Introduction
SFTs, which are known to be either localized fibrous
tumors or fibrous mesotheliomas, are rare spindle-cell neoplasms
first reported as originating in the pleura (1). Although most reported SFTs tend to
originate within the thoracic cavity, extrathoracic SFTs, which
occur in a wide range of anatomic sites, have also been reported
(2). Recent immunohistochemical and
ultrastructural studies support the mesenchymal histogenesis of SFT
(3). Most SFTs in deep soft tissue
are indolent and are found incidentally in the course of
examinations for other disorders or during medical check-ups. Some
cases are also diagnosed with hypoglycemia, due to insulin-like
growth factor II (IGF-2) secreted by the tumor cells of SFT
(4). In the present case, SFT was
found in the pelvis, with urinary retention caused by tumor
pressure on the urethra.
SFT with high cellularity, pleomorphism and
increased mitotic activity is classified as malignant SFT. However,
infiltrative features that prevent total resection significantly
affect their outcome. The outcome for patients with extrapleural
SFTs is unpredictable based on histological assessment (5). Therefore, complete resection is
essential to prolong prognosis. However, surgical resection of a
large tumor in the pelvis often injures the pelvic nerve plexus and
damages urinary and erectile functions. In this study, we attempted
complete surgical resection while preserving urinary and erectile
functions.
Case report
A 41-year-old man was referred to our hospital with
urinary retention. Abdominal ultrasound sonography (US) and
computed tomography (CT) revealed a hypervascular mass lesion,
measuring 125×95×129 mm, in the pelvis (Fig. 1). Magnetic resonance imaging (MRI)
showed a mass with low signal intensity on T1-weighted images and a
high signal intensity on T2-weighted images, as well as
mass-oppressed bladder, prostate and rectum in the retroperitoneum.
Blood biochemistry and urine examination results were in the normal
ranges, including prostate-specific antigen (PSA), α-fetoprotein
(AFP), carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9
(CA19-9). Transrectal biopsy showed SFT.
Following the diagnosis of SFT, a surgical resection
was performed using a retroperitoneal approach to prevent
peritoneal defects. During surgery, we performed an abruption
between the bladder and the peritoneum, entered the
retroperitoneum, and confirmed that the tumor was not connected to
neighboring organs such as the bladder, prostate, seminal vesicle
or rectum. A complete resection was performed, while preserving the
neural network related to urinary and erectile function, such as
the bladder branch of the pelvic nerve plexus and neurovascular
bundles (NVB). Macroscopically, the resected tumor was well
circumscribed and encapsulated, measuring 120×92×115 mm and
weighing 2,200 gr. The cut surface was grayish-white, showing
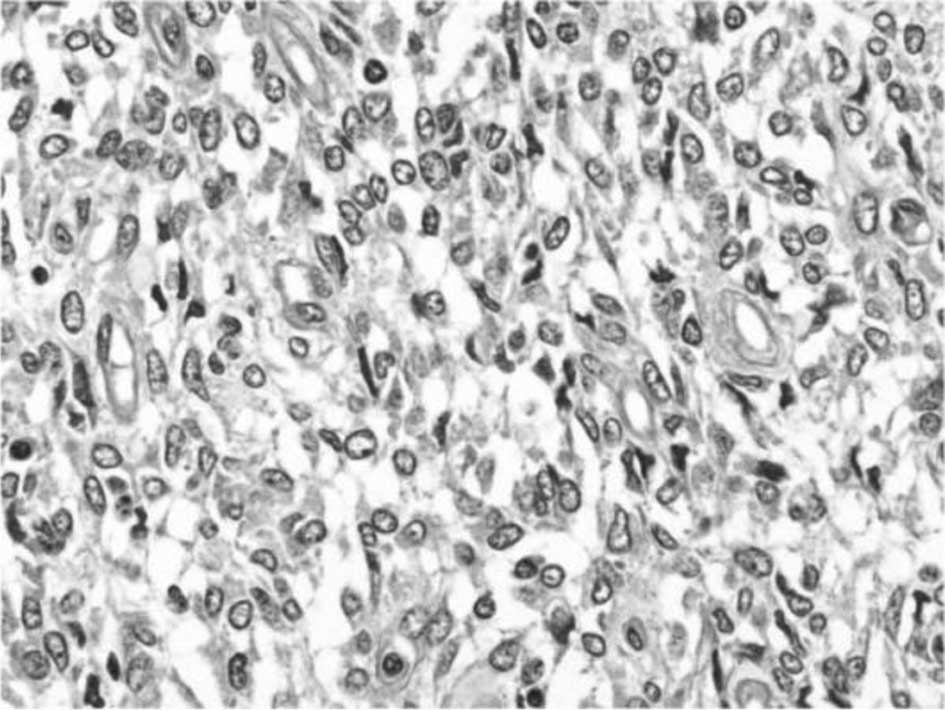
components of hemorrhaging. Microscopically, the tumor was composed
of spindle-shaped and oval cells in sarcoma, based on moderate
mitotic rate and cellularity (Fig.
2). Immunohistochemically, the tumor was positive for CD34,
CD99, vimentin, bcl-2 and p53, but was negative for keratin,
α-smooth muscle actin and S100 protein. The MIB-1 index, which
indicates cell proliferation capability, was 5%. Based on these
findings, the tumor was diagnosed to be malignant SFT in the pelvic
cavity. Prior to the operation, the scores of IPSS, QOL index,
OABSS, and IIEF-5 were 19, 6, 11 and 14, respectively. Six months
after the operation the scores had changed to 1, 0, 1 and 13,
respectively. Moreover, max flow rate, voiding time and residual
urine were 18 ml/sec, 19 sec and 35 ml. The patient showed no sign
of recurrence 12 months after surgery and required no additional
therapy.
Discussion
Since the initial description that SFT originates in
the pleura, SFTs have been reported to occur in a wide range of
anatomic sites (1,2). Among extrathoracic SFTs, primary SFT
in the pelvic cavity occurred in 16% of 79 cases of SFTs involving
various sites (2). The key symptoms
of abdominal SFTs are abdominal pain, abdominal fullness, or a
palpable abdominal mass. Hypoglycemia occurred in 4% of 360 cases
of SFTs of the pleura (6). In the
present case, no hypoglycemia was detected. The symptom of the
present case was urinary retention caused by tumor pressure on the
urethra. However, no previous cases of SFT with the symptom of
urinary retention were found in the literature. CT imaging of SFT
usually revealed a well-delineated, homogeneous, and occasionally
lobulated mass of soft tissue attenuation (7), and MRI revealed fibrous tissue of SFT
with a low signal intensity on T1-weighted images. However, mature
fibrous tissue has a low intensity, while malignant fibrous tissue
tends to exhibit a high signal intensity on T2-weighted images
(4). Although the radiological
findings in our case were typical of SFT, we performed US-guided
needle biopsy for diagnosis since cases of SFT are rare. The
pathological features of SFT were a ‘patternless pattern’
characterized by a haphazard, storiform arrangement of short
spindle or ovoid cells, and a ‘hemangiopericytoma-like appearance’
with prominent vascularity by thin-walled vessels (8).
Immunohistochemical examination of proteins, such as
CD34 and bcl-2, has been found to be helpful for diagnosing SFT
(8). In their study, England et
al reported that more than one-third of pleural SFTs are
histologically malignant, and proposed pathological criteria for
malignant SFT such as high cellularity with crowded and overlapping
nuclei and over 4 mitotic figures per 10 high-power fields.
However, the clinical features of retroperitoneal SFT are not
necessarily concordant with morphologic evaluations, and most
extrapleural SFTs in previous reports, even with malignant
histological features, showed a benign nature. Some investigators
stressed that intraoperative findings and surgical resectability
are more reliable prognostic factors based on the experience of a
small number of patients with recurrent or metastasized SFT
(9). SFTs have a low rate of local
recurrence and metastasis following surgical resection. However,
tumors larger than 10 cm or those demonstrating a histologically
malignant component have an increased risk of local recurrence and
metastasis. Complete en bloc surgical resection is the
standard therapy for SFT. We performed complete resection of the
tumor without any adhesion, and the pathological finding of margin
was negative for tumor cells in the present case. In addition,
surrounding tissue and peritoneum was not damaged when resecting
the pelvic mass, preserving the neural network connected to urinary
and erectile functions in the pelvic cavity. Urinary function
improved and erectile function remained good following the
operation. In the anatomical study, a fat layer tissue was revealed
between the peritoneum and bladder wall (Fig. 3). Consequently, we were able to
perform abruption between the bladder and peritoneum and enter the
retroperitoneum. Takizawa et al reported that
retroperitoneal SFTs required less adhesion than tumors of other
histotypes at the same location, including liposarcoma, leiomyomas,
leiomyosarcomas, malignant fibrous histiocytomas, nerve sheath
tumors, and germ cell tumors (10).
We propose that pelvic SFTs detected with no adhesion in and around
the tumor can be completely resected with ease, while preserving
the neural network connected to urinary and erectile functions in
the pelvic cavity.
References
|
1
|
Klemperer P and Rabin CB: Primary neoplasm
of the pleura: a report of five cases. Arch Pathol. 11:385–412.
1931.
|
|
2
|
Gold JS, Antonescu CR, Hajdu C, et al:
Clinicopathological correlates of solitary fibrous tumors. Cancer.
94:1057–1068. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Suster S, Nascimento AG, Miettinen M, et
al: Solitary fibrous tumors of soft tissue. A clinicopathological
and immunohistochemical study of 12 cases. Am J Surg Pathol.
19:1257–1266. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nagase T, Adachi I, Yamada T, et al:
Solitary fibrous tumor in the pelvic cavity with hypoglycemia:
report of a case. Surg Today. 35:181–184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
England DM, Hochholzer L and McCarthy MJ:
Localized benign and malignant fibrous tumors of the pleura. A
clinicopathologic review of 223 cases. Am J Surg Pathol.
13:640–658. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Briselli M, Mark EJ and Dickersin GR:
Solitary fibrosis tumors of the pleura: eight new cases and review
of 360 cases in the literature. Cancer. 47:2678–2689. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee KS, Im JG, Choe KO, Kim CJ and Lee BH:
CT findings in benign fibrous mesothelioma of the pleura. Am J
Roentgenol. 158:983–986. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yamashita S, Tochigi T, Kawamura S, et al:
Case of retroperitoneal solitary fibrous tumor. Hinyoukika Kiyo.
53:477–480. 2007.
|
|
9
|
Morimitsu Y, Nakajima M, Hisaoka M, et al:
Extrapleural solitary fibrous tumor: clinicopathologic study of 17
cases and molecular analysis of the p53 pathway. Acta Pathol
Microbiol Immunol Scand Suppl. 108:617–625. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Takizawa I, Saito T, Kitamura Y, et al:
Primary solitary fibrous tumor (SFT) in the peritoneum. Urol Oncol.
26:254–259. 2008. View Article : Google Scholar
|