Introduction
Pulmonary sclerosing hemangioma (PSH) is a
relatively rare neoplasm first described by Liebow and Hubbell in
1956 (1). In most patients, it is
often asymptomatic, the clinical course is benign and the prognosis
following resection is excellent (2). Biopsy is regarded as an important
diagnostic tool in PSH. Moreover, immunohistochemical staining
markedly suggests that sclerosing hemangioma originates from
primitive respiratory epithelium.
Radiological diagnosis is usually based on computed
tomography (CT) findings, typically presenting as a smooth or
slightly lobular, peripheral and solitary pulmonary nodule. To the
best of our knowledge, little is known regarding the appearance of
pulmonary sclerosing hemangioma, making it difficult to identify
this neoplasm on a 18F-fluorodeoxyglucose positron
emission tomography/computed tomography (18FDG PET/CT)
scan. An example of this rare benign neoplasm occurring in a young
adult female of Asian ethnicity is described in this study.
Case report
A 32-year-old woman was incidentally admitted to the
hospital for an abnormal nodule in the right lower lung field on
chest X-ray following an annual medical checkup. The patient was
asymptomatic and a non-smoker. The medical history, physical
examination and laboratory fndings were all normal. Serum levels of
carcinoembryonic antigen, squamous cell carcinoma antigen, cancer
antigen 125, cancer antigen 19-9 and neuron-specific antigen were
all normal. Sputum cytology was negative for malignancy.
To differentiate malignant from benign pulmonary
nodule, a whole-body 18FDG PET/CT scan was performed on
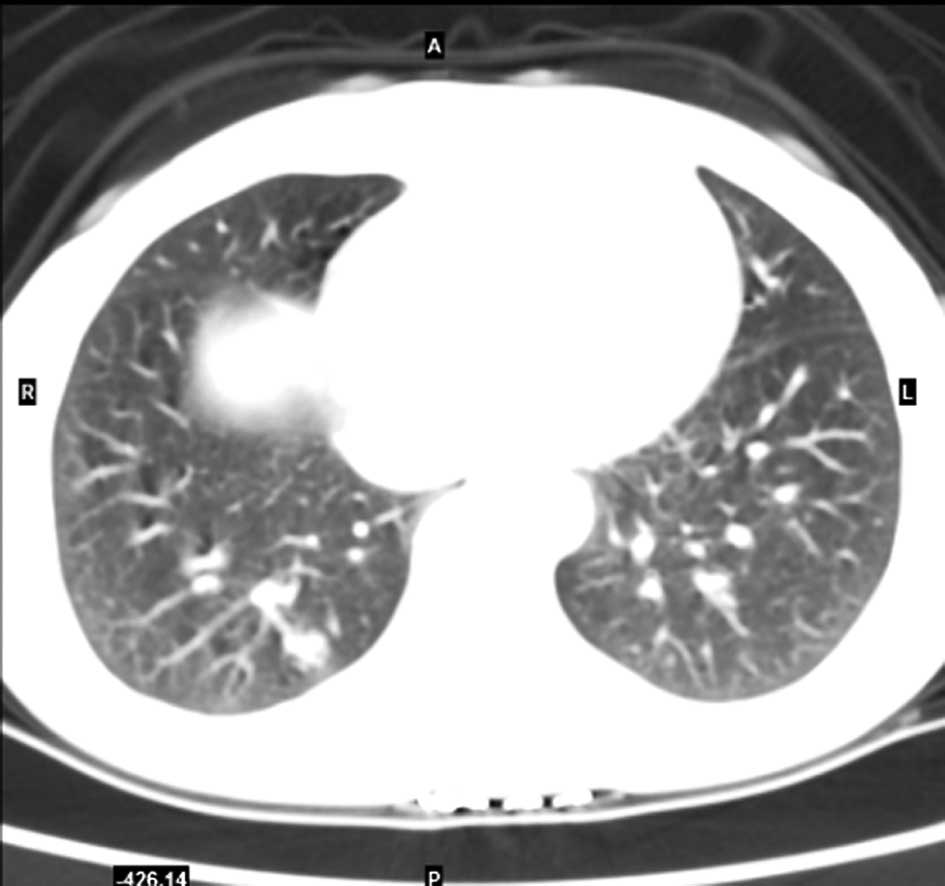
November 19, 2007. Chest CT scan revealed a 1.1 cm, solitary lesion
located in the right lower lobe. The margin appeared irregular and
slightly lobular (Fig. 1). A
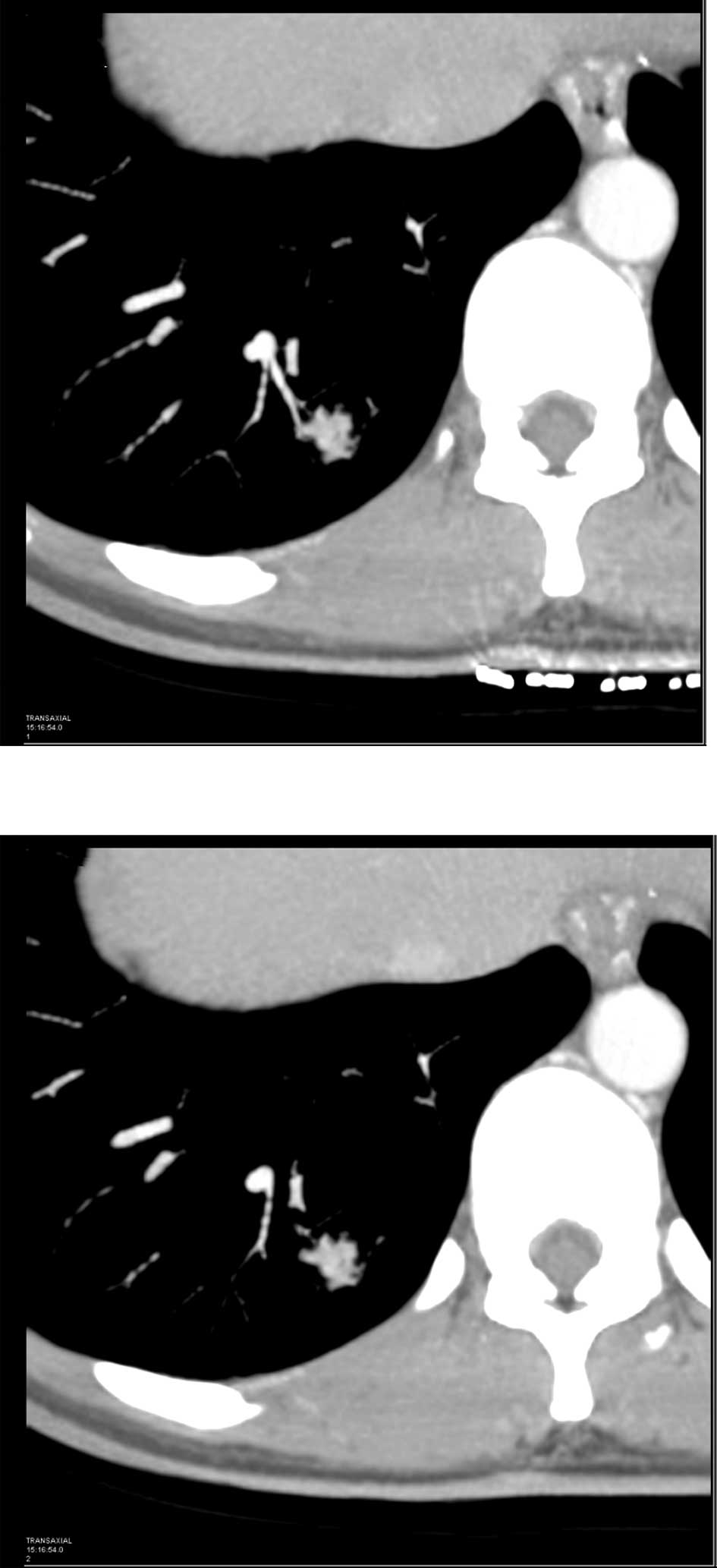
clearly lobulated nodule with heterogeneous moderate enhancement
and possible involvement of the vessel upon contrast-enhanced CT
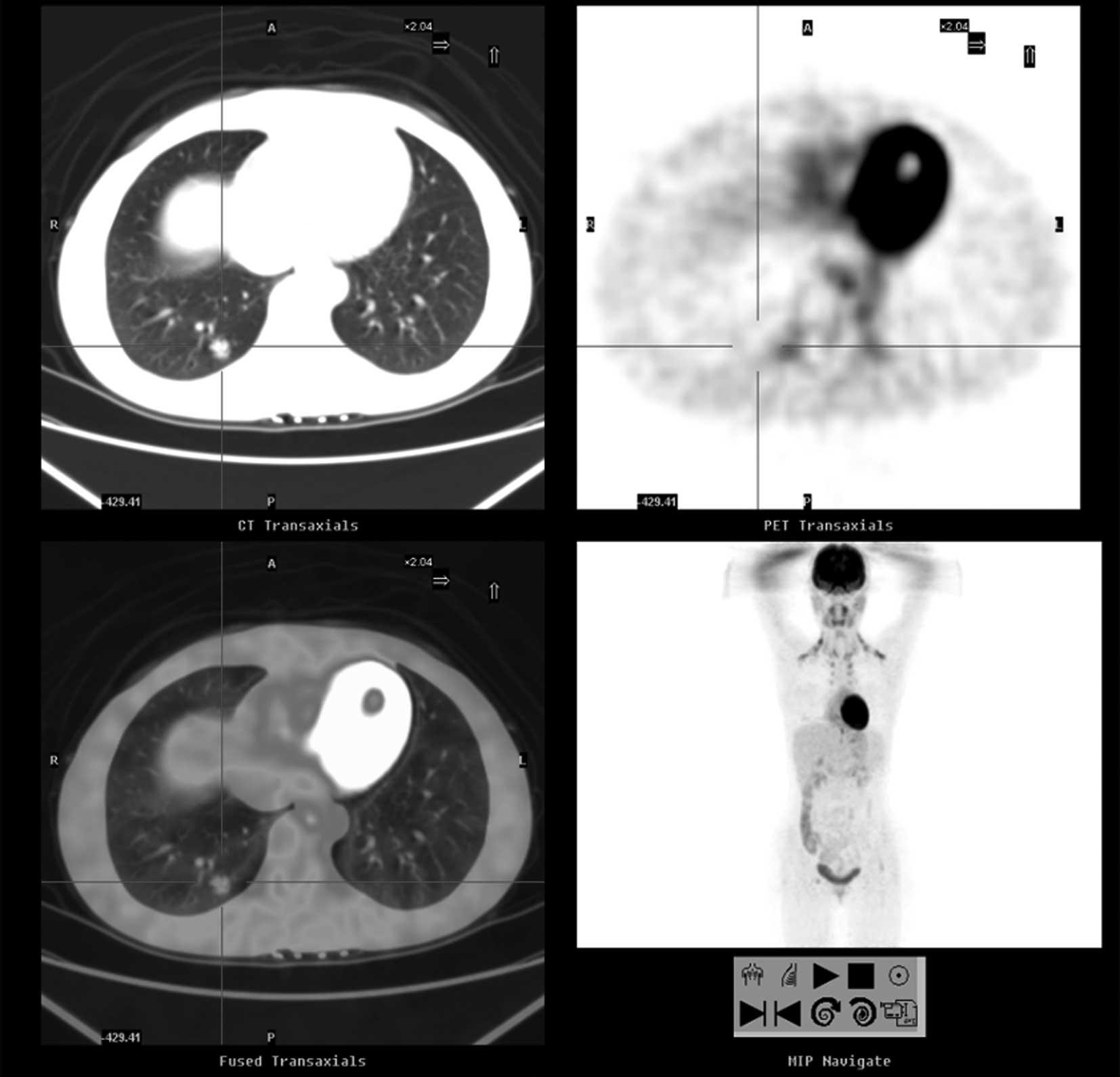
examination of the thorax was revealed (Fig. 2). It demonstrated low FDG uptake in
the right lower lobe of lung [standardized uptake value (SUV) not
shown]. No enlarged mediastinal lymph nodes, hepatic metastases or
mediastinal invasion were evident upon 18FDG PET scan
(Fig. 3).
Since the nodule is peripheral and small, the
bronchoscopic biopsy and fine needle aspiration cytology under CT
guidance was unable to be performed. Consequently, the patient
underwent an excisional lung biopsy for a definite diagnosis.
The resected specimens from the nodule were
diagnosed as sclerosing hemangioma (SH) following an intraoperative
examination of the frozen sections. Macroscopically, the tumor was
well circumscribed without invasion of the surrounding tissue.
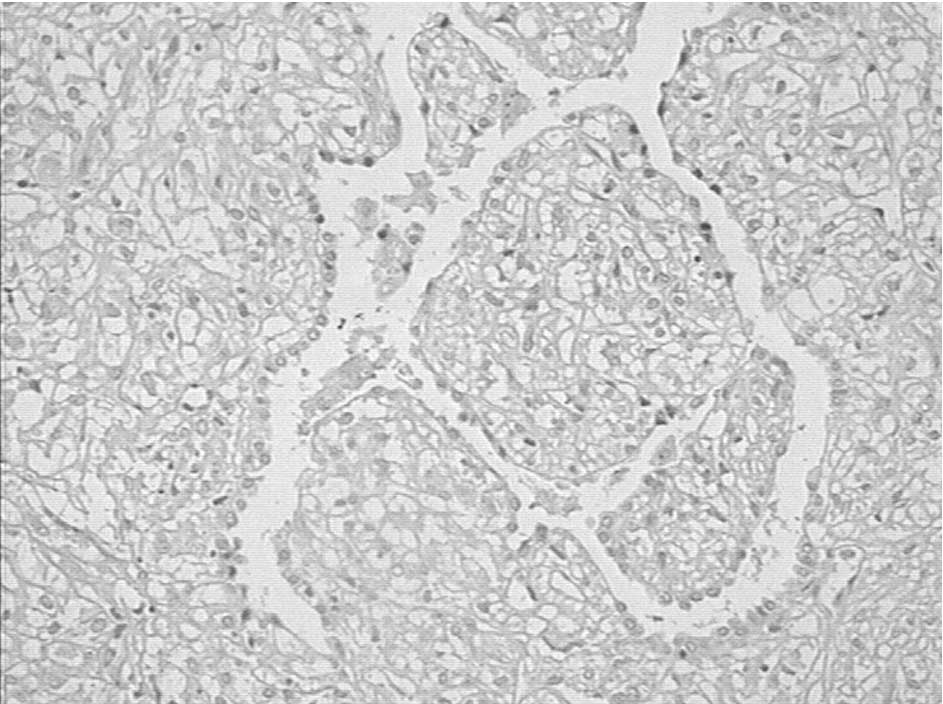
Microscopically, the tumor exhibited the typical histological
features of round stromal cells and cuboid surface cells in
papillary, sclerotic, solid and hemorrhagic patterns. The stromal
cells were small with well-defined borders, centrally located round
to oval bland nuclei and eosinophilic cytoplasm (Fig. 4). Immunohistochemical staining
revealed that the tumor cells were immunopositive for epithelial
membrane antigen, thyroid transcription factor-1 and vimentin and
cytoskeleton 7.
The patient recovered well and was discharged
following an uncomplicated postoperative course.
The study was approved by the local ethics committee
and the patient provided informed consent.
Discussion
PSH was first reported by Liebow and Hubbell in 1956
(1). PSH is predominantly
identified in middle-aged women and accounts for approximately 1%
of all benign pulmonary tumors. Most patients are asymptomatic,
with the lesion being found incidentally upon chest radiographs
performed for alternative reasons. Additionally, only a few
patients experience hemoptysis, dyspnea, cough or chest pain due to
an enlargement of the tumor and compression of surrounding tissue
(2–4).
The characteristic radiological and CT imaging
features of the PSH are reported as a solitary, well-defined, round
or oval nodule of less than 3 cm in diameter, and occasionally
exhibiting marked heterogeneous contrast enhancement and
calcification in a minority of tumors (4). However, cases involving large mass,
multiple lesions or nodal metastasis have also been reported
(5–7). In the present case, the patient was
free of symptoms and the tumor was found incidentally upon X-ray
examination. The chest CT examination revealed a solitary
heterogeneous lesion located in the right lower lobe. The margin
appeared irregular and slightly lobular. Contrast-enhanced CT
examination of the thorax revealed a clearly lobulated nodule with
heterogeneous moderate enhancement, with possible involvement of
the vessel. Furthermore, the mean size of PSH is 1.1 cm with no
calcification or fat in CT. We suspected that the lesion was
benign, but the diagnosis could not be confirmed preoperatively.
Thus, 18FDG PET/CT studies may be useful when neither
calcification nor fat are revealed on CT studies.
18FDG PET has been shown to be more
accurate than contrast-enhanced CT in differentiating malignant
from benign pulmonary nodules. Most malignant lesions have
increased uptake due to higher glycolytic activity, whereas benign
lesions are typically associated with lower uptake. However,
certain carcinoid tumor or inflammatory conditions may demonstrate
a false positive result to limit the accuracy of 18FDG
PET. The experience using 18FDG PET scans in sclerosing
hemangioma is limited. To the best of our knowledge, only a few
cases are available on 18FDG PET reported in PSH. In the
patient reported by Hara et al, only slightly elevated
uptake with an SUV of 1.8 was noted (8). In the patient reported by de Koning
et al, there was a slight amount of 18F-FDG
uptake (SUV of 1.6) (9). By
contrast, the two patients reported by Hsu et al
demonstrated SUV of 2.72 and 3.93, which were well above the
cut-off value (SUV of 2.5), suggestive of malignancy. The high FDG
uptake may be attributed to the larger tumor size and potentially
low-grade malignant nature of sclerosing hemangioma (10). The patient in the present study also
exhibited low uptake, which was preoperatively believed to most
likely represent a carcinoid on the 18FDT-PET/CT scan.
The 18FDG-PET scan features of our patient were
compatible with the pathological evaluation of PSH.
Cell proliferation is rarely identified in PSH,
suggesting a benign behavior. However, certain authors regard
sclerosing hemangioma as a potentially low-grade malignancy since
few cases of lymph node metastases and postoperative local
recurrence of PSH have been reported. The prognosis following
surgical resection is excellent, even when lymph node metastasis or
multiple lesions are present. The patient described in the present
study was also asymptomatic and had a favorable prognosis. Although
PSH is a benign condition, further careful follow-up is required
(6,11).
The pathogenesis of PSH has yet to be fully
elucidated. Previous studies have proposed various possibilities,
including mesothelial, mesenchymal, neuroendocrine and epithelial
(12). Based on immunohistochemical
and electron microscopic techniques, PSH reportedly arises from
type II pneumocyte and multipotential primitive respiratory
epithelium (13). Macroscopically,
PSH is typically well-defined, well circumscribed, encapsulated and
often hemorrhagic. Microscopically, sclerosing hemangiomas are
composed of round stromal cells and cuboid surface cells with
papillary, sclerotic, solid and hemorrhagic patterns (2). The use of immunohistochemical staining
is crucial in the diagnosis of PSH (3). It is reported that concomitant
positivity of round stromal cells and cuboidal surface cells for
epithelial membrane antigen and thyroid transcription factor-1, and
negativity of round stromal cells for cytokeratin confirm the
diagnosis of sclerosing hemangioma (2).
In conclusion, PSH is a relatively rare, benign
pulmonary neoplasm. The radiology findings are relatively
characteristic, particularly those of 18FDG PET scan.
When a benign tumor is highly suspected, observation is reasonable.
However, when the lesion has grown more rapidly than is expected
and is large and symptomatic, patients should undergo
resection.
References
|
1
|
Liebow AA and Hubbell DS: Sclerosing
hemangioma (histiocytoma, xanthoma) of the lung. Cancer. 9:53–75.
1956. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Devouassoux-Shisheboran M, Hayashi T,
Linnoila RI, Koss MN and Travis WD: A clinicopathologic study of
100 cases of pulmonary sclerosing hemangioma with
immunohistochemical studies: TTF-1 is expressed in both round and
surface cells, suggesting an origin from primitive respiratory
epithelium. Am J Surg Pathol. 24:906–916. 2000. View Article : Google Scholar
|
|
3
|
Sugio K, Yokoyama H, Kaneko S, Ishida T
and Sugimachi K: Sclerosing hemangioma of the lung: radiographic
and pathological study. Ann Thorac Surg. 53:295–300. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Iyoda A, Hiroshima K, Shiba M, et al:
Clinicopathological analysis of pulmonary sclerosing hemangioma.
Ann Thorac Surg. 78:1928–1931. 2004. View Article : Google Scholar
|
|
5
|
Komatsu T, Fukuse T, Wada H and Sakurai T:
Pulmonary sclerosing hemangioma with pulmonary metastasis. Thorac
Cardiovasc Surg. 54:348–349. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miyagawa-Hayashino A, Tazelaar HD, Langel
DJ and Colby TV: Pulmonary sclerosing hemangioma with lymph node
metastases: report of 4 cases. Arch Pathol Lab Med. 127:321–325.
2003.PubMed/NCBI
|
|
7
|
Noguchi M, Kodama T, Morinaga S, Shimosato
Y, Saito T and Tsuboi E: Multiple sclerosing hemangiomas of the
lung. Am J Surg Pathol. 10:429–435. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hara M, Iida A, Tohyama J, et al: FDG-PET
findings in sclerosing hemangioma of the lung: a case report.
Radiat Med. 19:215–218. 2001.PubMed/NCBI
|
|
9
|
De Koning DB, Drenth JP, Oyen WJ, Wagenaar
M, Aliredjo RP and Nagengast FM: Pulmonary sclerosing hemangioma
detected by fluorodeoxyglucose positron emission tomography in
familial adenomatous polyposis: report of a case. Dis Colon Rectum.
50:1987–1991. 2007.
|
|
10
|
Hsu PK, Cheng HF, Yeh YC, Wu YC and Hsu
WH: Pulmonary sclerosing haemangioma mimicking lung cancer on PET
scan. Respirology. 14:903–906. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Im JG, Kim WH, Han MC, et al: Sclerosing
hemangiomas of the lung and interlobar fissures: CT findings. J
Comput Assist Tomogr. 18:34–38. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fujiyoshi F, Ichinari N, Fukukura Y,
Sasaki M, Hiraki Y and Nakajo M: Sclerosing hemangioma of the lung:
MR findings and correlation with pathological features. J Comput
Assist Tomogr. 22:1006–1008. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang E, Lin D, Wang Y, Wu G and Yuan X:
Immunohistochemical and ultrastructural markers suggest different
origins for cuboidal and polygonal cells in pulmonary sclerosing
hemangioma. Hum Pathol. 35:503–508. 2004. View Article : Google Scholar : PubMed/NCBI
|