Introduction
Intracranial aneurysms are abnormal, balloon-shaped
dilations of the walls of intracranial arteries. Depending on their
size and other risk factors, such as cigarette smoking and an
uncontrollably high blood pressure, they have a tendency to
rupture.
Unruptured intracranial aneurysms (UIAs) are
comparatively frequent lesions that account for 0.4-6% of the
general population (1,2). During the previous decades, there was a
huge debate on whether to treat UIAs or follow them up. On the one
hand, the possible complications of the ‘wait and see’ approach,
namely the rupture of the aneurysm (electrolyte disturbance,
hydrocephalus, vasospasm, coma and mortality) had to be taken into
account, while on the other hand, the possible complications of the
elective surgical treatment of an intracranial aneurysm
(post-operative pain, blood loss, epileptic seizures, cerebral
laceration, neurological deficit and mortality) had to be
considered. The ‘compass’ that was used to provide guidance of
cases of UIAs was the annual rupture risk of a UIA vs. the risks
associated with surgical management (3).
The annual risk of rupture during the lifetime of a
patient with a UIA (also known as the natural risk) of UIAs is
found to be 1-2%, and that risk is added to the risk of the
following year for every year of life. Thus, for a 20-year-old
patient with a UIA, there is a 40-80% chance of an aneurysm rupture
by the age of 60 years, while for a 40-year-old patient with a UIA,
there is a 20-40% chance of an aneurysm rupture by the age of 60
years. Additionally, the mortality of rate of patients with a
ruptured aneurysm is 40%, while in other research series, that
number increases to 50% (3).
By contrast, the morbidity associated with the
microsurgical treatment of UIAs has been found to be lower than
that for ruptured aneurysms (4,5). Under
that scope, the suggested modality for UIAs was to treat them, as
the treatment has superior results and fewer complications compared
to the natural history of the disease and the possible
complications following an aneurysm rupture, at least for the
younger patients (4,5).
That dogma is used mostly for anterior circulation
aneurysms, while the management method of a posterior circulation
aneurysm is a debatable theme. The issue is that the majority of
studies which mention outcomes from the surgical management of UIAs
have excluded posterior circulation aneurysms, possibly since these
aneurysms are considered surgically challenging and are associated
with a higher morbidity risk compared with their anterior
circulation counterparts (3-5). In
detail, some reports mention a 4.2% unfavorable outcome rate
associated with the surgical management of posterior circulation
aneurysms. Notwithstanding, it should be noted that these reports
included only giant aneurysms (3,4,6), which are the most demanding when they
are treated surgically.
It is well known that there are some studies with
notable findings; these studies evaluated the natural risk of
bleeding in the UIAs and proposed various management options for
posterior and anterior circulation aneurysms (7,8).
However, there is limited information available regarding the
specific influence of the location of the aneurysm (anterior vs.
posterior circulation UIAs) on surgical outcomes.
The present meta-analysis aimed to assess the
association between the surgical outcomes of patients with anterior
vs. posterior circulation UIAs. Moreover, in order to define the
procedural good neurological outcomes, morbidity and mortality, the
modified Rankin scale (mRS) >2 was used for patients with a UIA
that were treated surgically.
Data and methods
Literature search strategy
The present meta-analysis investigated the
proportional articles on the surgical treatment of anterior vs.
posterior circulation UIAs through electronic databases, including
the Cochrane Library, PubMed (1980 to March, 2023), Medline (1980
to March, 2023) and EMBASE (1980 to March, 2023). Preferred
Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)
(9) served as the foundation for the
protocol and manuscript design. In the Medical Subject Headings
(MeSH) list, the following key words were used: ‘Anterior and
posterior circulation aneurysms’, ‘unruptured aneurysms’, ‘anterior
vs. posterior circulation aneurysm surgery’ and ‘unruptured
aneurysm surgery’.
Inclusion and exclusion criteria
All studies included in the present meta-analysis
met the PICOS criteria as follows: i) Population: Limited to
patients that underwent aneurysm clipping surgery for UIAs anterior
and posterior circulation; ii) Intervention: Surgical treatment for
UIAs; iii) Comparison: The outcomes were evaluated and compared;
iv) Outcome measures: One of the primary outcomes, such as
procedural morbidity (mRS >2), mortality and good neurological
outcomes related to aneurysmal surgical treatment, were all
evaluated. To shun publication bias, the concluding intent was to
assemble a homogenous sum of studies involving only articles that
evaluate only two modalities: A comparison between the surgical
treatment of anterior and posterior UIAs. The present study
excluded all articles that were reviews, editorials and case
reports. Moreover, articles that investigated the pediatric
population, unrelated outcomes, comorbidities, novel techniques in
the experimental stage, or one of the two treatment options, and
all those that revealed mixed or uncertain results, being divided
between anterior and posterior circulation UIAs surgical treatment,
were also excluded.
Data extraction and outcome
definition
Two authors (GF and KF) separately extracted data
from the contained articles according to the epidemiology
guidelines of the meta-analysis. The following critical information
was retained: The main authors, publication year, entire number of
cases in the anterior and posterior circulation UIA groups, outcome
indicator, study type, etc. According to the Cochrane Handbook, the
pulled-out data was entered into a planned, standardized table
(https://training.cochrane.org/handbook).
In the case of a discrepancy, an additional author
with authority made the concluding decision. Post-operative
outcomes declared in the final pool articles were assessed at least
6 months following surgical treatment (UIAs, anterior or posterior
circulation). Furthermore, to diminish the risk of bias in the
articles, a quality assessment tool (the Newcastle-Ottawa Scale)
was performed (Table I) (10). In addition, the patients were divided
into two groups as follows: Those with anterior circulation UIAs
and those with posterior circulation UIAs.
 | Table INewcastle-Ottawa scale quality
assessment of the final article pool. |
Table I
Newcastle-Ottawa scale quality
assessment of the final article pool.
| | Newcastle-Ottawa
scale |
|---|
| Authors, year of
publication | Study design | Selection | Comparability | Exposure | Total scores | (Refs.) |
|---|
| Asari and Ohmoto,
1994 | Retrospective | 3 | 3 | 3 | 9 | (18) |
| Khanna et
al, 1996 | Retrospective | 3 | 2 | 2 | 7 | (3) |
| Grigorian et
al, 2003 | Prospective | 3 | 3 | 3 | 9 | (15) |
| Aghakhani et
al, 2008 | Retrospective | 3 | 2 | 2 | 7 | (16) |
| Sharma et
al, 2013 | Retrospective | 3 | 2 | 2 | 7 | (14) |
| Spetzler et
al, 2013 | Prospective | 3 | 3 | 3 | 9 | (12) |
| Mahaney et
al, 2014 | Retrospective and
prospective | 3 | 3 | 3 | 9 | (11) |
| Bruneau et
al, 2016 | Prospective | 3 | 2 | 2 | 7 | (13) |
| Deruty et
al, 2016 | Retrospective | 3 | 2 | 2 | 7 | (17) |
Statistical analysis
All analyses were carried out using Review Manager
Software (RevMan), version 5.4 (https://training.cochrane.org/online-learning/core-software/revman).
Heterogeneity across trials was identified using I2
statistics; I2 >50% was considered high
heterogeneity. A meta-analysis was conducted using a random-effect
model according to the Cochrane Handbook for Systematic Reviews of
Interventions (version 5.1.0; https://training.cochrane.org/online-learning/coresoftware/revman);
or else, the fixed-effect model was carried out. The continuous
outcomes (procedural morbidity (mRS >2), mortality and good
neurological outcome related to aneurysmal surgical treatment) were
stated as a weighted mean difference with 95% confidence intervals
(CIs). In the case of discontinuous variables, odds ratios (ORs)
with 95% CIs were obtained for the evaluation. A P-value <0.05
was considered to indicate a statistically significant
difference.
Results
Studies in the final pool
Following the primary search, 18 studies were
suitable for further evaluation. When all the criteria were
applied, nine articles were contained in the final study pool
(Fig. 1) (3,11-18). The comprehensive data on these
articles are presented in Table II.
The total sample of patients collected from these nine articles was
3,253 (2,662 in the anterior and 591 in the posterior circulation
UIAs group).
 | Table IIDesign and baseline characteristics
of the included studies. |
Table II
Design and baseline characteristics
of the included studies.
| | Sample size | | Anterior
circulation | Posterior
circulation | Size | Good recovery | mRS >2 | Mortality | |
|---|
| Authors, year of
publication | Ant. circ | Post. circ | Mean age
(years) | No. of males | Acom | MCA | ICA | Pcom/PCA | PICA/SCA | Basilar type | <19 mm | >19 mm | Ant. circ | Post. circ | Anterior Circ | Post. circ | Ant. circ | Post. Circ | (Refs.) |
|---|
| Asari and Ohmoto,
1994 | 71 | 5 | 61.5 | 36 | 13 | 29 | 29 | 1 | - | 4 | 68 | 8 | 70 | 4 | 1 | 1 | 0 | 0 | (18) |
| Khanna et
al, 1996 | 150 | 22 | 51.9 | 50 | - | - | - | - | - | - | 140 | 32 | 118 | 12 | 7 | 5 | 0 | 0 | (3) |
| Grigorian et
al, 2003 | 325 | 40 | 53.5 | NR | 51 | 101 | 173 | - | - | 40 | 159 | 206 | 304 | 30 | 21 | 10 | 1 | 0 | (15) |
| Aghakhani et
al, 2008 | 194 | 44 | 49 | 127 | 44 | 117 | 33 | 40 | 3 | 1 | 178 | 60 | 194 | 42 | 0 | 2 | 0 | 0 | (16) |
| Sharma et
al, 2013 | 74 | 5 | 55.07 | 21 | 14 | 28 | 3 | 9 | 4 | 0 | 69 | 10 | 69 | 4 | 5 | 1 | 2 | 0 | (14) |
| Spetzler et
al, 2013 | 161 | 48 | NR | NR | 75 | 29 | 20 | 39 | 23 | 8 | 209 | 0 | 118 | 27 | 43 | 21 | 0 | 0 | (12) |
| Mahaney et
al, 2014 | 1,393 | 410 | 52.7 | NR | 285 | 615 | 493 | 304 | - | 106 | 701 | 407 | 1,322 | 338 | 1 | 4 | 0 | 0 | (11) |
| Bruneau et
al, 2016 | 215 | 13 | 51.3 | 55 | 22 | 137 | 4 | 1 | 7 | 5 | NR | NR | 215 | 13 | 0 | 0 | 0 | 0 | (13) |
| Deruty et
al, 2016 | 79 | 4 | 46 | 40 | 13 | 29 | 37 | - | - | 4 | NR | NR | 77 | 2 | 2 | 2 | 1 | 1 | (17) |
Good recovery
A total of nine articles (3,11-18)
provided information on good recovery following surgical treatment.
There were 2,959 patients (2,487 or 93.42% in the anterior
circulation group and 472 or 79.86% in the posterior circulation
group), and there was a statistically significant difference
between groups (OR, 3.38; 95% CI, 2.58 to 5.77; P<0.05),
demonstrating the statistical superiority of the anterior
circulation group of UIAs; however, there was low heterogeneity
(P=0.23 and I2=25%) (Fig.
2A). While evaluating the sensitivity, one study was removed at
a time using the ‘leave-one-out’ model (Table III). Following the removal of the
article by Deruty et al (17), there was additionally a statistically
significant superiority over the groups (OR, 3.66; 95% CI, 2.79 to
4.81; P<0.05), with no heterogeneity (P=0.46 and
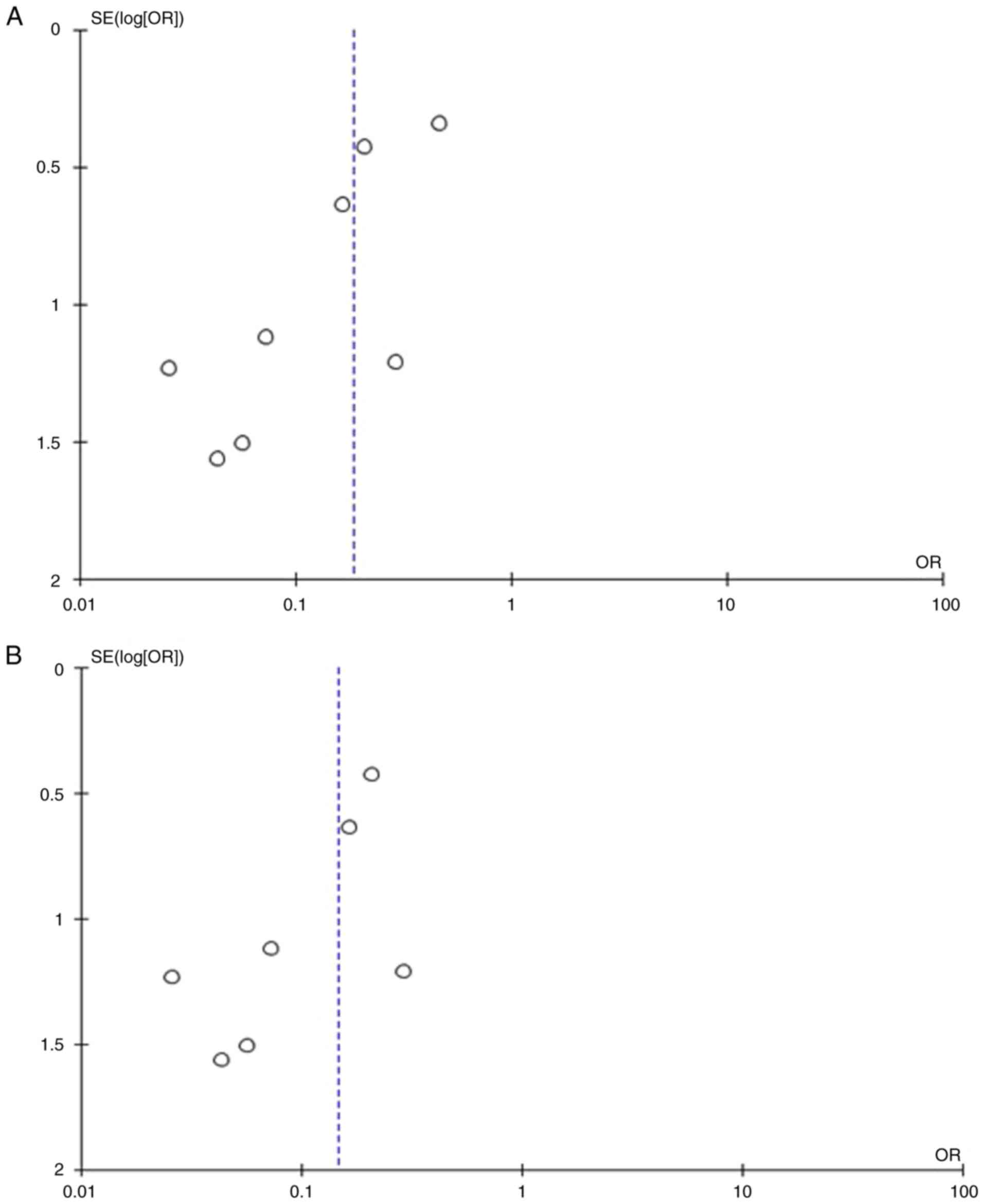
I2=0%) (Fig. 2Β). When
the funnel plot was utilized for the analysis of the same
parameter, it was found that the study results without the study by
Deruty et al (17) revealed a
better dispersion with no publication bias compared with the
results of the same analysis if this one article was included
(Fig. 2C and D).
 | Figure 2(A) Forest plot for good recovery: The
results demonstrate a statistically significant difference between
groups (OR 3.86; 95% CI, 2.58 to 5.77; P<0.05), with a low
heterogeneity. (B) OR forest plot for good recovery without the
study by Deruty et al (17).
The results demonstrate a statistically significant difference (OR,
3.66; 95% CI, 2.79 to 4.81; P<0.05). (C) Funnel plot of good
recovery between groups, with the study by Deruty et al
(17) and with a low heterogeneity
(P=0.23 and I2=25%). (D) Funnel plot of good recovery
between groups, without the study Deruty et al (17), and without heterogeneity (P=0.46 and
I2=0%). I2, the percentage of total variation
across studies that is due to heterogeneity rather than chance; CI,
confidence interval; OR, odds ratio. |
 | Table IIIOutcomes of the meta-analysis. |
Table III
Outcomes of the meta-analysis.
| | Groups | Overall effect | Heterogeneity | |
|---|
| Parameters | ‘Leave-one-out’
model | Trial, n=9 | Ant. circ | Post. circ | Effect
estimate | 95% CI | P-value | I2
(%) | P-value | (Refs.) |
|---|
| Good recovery | - | 9 | 2662 | 591 | 3.86 | (2.58-5.77) | <0.05 | 25 | 0.23 | |
| | Asari and Ohmoto,
1994 | 8 | 2591 | 586 | 3.75 | (2.50-5.63) | <0.05 | 28 | 0.22 | (18) |
| | Khanna et
al, 1996 | 8 | 2512 | 569 | 4.14 | (2.53-6.79) | <0.05 | 34 | 0.17 | (3) |
| | Grigorian et
al, 2003 | 8 | 2337 | 551 | 3.79 | (2.30-6.26) | <0.05 | 33 | 0.18 | (15) |
| | Aghakhani et
al, 2008 | 8 | 2468 | 547 | 3.73 | (2.52-5.53) | <0.05 | 25 | 0.24 | (16) |
| | Sharma et
al, 2013 | 8 | 2588 | 586 | 3.94 | (2.52-6.17) | <0.05 | 36 | 0.16 | (14) |
| | Spetzler et
al, 2013 | 8 | 2501 | 543 | 4.22 | (3.14-5.68) | <0.05 | 0 | 0.42 | (12) |
| | Mahaney et
al, 2014 | 8 | 1269 | 181 | 4.18 | (2.24-7.83) | <0.05 | 34 | 0.17 | (11) |
| | Bruneau et
al, 2016 | 8 | 2447 | 578 | 3.86 | (2.58-5.77) | <0.05 | 25 | 0.23 | (13) |
| | Deruty et
al, 2016 | 8 | 2583 | 587 | 3.66 | (2.79-4.81) | <0.05 | 0 | 0.46 | (17) |
| mRS >2 | - | 9 | 2662 | 591 | 0.19 | (0.10-0.36) | <0.05 | 35 | 0.15 | |
| | Asari et al,
1994 | 8 | 2591 | 586 | 0.19 | (0.10-0.39) | <0.05 | 39 | 0.13 | (18) |
| | Khanna et
al, 1996 | 8 | 2512 | 569 | 0.18 | (0.08-0.39) | <0.05 | 42 | 0.11 | (3) |
| | Grigorian et
al, 2003 | 8 | 2337 | 551 | 0.15 | (0.06-0.38) | <0.05 | 43 | 0.10 | (15) |
| | Aghakhani et
al, 2008 | 8 | 2468 | 547 | 0.20 | (0.10-0.39) | <0.05 | 37 | 0.14 | (16) |
| | Sharma et
al, 2013 | 8 | 2588 | 586 | 0.17 | (0.08-0.36) | <0.05 | 44 | 0.19 | (14) |
| | Spetzler et
al, 2013 | 8 | 2501 | 543 | 0.15 | (0.08-0.27) | <0.05 | 0 | 0.63 | (12) |
| | Mahaney et
al, 2014 | 8 | 1269 | 181 | 0.20 | (0.10-0.40) | <0.05 | 37 | 0.14 | (11) |
| | Bruneau et
al, 2016 | 8 | 2447 | 578 | 0.19 | (0.10-0.36) | <0.05 | 35 | 0.15 | (13) |
| | Deruty et
al, 2016 | 8 | 2583 | 587 | 0.24 | (0.13-0.41) | <0.05 | 18 | 0.29 | (17) |
| Mortality | - | 9 | 2662 | 591 | 0.17 | (0.03-0.77) | 0.05 | 0 | 0.49 | |
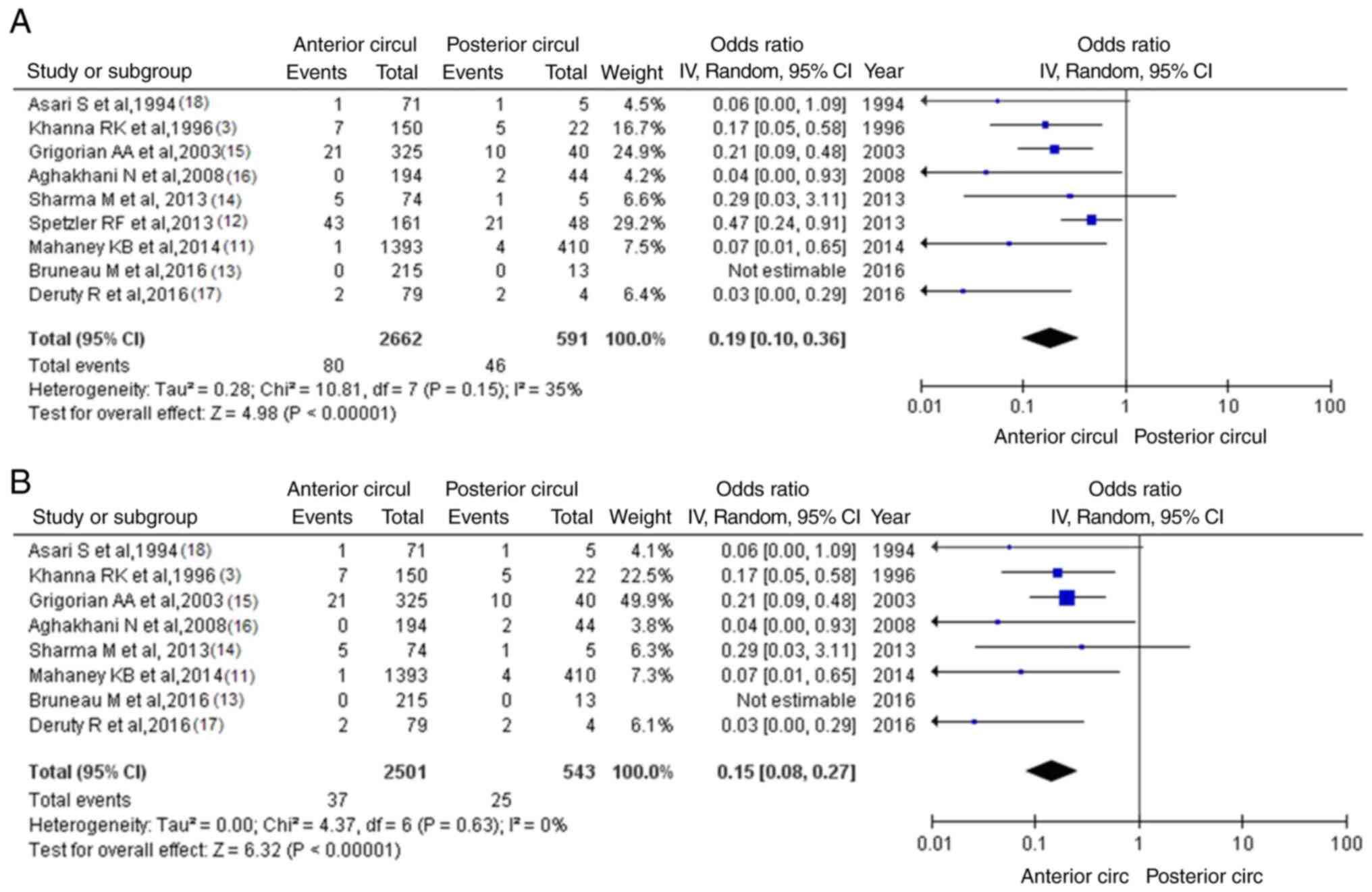
mRS >2
Information regarding mRS >2 was available in
nine articles (3,11-18).
There were 126 patients (80 or 3.00% in the anterior circulation
group and 46 or 7.78% in the posterior circulation group), and
there was a statistically significant difference between groups
(OR, 0.19; 95% CI, 0.10 to 0.36; P<0.05), demonstrating the
statistical superiority of the anterior circulation group of UIAs;
however, there was a low heterogeneity (P=0.15 and
I2=35%) (Fig. 3A). While
assessing the sensitivity, one study was removed at a time using
the ‘leave-one-out’ model (Table
III). After eliminating the article by Spetzler et al
(12), there was additionally a
statistically significant superiority over the groups (OR, 0.15;
95% CI, 0.08 to 0.27; P<0.05), with no heterogeneity (P=0.63 and
I2=0%) (Fig. 3Β). When
studying the funnel plot of the same parameter, it was observed
that the study results without the study by Spetzler et al
(12) revealed better dispersion
with no publication bias, in contrast to the same analysis
including this one article (Fig. 4A
and B). Given that the patients in
the study by Spetzler et al (12) represented 50.7% (64/126) of the
included articles, this was not a surprise.
Mortality
Information for mortality was available in nine
articles (3,11-18).
In the entry group of patients, there were 5 patients [4 (0.15%) in
the anterior circulation group and 1 (0.17%) in the posterior
circulation group], demonstrated a statistically significant
difference between the groups (OR, 0.17; 95% CI, 0.03 to 1.00;
P=0.05), with no heterogeneity (P=0.49 and I2=0%
(Fig. 5A) and the superiority of the
anterior circulation group compared with the posterior circulation
UIAs group. A summary of the results of the present meta-analysis
is presented in Table III.
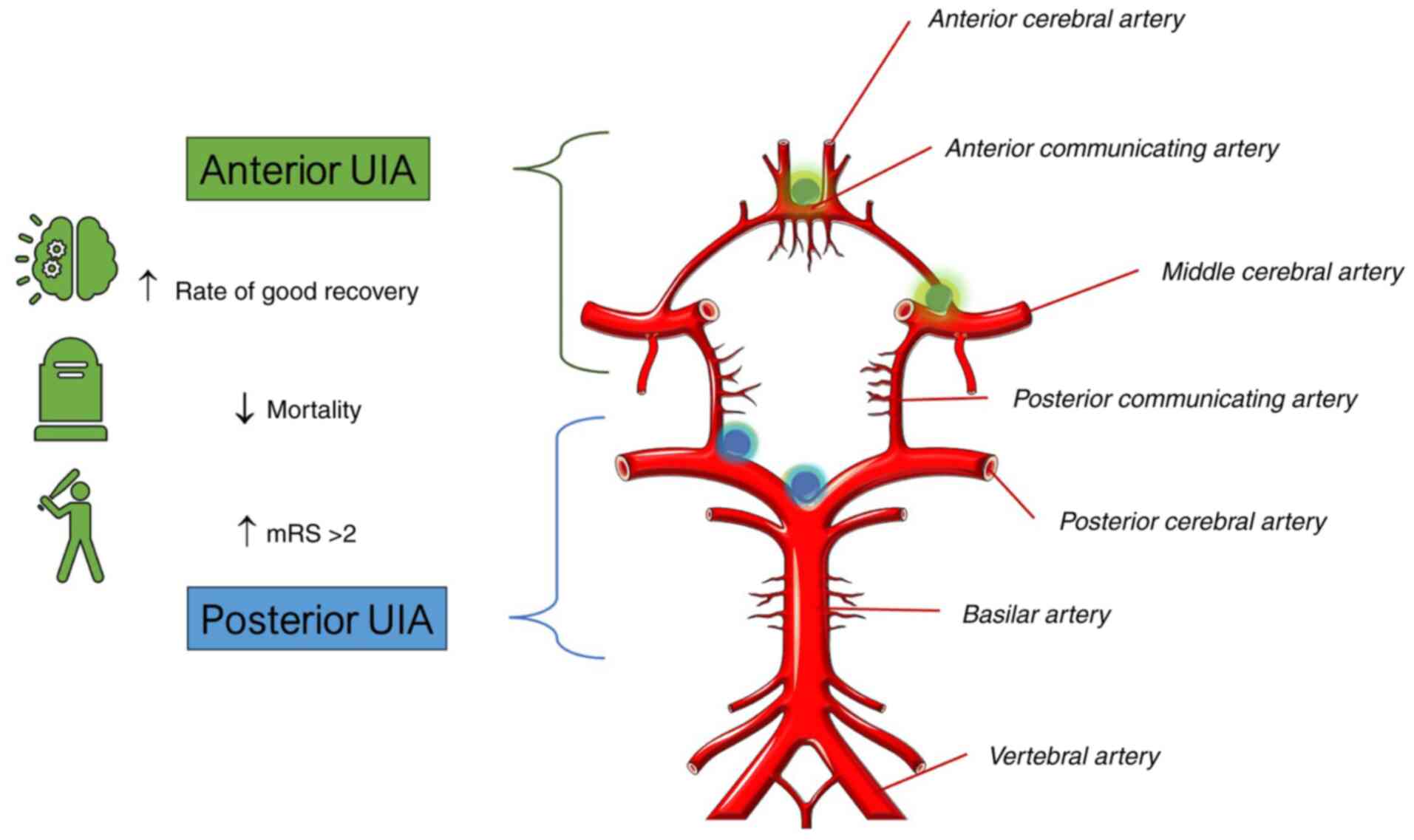
A summary of the meta-analysis results comparing the
outcomes of surgical treatment for UIAs in the anterior and
posterior circulation is presented in Fig. 6.
Discussion
Τhe optional modality for UIAs was to treat them
(4,5); however, that recommendation is applied
mostly for anterior circulation aneurysms, while the management
method of a posterior circulation aneurysm is a debatable issue
(3).
Thus, the present meta-analysis proposes that the
surgical treatment of the anterior circulation UIAs is associated
with better outcomes than the surgical management of posterior
circulation UIAs. More precisely, mortality was a statistically
significant parameter in patients with UIAs who were surgically
treated, demonstrating the superiority of anterior compared to
posterior circulation UIAs. In addition, mRS >2 and good
recovery were statistically significant factors, demonstrating the
advantage of surgical management of the anterior circulation UIAs
compared with posterior circulation UIAs.
It has been reported that hemorrhage rates are
significantly higher in the untreated group than in surgically
treated patients (3). However,
derived from a previously identified natural history between
posterior vs. anterior circulation aneurysms, anterior circulation
aneurysms hemorrhage less frequently (3). In addition, UIAs with posterior
circulation aneurysms have 0.5% 1-year hemorrhage rates and
morbidity. Of note, the hemorrhage rates and morbidity for patients
>65 years of age with UIAs have been shown to not differ
significantly by surgical management (3). On the other hand, in the same study and
for the same subgroup of patients with an aneurysm size >13 mm,
33% of procedure-related morbidity was reported (3). In the present meta-analysis, the
morbidity was twice higher in posterior compared with anterior
circulation UIAs.
Other studies accounting for outcomes following
surgery for UIAs have established 0 to 18% morbidity and 0 to 4%
mortality (3); however, these
studies did not include posterior circulation aneurysms, possibly
due to the high risk of morbidity related to their surgical
treatment (11,19-21).
On the other hand, Drake et al (22) reported a 14.3% morbidity rate with
the surgical management of UIAs in the posterior circulation
compared to 0% morbidity in anterior circulation UIAs. However, the
results of the present meta-analysis confirm the prognostic
significance of aneurysm location for surgical outcomes. In effect,
patients with an aneurysm in the posterior circulation had an
almost 2-fold higher risk of an unfavorable outcome following
surgical management than those with an aneurysm in the anterior
circulation. Posterior circulation and aneurysms in
difficult-to-access areas (arachnoid aneurysms, cavernous internal
carotid artery) are possibly technically complex for representation
and clip. They may have an increased morbidity and mortality
associated with their treatment. Thus, the aneurismal location
affects the operative morbidity. Even though limited data are
available on the surgical treatment of UIAs of the posterior
circulation exists, in the accommodating study (23), patients with UIAs in the anterior
circulation had surgical morbidity rates between 4.8 and 16.8%. In
addition, research has mentioned the high surgical risk of UIAs
sited on the vertebrobasilar artery (24). However, unruptured aneurysms of the
posterior circulation can be surgically treated with a low
operative risk (25). The
International Study of Unruptured Intracranial Aneurysms (ISUIA)
recorded the overall morbidity and mortality in microsurgically
treated patients at 1 year as 12.6%, counting cognitive impairment
(8) and the evaluated risk factors
as possible interpreters of the outcome. However, the ISUA included
a larger number of patients with large aneurysms, a larger sum of
patients with posterior communicating artery and posterior
circulation aneurysms, and the ISUIA had 12.4% cavernous aneurysms,
which are known to have a more benign course (8). In addition, a previous meta-analysis on
the outcomes of surgery for unruptured aneurysms, including studies
from 1966 to 1996, mentioned a mortality rate of 2.6% and a
morbidity of 10.9%. Still, compared with the present meta-analysis,
the majority of the involved studies did not include novel
neurosurgical techniques or equipment and analyzed separated
anterior and posterior circulation UIAs as surgical treatments.
Thus, there is a risk of bias (26).
The majority of comparable studies and reviews refer
to non-randomized studies (8,11) and
have found no direct facts of clinical benefit from either
treatment concerning the natural history of these lesions, raising
a dilemma for both patients and neurosurgeons. Furthermore,
patients with unruptured intracerebral aneurysms <7 mm in size
with no evidence of rupture have been shown to have a very low
bleeding rate (0 to 1% per year) (8,11).
Consequently, obtaining a better natural history of these aneurysms
would be challenging.
A number of considerations are used in the
management of patients with UIAs. Patients <50 years of age with
aneurysms that are ≤20 mm or less in the anterior circulation have
better surgical outcomes. By contrast, patients >50 years of
age, particularly those with large aneurysms in the posterior
circulation, have the lowest surgical morbidity (27). Other key topics that require
assessment include the patient's age (e.g., to establish whether
the older patient has a worse outcome), aneurysm size, location
(posterior and anterior circulation), history of stroke (major
stroke is related to the poorest outcome), sex (female vs. male)
and the duration of hospital stay.
In many studies for overall management, it has been
established that posterior circulation aneurysms have the poorest
outcome compared with anterior circulation, which was the case for
both microsurgically and coiled-treated patients (8,14,26). On
the other hand, further analysis in a number of types of research
has not succeeded in demonstrating a statistically significant
difference in the outcome of surgically managed aneurysms when
evaluating anterior and posteriorly located aneurysms, even though
this relation was preserved for coiled-treated aneurysms (26). The current year's modifications to
aneurysm management training standards may help to explain this.
Posterior aneurysms were treated more commonly with endovascular
procedures compared with microsurgical intervention; as a
consequence of the diversion of possible unfavorable outcomes,
posterior aneurysms avoided surgical intervention, and on the way
to endovascular management, morbidity for the comparatively small
number of posterior aneurysms in the microsurgical group of
patients revealed a minimal difference in outcomes compared with
the anterior lesions. Additional patients need to be studied before
any statistical significance can be reached. However, in the
present meta-analysis, a tendency towards improved outcomes for
patients with anterior circulation aneurysms undergoing
microsurgery was observed.
Studies indicate that large aneurysms in the
posterior region are more likely to hemorrhage, while small ones in
the anterior circulation are less likely to hemorrhage. Even though
this information should be considered when treating patients with
UIAs, the majority of neurosurgeons cannot disregard the fact that
several studies with ruptured aneurysms indicate that small-sized
lesions were the most frequent aneurysms to rupture (28-30).
This generates a question for physicians who are ambiguous about
what they face in their everyday practice and what is being
published in the literature. This is more complex, as the majority
of patients with a history of aneurysm rupture may not be admitted
to the hospital, and another 25% experience severe permanent brain
injury. In addition, it appears to be a very challenging case for
the treating neurosurgeon to decide for a young patient with a
small and unruptured aneurysm. In this challenging decision-making
situation, the neurosurgeon has to take into account the fact that
it is a very superficial thought that the location and size of an
aneurysm are sufficient data with which to make a serious choice in
forecasting the performance of an aneurysm (26).
On the other hand, it must be considered that
patients who undergo surgery for UIAs from the anterior or
posterior circulation may experience retained strokes or
hemorrhages on the additional follow-up. However, if we pay
attention to a complete aneurysm clipping, it is enormously
doubtful that it will be the reason for such strokes or novel
hemorrhages. However, if all the possible locations (anterior or
posterior) and other reasons for poor outcomes that could influence
a certain population are taken into account, this would lead to an
enormous amount of probability, from the inherent characteristics
of each patient to their type of nutrition habits. It should be
recognized that, even though statistics need calibration, medicine
necessitates much perception, and the reality is that statistical
results include several probabilities in the best case, while
medical management requires diligent conclusions.
There are several limitations to the present study.
First, the majority of the eligible reports that were included were
retrospective. These retrospective studies, by definition, rely on
imprecision and data loss. Additionally, the methods of the
included studies markedly differed. Among these differences was the
length of follow-up (e.g., 30-90 days). A longer follow-up period
with these patients is warranted in order to correctly set up
outcomes associated with treatment procedures. Additionally, the
present study did not address outcomes in patients with unruptured
aneurysms that are managed conservatively.
In conclusion, the present study demonstrates that
the surgical treatment of patients with anterior circulation UIAs
is associated with better outcomes than the surgical management of
posterior circulation UIAs. In fact, mortality was a statistically
significant parameter in patients with UIAs who were surgically
treated, exhibiting the superiority of anterior compared to
posterior circulation UIAs. In addition, mRS >2 and a good
recovery were statistically significant factors, demonstrating the
advantage of surgical management of the anterior circulation UIAs
more than the posterior circulation. These findings indicate that
surgical treatment may benefit the management of anterior
circulation UIAs. It is also beyond doubt that a randomized trial
is required in order to determine the difference in outcomes
between these two treatment modalities in these patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GF and KNF conceptualized the study. VEG, GF, NT,
PS, IGL, KF and KNF analyzed the data, and wrote and prepared the
draft of the manuscript. KNF and GF provided critical revisions.
All authors contributed to manuscript revision, and have read and
approved the final version of the manuscript. GF and KF confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Qureshi AI, Janardhan V, Hanel RA and
Lanzino G: Comparison of endovascular and surgical treatments for
intracranial aneurysms: An evidence-based review. Lancet Neurol.
6:816–825. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alshekhlee A, Mehta S, Edgell RC, Vora N,
Feen E, Mohammadi A, Kale SP and Cruz-Flores S: Hospital mortality
and complications of electively clipped or coiled unruptured
intracranial aneurysm. Stroke. 41:1471–1476. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Khanna RK, Malik GM and Qureshi N:
Predicting outcome following surgical treatment of unruptured
intracranial aneurysms: A proposed grading system. J Neurosurg.
84:49–54. 1996.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Henry J, Dablouk MO, Kapoor D, Koustais S,
Corr P, Nolan D, Coffey D, Thornton J, O'Hare A, Power S, et al:
Outcomes following poor-grade aneurysmal subarachnoid haemorrhage:
A prospective observational study. Acta Neurochir (Wien).
165:3651–3664. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
King JT Jr, Berlin JA and Flamm ES:
Morbidity and mortality from elective surgery for asymptomatic,
unruptured, intracranial aneurysms: A meta-analysis. J Neurosurg.
81:837–842. 1994.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Solomon RA, Fink ME and Pile-Spellman J:
Surgical management of unruptured intracranial aneurysms. J
Neurosurg. 80:440–446. 1994.PubMed/NCBI View Article : Google Scholar
|
|
7
|
International Study of Unruptured
Intracranial Aneurysms Investigators. Unruptured intracranial
aneurysms-risk of rupture and risks of surgical intervention. N
Engl J Med. 339:1725–1733. 1998.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wiebers DO, Whisnant JP, Huston J III,
Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols
D, O'Fallon WM, et al: Unruptured intracranial aneurysms: Natural
history, clinical outcome, and risks of surgical and endovascular
treatment. Lancet. 362:103–110. 2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Foster RL: Reporting guidelines: CONSORT,
PRISMA, and SQUIRE. J Spec Pediatr Nurs. 17:1–2. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bae JM: A suggestion for quality
assessment in systematic reviews of observational studies in
nutritional epidemiology. Epidemiol Health.
38(e2016014)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mahaney KB, Brown RD Jr, Meissner I,
Piepgras DG, Huston J III, Zhang J and Torner JC: ISUIA
Investigators. Age-related differences in unruptured intracranial
aneurysms: 1-year outcomes. J Neurosurg. 121:1024–1038.
2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Spetzler RF, McDougall CG, Albuquerque FC,
Zabramski JM, Hills NK, Partovi S, Nakaji P and Wallace RC: The
barrow ruptured aneurysm trial: 3-Year results. J Neurosurg.
119:146–157. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bruneau M, Amin-Hanjani S, Koroknay-Pal P,
Bijlenga P, Jahromi BR, Lehto H, Kivisaari R, Schaller K, Charbel
F, Khan S, et al: Surgical clipping of very small unruptured
intracranial aneurysms: A multicenter international study.
Neurosurgery. 78:47–52. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Sharma M, Brown B, Madhugiri V,
Cuellar-Saenz H, Sonig A, Ambekar S and Nanda A: Unruptured
intracranial aneurysms: comparison of perioperative complications,
discharge disposition, outcome, and effect of calcification,
between clipping and coiling: A single institution experience.
Neurol India. 61:270–276. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Grigorian AA, Marcovici A and Flamm ES:
Intraoperative factors associated with surgical outcome in patients
with unruptured cerebral aneurysms: The experience of a single
surgeon. J Neurosurg. 99:452–457. 2003.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Aghakhani N, Vaz G, David P, Parker F,
Goffette P, Ozan A and Raftopoulos C: Surgical management of
unruptured intracranial aneurysms that are inappropriate for
endovascular treatment: Experience based on two academic centers.
Neurosurgery. 62:1227–1235. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Deruty R, Pelissou-Guyotat I, Mottolese C
and Amat D: Management of unruptured cerebral aneurysms. Neurol
Res. 18:39–44. 1996.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Asari S and Ohmoto T: Long-term outcome of
surgically treated unruptured cerebral aneurysms. Clin Neurol
Neurosurg. 96:230–235. 1994.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Asari S: Surgical management of the
unruptured cerebral aneurysm accompanied by ischemic
cerebrovascular disease. Clin Neurol Neurosurg. 94:119–125.
1992.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Deruty R, Pelissou-Guyotat I, Mottolese C,
Bognar L and Oubouklik A: Surgical management of unruptured
intracranial aneurysms. Personal experience with 37 cases and
discussion of the indications. Acta Neurochir (Wien). 119:35–41.
1992.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Inagawa T, Hada H and Katoh Y: Unruptured
intracranial aneurysms in elderly patients. Surg Neurol.
38:364–370. 1992.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Drake CG: Progress in cerebrovascular
disease. Management of cerebral aneurysm. Stroke. 12:273–283.
1981.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Gerlach R, Beck J, Setzer M, Vatter H,
Berkefeld J, Du Mesnil de Rochemont R, Raabe A and Seifert V:
Treatment related morbidity of unruptured intracranial aneurysms:
Results of a prospective single centre series with an
interdisciplinary approach over a 6 year period (1999-2005). J
Neurol Neurosurg Psychiatry. 78:864–871. 2007.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Eskesen V, Rosenørn J, Schmidt K, Espersen
JO, Haase J, Harmsen A, Hein O, Knudsen V, Marcussen E, Midholm S,
et al: Clinical features and outcome in 48 patients with unruptured
intracranial saccular aneurysms: A prospective consecutive study.
Br J Neurosurg. 1:47–52. 1987.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Rice BJ, Peerless SJ and Drake CG:
Surgical treatment of unruptured aneurysms of the posterior
circulation. J Neurosurg. 73:165–173. 1990.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Krisht AF, Gomez J and Partington S:
Outcome of surgical clipping of unruptured aneurysms as it compares
with a 10-year nonclipping survival period. Neurosurgery.
58:207–216. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Williams LN and Brown RD Jr: Management of
unruptured intracranial aneurysms. Neurol Clin Pract. 3:99–108.
2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Fotakopoulos G, Tsianaka E, Fountas K,
Makris D, Spyrou M and Hernesniemi J: Clipping versus coiling in
anterior circulation ruptured intracranial aneurysms: A
meta-analysis. World Neurosurg. 104:482–488. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Fotakopoulos G, Andrade-Barazarte H,
Tjahjadi M, Goehre F and Hernesniemi J: Clipping versus coiling in
ruptured basilar apex aneurysms: A meta-analysis. Turk Neurosurg.
31:301–309. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Fotakopoulos G, Andrade-Barazarte H,
Alexandros B and Hernesniemi J: A meta-analysis of Lateral
supraorbital vs mini Pterional approach in the outcome of rupture
and unruptured noncomplex aneurysms' surgery. Neurocirugia (Astur:
Engl Ed). 34:128–138. 2023.PubMed/NCBI View Article : Google Scholar
|