Introduction
Testicular tumors in pediatrics are rare, with an
incidence of 2 cases per 100,000 males. They represent 1-2% of all
pediatric solid tumors and present at an average age of 18 months.
They are primarily categorized as germ cell tumors (GCTs) (69%) and
non-germ cell tumors (31%). Pediatric and adult GCTs have largely
similar histological features; however, they differ in the
proportion of the subtypes that are represented. In newborns and
children, the majority of cases consist of pure yolk sac tumors and
teratomas, while seminomas and embryonal carcinomas are uncommon
(1-3).
Teratomas, the most common tumors found in infants, develop from
germ cells and can occur in the sacrococcygeal area, ovaries,
testicles, or other sites in the body (4,5). These
tumors contain endodermal, mesodermal and ectodermal germ layer
derivatives (2). According to the
Gonzalez-Crussi histopathological classification, there are three
types of teratoma: Mature teratoma (MT), immature teratoma (IT) and
malignant teratoma (6). Both mature
and immature components are benign, and their potential for
metastasis is unclear. Although these lesions exhibit a benign
histological appearance, there is a small subset of patients who
may face a potentially fatal outcome (6).
As shown by the literature, the majority of cases of
MT occur in the intraabdominal region, with only one case of IT
observed in the testis (7). The
present study reports a rare case of MT in the descended testes of
an infant. The case described herein highlights the importance of
considering intratesticular MT in the differential diagnosis and
demonstrates the role of testis-preserving surgical intervention in
managing these cases. The eligibility of the references has been
confirmed (8), and the report is
organized in line with CaReL criteria and also includes a brief
review of the literature (9).
Case report
Patient information
A 6-month-old male patient presented Smart Health
Tower (Sulaymaniyah, Iraq) with right-sided scrotal swelling, which
as noted by his parents. He had no family history of similar
medical conditions, and his previous medical and surgical histories
were all negative.
Clinical findings
A physical examination revealed a solid mass without
erythema, tenderness, or warmth. The mass was palpable,
non-reducible and indistinguishable from the right testicle. It
exhibited transillumination and demonstrated no change in size
during crying or straining. All the vital signs of the patient were
normal, and the patient was pain-free.
Diagnostic assessment
A scrotal sonography was performed and revealed a
large anechoic cystic lesion measuring 30x18 mm within the right
scrotal sac. The surrounding testicular tissue appeared stretched
and thinned, particularly at its lower pole. No septation,
calcification, or solid component was observed. The left testicle
appeared to be of normal size and shape. The serum levels of
α-fetoprotein (AFP) and β-human chorionic gonadotropin (β-HCG) were
within the normal range for his age (AFP, 24.07 IU/ml; β-HCG,
<0.100 mIU/ml).
Therapeutic intervention
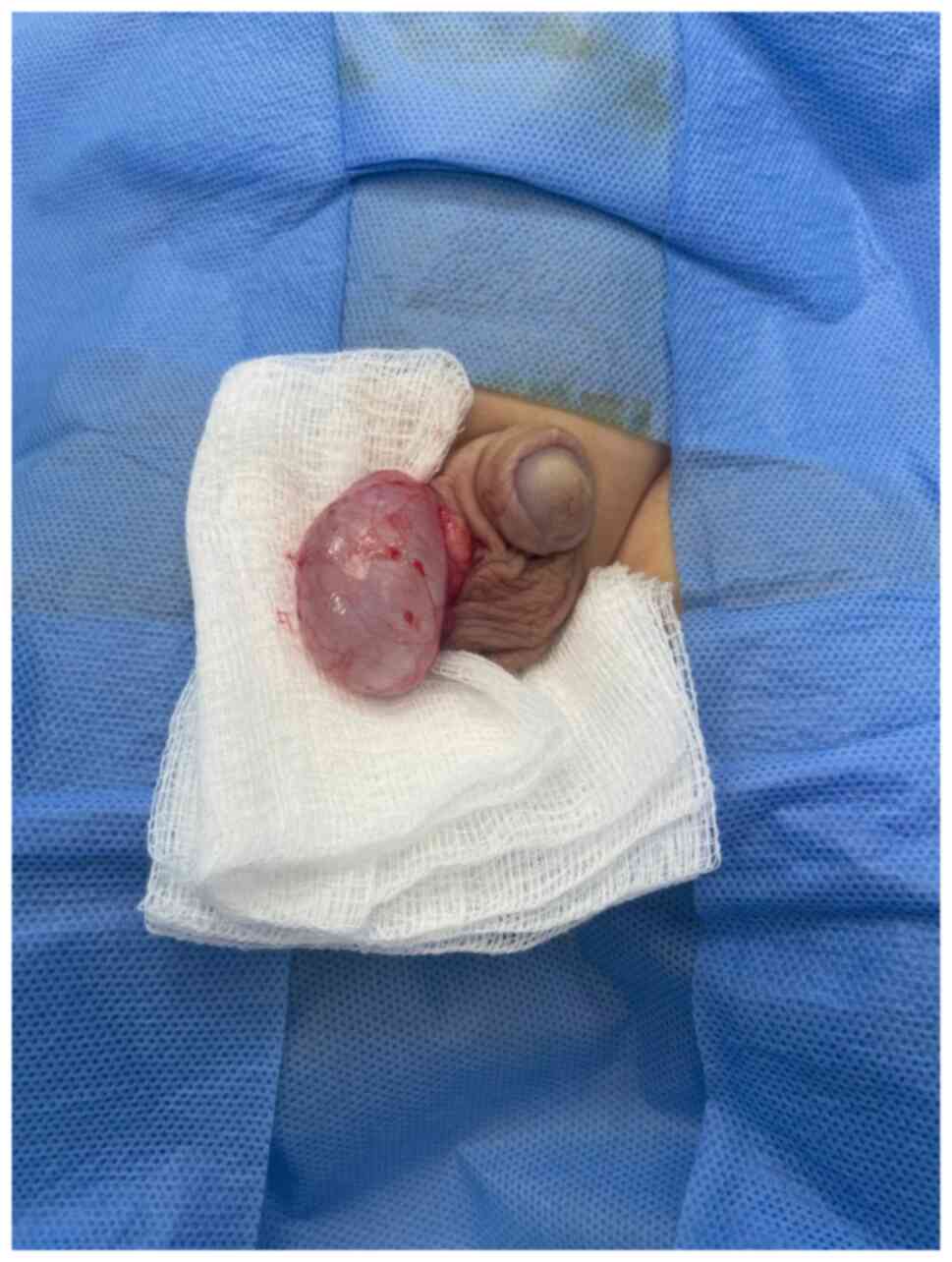
Testis-sparing tumor enucleation was performed. The
tunica albuginea was incised, and the cyst was carefully enucleated
intact without rupture (Fig. 1). The
remaining testicular parenchyma was sutured, hemostasis was
secured, and the testis was returned to its scrotal sac.
Grossly, the cyst measured 2.7x2.4x2 cm and was
unilocular with a shiny, yellow outer surface and a wall thickness
of up to 0.3 cm. It was filled with a homogeneous,
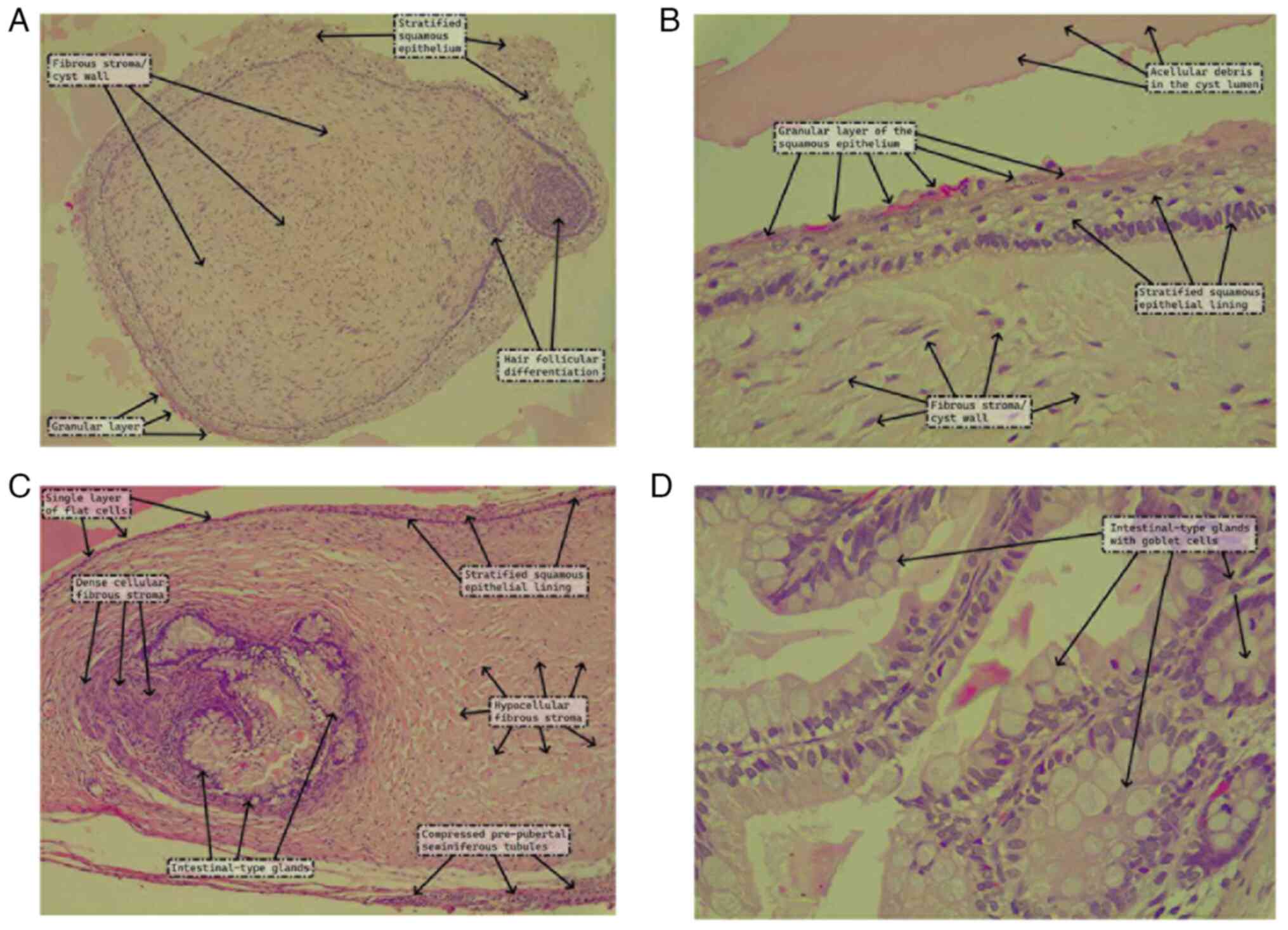
myxoid/gelatinous material. A microscopic examination was
performed. The section was 5-µm-thick and paraffin-embedded. The
section was then fixed in 10% neutral buffered formalin at room
temperature for 24 h and then stained with hematoxylin and eosin
(Bio Optica Co.) for 1-2 min at room temperature and observed under
a light microscope (Leica Microsystems GmbH). Upon the microscopic
examination, the cyst was found to have an epithelial lining that
varied from an attenuated single layer of flat cells to stratified
squamous epithelium with a patchy granular layer and focal hair
follicular differentiation. The lumen contained acellular debris,
while the underlying stroma had a fibro collagenous composition
with areas of cellular stromal condensation. There were clusters of
intestinal-type glands underneath the cyst lining that were lined
by absorptive cells (tall columnar cells with eosinophilic
cytoplasm and basal, round nuclei with fine chromatin) and numerous
goblet cells (Fig. 2). The
prepubertal, immature seminiferous tubules immediately adjacent to
the mass were compressed, but there was no germ cell neoplasia in
situ, sclerotic tubules, microlithiasis, parenchymal scars, or
necrosis. A diagnosis of prepubertal-type MT was thus rendered, and
the surgical excision was deemed adequate and sufficient.
Follow-up
The post-operative period was uneventful; the
patient recovered well and was discharged 1 day after the surgery.
At 6 to 7 weeks after the surgery, a post-operative ultrasound was
performed, which revealed a normal-sized right testis (image not
available; data not shown).
Discussion
Teratoma is a type of embryonic tumor resulting from
the improper development of embryonic cells within the primordial
germ cells, frequently occurring in primary areas such as the
sacrococcygeal and retroperitoneal regions (1,10). In
adults, malignant testicular teratoma represents ~60% of all
testicular teratomas, while in children, the majority teratomas are
of the prepubertal type which are benign (1). These tumors can manifest either as a
painful palpable mass or a painless one that is found accidentally,
as was the case in our patient (11).
According to the World Health Organization (WHO)
classification of tumors, testicular teratomas are classified into
the prepubertal-type and postpubertal-type. The prepubertal-type
teratomas are usually (although not always) observed in the
prepubertal testis, and they are characterized by various forms of
somatic tissue derived from any of the three germ layers and often
arranged in an organoid pattern and a lack of germ cell neoplasia
in situ, tubular atrophy (away from the tumor), parenchymal
scars, tubular microlithiasis, necrosis and impaired
spermatogenesis. They are diploid tumors with a lack of the
characteristic chromosome 12p gain observed in post-pubertal-type
teratomas and a lack of recurrent somatic mutations. Epidermoid
cysts (similar to epidermal inclusion cysts of the skin) and
dermoid cysts (similar to their ovarian counterparts) are
specialized subtypes of prepubertal-type teratomas that lack other
somatic elements. Prepubertal-type teratomas are benign tumors
without reports of malignant behavior. Thus, patients are treated
sufficiently with surgical excision alone, without the need for
systemic adjuvant therapy (12).
The literature review of seven case reports on MT
and IT in infants and children revealed 5 cases of MT and only 2
cases of IT, mostly arising from undescended testes within the
abdomen. The size of tumors ranged between 2 and 9 cm, with the
average age of cases being 15 months (Table I). The present study contributes
uniquely to understanding intratesticular prepubertal-type MT in
infants compared to cases reported in the literature. Previous
studies on prepubertal-type MTs typically involved larger tumors
located intra-abdominally, where interventions primarily focused on
mass removal, as demonstrated by Yam et al (11), Tanaka et al (4) and Mukai et al (10). Notably, Moritoki et al
(7) reported only one other case
involving an intratesticular location, which required orchidectomy
due to the nature of the teratoma. By contrast, the present study
documented a rare case of intratesticular MT in infant managed
successfully through testis-sparing tumor enucleation.
 | Table IReview of cases on mature teratoma and
immature teratoma in infants and children. |
Table I
Review of cases on mature teratoma and
immature teratoma in infants and children.
| Article no. | Authors, year of
publication | Age | Type of teratoma | Study design | Size (cm) | Weight | Location | Intervention | (Refs.) |
|---|
| 1 | Yam et al,
2010 | 7 Months | Mature teratoma | Case report | 7 | - | Intra-abdominal | Mass removal | (11) |
| 2 | Tanaka et al,
2009 | 2 Months | Mature teratoma | Case report | 9 | 723 g | Intra-abdominal | Mass removal | (4) |
| 3 | Pramanik et
al, 2011 | 5 Months | Mature teratoma | Case report | 4 | - | Iliac fossa | Mass removal | (14) |
| 4 | Moritoki et
al, 2019 | 7 Months | Immature
teratoma | Case report | 3 | - | Testicle | Orchidectomy | (7) |
| 5 | Doi et al,
2022 | 5 years | Mature teratoma | Case report | 4 | 30 g | Intra-abdominal | Laparotomy | (13) |
| 6 | Hasegawa et
al, 2006 | 3 Months | Immature
teratoma | Case report | 9 | 380 g | Intra-abdominal | Mass removal | (3) |
| 7 | Mukai et al,
1998 | 23 Months | Mature teratoma | Case report | 2 | - | Intra-abdominal | Mass removal | (10) |
While yolk sac tumors represent the most common form
of GCTs recognized in fully descended testes among prepubertal
males, the most common type of teratoma found in intra-abdominal
undescended testes is prepubertal-type MT (4,13). In
the present study, the prepubertal-type MT appeared in a descended
testis. Testicular prepubertal-type MT in the prepubertal age group
is typically found in children <5 years of age (11). While the average age of infants with
testicular tumors has been reported to be 15 months, the age of
presentation in infant cases with intratesticular prepubertal-type
MTs is unclear. The age at presentation in the case described
herein was 6 months. The accurate diagnosis of intratesticular
prepubertal-type MT in infants is crucial due to its rarity and the
diverse tissue types involved, and a comprehensive physical
examination is essential to differentiate it from hernias and other
testicular tissues (11). This
accuracy provides the appropriate surgical method and reduces the
risk of recurrence. According to reported cases, a precise
diagnosis leads to successful tumor enucleation and favorable
patient outcomes (1,7,10). An
ultrasound examination is essential for evaluating testicular
tumors, with evidence indicating that its sensitivity in diagnosing
testicular tumors can be as high as 96.6% (1). While an ultrasound plays a vital role,
diagnosis can be challenging and may require additional imaging
techniques such as computed tomography (CT) or magnetic resonance
imaging. A CT scan effectively detects prepubertal-type MT and can
provide a provisional diagnosis. The CT imaging features of
intra-abdominal testicular prepubertal-type MT are similar to those
observed in MTs in other regions of the body (11). A limitation of the present study was
the inability to perform a CT scan due to its high cost for the
patient's family, and the mass was identified and characterized
only through a scrotal ultrasound. Typically, prepubertal-type MT
manifests as a well-defined, rounded mass with cystic
characteristics (11). The AFP in
the serum is released by yolk sac cells during early fetal
development, as well as by the proximal small intestine and the
liver (1). Its level typically stays
elevated, and it only normalizes around the age of 9 months. In the
present case, the levels of AFP and β-HCG were normal (5,14).
Surgery has been extensively utilized to treat
benign testicular tumors in children, such as prepubertal-type MT,
including dermoid cysts. The prognosis of surgical excision of the
tumor without orchiectomy is excellent during childhood; it may not
increase the possibility of recurrence in cases of benign tumors
and is considered safe and feasible (4). Furthermore, since the testis is a vital
sexual organ in males, preserving it through surgery holds
functional, physiological, and psychological significance for
patients with testicular tumors. The only therapeutic intervention
performed in the case in the present study for prepubertal-type
mature testicular teratomas was testis-sparing tumor enucleation
surgery, which was completed without any intraoperative
complications (1,15).
The prepubertal-type MT in infants is a benign
tumor, and recurrence is uncommon. Radiologic tests are useful for
a provisional diagnosis, but they cannot reliably distinguish
benign from malignant tumors. Histopathological examination is thus
crucial for a definite diagnosis and complete characterization
(11).
In conclusion, prepubertal-type MT is a benign tumor
that is most commonly found in intra-abdominal testes; however, its
occurrence in descended testes, particularly in infants, is rare.
It may appear as a solid, non-reducible mass, exhibiting no signs
of inflammation or systemic symptoms. The present case report
highlights the unusual presentation of an intratesticular
prepubertal-type MT in an infant and demonstrates the effectiveness
of testis-sparing tumor enucleation. Early diagnosis and surgical
intervention are crucial for excellent outcomes with a favorable
prognosis and minimal risk of recurrence. Future research is
required to emphasize long-term follow-up and the development of
standardized guidelines for managing and monitoring benign
pediatric testicular tumors.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
SSF was the major contributor to the conception of
the study, as well as in the literature search for related studies.
SMA and HOA were involved in the literature review, in the writing
of the manuscript, and in the analysis and interpretation of the
patient's data. FHK, SSO, ReMA, BOM, RAK, KKM and SHM were involved
in the literature review, in the design of the study, in the
revision of the manuscript and in the processing of the figures.
RaMA was the pathologist who performed the histopathology
diagnosis. SMA and FHK confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The patient's parents provided written informed
consent to participate in the present study.
Patient consent for publication
Written informed consent was obtained from the
parents of the patient to publish any related data and any related
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Li Z, Zhang W, Song H and Sun N:
Testis-preserving tumor enucleation is applicable in children with
immature testicular teratoma. Urol Int. 105:27–30. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mingomataj E, Krasniqi M, Dedushi K,
Sergeevich KA, Kust D, Qadir AA, Abdullah AS, Ahmed MK and Fatah
GM: Cancer publications in one year (2023): A cross-sectional
study. Barw Med J. 2:3–11. 2024.
|
|
3
|
Hasegawa T, Maeda K, Kamata N and Okita Y:
A case of immature teratoma originating in intra-abdominal
undescended testis in a 3-month-old infant. Pediatr Surg Int.
22:570–572. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tanaka N, Yoneda A and Fukuzawa M: Mature
teratoma arising from an intraabdominal testis in a 2-month-old
boy: Case report and review of intraabdominal testicular tumors in
children. J Pediatr Surg. 44:E15–E18. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sabir WN, Ahmed SM, Hasan KM, Mohammed BA,
Kareem HO, Najmadden ZB, Abdalla BA, Salih RQ, Mohammed SH, Kakamad
FH and Azaldeen HA: Giant sacrococcygeal teratoma in an infant: A
case report with a literature review. Ann Med Surg (Lond).
85:5666–5669. 2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Terenziani M, D'Angelo P, Inserra A,
Boldrini R, Bisogno G, Babbo GL, Conte M, Dall' Igna P, De Pasquale
MD, Indolfi P, et al: Mature and immature teratoma: A report from
the second Italian pediatric study. Pediatr Blood Cancer.
62:1202–1208. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Moritoki Y, Mizuno K, Kato T, Hamamoto S,
Hattori H, Ito Y, Saitoh S, Yasui T and Hayashi Y: Testicular
teratoma demanded in-depth pathological exploration to rule out
malignancy: A pediatric case report. IJU Case Rep. 2:115–117.
2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
9
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RK, Evola G, Mustafa AM,
Abdullah HO, Abdalla B, et al: CaReL guidelines: A consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
10
|
Mukai M, Takamatsu H, Noguchi H and Tahara
H: Intra-abdominal testis with mature teratoma. Pediatr Surg Int.
13:204–205. 1998.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yam B, Georgiou NA, Khullar P, Coren CV
and Katz DS: Radiology-pathology conference: Mature teratoma
arising from an intra-abdominal undescended testis in a 7-month-old
infant. Clin Imaging. 34:466–471. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Amin MB: WHO classification of tumours.
Urinary and Male Genital Tumours. International Agency for Research
on Cancer, Lyon, 2022.
|
|
13
|
Doi O, Itoh F and Aoyama K: Mature
teratoma arising in intraabdominal undescended testis in an infant
with previous inguinal exploration: Case report and review of
intraabdominal testicular tumors in children. J Pediatr Surg.
37:1236–1238. 2002.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pramanik DD, Bhatnagar V, Subbarao KC,
Sharma MC, Agarwala S and Gupta AK: Antenatally detected mature
teratoma in an undescended testis. Eur J Pediatr Surg. 21:209–210.
2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Taskinen S, Fagerholm R, Aronniemi J,
Rintala R and Taskinen M: Testicular tumors in children and
adolescents. J Pediatr Urol. 4:134–137. 2008.PubMed/NCBI View Article : Google Scholar
|