGFR:2377 at 24 h after injection (2.6±0.5%
ID/g) and was significantly lower than uptake at 3 h after
injection (4.3±0.6% ID/g). The normal organ uptake of
89Zr-DFO-cetuximab at 48 h was at the same level or
higher than uptake of 89Zr-DFO-ZEGFR:2377 at 3 h after
injection (Fig. 4). As a result,
89Zr-DFO-ZEGFR:2377 provided at both time-points
significantly higher tumour-to-organ ratios than
89Zr-DFO-cetuximab for all organs except from kidneys
(Fig. 5). Thus, PET imaging using
89Zr-DFO-ZEGFR:2377 should provide better contrast and,
therefore, sensitivity than using 89Zr-DFO-cetuximab.
The imaging could be performed earlier after injection, which is an
additional clinical advantage.
In conclusion, labelling of anti-EGFR ZEGFR:2377
affibody molecule with the long-lived positron emitting
radio-nuclide 89Zr provides a probe capable of specific
PET imaging of EGFR expression in malignant tumours.
89Zr-DFO-ZEGFR:2377 provides higher tumour-to-organ
ratios than the anti-EGFR antibody, cetuximab. This should ensure
higher sensitivity in clinical imaging.
Acknowledgements
The present study was financially supported by
grants from the Swedish Research Council (Vetenskapsrådet) and the
Swedish Cancer Society (Cancerfonden).
References
|
1
|
Mendelsohn J and Baselga J: Epidermal
growth factor receptor targeting in cancer. Semin Oncol.
33:369–385. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Scaltriti M and Baselga J: The epidermal
growth factor receptor pathway: A model for targeted therapy. Clin
Cancer Res. 12:5268–5272. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goffin JR and Zbuk K: Epidermal growth
factor receptor: Pathway, therapies, and pipeline. Clin Ther.
35:1282–1303. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ang KK, Andratschke NH and Milas L:
Epidermal growth factor receptor and response of head-and-neck
carcinoma to therapy. Int J Radiat Oncol Biol Phys. 58:959–965.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tsutsui S, Kataoka A, Ohno S, Murakami S,
Kinoshita J and Hachitanda Y: Prognostic and predictive value of
epidermal growth factor receptor in recurrent breast cancer. Clin
Cancer Res. 8:3454–3460. 2002.PubMed/NCBI
|
|
6
|
Selvaggi G, Novello S, Torri V, Leonardo
E, De Giuli P, Borasio P, Mossetti C, Ardissone F, Lausi P and
Scagliotti GV: Epidermal growth factor receptor overexpression
correlates with a poor prognosis in completely resected
non-small-cell lung cancer. Ann Oncol. 15:28–32. 2004. View Article : Google Scholar
|
|
7
|
Humbert O, Riedinger JM, Charon-Barra C,
Berriolo-Riedinger A, Desmoulins I, Lorgis V, Kanoun S, Coutant C,
Fumoleau P, Cochet A and Brunotte F: Identification of biomarkers
including 18FDG-PET/CT for early prediction of response
to neoadjuvant chemotherapy in triple negative breast cancer. Clin
Cancer Res. 21:5460–5468. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ang KK, Berkey BA, Tu X, Zhang HZ, Katz R,
Hammond EH, Fu KK and Milas L: Impact of epidermal growth factor
receptor expression on survival and pattern of relapse in patients
with advanced head and neck carcinoma. Cancer Res. 62:7350–7356.
2002.PubMed/NCBI
|
|
9
|
Cappuzzo F, Hirsch FR, Rossi E, Bartolini
S, Ceresoli GL, Bemis L, Haney J, Witta S, Danenberg K, Domenichini
I, et al: Epidermal growth factor receptor gene and protein and
gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer
Inst. 97:643–655. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hirsch FR, Varella-Garcia M, Bunn PA Jr,
Franklin WA, Dziadziuszko R, Thatcher N, Chang A, Parikh P, Pereira
JR, Ciuleanu T, et al: Molecular predictors of outcome with
gefitinib in a phase III placebo-controlled study in advanced
non-small-cell lung cancer. J Clin Oncol. 24:5034–5042. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pirker R, Pereira JR, von Pawel J,
Krzakowski M, Ramlau R, Park K, de Marinis F, Eberhardt WE,
Paz-Ares L, Störkel S, et al: EGFR expression as a predictor of
survival for first-line chemotherapy plus cetuximab in patients
with advanced non-small-cell lung cancer: Analysis of data from the
phase 3 FLEX study. Lancet Oncol. 13:33–42. 2012. View Article : Google Scholar
|
|
12
|
Bradley JD, Paulus R, Komaki R, Masters G,
Blumenschein G, Schild S, Bogart J, Hu C, Forster K, Magliocco A,
et al: Standard-dose versus high-dose conformal radiotherapy with
concurrent and consolidation carboplatin plus paclitaxel with or
without cetuximab for patients with stage IIIA or IIIB
non-small-cell lung cancer (RTOG 0617): A randomised, two-by-two
factorial phase 3 study. Lancet Oncol. 16:187–199. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bentzen SM, Atasoy BM, Daley FM, Dische S,
Richman PI, Saunders MI, Trott KR and Wilson GD: Epidermal growth
factor receptor expression in pretreatment biopsies from head and
neck squamous cell carcinoma as a predictive factor for a benefit
from accelerated radiation therapy in a randomized controlled
trial. J Clin Oncol. 23:5560–5567. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vignot S, Besse B, André F, Spano JP and
Soria JC: Discrepancies between primary tumor and metastasis: A
literature review on clinically established biomarkers. Crit Rev
Oncol Hematol. 84:301–313. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yarom N, Marginean C, Moyana T,
Gorn-Hondermann I, Birnboim HC, Marginean H, Auer RC, Vickers M,
Asmis TR, Maroun J, et al: EGFR expression variance in paired
colorectal cancer primary and metastatic tumors. Cancer Biol Ther.
10:416–421. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wei Q, Shui Y, Zheng S, Wester K, Nordgren
H, Nygren P, Glimelius B and Carlsson J: EGFR, HER2 and HER3
expression in primary colorectal carcinomas and corresponding
metastases: Implications for targeted radionuclide therapy. Oncol
Rep. 25:3–11. 2011.
|
|
17
|
Gomez-Roca C, Raynaud CM, Penault-Llorca
F, Mercier O, Commo F, Morat L, Sabatier L, Dartevelle P, Taranchon
E, Besse B, et al: Differential expression of biomarkers in primary
non-small cell lung cancer and metastatic sites. J Thorac Oncol.
4:1212–1220. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Italiano A, Vandenbos FB, Otto J, Mouroux
J, Fontaine D, Marcy PY, Cardot N, Thyss A and Pedeutour F:
Comparison of the epidermal growth factor receptor gene and protein
in primary non-small-cell-lung cancer and metastatic sites:
Implications for treatment with EGFR-inhibitors. Ann Oncol.
17:981–985. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Goldenberg A, Masui H, Divgi C, Kamrath H,
Pentlow K and Mendelsohn J: Imaging of human tumor xenografts with
an indium-111-labeled anti-epidermal growth factor receptor
monoclonal antibody. J Natl Cancer Inst. 81:1616–1625. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Divgi CR, Welt S, Kris M, Real FX, Yeh SD,
Gralla R, Merchant B, Schweighart S, Unger M, Larson SM, et al:
Phase I and imaging trial of indium 111-labeled anti-epidermal
growth factor receptor monoclonal antibody 225 in patients with
squamous cell lung carcinoma. J Natl Cancer Inst. 83:97–104. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cai W, Chen K, He L, Cao Q, Koong A and
Chen X: Quantitative PET of EGFR expression in xenograft-bearing
mice using 64Cu-labeled cetuximab, a chimeric anti-EGFR
monoclonal antibody. Eur J Nucl Med Mol Imaging. 34:850–858. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ping Li W, Meyer LA, Capretto DA, Sherman
CD and Anderson CJ: Receptor-binding, biodistribution, and
metabolism studies of 64Cu-DOTA-cetuximab, a PET-imaging
agent for epidermal growth-factor receptor-positive tumors. Cancer
Biother Radiopharm. 23:158–171. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nayak TK, Garmestani K, Baidoo KE, Milenic
DE and Brechbiel MW: Preparation, biological evaluation, and
pharmacokinetics of the human anti-HER1 monoclonal antibody
panitumumab labeled with 86Y for quantitative PET of
carcinoma. J Nucl Med. 51:942–950. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nayak TK, Garmestani K, Milenic DE and
Brechbiel MW: PET and MRI of metastatic peritoneal and pulmonary
colorectal cancer in mice with human epidermal growth factor
receptor 1-targeted 89Zr-labeled panitumumab. J Nucl
Med. 53:113–120. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Aerts HJ, Dubois L, Perk L, Vermaelen P,
van Dongen GA, Wouters BG and Lambin P: Disparity between in vivo
EGFR expression and 89Zr-labeled cetuximab uptake
assessed with PET. J Nucl Med. 50:123–131. 2009. View Article : Google Scholar
|
|
26
|
Chang AJ, De Silva RA and Lapi SE:
Development and characterization of 89Zr-labeled
panitumumab for immuno-positron emission tomographic imaging of the
epidermal growth factor receptor. Mol Imaging. 12:17–27.
2013.PubMed/NCBI
|
|
27
|
Cuartero-Plaza A, Martínez-Miralles E,
Rosell R, Vadell-Nadal C, Farré M and Real FX: Radiolocalization of
squamous lung carcinoma with 131I-labeled epidermal
growth factor. Clin Cancer Res. 2:13–20. 1996.PubMed/NCBI
|
|
28
|
Reilly RM, Kiarash R, Sandhu J, Lee YW,
Cameron RG, Hendler A, Vallis K and Gariépy J: A comparison of EGF
and MAb 528 labeled with 111In for imaging human breast
cancer. J Nucl Med. 41:903–911. 2000.PubMed/NCBI
|
|
29
|
Velikyan I, Sundberg AL, Lindhe O, Höglund
AU, Eriksson O, Werner E, Carlsson J, Bergström M, Långström B and
Tolmachev V: Preparation and evaluation of
68Ga-DOTA-hEGF for visualization of EGFR expression in
malignant tumors. J Nucl Med. 46:1881–1888. 2005.PubMed/NCBI
|
|
30
|
Li W, Niu G, Lang L, Guo N, Ma Y,
Kiesewetter DO, Backer JM, Shen B and Chen X: PET imaging of EGF
receptors using [18F] FBEM-EGF in a head and neck
squamous cell carcinoma model. Eur J Nucl Med Mol Imaging.
39:300–308. 2012. View Article : Google Scholar :
|
|
31
|
Löfblom J, Feldwisch J, Tolmachev V,
Carlsson J, Ståhl S and Frejd FY: Affibody molecules: Engineered
proteins for therapeutic, diagnostic and biotechnological
applications. FEBS Lett. 584:2670–2680. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nygren PA: Alternative binding proteins:
Affibody binding proteins developed from a small three-helix bundle
scaffold. FEBS J. 275:2668–2676. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ahlgren S and Tolmachev V: Radionuclide
molecular imaging using Affibody molecules. Curr Pharm Biotechnol.
11:581–589. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Feldwisch J and Tolmachev V: Engineering
of affibody molecules for therapy and diagnostics. Methods Mol
Biol. 899:103–126. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sörensen J, Sandberg D, Sandström M,
Wennborg A, Feldwisch J, Tolmachev V, Åström G, Lubberink M,
Garske-Román U, Carlsson J, et al: First-in-human molecular imaging
of HER2 expression in breast cancer metastases using the
111In-ABY-025 affibody molecule. J Nucl Med. 55:730–735.
2014. View Article : Google Scholar
|
|
36
|
Friedman M, Orlova A, Johansson E,
Eriksson TL, Höidén-Guthenberg I, Tolmachev V, Nilsson FY and Ståhl
S: Directed evolution to low nanomolar affinity of a
tumor-targeting epidermal growth factor receptor-binding affibody
molecule. J Mol Biol. 376:1388–1402. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tolmachev V, Friedman M, Sandström M,
Eriksson TL, Rosik D, Hodik M, Ståhl S, Frejd FY and Orlova A:
Affibody molecules for epidermal growth factor receptor targeting
in vivo: Aspects of dimerization and labeling chemistry. J Nucl
Med. 50:274–283. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Tolmachev V, Rosik D, Wållberg H, Sjöberg
A, Sandström M, Hansson M, Wennborg A and Orlova A: Imaging of EGFR
expression in murine xenografts using site-specifically labelled
anti-EGFR 111In-DOTA-ZEGFR:2377 Affibody
molecule: aspect of the injected tracer amount. Eur J Nucl Med Mol
Imaging. 37:613–622. 2010. View Article : Google Scholar
|
|
39
|
Vosjan MJ, Perk LR, Visser GW, Budde M,
Jurek P, Kiefer GE and van Dongen GA: Conjugation and radiolabeling
of monoclonal antibodies with zirconium-89 for PET imaging using
the bifunctional chelate p-isothiocyanatobenzyl-desferrioxamine.
Nat Protoc. 5:739–743. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Malmberg J, Tolmachev V and Orlova A:
Imaging agents for in vivo molecular profiling of disseminated
prostate cancer--targeting EGFR receptors in prostate cancer:
comparison of cellular processing of [111In]-labeled
affibody molecule ZEGFR:2377 and cetuximab. Int J Oncol.
38:1137–1143. 2011.PubMed/NCBI
|
|
41
|
Barta P, Malmberg J, Melicharova L,
Strandgård J, Orlova A, Tolmachev V, Laznicek M and Andersson K:
Protein interactions with HER-family receptors can have different
characteristics depending on the hosting cell line. Int J Oncol.
40:1677–1682. 2012.
|
|
42
|
Tolmachev V and Stone-Elander S:
Radiolabelled proteins for positron emission tomography: Pros and
cons of labelling methods. Biochim Biophys Acta. 1800.487–510.
2010.
|
|
43
|
Altai M, Strand J, Rosik D, Selvaraju RK,
Eriksson Karlström A, Orlova A and Tolmachev V: Influence of
nuclides and chelators on imaging using affibody molecules:
Comparative evaluation of recombinant affibody molecules
site-specifically labeled with 68Ga and 111In
via maleimido derivatives of DOTA and NODAGA. Bioconjug Chem.
24:1102–1109. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Heskamp S, Laverman P, Rosik D, Boschetti
F, van der Graaf WT, Oyen WJ, van Laarhoven HW, Tolmachev V and
Boerman OC: Imaging of human epidermal growth factor receptor type
2 expression with 18F-labeled affibody molecule
ZHER2:2395 in a mouse model for ovarian cancer. J Nucl
Med. 53:146–153. 2012. View Article : Google Scholar
|
|
45
|
Strand J, Varasteh Z, Eriksson O,
Abrahmsen L, Orlova A and Tolmachev V: Gallium-68-labeled affibody
molecule for PET imaging of PDGFRβ expression in vivo. Mol Pharm.
11(3): 957–3964. 2014. View Article : Google Scholar
|
|
46
|
Miao Z, Ren G, Liu H, Qi S, Wu S and Cheng
Z: PET of EGFR expression with an 18F-labeled affibody
molecule. J Nucl Med. 53:1110–1118. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Su X, Cheng K, Jeon J, Shen B, Venturin
GT, Hu X, Rao J, Chin FT, Wu H and Cheng Z: Comparison of two
site-specifically 18F-labeled affibodies for PET imaging
of EGFR positive tumors. Mol Pharm. 11:3947–3956. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Dijkers EC, Kosterink JG, Rademaker AP,
Perk LR, van Dongen GA, Bart J, de Jong JR, de Vries EG and Lub-de
Hooge MN: Development and characterization of clinical-grade
89Zr-trastuzumab for HER2/neu immunoPET imaging. J Nucl
Med. 50:974–981. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Terwisscha van Scheltinga AG, Lub-de Hooge
MN, Abiraj K, Schröder CP, Pot L, Bossenmaier B, Thomas M,
Hölzlwimmer G, Friess T, Kosterink JG, et al: ImmunoPET and
biodistribution with human epidermal growth factor receptor 3
targeting antibody 89Zr-RG7116. MAbs. 6:1051–1058. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Dijkers EC, Oude Munnink TH, Kosterink JG,
Brouwers AH, Jager PL, de Jong JR, van Dongen GA, Schröder CP,
Lub-de Hooge MN and de Vries EG: Biodistribution of
89Zr-trastuzumab and PET imaging of HER2-positive
lesions in patients with metastatic breast cancer. Clin Pharmacol
Ther. 87:586–592. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Oosting SF, Brouwers AH, van Es SC,
Nagengast WB, Oude Munnink TH, Lub-de Hooge MN, Hollema H, de Jong
JR, de Jong IJ, de Haas S, et al: 89Zr-bevacizumab PET
visualizes heterogeneous tracer accumulation in tumor lesions of
renal cell carcinoma patients and differential effects of
antiangiogenic treatment. J Nucl Med. 56:63–69. 2015. View Article : Google Scholar
|
|
52
|
Fischer G, Seibold U, Schirrmacher R,
Wängler B and Wängler C: 89Zr, a radiometal nuclide with
high potential for molecular imaging with PET: Chemistry,
applications and remaining challenges. Molecules. 18:6469–6490.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Vegt E, de Jong M, Wetzels JF, Masereeuw
R, Melis M, Oyen WJ, Gotthardt M and Boerman OC: Renal toxicity of
radiolabeled peptides and antibody fragments: Mechanisms, impact on
radionuclide therapy, and strategies for prevention. J Nucl Med.
51:1049–1058. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ahlgren S, Orlova A, Wållberg H, Hansson
M, Sandström M, Lewsley R, Wennborg A, Abrahmsén L, Tolmachev V and
Feldwisch J: Targeting of HER2-expressing tumors using
111In-ABY-025, a second-generation affibody molecule
with a fundamentally reengineered scaffold. J Nucl Med.
51:1131–1138. 2010. View Article : Google Scholar : PubMed/NCBI
|