Introduction
Primary paratesticular sarcoma comprises a unique
subset of intrascrotal sarcoma that is neither associated with germ
cell nor testicular elements. Primary osteosarcoma of
paratesticular soft tissue is a rare tumor, with few reports in the
literature (1–3). To the best of our knowledge, only one
case (4) arising directly from
paratesticular soft tissue has been reported. Due to the rarity of
paratesticular osteosarcoma, histogenesis, treatment and specific
survival rates are not available. In this study, we report a second
case of primary osteosarcoma of paratesticular soft tissue with a
review of the literature.
Case report
A 52-year-old man presented with painless swelling
and a palpable mass of the left scrotum, which showed a steady
enlargement over the course of a year. Physical examination
revealed a hard and non-tender mass of the left scrotum. Clinical
impression was testicular tumor and a radiological evaluation was
performed. A pelvic CT scan revealed a large paratesticular mass
with calcification and internal necrosis in the left scrotum, which
displaced the left testis inferiorly (Fig. 1). No enlargement of the lymph node
was detected. Testicular ultrasonography also revealed a
heterogeneous mass of the left scrotum. Radiological findings
suggested a paratesticular sarcoma arising from the left spermatic
cord. The patient underwent a left orchiectomy. The specimen was
14.0×5.5×5.0 cm in size, containing the left testis, spermatic cord
and a gray-tan colored mass. Serial sectioning revealed a 6.5×5.0
cm-sized mass displacing the left testis inferiorly. The mass was
well circumscribed by a thick fibrous capsule, solid and firm, and
exhibited focal necrosis and hemorrhage (Fig. 2). The testis, epididymis and
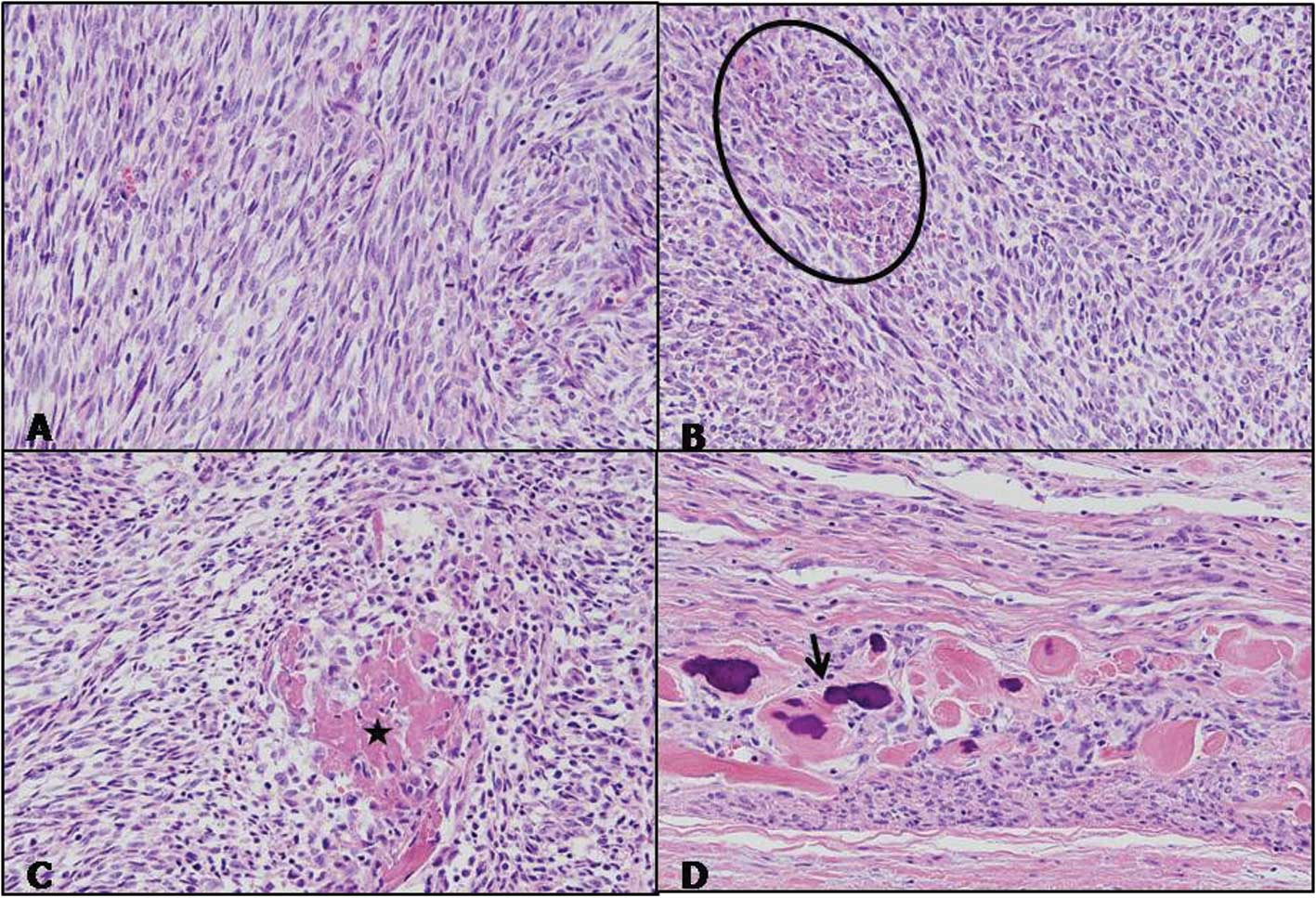
spermatic cord were intact. Microscopically, the tumor cells were
highly cellular with spindle or polyhedral cells that were
cytologically atypical and were mitotically active, frequently
demonstrating atypical mitotic figures. Portions of osteoid and
marked bony differentiation were frequently noted (Fig. 3). Immunohistochemically, the tumor
cells were reactive for vimentin, but not for smooth muscle actin,
CD34, cytokeratin, desmin, inhibin, myo-D1 and S-100 proteins. We
diagnosed this tumor as an extraosseous osteosarcoma of
paratesticular soft tissue. The postoperative course of the patient
was uneventful, and the patient has remained disease-free for 9
months. The research protocol was approved by the Ethics Committee
of Chosun University Hospital (IRB-11S-235).
Discussion
Paratesticular tumors may be clinically
indistinguishable from testicular tumors, particularly when they
are large. They usually present as a scrotal mass or swelling, with
or without pain. In certain cases, they may be clinically
misinterpreted as an inguinal hernia (4). Extraskeletal osteosarcoma is a
malignant mesenchymal neoplasm that produces osteoid, bone or
chondroid material, and is located in the soft tissue without
attachment to the skeleton. Compared with osteosarcoma of the bone,
extraskeletal osteosarcoma is rare, accounting for 1–2% of all soft
tissue sarcomas (5–7). Genitourinary sarcomas are also rare in
adults and are estimated to comprise less than 2.7% of all
sarcomas. Russo et al reported that of the 43 cases of
genitourinary sarcoma, the most common site of the tumor was
paratesticular, followed by the prostate/seminal vesicle, urinary
bladder and kidney, and that the most common histological type was
leiomyosarcoma, followed by rhabdomyosarcoma and liposarcoma
(8). Similarly, the paratestis is a
relatively common site of sarcoma; however, osteosarcoma arising
directly from paratesticular soft tissue is extremely rare. The
first reported case was that of a 52-year-old man who presented
with left scrotal swelling (4).
Histological examination of the left orchiectomy specimen revealed
a pure paratesticular osteosarcoma. Preoperative differential
diagnosis appears to be difficult and involves more common
intrascral processes, such as inguinal hernia, cord lipoma and
testicular mass. Ultrasonograghy (US), computed tomography (CT)
scan and magnetic resonance imaging (MRI) may be helpful in
defining preoperative diagnosis and the extent of the mass in the
neighboring tissue (9,10). In the present case, a pelvic CT scan
revealed a large paratesticular mass with calcification and
internal necrosis, and suggested sarcoma. When diagnosing
extraosseous osteosarcoma, careful clinical and radiological
evaluation is mandatory to exclude the possibility of a primary
osseous source for the tumor. In the present case, extensive
clinical and radiological work-up and thorough histological
examination did not reveal a skeletal lesion.
The histogenesis of testicular or paratesticular
osteo-sarcoma is unknown. However, in the case of intratesticular
osteosarcoma, two hypotheses have been suggested: i) a neoplastic
transformation of sequestered embryonic remains of osteogenic
tissue or primitive mesenchymal cells; ii) a transformation of
pre-existing teratomatous elements that acquire the potential for a
preferential mesenchymal malignancy (11,12).
Optimal local and systemic treatment of
paratesticular sarcomas remains controversial, since the
information used to guide it is based on small, retrospective
series of patients evaluated and treated in a non-uniform manner,
and typically spans a number of years. Local relapse is a
significant problem following orchiectomy, and reports have
suggested that additional local treatment with surgery or
irradiation may improve local control (11). In the case of osteosarcoma of
paratesticular spermatic cord, complete excision of the tumor with
radical inguinal orchiectomy and high ligation of the spermatic
cord was the main primary surgical procedure (1,2,12). A
more aggressive surgical policy in the management of spermatic cord
sarcomas has been proposed as primary surgery, involving wide
excision of surrounding soft tissue and re-excision in the case of
local recurrence of the disease, since of the patients without
clinically apparent disease who underwent re-excision, residual
tumor was discovered in almost one third of the cases (13). The prognosis of paratesticular
sarcomas is variable from case to case with reports describing
early metastasis and multiple recurrences, as well as long-term,
disease-free survival. The patient of the first reported
osteosarcoma arising in the paratesticular soft tissue succumbed to
the disease 6 months following the diagnosis with disseminated
disease (4). In the case of primary
pure testicular osteosarcoma, inguinal orchiectomy with strict and
careful follow-up evaluations appears to be a sufficient treatment.
However, the prognosis of testicular osteosarcoma is unclear due to
the short follow-up duration (14).
Lee et al concluded that primary pure testicular
osteosarcoma may be associated with a favorable prognosis (16).
In conclusion, we experienced an extremely rare form
of osteosarcoma arising directly from the paratesticular soft
tissue. This osteosarcoma appears to require a more aggressive
treatment strategy compared to testicular osteosarcoma, and may be
associated with poor prognosis compared to testicular
osteosarcoma.
References
|
1
|
Spirtos G, Abdu RA and Schaub CR:
Osteosarcoma of the spermatic cord. J Urol. 145:832–833.
1991.PubMed/NCBI
|
|
2
|
Beiswanger JC, Woodruff RD, Savane PD and
Assimos DG: Primary osteosarcoma of the spermatic cord with
synchronous bilateral renal cell carcinoma. Urology. 49:957–959.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stein BS, Petersen RO and Conger KB:
Malignant mesenchymoma of the spermatic cord. J Urol. 131:551–552.
1984.PubMed/NCBI
|
|
4
|
Al-Masri A, Al-Shraim M, Abu Al-Samen A,
Chetty R and Evans A: Primary paratesticular osteosarcoma: case
report and a review of the literature. Sci World J. 30:850–854.
2007. View Article : Google Scholar
|
|
5
|
Weiss SW and Goldblum JR: Enzinger and
Weiss’s Soft Tissue Tumors. 5th edition. Mosby, Inc; Maryland
Heights: pp. 1051–1053. 2008
|
|
6
|
Sordillo PP, Hajdu SI, Magill GB and
Golbey RB: Extraosseous osteogenic sarcoma: a review of 48
patients. Cancer. 51:7271983. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Klein MJ and Siegal GP: Osteosarcoma:
anatomic and histologic variants. Am J Clin Pathol. 125:5552006.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Russo P, Brady MS, Conlon K, et al: Adult
urological sarcoma. J Urol. 147:1032–1036. 1992.
|
|
9
|
Woodward PJ, Schwab C and Sesterhenn IA:
Extratesticular scrotal masses: radiologic-pathologic correlation.
Radiographics. 23:215–240. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stella M, Di Somma C, Solari N, et al:
Primary osteosarcoma of the spermatic cord: case report and
literature review. Anticancer Res. 27:1605–1608. 2007.PubMed/NCBI
|
|
11
|
Washecka RM, Mariani AJ, Zuna RE, Honda SA
and Chong CDK: Primary intratesticular sarcoma.
Immunohistochemical, ultrastructural and DNA flow cytometric study
of three cases with a review of the literature. Cancer.
44:1524–1528. 1996. View Article : Google Scholar
|
|
12
|
Tazi H, Karmouni T, Ouali M, Koutani A,
Hachimi M and Lakrissa A: Osteosarcoma of the testis. Int J Urol.
13:323–324. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Catton C, Jewett M, O’Sullivan B and
Kandel R: Paratesticular sarcoma: failure patterns after definitive
local therapy. J Urol. 161:1844–1847. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ballo MT, Zagars GK, Pisters PWT, Feig BW,
Patel SR and von Eschenbach AC: Spermatic cord sarcoma: outcome,
patterns of failure and management. J Urol. 166:1306–1310. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Coleman J, Brennan MF, Alektiar K and
Russo P: Adult spermatic cord sarcomas: management and results. Ann
Oncol. 38:635–638. 1999.
|
|
16
|
Lee JS, Choi YD and Choi C: Primary
testicular osteosarcoma with hydrocele. Virchows Arch. 445:210–213.
2004.PubMed/NCBI
|