Introduction
Cancer of unknown primary origin (CUP) is an
aggressive disease with a poor prognosis (1). The most frequently detected primary
carcinomas are those that are concealed in the lungs or pancreas
(2). Metastatic brain tumor is the
most common intracranial tumor, occurring in approximately 15% of
all cancer patients (3).
Additionally, in up to 10% of these patients, even after a
time-consuming and costly workup, the primary tumor tissue remains
unknown. The development of new modalities such as F-18
2′-deoxy-2fluoro-D-glucose (FDG) positron emission tomography
combined with computed tomography (PET/CT) has contributed to the
evaluation of various types of human cancer, and the benefits of
PET/CT for cancer staging are well established. FDG PET/CT detects
more metastatic sites than other modalities, and discloses the site
of the primary tumor in 20–40% of cases (2), while the usefulness of PET alone for
the detection of CUP origin is controversial (4). Pelosi et al observed that the
primary tumor site was correctly identified by FDG-PET/CT in 24 out
of 68 patients (35.3%) (5). The
above data strongly support the diagnostic contribution of
whole-body FDG-PET/CT scan in the evaluation of patients with CUP
syndrome and indicate its use in an early phase of the diagnostic
passageway to optimize patient management.
In the present study, we report a case of a
37-year-old man with an extremely rare lung cancer with a primary
lesion that had been revealed by PET/CT 1 year after the detection
of brain metastasis. This case revealed that 18F-FDG
PET/CT imaging of CUP syndrome is capable of impacting positively
on the identification of small primary tumor foci.
Patient and methods
This study was performed with the patient’s informed
consent and with the approval of the Ethics Committees of our
respective institutes (National Defense Medical College, Tokorozawa
PET Diagnostic Imaging Clinic and Tokorozawa Chuoh Hospital).
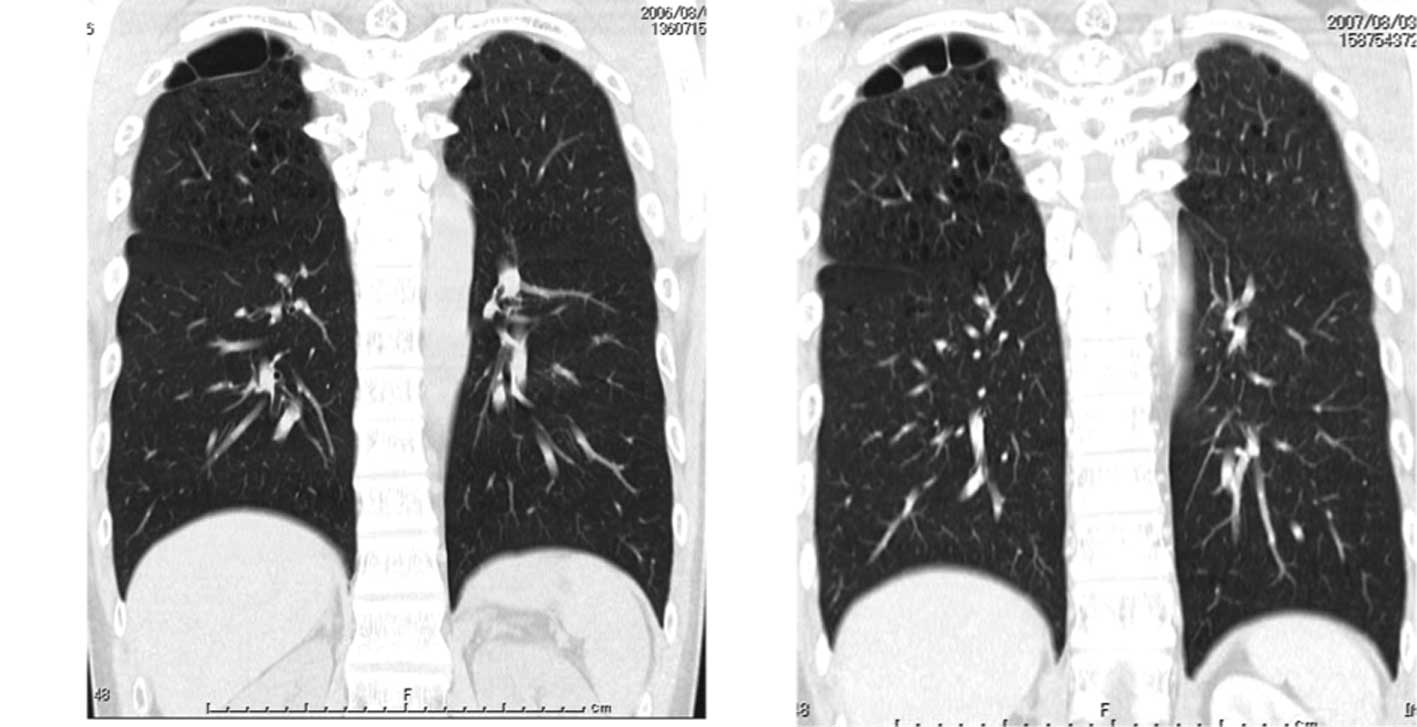
A 37-year-old man complaining of headache was
admitted to the Tokorozawa Chuoh Hospital. No abnormal findings
were revealed by physical examination. Blood analysis did not
reveal any remarkable abnormalities, including tumor markers such
as carcinoembryonic antigen (CEA) and CA19-9. The patient had been
a smoker (>30 cigarettes/day) since the age of 15 years. Brain
CT and magnetic resonance images revealed a brain tumor and surgery
was performed. Biopsy specimens indicated metastatic
undifferentiated carcinoma (Fig.
1A-B), while a systemic CT scan did not detect any
abnormalities with the exception of a right pulmonary bulla
(Fig. 2A).
The patient then underwent 18F-FDG PET/CT
scans. As described in our previous studies (6–8),
18F-FDG PET/CT scans were obtained with a Biograph Duo
(Siemens CTI) at Tokorozawa PET Diagnostic Imaging Clinic. To
determine a semi-quantitative FDG uptake, regions of interest
(ROIs) were placed over the lesion, including the highest uptake
area (circular ROI, 1 cm in diameter), and the standardized uptake
value (SUV) was calculated. PET/CT scan did not show any abnormal
FDG uptake besides the non-specific uptake in the gastrointestinal
tract (Fig. 3A). The patient was
followed up in order to diagnose CUP origin without further therapy
subsequent to resection of the brain tumor.
PET/CT showed abnormal intense FDG uptake (SUVmax:
5.09 in early scan, 5.22 in delayed scan) in the small nodular
lesion beside the bulla in the right lung 1 year after resection of
brain metastases. No other abnormal FDG uptake was observed
elsewhere in the body (Fig. 3B-E).
Right upper lobectomy and dissection of mediastinal lymph nodes
were performed at the National Defense Medical College Hospital.
The tumor in the right upper lobe measured 20 mm in diameter and
was located beside the pulmonary bulla. The microscopic findings
revealed the growth of atypical cells with abortive glandular
formation (Fig. 1C-D), and the
pathological diagnosis was poorly differentiated adenocarcinoma,
which was similar to the characteristics of the brain metastatic
lesions. No metastatic lesions were observed in the dissected lymph
nodes. PET/CT did not reveal any abnormalities 3.5 years after
thoracotomy and there were no signs of either recurrence or
systemic metastasis on any other examinations.
Discussion
Cancer of unknown primary (CUP) origin comprises a
variety of different pathologic entities with a poor overall 5-year
survival. Brain tumors are classified into primary and secondary
tumors or metastases. Findings of a retrospective cohort study that
included 63 adults with metastatic brain tumors showed lung cancer
to be the most common source (9).
Following definitive treatment of locally advanced non-small cell
lung cancer (NSCLC), the risk of developing brain metastases is
considered to be 30–50%. In their study, Hubbs et al
reported that in 975 NSCLC patients treated surgically during early
stage I–II lung cancer, the 5-year actuarial risk of developing
brain metastases was 10% (10).
Furthermore, results of the multivariate analysis revealed that
younger age, larger tumor size, lymphovascular space invasion and
hilar lymph node involvement were correlated with an increased risk
of developing brain metastases. Pimiento et al reported that
the pathologic diagnoses of 91 CUP patients included adenocarcinoma
(42.8%), undifferentiated carcinoma (34.5%), squamous cell
carcinoma (9.8%), neuroendocrine cancer (6.5%), sarcoma (3.2%), and
non-specific malignant neoplasm (3.2%) (1). Nonetheless, squamous cell and
neuroendocrine CUP are associated with a significantly more
favorable early prognosis than other malignancies. The patient in
the present study remains alive with no recurrence for 4.5 years
following brain tumor resection, while the pathology was poorly
differentiated adenocarcinoma.
The development of FDG-PET/CT has contributed to the
evaluation of human cancer staging and its benefits with regards to
cancer staging have been well established. This imaging modality
enables the otolaryngologist and radiation oncologist to treat head
and neck cancer patients more effectively and leads to appropriate
management changes (11). Pelosi
et al reported that the primary tumor site was correctly
identified by FDG-PET/CT in 24 out of 68 patients (35.3%),
including the lung (n=9), rhino/oro-pharynx (n=6), pancreas (n=5),
and other sites. (5). Salem et
al reported that occult squamous cell carcinoma of the uvula
was detected using 18F-FDG PET/CT in a case of CUP in
the head and neck (12). In this
case, the first PET/CT scan did not reveal any abnormal FDG uptake,
indicating a limitation of PET/CT with regard to the detection of
extremely small foci.
In conclusion, we have reported for the first time a
rare primary lung cancer lesion that was revealed by PET/CT 1 year
following the detection of brain metastasis. Additionally, it was
noted that F-18-FDG FDG PET/CT imaging of CUP origin is capable of
impacting positively on the identification of small primary tumor
foci.
Acknowledgements
We thank Mr. Kenji Kawai for technical
assistance.
References
|
1
|
Pimiento JM, Teso D, Malkan A, Dudrick SJ
and Palesty JA: Cancer of unknown primary origin: a decade of
experience in a community-based hospital. Am J Surg. 194:833–838.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pavlidis N, Briasoulis E, Hainsworth J and
Greco FA: Diagnostic and therapeutic management of cancer of an
unknown primary. Eur J Cancer. 39:1990–2005. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu AH, Drees JC, Wang H, VandenBerg SR,
Lal A, Henner WD and Pillai R: Gene expression profiles help
identify the tissue of origin for metastatic brain cancers. Diagn
Pathol. 26:262010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Podoloff DA: PET/CT and occult primary
tumors. J Natl Compr Canc Netw. 7:239–244. 2009.PubMed/NCBI
|
|
5
|
Pelosi E, Pennone M, Deandreis D,
Douroukas A, Mancini M and Bisi G: Role of whole body positron
emission tomography/computed tomography scan with
18F-fluorodeoxyglucose in patients with biopsy proven tumor
metastases from unknown primary site. Q J Nucl Med Mol Imaging.
50:15–22. 2006.PubMed/NCBI
|
|
6
|
Ueda S, Tsuda H, Asakawa H, Shigekawa T,
Fukatsu K, Kondo N, Yamamoto M, Hama Y, Tamura K, Ishida J, Abe Y
and Mochizuki H: Clinicopathological and prognostic relevance of
uptake level using 18F-fluorodeoxyglucose positron emission
tomography computed tomography fusion imaging (18F-FDG PET/CT) in
primary breast cancer. Jpn J Clin Oncol. 38:250–258. 2008.
View Article : Google Scholar
|
|
7
|
Abe Y, Tamura K, Sakata I, Ishida J, Mukai
M, Ohtaki M, Nakamura M and Machida K: Unique intense uptake
demonstrated by 18F-FDG positron emission tomography/computed
tomography (PET/CT) in primary pancreatic lymphoma: A case report.
Oncol Lett. 1:605–607. 2010.
|
|
8
|
Abe Y, Tamura K, Sakata I, Ishida J,
Fukuba I, Matsuoka R, Shimizu S, Murakami H and Machida K:
Usefulness of 18F-FDG positron emission tomography/computed
tomography for diagnosis of pyothorax-associated lymphoma: A report
of three cases. Oncol Lett. 1:833–836. 2010.PubMed/NCBI
|
|
9
|
Popović N and Kalacun D: Origin and
distribution of brain metastases. Med Pregl. 57:617–621.
2004.PubMed/NCBI
|
|
10
|
Hubbs JL, Boyd JA, Hollis D, Chino JP,
Saynak M and Kelsey CR: Factors associated with the development of
brain metastases: analysis of 975 patients with early stage
nonsmall cell lung cancer. Cancer. 116:5038–5046. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fleming AJ Jr and Johansen ME: The
clinician’s expectations from the use of positron emission
tomography/computed tomography scanning in untreated and treated
head and neck cancer patients. Curr Opin Otolaryngol Head Neck
Surg. 16:127–134. 2008.
|
|
12
|
Salem S, Patel NH, Barwick T, Al-Nahhas A,
Howard DJ, Zerizer I and Win Z: Occult squamous cell carcinoma of
the uvula detected by F-18 FDG PET/CT in a case of carcinoma of
unknown primary in the head and neck. Clin Nucl Med. 35:800–801.
2010. View Article : Google Scholar : PubMed/NCBI
|