Introduction
Syncope is a common health concern with significant
clinical consequences and diverse underlying etiologies. In
clinical practice, the accurate diagnosis of the causes of syncope
is often challenging and demanding (1,2).
Moreover, some rare electrocardiographic phenomena may complicate
the diagnostic workup, leading to imprecise diagnoses. Undoubtedly,
a specific diagnosis is a prerequisite for an effective management
plan (1,2).
The present study briefly describes the case of an
82-year-old male patient with ischemic cardiomyopathy who suffered
syncopal episodes in the setting of trifascicular block.
Case report
An 82-year-old male patient with a history of
anterior myocardial infarction and hypertension suffered two
syncopal episodes in the sitting position without prodromal
symptoms during the previous few weeks. His medications included
bisoprolol, valsartan, aspirin, and atorvastatin. The patient was
referred to The First Department of Cardiology, University Hospital
of Ioannina, Ioannina, Greece for further evaluation by his general
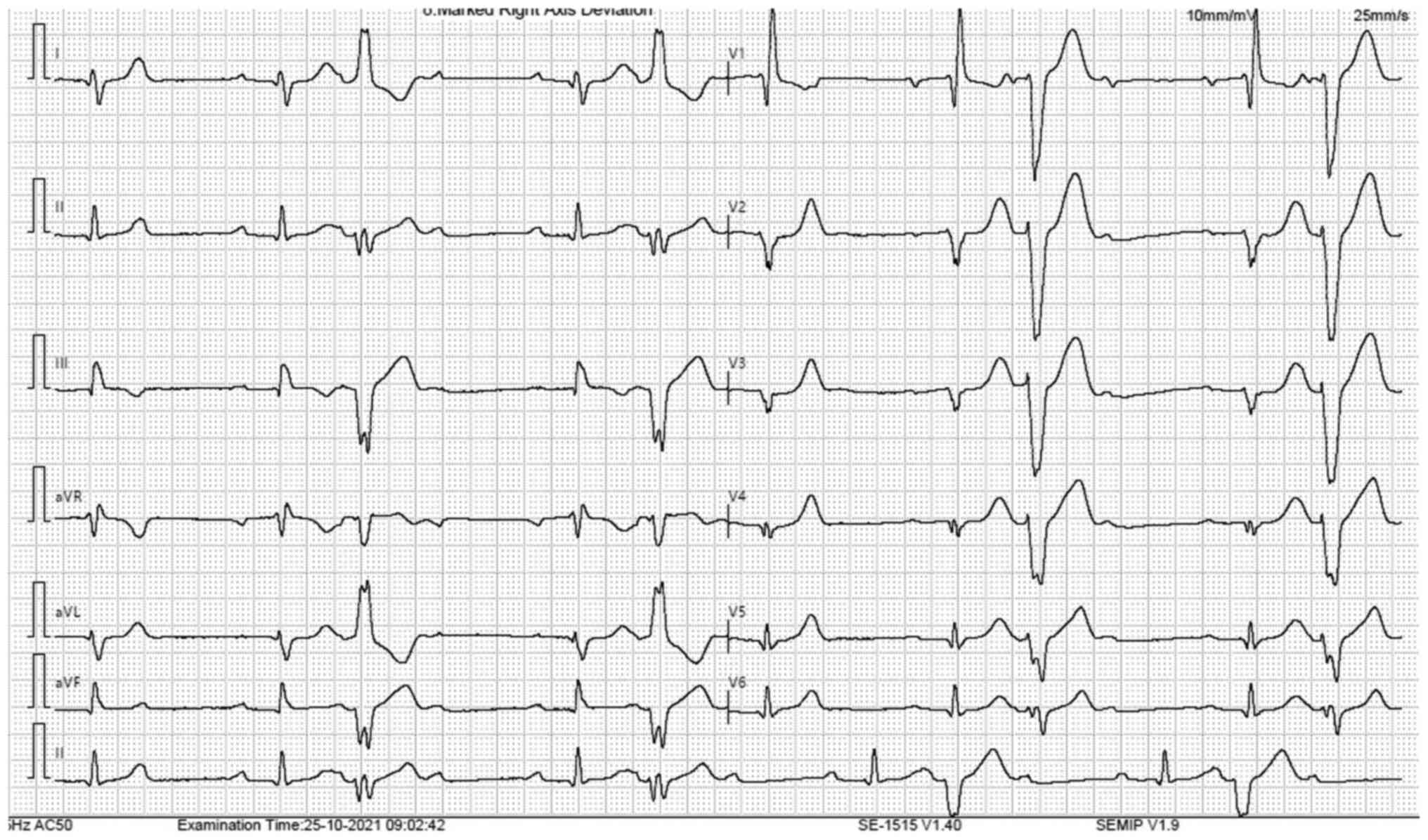
physician. His baseline 12-lead electrocardiogram (ECG) revealed
sinus rhythm, first-degree atrioventricular block, right bundle
branch block, left posterior hemiblock (LPH), Q wave in leads V1-V5
(consistent with the old myocardial infarction), and ventricular
bigeminy (Fig. 1). Of note, two
different morphologies of premature ventricular contractions (PVCs)
were evident, raising the suspicion of an ischemic substrate.
Interestingly, after each PVC, a non-conducted sinus beat was
evident (Fig. 1). This form of
atrioventricular block is not generally considered pathological,
since it is explained by the phenomenon of retrograde concealed
conduction. An echocardiogram revealed a left ventricular ejection
fraction (LVEF) of 40%, anterior wall akinesia, and mild mitral
regurgitation. A myocardial perfusion single photon emission
computed tomography did not demonstrate reversible myocardial
ischemia. Moreover, electrocardiographic monitoring for 24 h did
not reveal any bradycardia events or episodes of second- or
third-degree atrioventricular block. However, similar to the
baseline ECG, several episodes of ventricular bigeminy were
observed, while the burden of PVCs was 15% of the total beats.
Although an immediate implantation of a permanent
pacemaker would be a sensible approach based on the clinical
history and the electrocardiographic findings of trifascicular
block and LPH (which is not benign), an electrophysiological study
was first performed, given the presence of ischemic cardiomyopathy
with moderately depressed LVEF in order to exclude a predisposition
to malignant ventricular arrhythmias. Of note, the programmed
ventricular stimulation failed to induce ventricular tachycardia.
However, the HV interval was 90 msec, and the Wenckebach point was
at a cycle length of 650 msec (92 bpm). Based on these findings, as
well as on the depressed LVEF and the anticipated high burden of
ventricular pacing, a biventricular pacemaker was implanted.
Furthermore, medical treatment for heart failure was optimized, and
the dose of beta-blocker was up-titrated, leading to amelioration
of the burden of PVCs. At 12 months after the implantation, the
patient was clinically stable with a slightly improved LVEF (45%),
an effective biventricular pacing level of 97%, and without any
atrial or ventricular arrhythmias recorded by the device
diagnostics. No further syncopal episodes were noted, while the
daily level of PVCs during the last device interrogation was
<2%.
Discussion
Bearing in mind that the patient in the present
study had trifascicular block with LPH, the latter being associated
with structural heart disease and/or significant pathology in the
conduction system (3), it is
possible that the dropped sinus beats may have been falsely
attributed to atrioventricular block. However, these non-conducted
sinus beats occurred only after the PVCs. This rare phenomenon is
due to the incomplete retrograde penetration of the
atrioventricular node by the PVCs, causing a transient modification
of its antegrade conduction characteristics (4,5). Of
note, the retrograde electrical stimulation of the atrioventricular
node is not directly apparent on the ECG, as it is ‘concealed’.
However, it affects the subsequent conduction patterns, causing
increased refractoriness of the atrioventricular node, manifested
either as a prolonged PR interval in the subsequent conducted sinus
beat or as a block of the next sinus beat, as observed in the case
described herein (2,3).
Indeed, the consequences of retrograde concealed
conduction of a PVC may vary depending on whether there is
concomitant antegrade intranodal excitation, as well as on the
degree of retrograde penetration (4,6).
Therefore, the variable response of the atrioventricular
conduction/atrioventricular refractoriness following retrograde
concealed conduction may vary from a simple transient prolongation
of the PR interval (variable PR intervals may be observed) to a
completely blocked atrial beat (5,6).
Notably, both phenomena can be observed during a continuous
electrocardiographic recording of a particular patient (5). Another phenomenon that may ensue due to
retrograde concealed conduction of a PVC is a temporary nodal
escape rhythm with atrioventricular dissociation (6).
Retrograde concealed conduction per se is not an
indication for permanent pacemaker implantation. Atrioventricular
block due to retrograde concealed conduction is very transient and
usually does not cause symptoms, while beta-blocker therapy can be
continued and even up-titrated for the suppression of the PVCs
(5). In the case presented herein,
this phenomenon was evident in the setting of trifascicular block
in a patient with ischemic cardiomyopathy and moderately reduced
LVEF who suffered syncopal episodes. Therefore, after exclusion of
myocardial ischemia, further evaluation with an
electrophysiological study was performed, revealing severe
conduction abnormalities in the atrioventricular node and
His-Purkinje system, while malignant ventricular arrhythmias were
not induced. Of note, in patients with impaired atrioventricular
conduction and a diseased His-Purkinje system, retrograde concealed
conduction may aggravate these abnormalities (7).
In conclusion, even though retrograde concealed
conduction is considered a benign phenomenon, further meticulous
investigation is required in patients with concomitant baseline
conduction abnormalities and/or structural heart disease.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DS, CSK and PK managed the patient and
conceptualized the case report. DS and CSK searched the literature.
DS and PK wrote and prepared the draft of the manuscript. CSK and
PK provided critical revisions. All authors confirm the
authenticity of all the raw data. All authors contributed to
manuscript revision and have read and approved the final version of
the manuscript.
Ethics approval and consent to
participate
The patient provided signed consent for his
participation in the present study.
Patient consent for publication
The patient in the present study provided signed
consent for the publication of his medical case anonymously.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Brignole M and Rivasi G: New insights in
diagnostics and therapies in syncope: A novel approach to
non-cardiac syncope. Heart. 107:864–873. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pascual JF, Marchite PJ, Silva JR and
Gándara NR: Arrhythmic syncope: From diagnosis to management. World
J Cardiol. 15:119–141. 2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pérez-Riera AR, Barbosa-Barros R,
Daminello-Raimundo R, de Abreu LC, Mendes JE and Nikus K: Left
posterior fascicular block, state-of-the-art review: A 2018 update.
Indian Pacing Electrophysiol J. 18:217–230. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lehmann MH, Mahmud R, Denker S, Soni J and
Akhtar M: Retrograde concealed conduction in the atrioventricular
node: Differential manifestations related to level of intranodal
penetration. Circulation. 70:392–401. 1984.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Oh YZ, Tan VH and Wong KC: Concealed
conduction of premature ventricular complexes resulting in AV nodal
block. J Arrhythm. 33:528–529. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Schamroth L: Concealed retrograde
conduction. Am J Cardiol. 8:682–683. 1961.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Akhtar M: Retrograde Concealed conduction
in the His-Purkinje system. Card Electrophysiol Clin. 8:771–772.
2016.PubMed/NCBI View Article : Google Scholar
|