Coronaviruses (CoVs) belong to the family
Coronaviridae, a member of the order Nidovirales and exist widely
in nature (1). Particles of CoVs
with a diameter of ~60-220 nm are spherical or oval in shape and
display pleomorphism (2,3). CoVs are enclosed by an envelope with
spikes and have an internal genome comprising single stranded
positive sense RNA (+ssRNA), while being named for their crown- or
corona-like viral particles under the electron microscope (2). SARS-CoV-2 has been identified as the
seventh coronavirus that is capable of infecting human beings and
the remaining six CoVs are HCoV-229E, HCoV-OC43, HCoV-NL63,
HCoV-HKU1, SARS-CoV and MERS-CoV (1,3-5).
Compared with other CoVs, SARS-CoV-2 possesses higher infectivity
and pathogenicity because some key sites within the receptor
binding domain of spike protein on the surface of SARS-CoV-2 are
different from other types of CoVs (3,6,7).
In February 2020, the World Health Organization termed
SARS-CoV-2-infected pneumonia COVID-19 (8). A great number of patients with
severe COVID-19 are either elderly individuals or complicated with
other basic diseases. Particularly, patients with malignant tumor
are vulnerable to the COVID-19 pandemic due to declined immune
function caused by tumor depletion, malnutrition and anti-tumor
therapy (9,10). As a result, declined immune
function could lead patients with cancer to be more susceptible to
COVID-19 and to have a higher chance of developing a severe and
critical illness with a poorer prognosis following COVID-19
infection. In addition, SARS-CoV-2 infection may elicit metabolic
reprogramming in tumor cells and affect cancer progression
(11). Notably,
SARS-CoV-2-induced immune response could counteract NK/T cell
lymphoma progression to a certain extent (12), suggesting that genetically
modified SARS-CoV-2 may exhibit potential oncolytic
characteristics. The present review examined the association of
SARS-CoV-2 with cancer, providing new ideas to protect patients
with cancer during the COVID-19 pandemic.
In most cases, virus multiplication in host cells
can block protein synthesis and DNA replica- tion of the cells,
leading to cell metabolism disorder, while massive replication of
virus causes damage to numerous cellular organelles (13,14). After the replication, large
numbers of progeny viruses are then released from the cells,
resulting in lytic cell death referred to as a destructive process
(14,15). Conversely, certain viruses known
as 'tumor viruses' do not cause the destruction of infected host
cells. Instead, tumor viruses can control the complex genome of
host cells, promoting unrestricted cell proliferation (13-15). Experiments on induction of chicken
sarcoma by Rous virus demonstrate that virus infection can
successfully induce tumor formation (16,17), showing that tumors can either
develop spontaneously in organisms or be formed by virus induction.
The above observation has laid a foundation for the following in
vitro tumor cell cultures and in vivo transfection in
mice. It has been shown that infection of Rous virus leads to the
occurrence of tumor cell traits in the cultured cells in
vitro, which include a loss of contact inhibition, continued
proliferation and anchoring independence (17). To date, several tumor viruses have
been identified, including human herpes virus 8 (HHV-8) (18-20), human papilloma virus (HPV)
(19,21-27), hepatitis B virus (HBV) (19,28-30), Epstein-Barr virus (EBV) (19,26,31-35), Cytomegalovirus (CMV) (19,27,36-38), human immunodeficiency virus (HIV)
(19,39-42), human T cell lymphotropic virus
(HTLV) (43,44) and hepatitis C virus (HCV)
(45-48) (Fig.
1).
Viruses have a very small genome in which most genes
encode proteins involved in virus replication, while only a very
small portion of the genes may be related to tumor cell
transformation (27). The
carcinogenic mechanism of tumor viruses has not yet been fully
elucidated, which may be related to the destruction of host cell
genetic stability, cell gene phenotype changes and virus
latency/reactivation. These mechanisms are not inde- pendent and
there are complex connections between them. Although different
tumor viruses encode different virus products, they can target some
of the same mechanisms, such as inhibiting tumor suppressor gene
expression, abnormally activating oncogenes to interfere with cell
growth and differentiation-related signals including NF-κB,
telomerase reverse transcriptase (TERT), tumor necrosis factor
receptor associated factors (TRAFs), PI3K-AKT-mTOR, β-catenin and
interferon signaling pathway, thereby affecting cell growth cycle
regulation and inducing malignant cell transformation (49-51). DNA viruses encode viral oncogenes
and RNA viruses can directly encode oncogenes or activate cell
oncogenes through cis- or trans activation. Centrifugation-based
measurement of the molecular mass of nucleic acids reveals that
viral nucleic acid sequences co-sediment with host nucleic acid
macromolecules, indicating that viral nucleic acids have become
integrated into host chromosomes, constituting the cellular genome
(52). It is noteworthy that
instead of the whole nucleic acid sequence of viruses, only a part
of the sequence with oncogenic role becomes integrated into the
cellular genome. In these cases, part of single-strand RNAs in the
genome of RNA viruses are reverse-transcribed into double-strand
DNAs that are subsequently integrated into host chromosomal DNAs.
These integrated viral double-strand DNAs are known as proviruses
(53).
The genome of organisms harbors a large number of
proto-oncogenes, such as Myc, c-Kit, Raf, Ret, H-ras and K-ras
(54-58). Among >30 proto-oncogenes
identified to date, most have derived their names from the
respective viruses in which they were originally discovered. Once
proto-oncogenes in the genome of organisms are captured and
activated by the respective viruses, malignant transformation of
cells will occur (59).
Retroviruses containing oncogenes can capture and activate
proto-oncogenes. By contrast, retroviruses without oncogenes
activate proto-oncogenes by inserting their own genomes adjacent to
those genes (insertion mutations) (60). It has been demonstrated that this
insertion is not random and the insertion sites of retrovirus
double-strand DNAs (proviruses) are closely adjoined to the
proto-oncogenes (60), suggesting
the presence of a mechanism underlying the recognition of
proto-oncogenes in retroviruses. Under this circumstance,
integrated transcriptional promoter of the viral genome causes a
damage to the regulatory mechanism of proto-oncogene expression,
enabling the expression of cellular genes under the control of the
viral promotor and eliciting a constitutive expression of
proto-oncogenes (61-63).
In addition to changes in proto-oncogenes and tumor
suppressor genes, the origin of tumors also includes the effects on
host cell gene stability and gene phenotype. Tumor viruses can
inhibit the expression of host tumor suppressor genes and interfere
with cell cycle regulation by affecting the form of DNA methylation
and histone modification (64,65). In addition, the virus has caused
damage to cells before entering the incubation period, resulting in
permanent genetic and epigenetic changes in the cells; the virus
entering the incubation period may reactivate and cause damage to
the cell (64, 65). The virus may experience
latency/reactivation cycle changes and the cells surviving
continuous damage continue to accumulate DNA damage during this
period and then a series of effects such as genetic instability,
cell immortalization and tumors occur (66).
The novel coronavirus SARS-CoV-2 belongs to the
β-coronaviruses genus, has an envelope, is 60-140 nm in diameter
and round or oval in shape (62).
SARS-CoV-2 virus is sensitive to ultraviolet and heat and can be
effectively inactivated by heating at 56°C for 30 min or treatment
with numerous lipid solvents including ether, 75% ethanol, chlorine
containing disinfectant, peracetic acid and chloroform. At present,
epidemiological investigation and research reveal that the
incubation period of SARS-CoV-2 lasts 1-14 days, generally 3-7 days
(67,68). Individuals infected with
SARS-CoV-2 are highly infectious 1-2 days before the onset and at
the early stage of the disease, while patients infected with
SARS-CoV-2 and asymptomatic infected persons are considered the
main source of infection (68).
Respiratory droplets and close contact transmission have been found
to be the main transmission routes. In addition, while contact with
virus contaminated items may lead to infection, there is the
possibility of aerosol transmission under the condition of
long-term exposure to high concentration of aerosol in a relatively
closed environment (69-71). Given that SARS-CoV-2 has been
isolated from feces and urine, attention should be paid to contact
or aerosol transmission caused by environmental pollution of feces
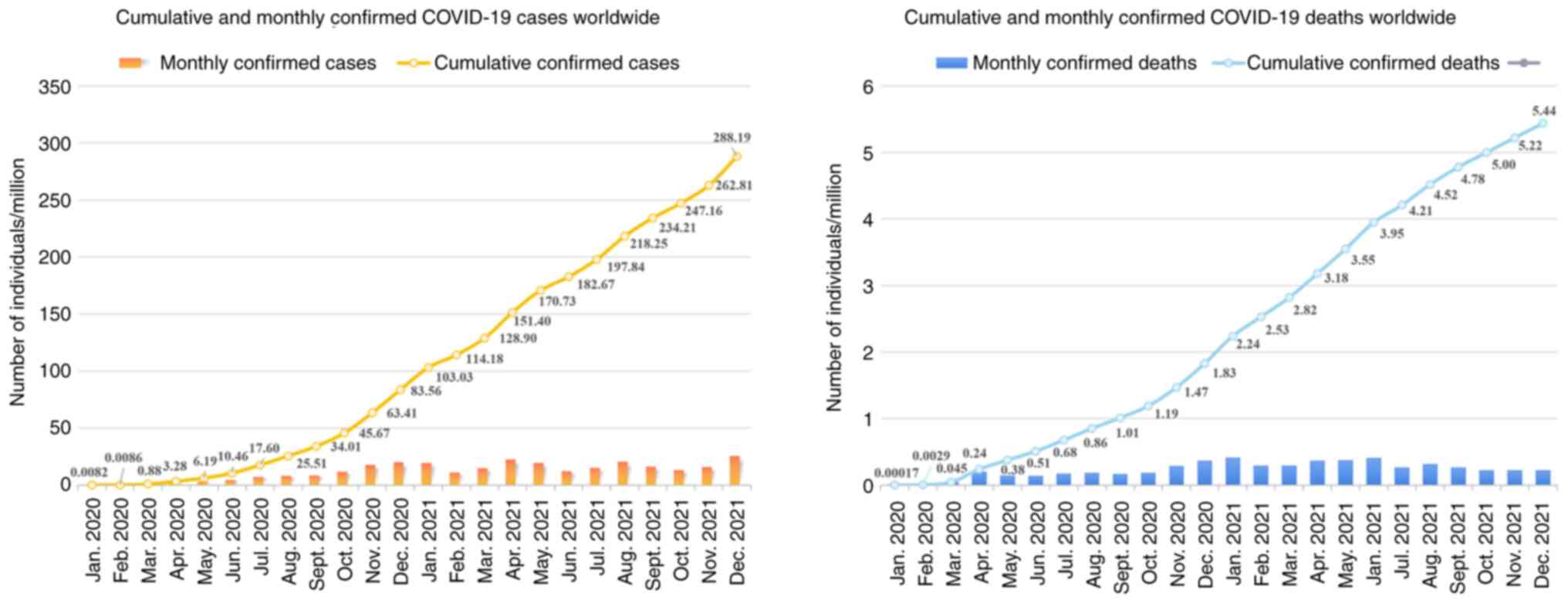
and urine. SARS-CoV-2 is highly infectious and the total number of
infected individuals is now >290 million (71,72). In the meantime, over 5.4 million
individuals have succumbed to SARS-CoV-2-caused COVID-19 worldwide
(Fig. 2). Similar to tumor
viruses, SARS-CoV-2 may accelerate tumor progression by altering
the metabolic pathways of tumor cells. It has been shown that
SARS-CoV-2 infection of human colon epithelial carcinoma cell line
Caco-2 remodels the central cell pathways, including translation,
splicing, carbon metabolism and nucleic acid metabolism, while
small molecule inhibitors targeting the aforementioned pathways are
capable of inhibiting the replication of SARS-CoV-2 in Caco-2 cells
(73). For example, nucleic acid
metabolism inhibitor Ribavirin can suppress the replication of
SARS-CoV-2 at a low molar concentration (73,74). In addition, the proteomics of
Caco-2 cells undergo an extensive regulation after 24 h of
SARS-CoV-2 infection, which mainly involves a decrease in
cholesterol rich metabolic proteins and an increase in carbohydrate
metabolism-modifying proteins during the infection (73). Studies imply that SARS-CoV-2 may
stimulate metabolism switch in tumor cells to initiate metabolic
modes with higher productivity efficiency, such as glycolysis, for
facilitating the massive replication of SARS-CoV-2 (75,76). In this case, inhibiting glycolysis
metabolism in tumor cells using 2-DG, a hexokinase inhibitor, can
significantly suppress the replication of SARS-CoV-2 in Caco-2
cells (73,75). This suggests that SARS-CoV-2
infection may elicit metabolic reprogramming in tumor cells,
thereby affecting cancer progression (Fig. 3).
The risk of developing a severe illness in patients
with COVID-19 complicated with malignancy is 3.61 times as high as
that in those without malignancy (77). Recently, epidemiological studies
of COVID-19 conducted in New York tertiary health cancer center
revealed that 56% of patients with COVID-19 are adults aged >60,
while the most common malignancies involved include numerous solid
tumors such as breast cancer, colorectal cancer and lung cancer
(78). Lymphoma is the most
prevalent hematopoietic malignancy and >50% the cases are
metastatic solid tumors (78,79). Among patients with cancer and
COVID-19, 59% had at least one of the designated complications,
including diabetes, hypertension, chronic kidney disease and heart
disease (77). Adjuvant
therapeutic drugs currently used in clinic include
hydroxychloroquine, azithromycin, redcivir, tosilizumab, recovery
plasma and corticosteroids (80-84). Patients with hematological cancer
and SARS-CoV-2 infection exhibit a higher rate of mortality
compared with patients infected with SARS-CoV-2 and with other
types of cancer, since malignant or dysfunctional plasma cells,
lymphocytes or white blood cells present in hematopoietic
malignancies (leukemia, myeloma and lymphoma) can reduce the immune
function of organisms (85).
Among all solid tumors, lung cancer has been shown
to be the most dangerous class of diseases to patients infected
with SARS-CoV-2 (85). For
patients with COVID-19 compli- cated with lung cancer, fever and
cough are the most obvious clinical symptoms, while the most
significant features of computerized tomography (CT) imaging
include ground glass shadow and patchy shadow (85). In addition, laboratory examination
reveals that patients with COVID-19 complicated with malignancy,
particularly those critical cases, clearly manifest cytokine storm,
immune system dysfunction and multiple organ/system damage
including a relatively prominent coagulation disorder (86). The risk factors for developing a
severe COVID-19 case include old age, IL-6, procalcitonin,
increased D-dimer, declined lymphocytes, cancer type, cancer
staging and cancer treatment (87-89). According to the data analysis of
7,094 Chinese patients with COVID-19 with an average age of 50, the
cancer prevalence in COVID-19 population is 2.3%, which is four
times higher compared with that in the entire Chinese population
(0.26%) and also three times higher compared with that in the
50-year-old Chinese population (0.39%) (90). This suggests that tumors are
closely associated with the risk of severe illness and death in
patients with COVID-19. Notably, no difference in the fatality rate
or severity of COVID-19 was observed between patients with cancer
at an early stage without tumor metastasis and non-cancer patients
(85). Conversely, patients with
advanced metastatic cancer are more likely to be infected with
SARS-CoV-2 (85).
It has also been reported that patients with cancer
and COVID-19 display a poor prognosis; this observation was more
evident in those with hematological malignancy and a higher risk of
death was found in male patients (91). Chemotherapy administered four
weeks before the onset of symptoms and being male are considered
the high-risk factors for COVID-19 infection in patients with
cancer. Among 182 patients with COVID-19 and a complete history of
tumor therapy, 31 underwent chemotherapy within 4 weeks prior to
being infected with COVID-19 (91). Markedly, the mortality risk of the
31 patients was 3.51 times as high as that of the remaining 151
patients. A relative low mortality was detected in patients with
COVID-19 with frequently occurring cancer in women, such as breast
cancer, thyroid carcinoma and cervical cancer (91). Conversely, the mortality risk of
male patients with cancer infected with COVID-19 was 3.86 times as
high as that of the female counterparts (91).
Given that patients with cancer and COVID-19 are
characterized by high mortality (92), it is recommended that these
patients continue to take anticancer drugs orally during the
COVID-19 pandemic. However, the antitumor therapy should be
undertaken carefully and reasonably, while postponing adjuvant
chemotherapy or selective operation needs to be considered on a
discretionary basis to avoid the aggravation of pneumonia symptoms
(93). In addition, it has been
shown that patients with COVID-19 and a history of cancer who are
undergoing an active treatment have a higher risk of developing a
severe event than those without cancer (94). It is noteworthy that during the
hospitalization, the mortality risk of those patients recently
undergoing antitumor therapy is 4 times as high as that of general
population (88). In addition,
targeted therapy or immunotherapy could lead to a 3.29-fold
increase in the risk of developing a severe and critical COVID-19
(88). Notably, among all
patients with COVID-19 and cancer receiving various therapies,
those undergoing immunotherapy displayed the highest mortality rate
as well as the most severe case (88). This increase can be attributed to
the enhancement in immune system-mediated attack against SARS-CoV-2
in the later stage of the virus infection, which aggravates the
lung damage and then elicits severe symptoms (Fig. 4) (95). In addition, pneumonia accounts for
42% of all death cases caused by the side effects of programmed
death-1 (PD-1) antibodies (96).
Similarly, either autologous and allogeneic hematopoietic stem cell
transplantation or chimeric antigen receptor T cell therapy may
lead patients with cancer to be highly susceptible to SARS-CoV-2
infection (88).
By contrast, it has also been demonstrated that
blockage of PD-1/PDL-1 pathway can inhibit acute or chronic viral
infection to a certain extent. An elderly patient infected with
SARS-CoV-2 took nivolumab for metastatic malignant melanoma in the
meantime. Surprisingly, considering her age, complications and
cancer diagnosis, her virus infection condition was well controlled
and no pneumonia was developed (97). This may be attributed to
nivolumab-induced blockage of PD-1/PDL-1 pathway and its anti-viral
effect. In addition, use of immune checkpoint inhibitors (ICIs) for
the cancer treatment is getting more and more prevalent. However,
ICI-caused recovery of immune function in patients with cancer may
lead to generation of potential lung toxicity, thus aggravating
COVID-19 and acute respiratory distress syndrome (ARDS) (98,99). Tocilizumab has been shown to be
successfully applied for treatment of the immune-related adverse
event (irAE), such as arthritis in patients undergoing ICI
treatment (100). As a
monoclonal antibody raised against IL-6 receptor, tocilizumab may
serve as a potential neutralizing antibody for COVID-19 treatment
(95,101,102). Thus, the study of ICI and
tocilizumab may provide some new thoughts for overcoming the side
effects of irAEs in patients with cancer and COVID-19. In addition,
the PD-1 block did not appear to affect the severity of COVID-19 in
lung patients with cancer after the risk factors for smoking were
excluded (103). Despite all
these observations, whether or not ICIs including PD-1 antibody
should be given to patients with cancer during SARS-CoV-2 infection
needs to be determined based on larger scale clinical analysis,
including the perspectives of immune function of patients, tumor
type, tumor stage, antiviral efficacy of drugs and so forth. For
patients who need to receive cancer treatments, assessment of the
immune function of patients based on immune deficiency score index,
strengthening nursing care of patients prior to the recovery of
immune function and early vaccination against respiratory
pathogens, such as seasonal influenza and streptococcus pneumoniae,
should be carried out (104).
During the COVID-19 pandemic, chemotherapy can only
be applied to patients with cancer unless immunosuppression, blood
toxicity, pneumonia/interstitial lung disease and other serious
risks caused by chemotherapy are reduced (94). For example, when chemotherapy
regimens with moderate/high risk of immunosuppression (e.g.
anthracyclines, docetaxel, cisplatin or carboplatin 3 times a week)
are administered to patients with triple-negative breast cancer, it
is recommended that the patients should be supplemented with
preventive hematopoietic growth factors to reduce the risk of
suffering from neutropenia (105). Application of steroids needs to
be strictly controlled to prevent an increased risk of
immunosuppression. During the pandemic, the oral preparation is
usually the first choice for adjuvant bisphosphonates. Low-dose
oral medication such as capecitabine and vinorelbine should be
considered preferentially in choosing the chemotherapy regimen for
avoiding hematological toxicity (94). In case intravenous injection is
considered unavoidable, preferential use of liposome preparation of
anthracyclines and prolonged dosing interval of intravenous
injection should be applied.
It has been suggested that during the COVID-19
outbreak, RT-hypo can be applied for the treatment of neck squamous
cell carcinoma (HNSCC) patients with a relatively lower risk of
distant metastasis (106). It is
proposed that RT-hypo be considered in place of concurrent
chemoradiotherapy for HPV+T1-T3N0-N2c (TNM-7) HNSCCs, HPV-T1-T2N0
HNSCCs and selected stage III HNSCCs during the outbreak (106). When shorter and fewer hospital
visits, as well as avoidance of immunosuppressive chemotherapy, are
needed to reduce the risk of SARS-CoV-2 infection, RT-hypo or short
fractionated radiotherapy may provide a more appropriate regimen
for patients with non-metastatic cancer. Therefore, it is necessary
to assess the risk of disease progression for those patients who do
not receive a timely and effective antitumor therapy. In this case,
a timely diagnosis and tumor treatment should be applied to those
patients with a rapidly progressed cancer such as lung cancer,
pancreatic cancer, leukemia and highly invasive lymphoma. By
contrast, targeted tumor therapy may be postponed for patients with
thyroid carcinoma, breast cancer, or other carcinoma at a
relatively low risk of disease progression. Particularly, for
hospitalized elder tumor patients with COVID-19 or patients
complicated with other basic diseases, early clinical monitoring
should be strengthened, while timely and effective tumor
intervention measurements need to be formulated. If possible,
priority should be given to minimally invasive surgery because
compared with open surgery, minimally invasive surgery can shorten
the duration of hospitalization and improve the recovery of
patients with cancer, thereby reducing the risk of SARS-CoV-2
infection in hospital (67).
Some evidence suggests that therapeutic drugs for
prostatic cancer may serve a synergistic role in treating COVID-19
(107). Inhibition of androgen
signaling is considered the symbolic therapeutic strategy of
prostatic cancer, while androgen inhibitors (e.g. leuprolide) and
androgen receptor (AR) signaling inhibitors (e.g. enzalutamide,
apalutamide and darolutamide) constitute the basis for the
treatment of prostate cancer (107). In particular, either inhibition
of AR expression and transcription or blockade of CYP17 using
abiraterone provide a new perspective for the treatment of
hormone-independent prostatic cancer (107). Transmembrane serine protease 2
(TMPRSS2) and angiotensin-converting enzyme 2 (ACE2) have been
identified as the key targets for enhanced entry of SARS-CoV-2 into
host cells (72,108,109). In addition, AR signaling has
been demonstrated to promote the expression of TMPRSS2 (107). Thus, inhibition of AR signaling
for treating prostatic cancer may suppress infection of SARS-CoV-2
in host cells by downregulating TMPRSS2, thereby preventing and
treating COVID-19 (Fig. 5).
However, preclinical studies have demonstrated that while
inhibition of AR decreases the expression of TMPRSS2, it may lead
to an upregulation in the expression of ACE2, increasing the risk
of SARS-CoV-2 infection (107).
Therefore, the potential negative outcome caused by inhibition of
AR needs to be further evaluated.
It has been reported that patients with various
cardiovascular diseases, diabetes or hypertension have an elevated
level of ACE2, while displaying a relatively high risk of dying
from COVID-19 (110). Notably,
the expression level of ACE2 in kidney is higher than that in other
organs; the level in kidney can be 100 times as high as that in
lung (110). Thus, studies on
shared molecular markers and overlapping signaling pathways between
renal cell carcinoma (RCC) and COVID-19 will be of great clinical
significance for the treatment of RCC patients complicated with
COVID-19. Administration with ACEIs can reduce the tumor growth and
metastatic potential, prolonging the survival period of patients
with RCC. In addition, ACE2 inhibition leads to decreased ACE2
available for binding with the viruses (111-113), probably reducing the
susceptibility of patients with RCC to SARS-CoV-2. Likewise,
inhibition of ACE2 in other types of malignancies can effectively
block the entry of SARS-CoV-2 into host cells. Cancer cells in
general express higher levels of ACE2 compared with their adjacent
normal cells and thus can be potentially more susceptible to
SARS-CoV-2 infection (3). Since
cancer cells have managed to evade host immune response in the
first place, this may provide a better microenvironment for
SARS-CoV-2 replication in cancer cells/tissues, which may partly
explain why patients with cancer seem to be more susceptible to
SARS-CoV-2 infection (87).
Although ACEI-caused decline in bradykinin degradation may
stimulate the growth, survival and migration of cancer cells, these
effects can be finally counteracted by decreased expression of
VEGFs due to ACEI-caused reduction in Ang II level and angiogenesis
(110).
It has been shown that the expression of tissue
factor in tumor cells can promote tumor growth and angiogenesis,
thereby resulting in release of coagulant particles into
circulation system, which subsequently trig- gers thromboembolism
in patients with cancer (114).
Given that concomitant infection with COVID-19 and hypoxia in
patients with cancer lead to a higher risk of developing a
thrombotic event, anticoagulant therapy could serve as one of
preventive and treatment strategies for patients with cancer and
infected with COVID-19 (115).
It is thought that early administration of heparin can defer the
dramatic increase of inflammatory biomarkers and downregulate
coagulation state. A retrospective study conducted in China
investigated 449 patients with severe COVID-19, among which 272
suffered from one or more chronic underlying diseases such as
hypertension and heart diseases. In that study, patients underwent
the treatment with various forms of heparin and a relatively lower
mortality rate was observed in patients treated with heparin (40%
vs. 64.2%, P=0.029) (116).
Similarly, statins with anti-inflammatory, anti-thrombotic and
immunomodulatory effects may reduce the risk of cardiovascular
complications and thromboembolic events in patients with COVID-19
(117). In addition, ACEI,
angiotensin receptor blockers, CCR5 treatment (118-120), tyrosine kinase inhibitors (TKIs)
(121-125), bevacizumab (126,127), ruxolitinib (126,128), carmofur (126,129) and toremi- fene (126,130) could potentially be used as
cancer therapy regimens aimed at counteracting COVID-19
mechanistically (Table I).
Notably, SARS-CoV-2 RNAs have been detected in the
feces of certain patients with COVID-19 (131). Thus, diversity of intestinal
flora and the presence of intestinal probiotics may serve an
important role in assessing the disease course of COVID-19
(132). Patients with cancer
usually display a compromised immune function as well as general
imbalance of intestinal flora, which are very likely to aggravate
the clinical manifestation of COVID-19 (132). Therefore, the recovery of
patients with cancer infected with SARS-CoV-2 could be promoted by
the administration of effective probiotics (e.g.,
fructooligosaccharide (FOS), galactooligosaccharides (GOS) and
various Lactobacillus strains), which are selected based on
analysis of intestinal flora in these patients. Alternatively,
patients with cancer can take special probiotics for improving
intestinal dystrophy, enhancing immunity and preventing against
SARS-CoV-2 infection. Studies on effects of SARS-CoV-2 on the
intestinal ecosystem in patients with cancer will provide new ideas
for preventing and controlling the viral infection of patients with
declined immunity such as patients with cancer.
Vitamin D is a fat-soluble vitamin that can be
obtained from the diet, the classic role of which is to promote
bone remodeling (133). Serum
levels of 25-hydroxyvitamin D [25 (OH) D] have been shown to be
negatively associated with a higher risk of colon, breast,
prostate, stomach and other cancers (134). Vitamin D deficiency has been
proved to contribute to the occurrence and progression of a number
of cancers, so maintaining adequate serum vitamin D levels may be
beneficial for cancer prevention and treatment (134). Recent studies have reported a
significant association between the average level of vitamin D and
the number of patients with COVID-19, especially the mortality rate
(133,135-137). Vitamin D deficiency is present
in >80% of patients with severe COVID-19 and is associated with
poor prognosis (133,136). Vitamin D deficiency may
contribute to the exacerbation of COVID-19 through inducing
thrombotic effects and immune dysregulation (136). In immune response, vitamin
D-dependent antimicrobial pathways are known to respond to
double-stranded RNA produced in replication processes of SARS-CoV-2
(136,138). These path- ways subsequently
upregulated the autophagy of damaged cells, as well as levels of
various antimicrobial and antiviral peptides (136,138). Thus, vitamin D deficiency may
predispose a host to SARS-CoV-2 infection by blocking the
activation of above defense pathways and the migration of
lymphocytes and macrophages (136). These findings suggest that
vitamin D may protect the body from acute respiratory infections,
while elderly patients with cancer and extreme vitamin D deficiency
may be more susceptible to COVID-19. In addition to vitamin D,
adequate levels of vitamin C and E are also essential to reduce the
burden of symptoms and shorten the duration of respiratory
infections during the COVID-19 pandemic (137). Micronutrients such as selenium
and zinc, the dietary supplements in multivitamin tablets, not only
serve important roles in cancer progression and therapy, but can
also increase the immune responses against viral infection
(138,139). It is speculated that selenium
and zinc may also have a potential inhibitory effect on COVID-19
infection (137,138). Thus, regular supplementation of
vitamin and other micronutrients may improve severe COVID-19
symptoms and survival in elderly patients with cancer. However, it
is worth noting that further research is needed to determine the
effective dose of vitamin and micronutrients supplements to help
patients with cancer alleviate the symptoms of COVID-19.
At present, there are differences in the COVID-19
vaccination policy for patients with cancer. In some countries, the
COVID-19 vaccine is not recommended for patients with malignant
tumors, or even as a contraindication for vaccination (140). The main reason is the lack of
clinical data on COVID-19 vaccine for patients with cancer, so the
safety status, effectiveness and immune response after vaccination
cannot be evaluated. However, recent reports show that even for
patients with cancer, if there are no contraindications to the
vaccine components, they may still receive COVID-19 vaccination and
get sufficiently high immunogenicity (141-143). Although patients with cancer may
have a delayed response to the vaccine, it may still bring some
benefits, which is important for reducing the risk or severity of
SARS-CoV-2 to patients with cancer (141,142). However, certain treatments for
cancer, such as chemotherapy or immunotherapy, can weaken the
immune system and may increase the risk of COVID-19 infection
(144). Therefore, patients with
early malignant tumors who have completed radical treatment and are
not receiving anti-tumor therapy, can be vaccinated with COVID-19
vaccine; for patients with malignant tumors who are receiving
chemotherapy, targeted therapy or immunotherapy, the vaccine should
be used with caution; for patients with malignant tumors who are
receiving endocrine therapy, the vaccine can be given to those in
good health, while is not recommended for patients in poor health,
whether or not they are receiving anti-tumor therapy (141,145). In the case of breast cancer,
inactivated vaccines are recommended during breast cancer
rehabilitation, including endocrine therapy and HER2 targeted
therapy; whereas for patients undergoing surgery, chemotherapy and
PD-1 treatment, it is recommended to wait for the sufficient
clinical evidence to prove the safety and effectiveness before
vaccination. For patients with cancer and impaired immune function,
it is recommended to vaccinate live attenuated vaccines and
recombinant subunit vaccines; and it is recommended to weigh the
benefit and the risk before vaccinating with adenovirus vector
vaccines (142). Notably, due to
the low immune function, the degree of immunity of patients with
cancer after vaccination is still uncertain. Patients with cancer
vaccinated should continue to follow current guidance to avoid
COVID-19 infection.
Oncolytic viruses are a class of natural or
genetically-modified viruses that are capable of self-replicating
and killing cancer cells (146).
After infecting cancer cells, oncolytic viruses will replicate
massively in the cells and promote the lytic cell death during the
replicative process (Fig. 6)
(146-149). At present, the latest clinical
regimen for combined therapy of oncolytic viruses involves a
combination with PD-1/PD-L1 antibodies, providing effective and
individualized tumor specific oncolytic immunotherapy to patients
with cancer who are resistant to PD-1/PD-L1 blockade therapy
(149,150). Notably, it has been shown that
oncolytic viruses can trigger antiviral response of the immune
system to increase the level of interferons in the tumor
environment, thereby promoting PD-L1 production for the immune
evasion (Fig. 7) (149).
It has been shown that ACE2 serves as a key target
for SARS-CoV-2 infection of host cells (3,110). As NK cells massively express
ACE2, they are easily infected by SARS-CoV-2, resulting in a
decline in cell numbers as well as loss of immune function
(151). Certain RNA viruses
causing acute pulmonary infection have been found to promote
apoptosis in NK cells (12).
Notably, elevated levels of IL-6 and IL-10 caused by SARS-CoV-2
infection lead to a marked decrease in the cytotoxicity of NK
cells, while SARS-CoV-2-induced release of IL-2 and TNF-α recruits
NK and T cells into the tumor tissue (12). Based on the above observations, it
is hypothesized that excessive production of proinflammatory
cytokines during COVID-19 infection may serve a pivotal role in
lymph node clearance. The depletion and inactivation of NK cells
could serve as a therapeutic regimen for NK lymphoma patients who
are resistant to conventional chemotherapy and improve the signs
and clinical symptoms of the patients with cancer. In addition, the
viral copy number of EBV-DNA, a sensitive biomarker of NK/T cell
lymphoma, has been shown to be markedly declined during the course
of COVID-19 (12). In addition,
serum copy number of EBV-DNA, cell number of NK cell clones and
recurrence rate of lymphoma in patients with NK lymphoma are
increased after the subsiding of SARS-CoV-2 infection (12), indicating that COVID-19 infection
can defer the tumor progression of NK lymphoma patients. The
binding between SARS-CoV-2 and the respective receptors such as
ACE2 in NK cells may determine its targeting of oncolytic
adenoviruses. All these observations suggest that while
SARS-CoV-2-induced immune response exerts an anti-tumor effect to a
certain extent, SARS-CoV-2 displays potential oncolytic
characteristics for lymphoma patients.
In addition, recent studies have suggested that
SARS-CoV-2 infection may protect against Hodgkin's lymphoma by
eliciting an anti-tumor immune response (149). Shortly after having been
diagnosed with advanced Hodgkin's lymphoma, a 61-year-old man with
severe kidney disease who was on long-term dialysis had been
confirmed with COVID-19 infection (149). After 11 days hospitalization, he
was discharged and returned home for rehabilitation. No
corticosteroids or immunochemotherapy was received during his
hospitalization and rehabilitation. However, four months after
being discharged from the hospital, CT reviews of the patient
demonstrated reduced palpable lymphadenopathy, interim PET/CT scans
displayed the extensive retrogression of lymphadenopathy and an
overall reduction of metabolic absorption and levels of
tumor-related biomarkers decreased by >90% (149,152). This medical report suggests that
possible mechanisms of oncolytic responses of SARS-CoV-2 may cover
cross reactions between pathogen-specific T-cells and tumor
antigens and the activation of natural killer cells through
inflammatory cytokines generated during response to the infection
of SARS-CoV-2. In addition, the majority of tumor patients suffer
from nephropathy, diabetes and other complications and oncolytic
virus therapy can partially offset the hepatorenal toxicity and
metabolic disorders caused by chemotherapy and immunosuppressive
agents. At present, studies provide evidence that combination
therapy with oncolytic vaccine and toxoid can help initiate
anti-tumor immune response of the immune system via CD4+ memory T
cells. Therefore, if oncolytic characteristics of SARS-CoV-2 could
be combined with the memory of T cells by genetic modification to
recall the immunity of known antigens to coronavirus, this scenario
may provide a new approach for the genetic modification of
oncolytic viruses.
SARS-CoV-2 may affect tumor progression through
multiple mechanisms, including glycolysis, translational
modification, nucleic acid synthesis, lipid metabolism and
transcriptional splicing. Patients with cancer complicated with
COVID-19 have a greater chance of developing a severe and critical
illness as well as a poorer prognosis. Given that
immunopotentiation therapies such as ICI and CAR-T used for tumor
treatment could aggravate inflammatory symptoms of patients with
COVID-19, targeted therapy or immunotherapy should be postponed
accordingly based on risk of disease progression. While either
chemotherapeutic drugs with low risk of immunosuppression or short
fractionated radiotherapy can be preferentially applied to
non-metastatic patients with cancer or those with cancer at early
stage; administration with high selective inhibitors targeting for
TMPRSS2 or ACE2 might be a feasible regimen for protecting advanced
patients with cancer against SARS-CoV-2 infection. In addition,
regular supplementation of vitamin and other micronutrients may
improve severe COVID-19 symptoms and survival in elderly patients
with cancer. The correlation of dynamic changes of COVID-19
antibody, nucleic acids, tumor metabolism pathway switch and levels
of tumor-related cytokines with the prognosis during the disease
course of patients with cancer is worthy of further study. Given
SARS-CoV-2-activated anti-tumor immune response and its toxic
inhibitory effect on NK cells, SARS-CoV-2 may possess potential
oncolytic characteristics in lymphoma patients. Therefore, genetic
modification of SARS-CoV-2 and in-depth studies of
immune-stimulating mechanism may provide more new directions for
oncolytic virotherapy.
Data sharing is not applicable to this article, as
no data sets were generated or analyzed during the current
study.
YSL conceived the study and wrote the manuscript.
HCR summarized and analyzed the data and produced graphs. JHC
contributed to the critical reading and correction of the manu-
script. Data authentication is not applicable. All authors have
read and approved the final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
Not applicable.
No funding was received.
|
1
|
Hartenian E, Nandakumar D, Lari A, Ly M,
Tucker JM and Glaunsinger BA: The molecular virology of
coronaviruses. J Biol Chem. 295:12910–12934. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mortaz E, Tabarsi P, Varahram M, Folkerts
G and Adcock IM: The immune response and immunopathology of
COVID-19. Front Immunol. 11:20372020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tan HW, Xu YM and Lau ATY:
Angiotensin-converting enzyme 2: The old door for new severe acute
respiratory syndrome coronavirus 2 infection. Rev Med Virol.
30:e21222020. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ye ZW, Yuan S, Yuen KS, Fung SY, Chan CP
and Jin DY: Zoonotic origins of human coronaviruses. Int J Biol
Sci. 16:1686–1697. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chang L, Yan Y and Wang L: Coronavirus
disease 2019: Coronaviruses and blood safety. Transfus Med Rev.
34:75–80. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yi C, Sun X, Ye J, Ding L, Liu M, Yang Z,
Lu X, Zhang Y, Ma L, Gu W, et al: Key residues of the receptor
binding motif in the spike protein of SARS-CoV-2 that interact with
ACE2 and neutralizing antibodies. Cell Mol Immunol. 17:621–630.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yuan M, Wu NC, Zhu X, Lee CD, So RTY, Lv
H, Mok CKP and Wilson IA: A highly conserved cryptic epitope in the
receptor binding domains of SARS-CoV-2 and SARS-CoV. Science.
368:630–633. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jiang S, Hillyer C and Du L: Neutralizing
antibodies against SARS-CoV-2 and other human coronaviruses. Trends
Immunol. 41:355–359. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
van Dam PA, Huizing M, Mestach G,
Dierckxsens S, Tjalma W, Trinh XB, Papadimitriou K, Altintas S,
Vermorken J, Vulsteke C, et al: SARS-CoV-2 and cancer: Are they
really part- ners in crime? Cancer Treat Rev. 89:1020682020.
View Article : Google Scholar
|
|
10
|
Garrone O, Denaro N, Ruatta F, Vanella P,
Granetto C, Vandone AM, Occelli M, Cauchi C, Ricci V, Fea E, et al:
Treating patients with cancer amidst the COVID-19 pandemic:
Experience of a regional hospital in the Piedmont region in
northern Italy. Tumori. 106:427–431. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bojkova D, Klann K, Koch B, Widera M,
Krause D, Ciesek S, Cinatl J and Münch C: Proteomics of
SARS-CoV-2-infected host cells reveals therapy targets. Nature.
583:469–472. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pasin F, Mascalchi Calveri M, Calabrese A,
Pizzarelli G, Bongiovanni I, Andreoli M, Cattaneo C and Rignanese
G: Oncolytic effect of SARS-CoV2 in a patient with NK lymphoma.
Acta Biomed. 91:e20200472020.
|
|
13
|
Akram N, Imran M, Noreen M, Ahmed F, Atif
M, Fatima Z and Bilal Waqar A: Oncogenic role of tumor viruses in
humans. Viral Immunol. 30:20–27. 2017. View Article : Google Scholar
|
|
14
|
White MK, Pagano JS and Khalili K: Viruses
and human cancers: A long road of discovery of molecular paradigms.
Clin Microbiol Rev. 27:463–481. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kuss-Duerkop SK, Westrich JA and Pyeon D:
DNA tumor virus regulation of host DNA methylation and its
implications for immune evasion and oncogenesis. Viruses.
10:822018. View Article : Google Scholar :
|
|
16
|
Liu S, Kaddis Maldonado R, Rye-McCurdy T,
Binkley C, Bah A, Chen EC, Rice BL, Parent LJ and Musier-Forsyth K:
Rous sarcoma virus genomic RNA dimerization capability in vitro is
not a prerequisite for viral infectivity. Viruses. 12:5682020.
View Article : Google Scholar :
|
|
17
|
Simatou A, Simatos G, Goulielmaki M,
Spandidos DA, Baliou S and Zoumpourlis V: Historical retrospective
of the SRC oncogene and new perspectives (review). Mol Clin Oncol.
13:212020.
|
|
18
|
Dupin N and Deleuze J: Kaposi sarcoma and
HHV-8: A model of cutaneous cancer in immunosuppressed patients.
Rev Prat. 64:311–316. 2014.In French. PubMed/NCBI
|
|
19
|
Stern J, Miller G, Li X and Saxena D:
Virome and bacteriome: Two sides of the same coin. Curr Opin Virol.
37:37–43. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Etta EM, Alayande DP, Mavhandu-Ramarumo
LG, Gachara G and Bessong PO: HHV-8 seroprevalence and genotype
distribution in Africa, 1998-2017: A systematic review. Viruses.
10:4582018. View Article : Google Scholar
|
|
21
|
Rusan M, Li YY and Hammerman PS: Genomic
landscape of human papillomavirus-associated cancers. Clin Cancer
Res. 21:2009–2019. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ojesina AI, Lichtenstein L, Freeman SS,
Pedamallu CS, Imaz-Rosshandler I, Pugh TJ, Cherniack AD, Ambrogio
L, Cibulskis K, Bertelsen B, et al: Landscape of genomic
alterations in cervical carcinomas. Nature. 506:371–375. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Parfenov M, Pedamallu CS, Gehlenborg N,
Freeman SS, Danilova L, Bristow CA, Lee S, Hadjipanayis AG, Ivanova
EV, Wilkerson MD, et al: Characterization of HPV and host genome
interactions in primary head and neck cancers. Proc Natl Acad Sci
USA. 111:15544–15549. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lei J, Ploner A, Elfström KM, Wang J, Roth
A, Fang F, Sundström K, Dillner J and Sparén P: HPV vaccination and
the risk of invasive cervical cancer. N Engl J Med. 383:1340–1348.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sadri Nahand J, Moghoofei M, Salmaninejad
A, Bahmanpour Z, Karimzadeh M, Nasiri M, Mirzaei HR, Pourhanifeh
MH, Bokharaei-Salim F, Mirzaei H and Hamblin MR: Pathogenic role of
exosomes and microRNAs in HPV-mediated inflammation and cervical
cancer: A review. Int J Cancer. 146:305–320. 2020. View Article : Google Scholar
|
|
26
|
Chen J, Kendrick S and Qin Z: Mechanistic
insights into chemoresistance mediated by oncogenic viruses in
lymphomas. Viruses. 11:11612019. View Article : Google Scholar
|
|
27
|
Paradowska E, Jabłońska A, Studzińska M,
Wilczyński M and Wilczyński JR: Detection and genotyping of CMV and
HPV in tumors and fallopian tubes from epithelial ovarian cancer
patients. Sci Rep. 9:199352019. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li A, Wu J, Zhai A, Qian J, Wang X, Qaria
MA, Zhang Q, Li Y, Fang Y, Kao W, et al: HBV triggers APOBEC2
expression through miR-122 regulation and affects the proliferation
of liver cancer cells. Int J Oncol. 55:1137–1148. 2019.PubMed/NCBI
|
|
29
|
Levrero M and Zucman-Rossi J: Mechanisms
of HBV-induced hepatocellular carcinoma. J Hepatol. 64(Suppl 1):
S84–S101. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zapatka M, Borozan I, Brewer DS, Iskar M,
Grundhoff A, Alawi M, Desai N, Sültmann H, Moch H, et al; PCAWG
Pathogens. The landscape of viral associations in human cancers.
Nat Genet. 52:320–330. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Peng RJ, Han BW, Cai QQ, Zuo XY, Xia T,
Chen JR, Feng LN, Lim JQ, Chen SW, Zeng MS, et al: Genomic and
transcriptomic landscapes of Epstein-Barr virus in extranodal
natural killer T-cell lymphoma. Leukemia. 33:1451–1462. 2019.
View Article : Google Scholar :
|
|
32
|
Re De V, Caggiari L, De Zorzi M, Fanotto
V, Miolo G, Puglisi F, Cannizzaro R, Canzonieri V, Steffan A,
Farruggia P, et al: Epstein-Barr virus BART microRNAs in
EBV-associated Hodgkin lymphoma and gastric cancer. Infect Agents
Cancer. 15:422020. View Article : Google Scholar
|
|
33
|
Camargo MC, Kim KM, Matsuo K, Torres J,
Liao LM, Morgan D, Michel A, Waterboer T, Song M, Gulley ML, et al:
Circulating antibodies against Epstein-Barr virus (EBV) and p53 in
EBV-positive and -negative gastric cancer. Cancer Epidemiol
Biomarkers Prev. 29:414–419. 2020. View Article : Google Scholar
|
|
34
|
Fitzsimmons L, Cartlidge R, Chang C, Sejic
N, Galbraith LCA, Suraweera CD, Croom-Carter D, Dewson G, Tierney
RJ, Bell AI, et al: EBV BCL-2 homologue BHRF1 drives
chemo-resistance and lymphomagenesis by inhibiting multiple
cellular pro-apoptotic proteins. Cell Death Differ. 27:1554–1568.
2020. View Article : Google Scholar
|
|
35
|
Fukayama M, Abe H, Kunita A,
Shinozaki-Ushiku A, Matsusaka K, Ushiku T and Kaneda A: Thirty
years of Epstein-Barr virus-associated gastric carcinoma. Virchows
Arch. 476:353–365. 2020. View Article : Google Scholar
|
|
36
|
Rahman M, Dastmalchi F, Karachi A and
Mitchell D: The role of CMV in glioblastoma and implications for
immunotherapeutic strategies. Oncoimmunology. 8:e15149212018.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chang Z, Wang Y, Zhou X and Long JE: STAT3
roles in viral infection: Antiviral or proviral? Future Virol.
13:557–574. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wilski NA and Snyder CM: From vaccine
vector to oncomodulation: Understanding the complex interplay
between CMV and cancer. Vaccines (Basel). 7:622019. View Article : Google Scholar
|
|
39
|
Bayurova E, Jansons J, Skrastina D,
Smirnova O, Mezale D, Kostyusheva A, Kostyushev D, Petkov S,
Podschwadt P, Valuev-Elliston V, et al: HIV-1 reverse transcriptase
promotes tumor growth and metastasis formation via ROS-dependent
upregulation of twist. Oxid Med Cell Longev. 2019:60162782019.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Purushothaman P, Uppal T, Sarkar R and
Verma SC: KSHV-mediated angiogenesis in tumor progression. Viruses.
8:1982016. View Article : Google Scholar :
|
|
41
|
Dupin N: Update on oncogenesis and therapy
for Kaposi sarcoma. Curr Opin Oncol. 32:122–128. 2020. View Article : Google Scholar
|
|
42
|
Markazi A, Bracci PM, McGrath M and Gao
SJ: Pseudomonas aeruginosa stimulates inflammation and enhances
Kaposi's sarcoma herpesvirus-induced cell proliferation and
cellular transformation through both lipopolysaccharide and
flagellin. mBio. 11:e02843–20. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yasunaga JI: Strategies of human T-cell
leukemia virus type 1 for persistent infection: Implications for
leukemogenesis of adult T-cell leukemia-lymphoma. Front Microbiol.
11:9792020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Higuchi Y, Yasunaga JI, Mitagami Y,
Tsukamoto H, Nakashima K, Ohshima K and Matsuoka M: HTLV-1 induces
T cell malignancy and inflammation by viral antisense
factor-mediated modulation of the cytokine signaling. Proc Natl
Acad Sci USA. 117:13740–13749. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Benkheil M, Paeshuyse J, Neyts J, Van
Haele M, Roskams T and Liekens S: HCV-induced EGFR-ERK signaling
promotes a pro-inflammatory and pro-angiogenic signature
contributing to liver cancer pathogenesis. Biochem Pharmacol.
155:305–315. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
El-Bendary M, Nour D, Arafa M and
Neamatallah M: Methylation of tumour suppressor genes RUNX3,
RASSF1A and E-Cadherin in HCV-related liver cirrhosis and
hepatocellular carcinoma. Br J Biomed Sci. 77:35–40. 2020.
View Article : Google Scholar
|
|
47
|
Huang P, Wang CH, Zhuo LY, Xia XS, Yang S,
Zhang JW, Fan HZ, Wu JJ, Yu R, Yue M and Zhang Y: Polymorphisms
rs763110 in FASL is linked to hepatitis C virus infection among
high-risk populations. Br J Biomed Sci. 77:112–117. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Defrancesco I, Zerbi C, Rattotti S, Merli
M, Bruno R, Paulli M and Arcaini L: HCV infection and non-Hodgkin
lymphomas: An evolving story. Clin Exp Med. 20:321–328. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Elgui de Oliveira D: DNA viruses in human
cancer: An integrated overview on fundamental mechanisms of viral
carcinogenesis. Cancer Lett. 247:182–196. 2007. View Article : Google Scholar
|
|
50
|
Fujimuro M, Wu FY, ApRhys C, Kajumbula H,
Young DB, Hayward GS and Hayward SD: A novel viral mechanism for
dysregulation of beta-catenin in Kaposi's sarcoma-associated
herpesvirus latency. Nat Med. 9:300–306. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Buchkovich NJ, Yu Y, Zampieri CA and
Alwine JC: The TORrid affairs of viruses: Effects of mammalian DNA
viruses on the PI3K-Akt-mTOR signalling pathway. Nat Rev Microbiol.
6:266–275. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Gaglia MM and Munger K: More than just
oncogenes: Mechanisms of tumorigenesis by human viruses. Curr Opin
Virol. 32:48–59. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Imamichi H, Smith M, Adelsberger JW, Izumi
T, Scrimieri F, Sherman BT, Rehm CA, Imamichi T, Pau A, Catalfamo
M, et al: Defective HIV-1 proviruses produce viral proteins. Proc
Natl Acad Sci USA. 117:3704–3710. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Takahashi M, Kawai K and Asai N: Roles of
the RET proto- oncogene in cancer and development. JMA J.
3:175–181. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Wang H, Boussouar A, Mazelin L,
Tauszig-Delamasure S, Sun Y, Goldschneider D, Paradisi A and Mehlen
P: The proto-oncogene c-Kit inhibits tumor growth by behaving as a
dependence receptor. Mol Cell. 72:413–425.e5. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chen S, Li F, Xu D, Hou K, Fang W and Li
Y: The function of RAS mutation in cancer and advances in its drug
research. Curr Pharm Des. 25:1105–1114. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Terrell EM, Durrant DE, Ritt DA, Sealover
NE, Sheffels E, Spencer-Smith R, Esposito D, Zhou Y, Hancock JF,
Kortum RL and Morrison DK: Distinct binding preferences between Ras
and Raf family members and the impact on oncogenic Ras signaling.
Mol Cell. 76:872–884.e5. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang Y, Wu D and Wang D: Long non-coding
RNA ARAP1-AS1 promotes tumorigenesis and metastasis through
facilitating proto-oncogene c-Myc translation via dissociating
PSF/PTB dimer in cervical cancer. Cancer Med. 9:1855–1866. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Trigo J, Subbiah V, Besse B, Moreno V,
López R, Sala MA, Peters S, Ponce S, Fernández C, Alfaro V, et al:
Lurbinectedin as second-line treatment for patients with small-cell
lung cancer: A single-arm, open-label, phase 2 basket trial. Lancet
Oncol. 21:645–654. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Adoue V and Joffre O: Endogenous
retroviruses: Friend or foe of the immune system? Med Sci (Paris).
36:253–260. 2020.In French. View Article : Google Scholar
|
|
61
|
Giannuzzi D and Aresu L: A first NGS
investigation suggests no association between viruses and canine
cancers. Front Vet Sci. 7:3652020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
He J, Tao H, Yan Y, Huang SY and Xiao Y:
Molecular mechanism of evolution and human infection with
SARS-CoV-2. Viruses. 12:4282020. View Article : Google Scholar :
|
|
63
|
Wang IH, Burckhardt CJ, Yakimovich A and
Greber UF: Imaging, tracking and computational analyses of virus
entry and egress with the cytoskeleton. Viruses. 10:1662018.
View Article : Google Scholar :
|
|
64
|
McLaughlin-Drubin ME, Crum CP and Münger
K: Human papillomavirus E7 oncoprotein induces KDM6A and KDM6B
histone demethylase expression and causes epigenetic reprogramming.
Proc Natl Acad Sci USA. 108:2130–2135. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Burgers WA, Blanchon L, Pradhan S, de
Launoit Y, Kouzarides T and Fuks F: Viral oncoproteins target the
DNA methyltransferases. Oncogene. 26:1650–1655. 2007. View Article : Google Scholar
|
|
66
|
Avanzi S, Alvisi G and Ripalti A: How
virus persistence can initiate the tumorigenesis process. World J
Virol. 2:102–109. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Addeo A and Friedlaender A: Cancer and
COVID-19: Unmasking their ties. Cancer Treat Rev. 88:1020412020.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng
Q, Meredith HR, Azman AS, Reich NG and Lessler J: The incubation
period of coronavirus disease 2019 (COVID-19) from publicly
reported confirmed cases: Estimation and application. Ann Intern
Med. 172:577–582. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Tang S, Mao Y, Jones RM, Tan Q, Ji JS, Li
N, Shen J, Lv Y, Pan L, Ding P, et al: Aerosol transmission of
SARS-CoV-2? Evidence, prevention and control. Environ Int.
144:1060392020. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
van Doremalen N, Bushmaker T, Morris DH,
Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL,
Thornburg NJ, Gerber SI, et al: Aerosol and surface stability of
SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med.
382:1564–1567. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Smither SJ, Eastaugh LS, Findlay JS and
Lever MS: Experimental aerosol survival of SARS-CoV-2 in artificial
saliva and tissue culture media at medium and high humidity. Emerg
Microbes Infect. 9:1415–1417. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bouhaddou M, Memon D, Meyer B, White KM,
Rezelj VV, Correa Marrero M, Polacco BJ, Melnyk JE, Ulferts S,
Kaake RM, et al: The global phosphorylation landscape of SARS-CoV-2
infection. Cell. 182:685–712.e19. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Kim JM, Kim HM, Lee EJ, Jo HJ, Yoon Y, Lee
NJ, Son J, Lee YJ, Kim MS, Lee YP, et al: Detection and isolation
of SARS-CoV-2 in serum, urine, and stool specimens of COVID-19
patients from the Republic of Korea. Osong Public Health Res
Perspect. 11:112–117. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Elfiky AA: Ribavirin, remdesivir,
sofosbuvir, galidesivir, and tenofovir against SARS-CoV-2 RNA
dependent RNA polymerase (RdRp): A molecular docking study. Life
Sci. 253:1175922020. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Icard P, Lincet H, Wu Z, Coquerel A,
Forgez P, Alifano M and Fournel L: The key role of Warburg effect
in SARS-CoV-2 replication and associated inflammatory response.
Biochimie. 180:169–177. 2021. View Article : Google Scholar
|
|
76
|
Codo AC, Davanzo GG, Monteiro LB, de Souza
GF, Muraro SP, Virgilio-da-Silva JV, Prodonoff JS, Carregari VC, de
Biagi Junior CAO, Crunfli F, et al: Elevated glucose levels favor
SARS-CoV-2 infection and monocyte response through a
HIF-1α/glycolysis-dependent axis. Cell Metab. 32:498–499. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Raymond E, Thieblemont C, Alran S and
Faivre S: Impact of the COVID-19 outbreak on the management of
patients with cancer. Target Oncol. 15:249–259. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Robilotti EV, Babady NE, Mead PA, Rolling
T, Perez-Johnston R, Bernardes M, Bogler Y, Caldararo M, Figueroa
CJ, Glickman MS, et al: Determinants of COVID-19 disease severity
in patients with cancer. Nat Med. 26:1218–1223. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lewis WD, Lilly S and Jones KL: Lymphoma:
Diagnosis and treatment. Am Fam Physician. 101:34–41.
2020.PubMed/NCBI
|
|
80
|
Arshad S, Kilgore P, Chaudhry ZS, Jacobsen
G, Wang DD, Huitsing K, Brar I, Alangaden GJ, Ramesh MS, McKinnon
JE, et al: Treatment with hydroxychloroquine, azithromycin, and
combination in patients hospitalized with COVID-19. Int J Infect
Dis. 97:396–403. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Johnson KM, Belfer JJ, Peterson GR,
Boelkins MR and Dumkow LE: Managing COVID-19 in renal transplant
recipients: A review of recent literature and case supporting
corticosteroid- sparing immunosuppression. Pharmacotherapy.
40:517–524. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Singh AK, Majumdar S, Singh R and Misra A:
Role of corticosteroid in the management of COVID-19: A systemic
review and a Clinician's perspective. Diabetes Metab Syndr.
14:971–978. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Luo P, Liu Y, Qiu L, Liu X, Liu D and Li
J: Tocilizumab treatment in COVID-19: A single center experience. J
Med Virol. 92:814–818. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Wooding DJ and Bach H: Treatment of
COVID-19 with convalescent plasma: Lessons from past coronavirus
outbreaks. Clin Microbiol Infect. 26:1436–1446. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z,
Zhang Z, You H, Wu M, Zheng Q, et al: Patients with cancer appear
more vulnerable to SARS-CoV-2: A multicenter study during the
COVID-19 outbreak. Cancer Discov. 10:783–791. 2020.PubMed/NCBI
|
|
86
|
Li D, Liu C, Liu J, Hu J, Yang Y and Zhou
Y: Analysis of risk factors for 24 patients with COVID-19
developing from moderate to severe condition. Front Cell Infect
Microbiol. 10:5485822020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y,
Shi J, Zhou M, Wu B, Yang Z, et al: Risk factors for severity and
mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin
Immunol. 146:110–118. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Turnquist C, Ryan BM, Horikawa I, Harris
BT and Harris CC: Cytokine storms in cancer and COVID-19. Cancer
Cell. 38:598–601. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Gosain R, Abdou Y, Singh A, Rana N,
Puzanov I and Ernstoff MS: COVID-19 and cancer: A comprehensive
review. Curr Oncol Rep. 22:532020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Tian Y, Qiu X, Wang C, Zhao J, Jiang X,
Niu W, Huang J and Zhang F: Cancer associates with risk and severe
events of COVID-19: A systematic review and meta-analysis. Int J
Cancer. 148:363–374. 2021. View Article : Google Scholar
|
|
91
|
Yang K, Sheng Y, Huang C, Jin Y, Xiong N,
Jiang K, Lu H, Liu J, Yang J, Dong Y, et al: Clinical
characteristics, outcomes, and risk factors for mortality in
patients with cancer and COVID-19 in Hubei, China: A multicentre,
retrospective, cohort study. Lancet Oncol. 21:904–913. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Pinato DJ, Zambelli A, Aguilar-Company J,
Bower M, Sng C, Salazar R, Bertuzzi A, Brunet J, Mesia R, Segui E,
et al: Clinical portrait of the SARS-CoV-2 epidemic in European
cancer patients. Cancer Discov. 10:1465–1474. Jul 31–2020.Epub
ahead of print. View Article : Google Scholar :
|
|
93
|
Jindal V, Sahu KK, Gaikazian S, Siddiqui
AD and Jaiyesimi I: Cancer treatment during COVID-19 pandemic. Med
Oncol. 37:582020. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Moris D, Tsilimigras DI and Schizas D:
Cancer and COVID-19. Lancet. 396:10662020. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Arnaldez FI, O'Day SJ, Drake CG, Fox BA,
Fu B, Urba WJ, Montesarchio V, Weber JS, Wei H, Wigginton JM and
Ascierto PA: The society for immunotherapy of cancer perspective on
regulation of interleukin-6 signaling in COVID-19-related systemic
inflammatory response. J Immunother Cancer. 8:e0009302020.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zhang C, Rong HM, Li T, Zhai K and Tong
ZH: PD-1 deficiency promotes macrophage activation and T-helper
cell type 1/T-helper cell type 17 response in pneumocystis
pneumonia. Am J Respir Cell Mol Biol. 62:767–782. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Yekedüz E, Dursun B, Aydın GÇ, Yazgan SC,
Öztürk HH, Azap A, Utkan G and Ürün Y: Clinical course of COVID-19
infection in elderly patient with melanoma on nivolumab. J Oncol
Pharm Pract. 26:1289–1294. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Dumoulin DW, Gietema HA, Paats MS,
Hendriks LEL and Cornelissen R: Differentiation of COVID-19
pneumonitis and ICI induced pneumonitis. Front Oncol.
10:5776962020. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Sullivan RJ, Johnson DB, Rini BI, Neilan
TG, Lovly CM, Moslehi JJ and Reynolds KL: COVID-19 and immune
checkpoint inhibitors: Initial considerations. J Immunother Cancer.
8:e0009332020. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Presti M, Westergaard MCW, Draghi A,
Chamberlain CA, Gokuldass A, Svane IM and Donia M: The effects of
targeted immune-regulatory strategies on tumor-specific T-cell
responses in vitro. Cancer Immunol Immunother. 70:1771–1776. 2021.
View Article : Google Scholar
|
|
101
|
Klopfenstein T, Zayet S, Lohse A, Balblanc
JC, Badie J, Royer PY, Toko L, Mezher C, Kadiane-Oussou NJ, Bossert
M, et al: Tocilizumab therapy reduced intensive care unit
admissions and/or mortality in COVID-19 patients. Med Mal Infect.
50:397–400. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Toniati P, Piva S, Cattalini M, Garrafa E,
Regola F, Castelli F, Franceschini F, Airò P, Bazzani C, Beindorf
EA, et al: Tocilizumab for the treatment of severe COVID-19
pneumonia with hyperinflammatory syndrome and acute respiratory
failure: A single center study of 100 patients in Brescia, Italy.
Autoimmun Rev. 19:1025682020. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Luo J, Rizvi H, Egger JV, Preeshagul IR,
Wolchok JD and Hellmann MD: Impact of PD-1 blockade on severity of
COVID-19 in patients with lung cancers. Cancer Discov.
10:1121–1128. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Weinkove R, McQuilten ZK, Adler J, Agar
MR, Blyth E, Cheng AC, Conyers R, Haeusler GM, Hardie C, Jackson C,
et al: Managing haematology and oncology patients during the
COVID-19 pandemic: Interim consensus guidance. Med J Aust.
212:481–489. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Curigliano G, Cardoso MJ, Poortmans P,
Gentilini O, Pravettoni G, Mazzocco K, Houssami N, Pagani O, Senkus
E and Cardoso F; editorial board of The Breast: Recommendations for
triage, prioritization and treatment of breast cancer patients
during the COVID-19 pandemic. Breast. 52:8–16. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Huang SH, O'Sullivan B, Su J, Ringash J,
Bratman SV, Kim J, Hosni A, Bayley A, Cho J, Giuliani M, et al:
Hypofractionated radiotherapy alone with 2.4 Gy per fraction for
head and neck cancer during the COVID-19 pandemic: The princess
margaret experience and proposal. Cancer. 126:3426–3437. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Bhowmick NA, Oft J, Dorff T, Pal S,
Agarwal N, Figlin RA, Posadas EM, Freedland SJ and Gong J: COVID-19
and androgen-targeted therapy for prostate cancer patients. Endocr
Relat Cancer. 27:R281–R292. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Shang J, Wan Y, Luo C, Ye G, Geng Q,
Auerbach A and Li F: Cell entry mechanisms of SARS-CoV-2. Proc Natl
Acad Sci USA. 117:11727–11734. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Zhou P, Yang XL, Wang XG, Hu B, Zhang L,
Zhang W, Si HR, Zhu Y, Li B, Huang CL, et al: A pneumonia outbreak
associated with a new coronavirus of probable bat origin. Nature.
579:270–273. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Mihalopoulos M, Dogra N, Mohamed N, Badani
K and Kyprianou N: COVID-19 and kidney disease: Molecular
determinants and clinical implications in renal cancer. Eur Urol
Focus. 6:1086–1096. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Li G, Hu R and Zhang X: Antihypertensive
treatment with ACEI/ARB of patients with COVID-19 complicated by
hypertension. Hypertens Res. 43:588–590. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Rico-Mesa JS, White A and Anderson AS:
Outcomes in patients with COVID-19 infection taking ACEI/ARB. Curr
Cardiol Rep. 22:312020. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
De Spiegeleer A, Bronselaer A, Teo JT,
Byttebier G, De Tré G, Belmans L, Dobson R, Wynendaele E, Van De
Wiele C, Vandaele F, et al: The effects of ARBs, ACEis, and statins
on clinical outcomes of COVID-19 infection among nursing home
residents. J Am Med Dir Assoc. 21:909–914.e2. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Ender F, Freund A, Quecke T, Steidel C,
Zamzow P, von Bubnoff N and Gieseler F: Tissue factor activity on
microvesicles from cancer patients. J Cancer Res Clin Oncol.
146:467–475. 2020. View Article : Google Scholar :
|
|
115
|
Barnes GD, Burnett A, Allen A, Blumenstein
M, Clark NP, Cuker A, Dager WE, Deitelzweig SB, Ellsworth S, Garcia
D, et al: Thromboembolism and anticoagulant therapy during the
COVID-19 pandemic: Interim clinical guidance from the
anticoagulation forum. J Thromb Thrombolysis. 50:72–81. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Asokan I, Rabadia SV and Yang EH: The
COVID-19 pandemic and its impact on the cardio-oncology population.
Curr Oncol Rep. 22:602020. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Lee KCH, Sewa DW and Phua GC: Potential
role of statins in COVID-19. Int J Infect Dis. 96:615–617. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Aldinucci D, Borghese C and Casagrande N:
The CCL5/CCR5 axis in cancer progression. Cancers (Basel).
12:17652020. View Article : Google Scholar
|
|
119
|
Patterson BK, Seethamraju H, Dhody K,
Corley MJ, Kazempour K, Lalezari J, Pang APS, Sugai C, Mahyari E,
Francisco EB, et al: CCR5 inhibition in critical COVID-19 patients
decreases inflammatory cytokines, increases CD8 T-cells, and
decreases SARS-CoV2 RNA in plasma by day 14. Int J Infect Dis.
103:25–32. 2021. View Article : Google Scholar
|
|
120
|
Patterson BK, Seethamraju H, Dhody K,
Corley MJ, Kazempour K, Lalezari JP, Pang AP, Sugai C, Francisco
EB, Pise A, et al: Disruption of the CCL5/RANTES-CCR5 pathway
restores immune homeostasis and reduces plasma viral load in
critical COVID-19. medRxiv. 2020.05.02.20084673. 2020.
|
|
121
|
Choueiri TK, Motzer RJ, Rini BI, Haanen J,
Campbell MT, Venugopal B, Kollmannsberger C, Gravis-Mescam G,
Uemura M, Lee JL, et al: Updated efficacy results from the JAVELIN
Renal 101 trial: First-line avelumab plus axitinib versus sunitinib
in patients with advanced renal cell carcinoma. Ann Oncol.
31:1030–1039. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Aeppli S, Eboulet EI, Eisen T, Escudier B,
Fischer S, Larkin J, Gruenwald V, McDermott D, Oldenburg J, Omlin
A, et al: Impact of COVID-19 pandemic on treatment patterns in
metastatic clear cell renal cell carcinoma. ESMO Open. 5(Suppl 3):
e0008522020. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Wang C, Wang J, Shuai L, Ma X, Zhang H,
Liu R, Chen W, Wang X, Ge J, Wen Z and Bu Z: The serine/threonine
kinase AP2-associated kinase 1 plays an important role in rabies
virus entry. Viruses. 12:452019. View Article : Google Scholar
|
|
124
|
Abdelgalil AA, Al-Kahtani HM and
Al-Jenoobi FI: Erlotinib Profiles Drug Subst Excip Relat Methodol.
45:93–117. 2020. View Article : Google Scholar
|
|
125
|
Birk R, Schell A, Aderhold C, Hoch S,
Huber L, Mueller CE, Lammert A, Scherl C, Rotter N, Sommer JU and
Kramer B: Apoptosis-related proteins are altered by selective
tyrosine kinase inhibitors and everolimus in HPV-dependent SCC.
Anticancer Res. 40:6195–6203. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
El Bairi K, Trapani D, Petrillo A, Le Page
C, Zbakh H, Daniele B, Belbaraka R, Curigliano G and Afqir S:
Repurposing anticancer drugs for the management of COVID-19. Eur J
Cancer. 141:40–61. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Pang J, Xu F, Aondio G, Li Y, Fumagalli A,
Lu M, Valmadre G, Wei J, Bian Y, Canesi M, et al: Efficacy and
tolerability of bevacizumab in patients with severe Covid-19. Nat
Commun. 12:8142021. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Stebbing J, Phelan A, Griffin I, Tucker C,
Oechsle O, Smith D and Richardson P: COVID-19: Combining antiviral
and anti- inflammatory treatments. Lancet Infect Dis. 20:400–402.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Jin Z, Zhao Y, Sun Y, Zhang B, Wang H, Wu
Y, Zhu Y, Zhu C, Hu T, Du X, et al: Structural basis for the
inhibition of SARS-CoV-2 main protease by antineoplastic drug
carmofur. Nat Struct Mol Biol. 27:529–532. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Martin WR and Cheng F: Repurposing of
FDA-approved toremifene to treat COVID-19 by blocking the spike
glycoprotein and NSP14 of SARS-CoV-2. J Proteome Res. 19:4670–4677.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Dhar D and Mohanty A: Gut microbiota and
Covid-19-possible link and implications. Virus Res. 285:1980182020.
View Article : Google Scholar
|
|
132
|
Bottari B, Castellone V and Neviani E:
Probiotics and Covid-19. Int J Food Sci Nutr. 72:293–299. 2021.
View Article : Google Scholar
|
|
133
|
Annweiler G, Corvaisier M, Gautier J,
Dubée V, Legrand E, Sacco G and Annweiler C: Vitamin D
supplementation associated to better survival in hospitalized frail
elderly COVID-19 patients: The GERIA-COVID quasi-experimental
study. Nutrients. 12:33772020. View Article : Google Scholar :
|
|
134
|
Jeon SM and Shin EA: Exploring vitamin D
metabolism and function in cancer. Exp Mol Med. 50:1–14. 2018.
|
|
135
|
Munshi R, Hussein MH, Toraih EA, Elshazli
RM, Jardak C, Sultana N, Youssef MR, Omar M, Attia AS, Fawzy MS, et
al: Vitamin D insufficiency as a potential culprit in critical
COVID-19 patients. J Med Virol. 93:733–740. 2021. View Article : Google Scholar
|
|
136
|
Carpagnano GE, Di Lecce V, Quaranta VN,
Zito A, Buonamico E, Capozza E, Palumbo A, Di Gioia G, Valerio VN
and Resta O: Vitamin D deficiency as a predictor of poor prognosis
in patients with acute respiratory failure due to COVID-19. J
Endocrinol Invest. 44:765–771. 2021. View Article : Google Scholar
|
|
137
|
Shakoor H, Feehan J, Al Dhaheri AS, Ali
HI, Platat C, Ismail LC, Apostolopoulos V and Stojanovska L:
Immune-boosting role of vitamins D, C, E, zinc, selenium and
omega-3 fatty acids: Could they help against COVID-19? Maturitas.
143:1–9. 2021. View Article : Google Scholar
|
|
138
|
Akula SM, Abrams SL, Steelman LS, Candido
S, Libra M, Lerpiriyapong K, Cocco L, Ramazzotti G, Ratti S, Follo
MY, et al: Cancer therapy and treatments during COVID-19 era. Adv
Biol Regul. 77:1007392020. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Tan HW, Mo HY, Lau ATY and Xu YM: Selenium
species: Current status and potentials in cancer prevention and
therapy. Int J Mol Sci. 20:752018. View Article : Google Scholar
|
|
140
|
Chung YH, Beiss V, Fiering SN and
Steinmetz NF: COVID-19 vaccine frontrunners and their
nanotechnology design. ACS Nano. 14:12522–12537. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Thakkar A, Gonzalez-Lugo JD, Goradia N,
Gali R, Shapiro LC, Pradhan K, Rahman S, Kim SY, Ko B, Sica RA, et
al: Seroconversion rates following COVID-19 vaccination among
patients with cancer. Cancer Cell. 39:1081–1090.e2. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Rodriguez Socarrás M, Gómez Rivas J, Teoh
JY, Puente J, Moschini M and Moreno-Sierra J: The Uro-oncology
patient and vaccination against SARS-CoV-2. Eur Urol Open Sci.
29:77–81. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Gavriatopoulou M, Ntanasis-Stathopoulos I,
Korompoki E, Terpos E and Dimopoulos MA: SARS-CoV-2 vaccines in
patients with multiple myeloma. Hemasphere. 5:e5472021. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Han HJ, Nwagwu C, Anyim O, Ekweremadu C
and Kim S: COVID-19 and cancer: From basic mechanisms to vaccine
development using nanotechnology. Int Immunopharmacol.
90:1072472021. View Article : Google Scholar
|
|
145
|
von Lilienfeld-Toal M, Rieger C, Giesen N
and Wörmann B: Vaccination against SARS-CoV-2 in cancer patients.
Onkologe (Berl). 1–6. May 17–2021.In German. Epub ahead of print.
View Article : Google Scholar
|
|
146
|
Mondal M, Guo J, He P and Zhou D: Recent
advances of oncolytic virus in cancer therapy. Hum Vaccin
Immunother. 16:2389–2402. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Cao GD, He XB, Sun Q, Chen S, Wan K, Xu X,
Feng X, Li PP, Chen B and Xiong MM: The oncolytic virus in cancer
diagnosis and treatment. Front Oncol. 10:17862020. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Nguyen HM, Guz-Montgomery K and Saha D:
Oncolytic virus encoding a master pro-inflammatory cytokine
interleukin 12 in cancer immunotherapy. Cells. 9:4002020.
View Article : Google Scholar :
|
|
149
|
Wang G, Kang X, Chen KS, Jehng T, Jones L,
Chen J, Huang XF and Chen SY: An engineered oncolytic virus
expressing PD-L1 inhibitors activates tumor neoantigen-specific T
cell responses. Nat Commun. 11:13952020. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Ji W, Li L, Zhou S, Qiu L, Qian Z, Zhang H
and Zhao P: Combination immunotherapy of oncolytic virus
nanovesicles and PD-1 blockade effectively enhances therapeutic
effects and boosts antitumour immune response. J Drug Target.
28:982–990. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Duijf PHG: Low baseline pulmonary levels
of cytotoxic lymphocytes as a predisposing risk factor for severe
COVID-19. mSystems. 5:e00741202020. View Article : Google Scholar
|
|
152
|
Challenor S and Tucker D:
SARS-CoV-2-induced remission of Hodgkin lymphoma. Br J Haematol.
192:4152021. View Article : Google Scholar : PubMed/NCBI
|