Introduction
Due to advances in radiation technology,
intensity-modulated radiotherapy (IMRT) has been widely applied in
cancer treatment. IMRT with inverse planning enables us to achieve
the desired dose distribution, due to its ability to provide sharp
dose gradients at the junction of the tumor and the adjacent
critical organs (1). Although it is
considered safe and effective, IMRT should be regarded with
caution; lung irradiation involves high-risk procedures, including
chemotherapy and surgery. Here, we report a case of fatal
treatment-related pneumonitis caused by postoperative IMRT in lung
cancer. The study was approved by the Ethics Xommittee of the First
People’s Hospital of Jingzhou, Jingzhou, Hubei, China. Written
informed patient consent was obtained from the patient’s
family.
Case report
A 65-year-old male patient presented with a dry
cough for one month, and a computed tomography (CT) scan revealed a
mass in the right upper lobe of the lung. The patient was referred
to the First People’s Hospital of Jingzhou (Jingzhou, China) for
detailed examination and treatment. The patient underwent a right
upper lobectomy on 6th January, 2011. The postoperative
pathological diagnosis confirmed the mass to be a squamous cell
carcinoma (pT2N2M0, stage IIIA). The lymph node metastasis was also
pathologically diagnosed as a squamous cell carcinoma.
Three weeks post-surgery, the patient received
adjuvant chemotherapy with cisplatin and vinorelbine. One week
after two complete cycles of chemotherapy, IMRT was delivered using
the Eclipse treatment planning system with a 6 MV linear
Varian-23EX accelerator (Varian Medical Systems, Inc., Palo Alto,
CA, USA).
Surgical stump, ipsilateral hilar and ipsilateral
mediastinal lymph node were delineated as the clinical target
volume (CTV). The planning target volume (PTV) was defined as the
CTV with a 6-mm margin for tumor motion and set-up uncertainty. The
contoured organs at risk (OARs), dose constraints/penalty functions
and planning parameters are listed in Tables I and II. IMRT was delivered at a dose of 50.4 Gy
(1.8 Gy/fraction).
 | Table I.Dose/volume constraints and mean dose
for sensitive structures. |
Table I.
Dose/volume constraints and mean dose
for sensitive structures.
| Structure | Importance | Max. dose constraint
(Gy) | Max. volume
constraint (%) | Mean dose (Gy) |
|---|
| Heart | 50 | 50 | 50 | 13.2 |
| Lungs | 70 | 17 | 22 | 12.6 |
| Spinal cord | 70 | 35 | 42 | 15.6 |
 | Table II.Lung planning parameters. |
Table II.
Lung planning parameters.
| Parameters | Left lung | Right lung | Both lungs |
|---|
| V30 (%) | 4.7 | 34.4 | 17.0 |
| V20 (%) | 9.6 | 52.7 | 27.5 |
| V10 (%) | 32.7 | 79.28 | 52.0 |
| V5 (%) | 64.0 | 84.5 | 72.4 |
| Mean dose (Gy) | 9.4 | 24.3 | 12.6 |
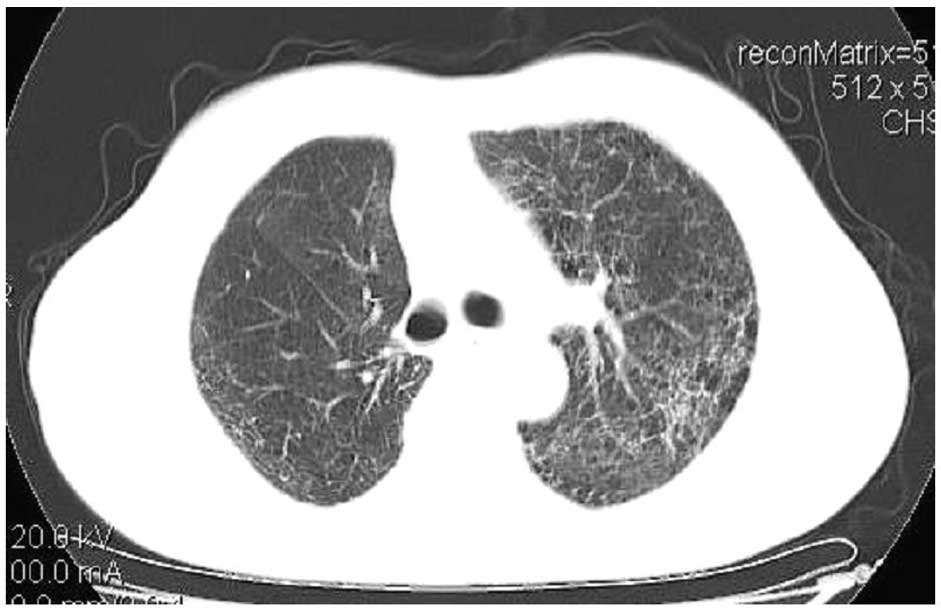
Radiotherapy was completed on 28th March. However,
the patient developed a low-grade fever, a dry cough and dyspnea on
30th March. A chest CT scan demonstrated the presence of diffuse
reticular interstitial processes and honeycombing in both lungs
(Fig. 1). An atypical infection was
suspected. The blood and sputum culture results were negative, and
the fibrotic change in both lungs in a transverse view was
compatible with low-dose irradiation of non-target OARs (Figs. 1 and 2). Acute radiation pneumonitis (RP) was
diagnosed and empirical antibiotics were injected. Steroid therapy
comprising methylprednisolone (40 mg), 20 mg iv. q8h, was
administered for inflammatory lung disease. The patient also
received supportive treatment simultaneously. However, the patient
succumbed due to respiratory failure after one week.
Discussion
RP is a common complication in radiotherapy and is
the most significant treatment-related toxicity in lung cancer. The
symptoms of treatment-related pneumonitis (TRP) are a dry cough, a
low-grade fever, chest pain and shortness of breath. Such clinical
symptoms of RP may lead to a poor quality of life for lung cancer
patients and even induce fatality. The MD Anderson experience
demonstrated that the rates of grade ≥3 maximum treatment-related
pneumonitis (TRP max) were 11 and 14% at 6 and 12 months,
respectively. IMRT has been observed to offer TRP rates that are
comparable with those achieved by three-dimensional conformal
radiotherapy (3D-CRT) (2).
The majority of DVH parameters have been
demonstrated to be associated with the occurrence of RP (14). The incidence and grade of RP have
been revealed to be significantly correlated with the V20 value
(percentage of both lungs receiving >20 Gy, not including the
gross tumor volume) and mean lung dose (MLD) (3). Thus, the V20 value is hypothesized to
be a factor that may be used for predicting RP after concurrent
chemoradiation for lung cancer. Kong et al(4) demonstrated that the V20 value should
be <35% in 3D-CRT. Belderbos et al(5) revealed that the overall treatment time
is safe for small-volume lung tumors with an MLD ≤13.6 Gy. In the
present case, the V20 value was 27.5% and the MLD was 12.6 Gy; both
of which are lower than the recommended value. However, the V5
value (72.4%) was higher than the recommended value. Therefore, it
is possible that the low-dose irradiated volume induced the fatal
pneumonitis.
IMRT delivered in a static mode produces homogeneous
dose distributions in the target. However, Murshed et
al(6) demonstrated that when
dynamic multi-leaf collimator (MLC) sequencing was selected, the
increased volume of lung irradiated at 5 Gy was observed to be a
potential problem when IMRT was applied in the lung region. In a
study by Yorke et al(7), the
V5, V10 and V13 values for total and ipsilateral lung were more
strongly correlated than the lung figures currently used in
clinical anlaysis (total lung V20, mean dose, effective uniform
dose, normal tissue complication probability and fraction of
damaged subunits). The MD Anderson experience (2,8) also
revealed that the V10 and V20 values of the normal lung decreased
by a median of 7 and 10%, respectively, with IMRT. However, the V5
value of thoracic tissue increased with IMRT, and rV5 was the only
factor to be significantly correlated with lung toxicity.
Postoperative radiotherapy is capable of
significantly improving the survival of patients with resected
pathological stage IIIA-N2 non-small cell lung cancer (NSCLC)
(9). For patients receiving
postoperative radiotherapy, the appropriate dose limits are not yet
clear. Ji et al(10)
demonstrated that >340 cm3 of the ipsilateral lung
receiving 30 Gy was significantly correlated with the risk of RP in
patients undergoing a lobectomy. It was considered safe for
patients who undergo a pneumonectomy to receive postoperative
3D-CRT, provided that the lung V20 value was <10%.
IMRT planning is dependent on the treatment-planning
systems (TPSs) and MLC, while data in low-dose regions is often
ignored. Jang et al(11)
found that in the commercial TPS-generated IMRT plans, dose
calculation errors primarily occurred in the low-dose regions of
IMRT plans (<50% of the radiation dose prescribed for the
tumor). These errors were identified to be caused by inadequate
modeling of the MLC transmission and leaf scatter in commercial
TPSs.
In addition, there are different views concerning
concurrent or sequential chemoradiotherapy-related RP. Shi et
al(12) demonstrated that
thoracic concurrent chemoradiotherapy should be planned with
caution with IMRT when the volume of normal lung receiving ≥10 Gy
is large. A study by Vogelius et al(13) demonstrated that for radiotherapy
alone, the critical volume model predicts that the two IMRT plans
(TPS and MLC) are associated with a lower risk of radiation
pneumonitis than the 3D-CRT plan. However, when the chemotherapy
equivalent radiation dose exceeds a certain threshold, the
radiation pneumonitis risk following IMRT is greater than that
which follows 3D-CRT. The threshold dose is within the range
estimated from clinical chemoradiotherapy data sets (13).
Treatment of lung cancer remains a significant
challenge for modern medicine. It is essential to evaluate the DVH
of critical structures and to limit the doses to lungs. The curve
composed of multiple DVH parameters was demonstrated to be more
important than any single DVH parameter (14). For patients receiving postoperative
IMRT, low-dose irradiation volumes should be considered for lungs,
as well as strict DVH parameters.
References
|
1.
|
Kataria T, Rawat S, Sinha SN, Garg C,
Bhalla NK and Negi PS: Dose reduction to normal tissues as compared
to the gross tumor by using intensity modulated radiotherapy in
thoracic malignancies. Radiat Oncol. 1:312006. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Jiang ZQ, Yang K, Komaki R, Wei X, Tucker
SL, Zhuang Y, Martel MK, Vedam S, Balter P, Zhu G, Gomez D, et al:
Long-term clinical outcome of intensity-modulated radiotherapy for
inoperable non-small-cell lung cancer: the MD Anderson experience.
Int J Radiat Oncol Biol Phys. 11:1–8. 2011.PubMed/NCBI
|
|
3.
|
Tsujino K, Hirota S, Endo M, Obayashi K,
Kotani Y, Satouchi M, Kado T and Takada Y: Predictive value of
dose-volume histogram parameters for predicting radiation
pneumonitis after concurrent chemoradiation for lung cancer. Int J
Radiat Oncol Biol Phys. 55:110–115. 2003.
|
|
4.
|
Kong FM, Ritter T, Quint DJ, Senan S,
Gaspar LE, Komaki RU, Hurkmans CW, Timmerman R, Bezjak A, Bradley
JD, Movsas B, et al: Consideration of dose limits for organs at
risk of thoracic radiotherapy: atlas for lung, proximal bronchial
tree, esophagus, spinal cord, ribs, and brachial plexus. Int J
Radiat Oncol Biol Phys. 81:1442–1457. 2011. View Article : Google Scholar
|
|
5.
|
Belderbos JS, Heemsbergen WD, De Jaeger K,
Baas P and Lebesque JV: Final results of a Phase I/II dose
escalation trial in non-small cell lung cancer using
three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol
Phys. 66:126–134. 2006. View Article : Google Scholar
|
|
6.
|
Murshed H, Liu HH, Liao Z, Barker JL, Wang
X, Tucker SL, Chandra A, Guerrero T, Stevens C, Chang JY, Jeter M,
et al: Dose and volume reduction for normal lung using
intensity-modulated radiotherapy for advanced-stage non-small-cell
lung cancer. Int J Radiat Oncol Biol Phys. 58:1258–1267.
2004.PubMed/NCBI
|
|
7.
|
Yorke ED, Jackson A, Rosenzweig KE, Braban
L, Leibel SA and Ling CC: Correlation of dosimetrie factors and
radiation pneumonitis for non-small cell lung cancer patients in a
recently completed dose escalation study. Int J Radiat Oncol Biol
Phys. 63:672–682. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Wang S, Liao Z, Wei X, Liu HH, Tucker SL,
Hu CS, Mohan R, Cox JD and Komaki R: Analysis of clinical and
dosimetric factors associated with treatment-related pneumonitis
(TRP) in patients with non-small cell lung cancer (NSCLC) treated
with concurrent chemotherapy and three-dimensional conformal
radiotherapy (3D-CRT). Int J Radiat Oncol Biol Phys. 66:1399–1407.
2006. View Article : Google Scholar
|
|
9.
|
Dai H, Hui Z, Ji W, Liang J, Lu J, Ou G,
Zhou Z, Feng Q, Xiao Z, Chen D, Zhang H, et al: Postoperative
radiotherapy for resected pathological stage IIIA-N2 non-small cell
lung cancer: a retrospective study of 221 cases from a single
institution. Oncologist. 16:641–650. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Ji W, Wang LH, Ou GF, Hang J, Feng QF,
Chen DF, Zhou ZM, Zhang HX, Xiao ZF and Yin WB: Risk factors for
radiation pneumonitis in patients with non-small-cell lung cancer
treated with postoperative three-dimensional conformal
radiotherapy. Chin J Radiat Oncol. 18:274–277. 2009.
|
|
11.
|
Jang SY, Liu HH and Mohan R:
Underestimation of low-dose radiation in treatment planning of
intensity-modulated radio-therapy. Int J Radiat Oncol Biol Phys.
71:1537–1546. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Shi A, Zhu G, Wu H, Yu R, Li F and Xu B:
Analysis of clinical and dosimetric factors associated with severe
acute radiation pneumonitis in patients with locally advanced
non-small cell lung cancer treated with concurrent chemotherapy and
intensity-modulated radiotherapy. Radiat Oncol. 5:352010.
View Article : Google Scholar
|
|
13.
|
Vogelius IS, Westerly DC, Cannon GM,
Mackie TR, Mehta MP, Sugie C and Bentzen SM: Intensity-modulated
radiotherapy might increase pneumonitis risk relative to
three-dimensional conformal radiotherapy in patients receiving
combined chemo-therapy and radiotherapy: a modeling study of dose
dumping. Int J Radiat Oncol Biol Phys. 80:893–899. 2011. View Article : Google Scholar
|
|
14.
|
Dang J, Li G, Lu X, Yao L, Zhang S and Yu
Z: Analysis of related factors associated with radiation
pneumonitis in patients with locally advanced non-small-cell lung
cancer treated with three-dimensional conformal radiotherapy. J
Cancer Res Clin Oncol. 136:1169–1178. 2010. View Article : Google Scholar : PubMed/NCBI
|