Introduction
Knee arthroplasty is a valuable surgical
intervention that markedly enhances the quality of life of patients
suffering from knee joint degeneration. This procedure is
considered for patients with varying degrees of disease severity,
aiming to alleviate pain and restore joint function (1). However, in some cases, patients present
with pre-existing bone loss in the tibia area, leading to more
complex surgical challenges (2,3).
The successful correction of bone loss in the tibia
region depends on the type and extent of the bone defect. The
primary objective of correcting a bone defect is to establish a
stable foundation capable of adequately supporting the knee joint
components, ensuring the weight-bearing capacity of the femoral and
tibial components without compromise (4,5). This,
in turn, enables patients to regain mobility and engage in
weight-bearing activities more efficiently post-surgery. Several
methods are employed to address bone defects, including the use of
bone cement (6), bone grafting
(7), metal and rods (8) and combinations thereof (9).
For the treatment of uncontained or segmental
defects, which entail the loss of bone extending from the internal
bone tissue to the outer edge, the combination of screws and bone
cement has emerged as the preferred approach (10). The screws play a crucial role in
reinforcing bone cement by providing an anchor for it to adhere to,
thereby increasing the overall stability (11). This approach is particularly suitable
for cases where the bone defect comprises <50% of the tibial
plateau on each side and the defect is <1 cm in depth. Studies
with long-term follow-ups have reported positive outcomes using
this method (12-14).
Despite the effectiveness of the screw-cement
combination, there is currently a wide array of screw types
available. The choice of which to use remains largely dependent on
individual surgeon preference and familiarity. Notably, there
exists a limitation in comparative studies evaluating the clinical
efficacy and mechanical impact of various screw insertion factors,
such as the screws themselves or the methods by which they are
anchored to the bone. Consequently, there is a need to investigate
these factors, which, when utilized in total knee arthroplasty
(TKA) for treating limited marginal tibial bone loss, may yield
distinct effects.
The present study aimed to address this gap by
employing finite element analysis, an advanced computer technique
for structural stress analysis developed in engineering mechanics.
The aim was to evaluate the mechanical effects of using a different
number of screws, screw locations, screw lengths and angles of
screw insertion. The findings presented herein may provide valuable
insight for surgeons when selecting the most appropriate screw
conditions for their surgical interventions.
Materials and methods
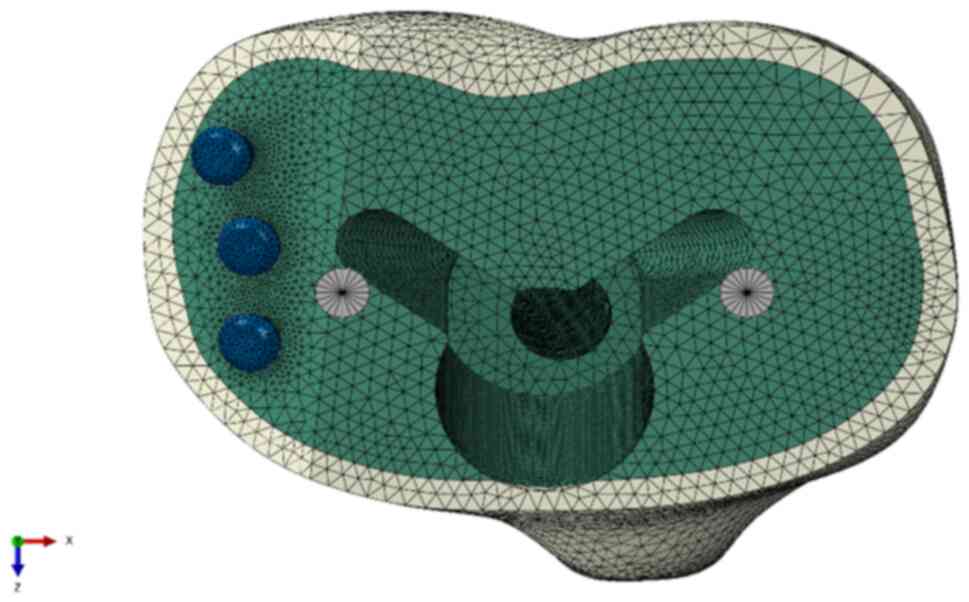
The present study commenced with the construction of
a knee prosthesis model featuring an uncontained bone defect,
specifically constituting 50% of the medial tibial plateau. The
dimensions of the defect are precise, measuring 1 cm in depth and
an incline at 30 degrees. Various parameters were systematically
adjusted in the computer model and evaluated by finite element
analysis to assess their impact on the model. This involved testing
different quantities of screws (1, 2 or 3 screws), various screw
lengths (10, 18, 30 or 40 mm), and exploring different screw
positions with lateral shifts of 2, 4 or 6 mm from the original
sites. Additionally, rotational adjustments were examined,
introducing angles of 5, 10 and 15 degrees away from the original
sites in an abduction direction.
Finite element model of knee
arthroplasty with an uncontained tibial bone defect model
construction
An artificial left tibia (Sawbones® #3401
4th gen., Composite, 17 PCF Solid Foam Core, Medium, Pacific
Research Laboratories, Inc.) with a tibial tray (Zimmer®
NexGen® Complete Knee Solution, Size 5, Zimmer Biomet
Holdings, Inc.), along with relevant components including
polymethylmethacrylate (PMMA) bone cement and Ø3.5 mm screws, was
meticulously assembled to replicate the conditions of knee
arthroplasty with an uncontained tibial bone defect. This construct
was transformed into a three-dimensional (3D) model by utilizing a
series of 256 computed tomography (CT) images, each boasting a
resolution of 512x512 pixels and a slice thickness of 1.0 mm. The
processes involved in creating the 3D model of knee arthroplasty
with an uncontained tibial bone defect encompassed the segmentation
of artificial bone and implant regions, followed by voxel
generation for constructing the 3D model. These steps were executed
using Mimics Research software (version 20.0, Materialise NV).
Subsequently, the 3D model, with a particular focus
on the tibial cortical and cancellous bones, underwent enhancement
using 3-matic research software (version 12.0, Materialise NV).
This enhancement process included the removal of extraneous
components, rectification of defects and the refinement of surfaces
to attain a precise representation of the intended construct.
To finalize the 3D model of knee arthroplasty with
an uncontained tibial bone defect, the enhanced 3D models of the
construct were imported into NX software (version 12.0, Siemens
Product Lifecycle Management Software, Inc.) for further
modifications, employing a range of functions available within the
software. The unnecessary distal portion of the artificial tibia
was removed to economize the analysis, and the uncontained bone
defect of 50% on the medial tibial plateau was refined. Due to the
metal-related artifacts evident in the CT images, it was imperative
to accurately reproduce the tibial tray and the screws. The
geometry of the tibial tray was simplified, while the geometry of
screw was enhanced to adhere to the ISO standard for metallic bone
screws. A layer of PMMA bone cement was modeled to correspond with
the surrounding tibial tray and tibial bone. The aim was to ensure
adhesion between the tibial tray and tibial bone, as well as to
fill the existing defect. However, the original positions of all 3D
components were maintained in alignment with the CT images.
The completed 3D model of the construct was then
imported into Abaqus/CAE software (version 2020, Dassault Systèmes
Simulia Corp.) to commence the creation of a finite element model.
At this stage, the tibial cancellous bone was interconnected with
the tibial cortical bone, and cavities were simulated to mimic the
fixing hole of the screw and the installation hole for the stem of
the tibial tray in relation to the PMMA bone cement and the tibial
bone (Fig. 1).
Material properties
The material properties of all components in the
present study were assumed to be homogenous, isotropic and linearly
elastic. The Young's moduli of the synthetic cortical and
cancellous bones, as provided by the manufacturer, were 16.7 GPa
and 155 MPa respectively, with Poisson's ratios of 0.30 for both.
The tibial tray and all screw types were assumed to be composed of
a titanium alloy, possessing Young's modulus and Poisson's ratios
of 110 GPa and 0.3, respectively (15). The corresponding values for the PMMA
bone cement were 2.28 GPa for the Young's modulus and 0.3 for the
Poisson's ratio (16).
Interactions, loads and boundary
conditions
In the present study, the PMMA bone cement served as
the adhesive that secured all components, including the tibial
bone, bone screw and tibial tray. These interrelated properties
were established as fully constrained to simulate the adhesive
force of the PMMA bone cement. However, the distal part of the bone
screw extended beyond the boundary of the PMMA bone cement and
penetrated into the tibial bone. Defining the bone-screw interface
property was also imperative. The contact properties between the
tibial bone, encompassing both cortical and cancellous sections,
and the bone screws were categorized into two types. The interface
of the bone screw was assigned a coefficient of friction of
0.3.
The distal end of the tibial shaft was entirely
immobilized. A compressive force of 2,100 N, equating to 2-3-fold
the normal body weight, was exerted on the tibial tray through two
loading points; one loading point was positioned approximately at
the midpoint of the medial tibial plateau, while the other was
situated near the midpoint of the lateral tibial plateau.
Furthermore, the loading conditions were bifurcated, 55 and 45% of
the total load were applied to the medial and lateral tibial
plateaus, respectively, emulating normal varus-valgus
alignment.
A mesh convergence study and sensitivity analysis
were conducted on models representing the tibial bone, as well as
bone screws. These analyses were performed to enhance the accuracy
and reliability of the simulation results.
Results
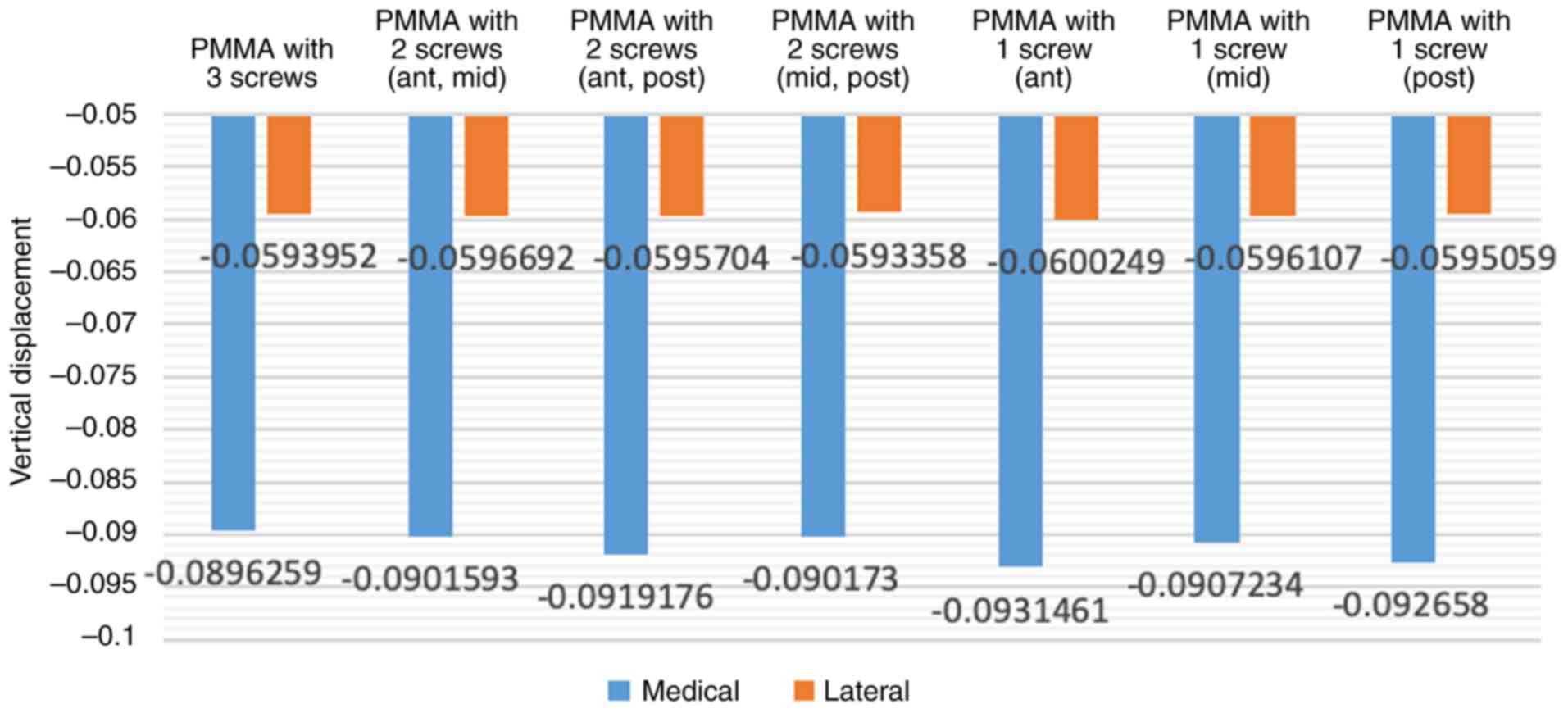
Finite element analysis of different
quantities of screws
(Fig. 2)
The comparison of the effects of the three-screw
reinforcement with those of one- or two-screw reinforcement in the
uncontained tibial bone defect filled with bone cement model
revealed that the vertical displacement values in the three-screw
reinforcement condition were lower (Fig.
3). However, in specific positions, a single screw exhibited
inferior load-bearing performance when compared to certain
scenarios involving the use of two screws. Notably, the utilization
of a single screw in the middle position exhibited superior
performance in preventing deformation in the form of abduction
angles compared to the use of two screws at anterior and posterior
positions without a middle screw. Placing a screw in the middle
position appears to play a crucial role in enhancing load-bearing
capacity.
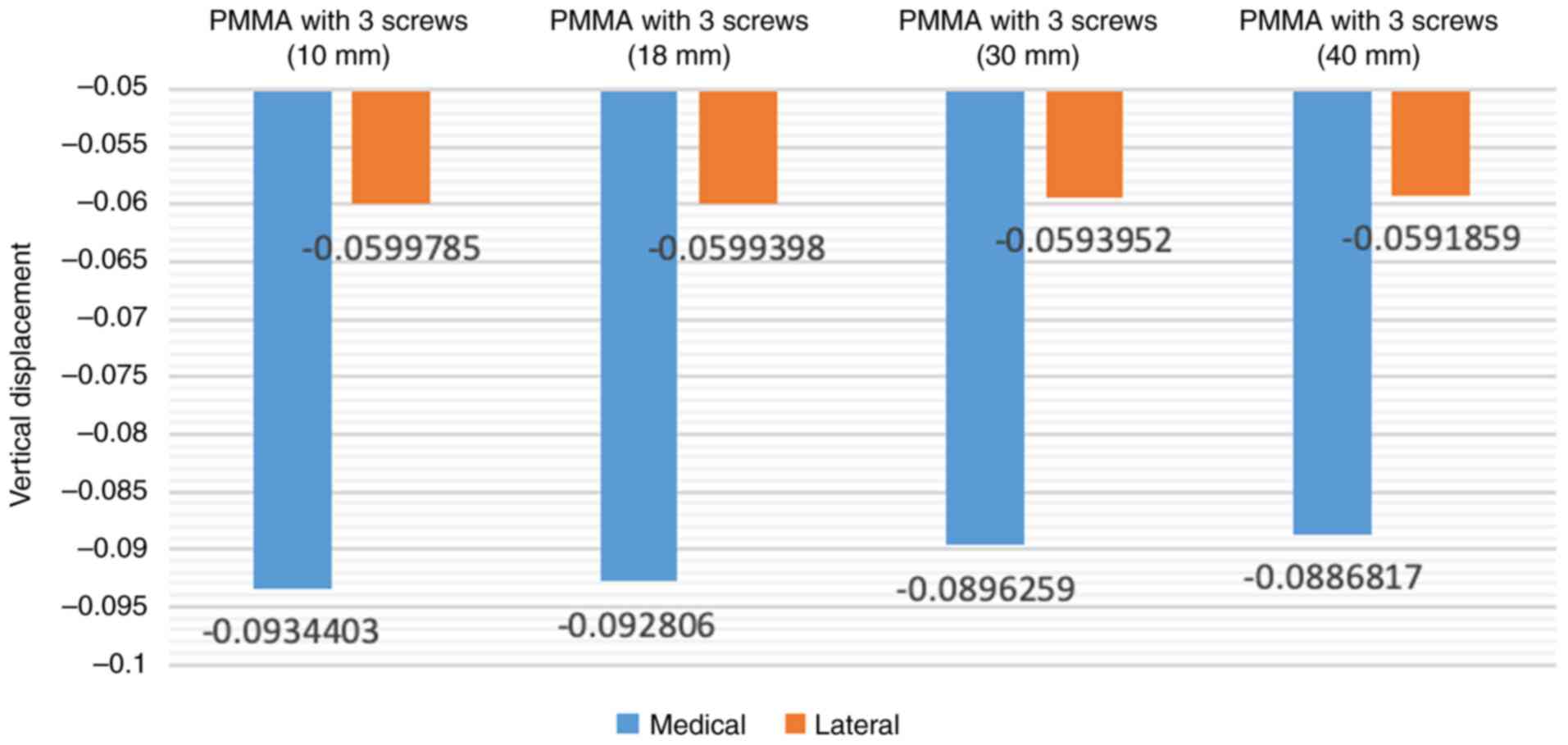
Finite element analysis of different
lengths of screws
In the initial model, the screw length employed in
the present study was 30 mm. Increasing the screw length to 40 mm
resulted in a reduction of vertical displacement values by up to
1%, and the abduction angle decreased by approximately 2.5%.
Conversely, the vertical displacement values measured at the
loading point on the tibial tray increased when the screw lengths
were decreased (10 and 18 mm screws), exhibiting an inverse
variation. The findings indicated that the length of screw
reinforcement had a direct association with the load-bearing
performance of tibial arthroplasty in the condition of an
uncontained tibial bone defect filled with bone cement (Fig. 4).
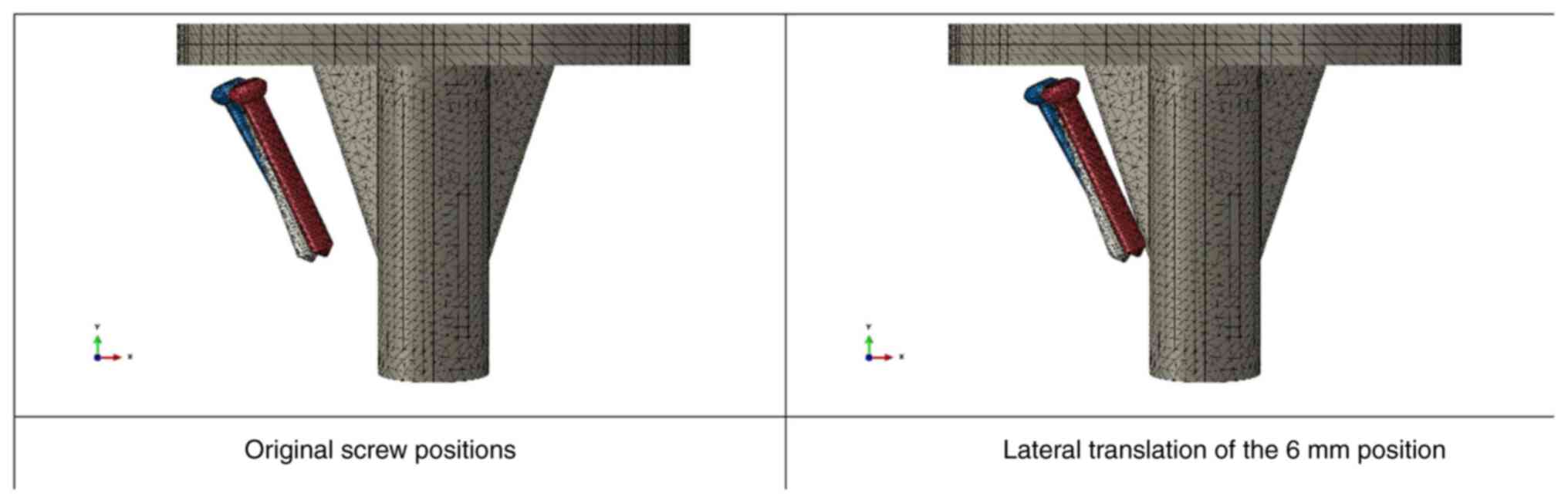
Finite element analysis of screw
placement locations
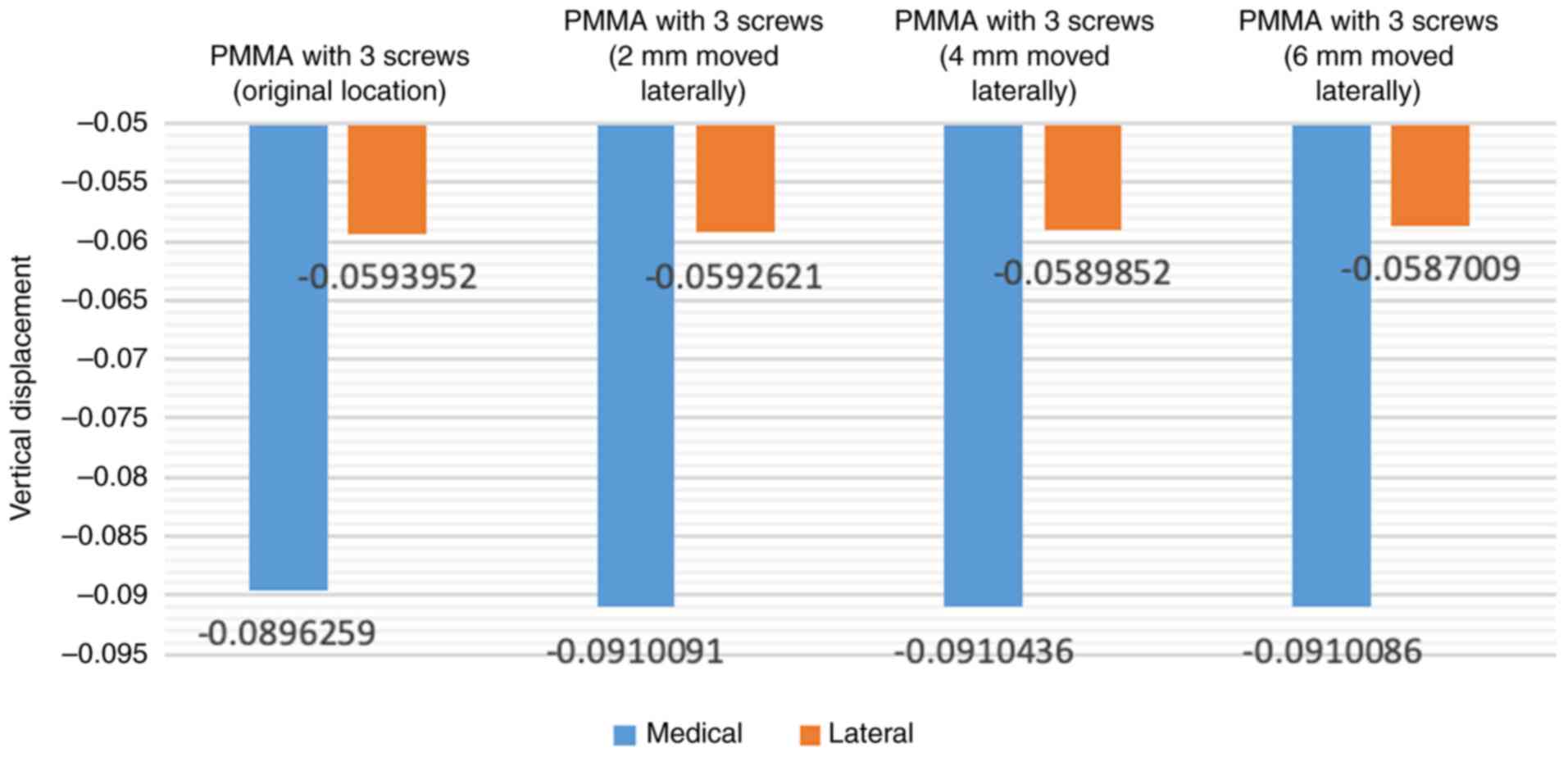
When adjusting the position of the screw laterally
to gradually approach the center of the tibial tray (2, 4 and 6 mm
laterally), there was an increase in vertical displacement values
(Fig. 5). Shifting the screws
laterally to increase the distance from the original location of
the screw to 6 mm resulted in an increase of ~1.5% in vertical
displacement values and around 6.9% in the abduction angle
(Fig. 6).
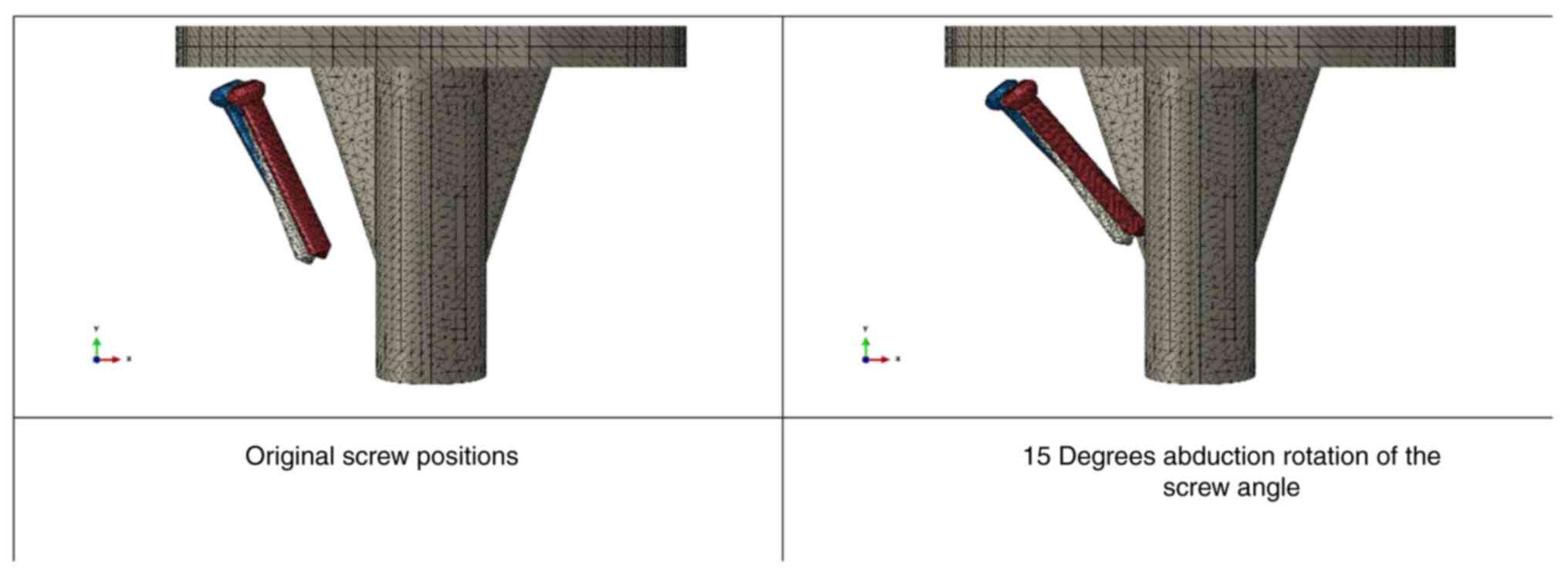
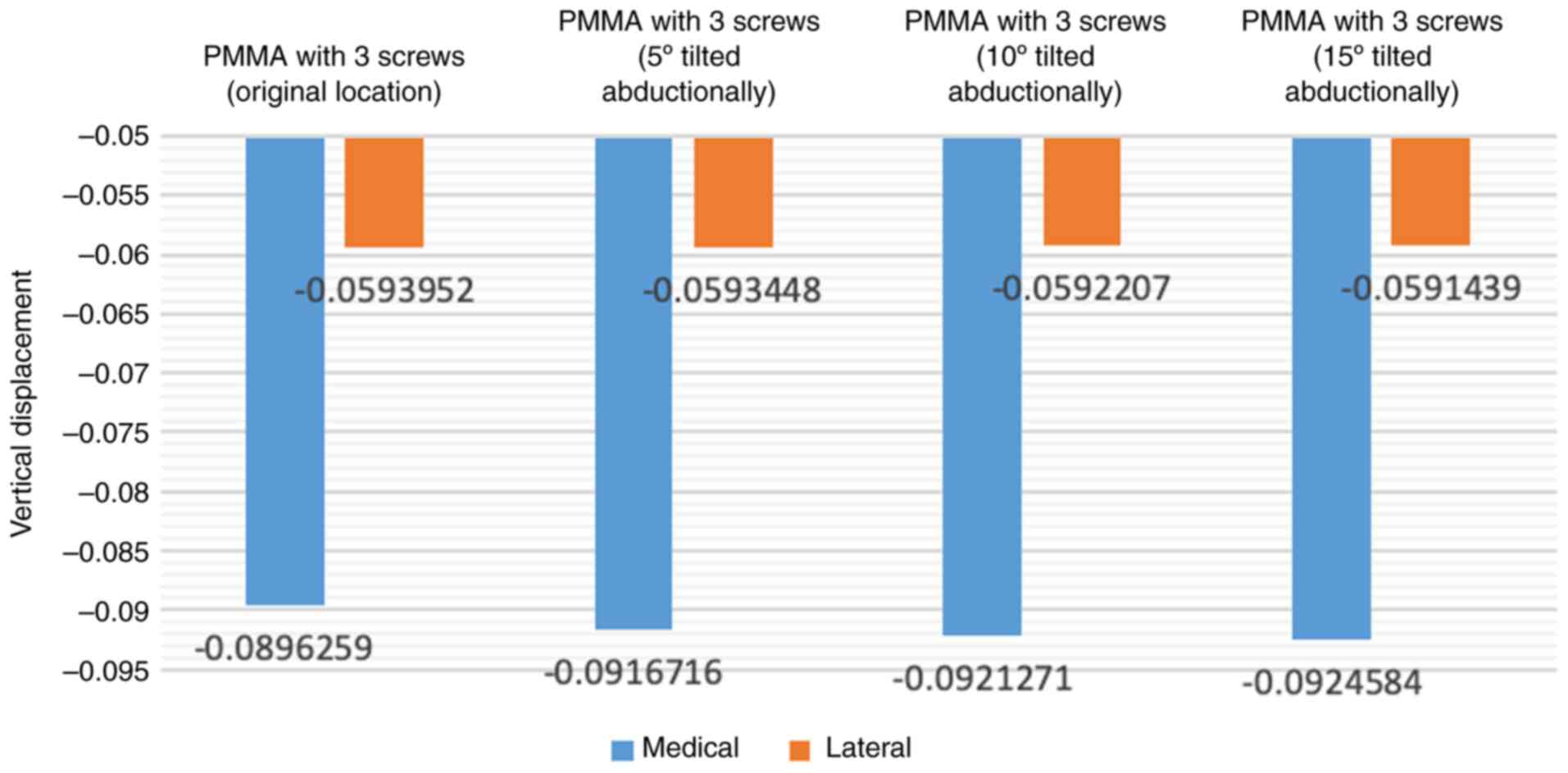
Similarly, when incrementally increasing the degree
of abduction rotation of the screw angle (5, 10 and 15 degrees),
the load-bearing performance gradually diminished (Fig. 7). Rotating the screws further in
abduction to increase the angle from the original location of the
screw to 15 degrees led to an increase of ~3.2% in vertical
displacement values and ~10.2% in the abduction angle (Fig. 8).
Discussion
Bone defects pose a significant challenge in TKA as
they affect prosthesis stability and may affect implant survival
(17,18). The combination of screws and bone
cement has been identified as an effective strategy to address this
issue, as evidenced by the successful long-term results reported by
Ritter and Harty (19). In their
study involving 125 TKA with metal-backed tibial components, screws
in cement were employed to manage medial defects caused by large
varus deformities. With an average follow-up of 7.9 years, only two
knees (1.6%) exhibited medial collapse, with no need for revision.
Özcan et al (10) also
reported positive outcomes in high body mass index patients, where
no implant failure or revision was observed during the follow-up
period. However, the existing literature lacks consensus on optimal
screw insertion techniques. The aim of the present study was to
evaluate the mechanical effects of different screw parameters,
including the number of screws, screw positioning, length and
angulation, in uncontained medial tibial defects using finite
element analysis. The results suggest that three-screw
reinforcement is preferable for larger defects, the middle position
is crucial for enhancing load-bearing capacity, longer screws are
advantageous, a smaller abduction angle is favorable and medial
placement outperforms lateral placement.
In the present study, the three-screw reinforcement
condition demonstrated the lowest displacement values, aligning
with the findings of a prior study conducted by Zheng et al
(20). Zheng et al (20) assessed the impact of the number of
screws on stresses at the surface of uncontained tibial defects
using finite element analysis and reported that in models with a
12% defect area and a 12-mm depth, the use of two screws, as
opposed to a single screw, led to a reduction in stresses on the
defect surface. Furthermore, a separate finite element study by
Zhao et al (21) revealed
that in models with an 18% defect area and a 15 mm depth, higher
bone stresses were observed with the use of one screw compared to
two screws. Despite variations in the specific metrics measured
between studies, the collective evidence emphasizes the beneficial
effects of increasing the number of screws in reinforcing tibial
defects. This augmentation may contribute to an overall improvement
in stability within the context of tibial prostheses.
The present study identified a notable reduction in
vertical displacement of the tibial tray with the use of longer
screws. This observation contrasts with the findings of a prior
orthopedic study by Ma et al (22), employing finite element analysis to
evaluate the impact of screw length in tibial defects during TKA
with a cement-screw technique. In the study by Ma et al
(22), contact stresses on the
surface of cancellous bone screws remained consistent, exhibiting
no significant difference with varying screw lengths of the same
diameter. Additionally, stresses on the tibial surface did not
exhibit notable variations based on screw length. It is suggested
that the discrepancy in outcomes may be attributed to differences
in defect size. The study by Ma et al (22) focused on smaller defects, comprising
<12% of the total plateau and with a depth of <10 mm. By
contrast, the present study specifically addressed larger defects,
constituting ~25% of the total plateau. This substantial difference
in defect size may underlie the observed variations in the
influence of different screw lengths on vertical displacement in
the present study, highlighting the clinical relevance of defect
dimensions in TKA outcomes. However, the authors still believe that
in the clinical setting, choosing longer screws may provide a
benefit without incurring additional costs or risks for the
patient. Future comparative studies evaluating different screw
lengths in clinical settings would be beneficial to further guide
optimal screw selection for patient outcomes.
The present study observed a gradual diminishment in
load-bearing performance with decreasing vertical angles of the
screw. This trend concurs with the findings of a pertinent finite
element study conducted by Zheng et al (20). In their study conducted on models
with a 12% defect area and a 12-mm depth, the researchers reported
that utilizing one vertical screw for defect reconstruction
resulted in a lower focused stress within the cancellous bone
surrounding the screws (1.05 MPa) compared to the stress observed
with one oblique screw (1.23 MPa). Additionally, a complementary
finite element study by Zhao et al (21), examining models with a 9% defect area
and an 8 mm depth, demonstrated that the use of one vertical screw
yielded significantly lower focused stress (0.45 MPa) than one
oblique screw (1.72 MPa). These consistent findings underscore the
clinical importance of screw angles in influencing focused stress
within the cancellous bone, emphasizing its significance for
optimizing load-bearing performance, as reported in orthopedic
literature.
The present study has a number of limitations that
warrant consideration. Firstly, the finite element analysis relies
on simulation, offering controlled experimentation, but potentially
deviating from the intricate in vivo conditions. Secondly,
the study specifically targeted a defect size of 25% of the total
plateau, and caution should be exercised in applying the findings
to cases with different defect dimensions. Third, the assumption of
material homogeneity may not fully capture clinical variations and
did not account for potential individual variations in bone
quality, factors that could have implications. Finally, the
analysis, centered on mechanical aspects, necessitates further
validation through experimental and clinical studies for robust
clinical translation. Acknowledging these limitations is crucial
for a nuanced interpretation of the outcomes of the study and
offers directions for future research to systematically address
these constraints.
In conclusion, the finite element analysis performed
in the present study suggested that, for the treatment of medial
uncontained tibial defects, three-screw reinforcement is
advantageous for larger defects. Longer screws and a smaller
abduction angle are deemed favorable. Moreover, the results
underscore the superiority of medial screw placement over lateral
placement. It is imperative to note that further clinical
validation is essential to corroborate the biomechanical
implications observed herein.
Acknowledgements
Not applicable.
Funding
Funding: Some of finite element analysis expenses were funded by
the Horizon Europe Framework Programme (grant no. 101086348). The
present study was supported by the Faculty of Medicine, Prince of
Songkla University, Songkhla, Thailand through a funding support
for materials and laboratory expenses in this study.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AK, KI and VY were involved in the conception and
design of the study. AK, PS and VY were involved in the acquisition
of data or the finite element analysis. AK, PS, KI and VY were
involved in the analysis and interpretation of the data. AK and VY
confirm the authenticity of all the raw data. AK, PS, KI and VY
were involved in the writing of the manuscript. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee and Institutional Review Board of the Faculty of
Medicine, Prince of Songkla University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kim SE, Ro DH, Lee MC and Cholewa JM:
Early- to mid-term review of a prospective, multi-center,
international, outcomes study of an anatomically designed implant
with posterior-stabilized bearing in total knee arthroplasty.
Medicina (Kaunas). 59(2105)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alasaad H and Ibrahim J: Primary total
knee arthroplasty in patients with a significant bone defect in the
medial tibial plateau: Case series and literature review. Int J
Surg Case Rep. 110(108779)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lei PF, Hu RY and Hu YH: Bone defects in
revision total knee arthroplasty and management. Orthop Surg.
11:15–24. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Tang Q, Guo S, Deng W and Zhou Y: Using
novel porous metal pillars for tibial bone defects in primary total
knee arthroplasty. BMC Musculoskelet Disord. 24(829)2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Brooks PJ, Walker PS and Scott RD: Tibial
component fixation in deficient tibial bone stock. Clin Orthop
Relat Res. 302–308. 1984.PubMed/NCBI
|
|
6
|
Engh GA and Ammeen DJ: Bone loss with
revision total knee arthroplasty: Defect classification and
alternatives for reconstruction. Instr Course Lect. 48:167–175.
1999.PubMed/NCBI
|
|
7
|
Cuckler JM: Bone loss in total knee
arthroplasty: Graft augment and options. J Arthroplasty. 19 (4
Suppl 1):S56–S58. 2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rand JA: Bone deficiency in total knee
arthroplasty. Use of metal wedge augmentation. Clin Orthop Relat
Res. 63–71. 1991.PubMed/NCBI
|
|
9
|
Whittaker JP, Dharmarajan R and Toms AD:
The management of bone loss in revision total knee replacement. J
Bone Joint Surg Br. 90:981–987. 2008.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Özcan Ö, Yeşil M, Yüzügüldü U and Kaya F:
Bone cement with screw augmentation technique for the management of
moderate tibial bone defects in primary knee arthroplasty patients
with high body mass index. Jt Dis Relat Surg. 32:28–34.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ritter MA: Screw and cement fixation of
large defects in total knee arthroplasty. J Arthroplasty.
1:125–129. 1986.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ritter MA, Keating EM and Faris PM: Screw
and cement fixation of large defects in total knee arthroplasty. A
sequel. J Arthroplasty. 8:63–65. 1993.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Berend ME, Ritter MA, Keating EM, Jackson
MD and Davis KE: Use of screws and cement in primary TKA with up to
20 years follow-up. J Arthroplasty. 29:1207–1210. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cinotti G, Perfetti F, Petitti P and
Giannicola G: Primary complex total knee arthroplasty with severe
varus deformity and large bone defects: Mid-term results of a
consecutive series treated with primary implants. Eur J Orthop Surg
Traumatol. 32:1045–1053. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Completo A, Rego A, Fonseca F, Ramos A,
Relvas C and Simões JA: Biomechanical evaluation of proximal tibia
behaviour with the use of femoral stems in revision TKA: An in
vitro and finite element analysis. Clin Biomech (Bristol, Avon).
25:159–165. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zhao Y, Robson Brown KA, Jin ZM and Wilcox
RK: Trabecular level analysis of bone cement augmentation: A
comparative experimental and finite element study. Ann Biomed Eng.
40:2168–2176. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Qiu YY, Yan CH, Chiu KY and Ng FY: Review
article: Treatments for bone loss in revision total knee
arthroplasty. J Orthop Surg (Hong Kong). 20:78–86. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mancuso F, Beltrame A, Colombo E, Miani E
and Bassini F: Management of metaphyseal bone loss in revision knee
arthroplasty. Acta Biomed. 88:98–111. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ritter MA and Harty LD: Medial screws and
cement: A possible mechanical augmentation in total knee
arthroplasty. J Arthroplasty. 19:587–589. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zheng C, Ma HY, Du YQ, Sun JY, Luo JW, Qu
DB and Zhou YG: Finite element assessment of the screw and cement
technique in total knee arthroplasty. Biomed Res Int.
2020(3718705)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhao G, Yao S, Ma J and Wang J: The
optimal angle of screw for using cement-screw technique to repair
tibial defect in total knee arthroplasty: A finite element
analysis. J Orthop Surg Res. 17(363)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ma J, Xu C, Zhao G, Xiao L and Wang J: The
optimal size of screw for using cement-screw technique to repair
tibial defect in total knee arthroplasty: A finite element
analysis. Heliyon. 9(e14182)2023.PubMed/NCBI View Article : Google Scholar
|