Introduction
Thyroid cancer is one of the 10 most common
malignancies in populations worldwide (1,2).
Epidemiological data from the USA have demonstrated a 2.4-fold
increase in the occurrence of this disease between 1973 and 2002
(3). No global agreement has been
reached for thyroid cancer treatment, predominantly due to the fact
that it is a long-standing disease with a good prognosis in the
majority of patients. A lack of prospective data has meant that
practice guidelines are based on large retrospective series and
expert opinions. Various authoritative guidelines have been
established (4), and these have
large differences mainly concerning the extent of thyroidectomy,
the extent of lymphadenectomy (central compartment, lateral neck
and superior mediastinum) and the post-operative treatment to be
performed. The debate regarding the extent of the thyroidectomy to
be performed in well-differentiated thyroid cancer focuses on total
compared with less than total thyroidectomy, and there continues to
be considerable controversy related to unilateral compared with
bilateral central compartment dissection (5). The guidelines are dependent on the
surgical center, the approach taken by the individual surgeons, the
economic situation and the quality of the medical supplies.
Recently, the focus of surgical treatment has shifted from
increasing the survival rate to decreasing the recurrence rate and
improving the quality of life in the treatment of patients with
papillary thyroid cancer (PTC) (6)
This is due to the excellent prognosis of the disease, which causes
operative modalities of thyroid cancer to be more complex.
China has a large area and population size; the
number of thyroid cancer patients is extremely high, while the
treatment methods vary due to the great disparity in the level of
medical care available in different areas, implicating that
numerous patients receive an insufficient level of surgery. In
China, surgeons managing thyroid cancer include head and neck
surgeons, general surgeons and otorhinolaryngologists. Head and
neck surgeons in cancer hospitals have received specialized
training and are able to perform a standardized thyroidectomy and
neck dissection, with the aim of increasing the survival rate,
decreasing the recurrence rate and improving the quality of life of
thyroid cancer patients. However, the number of thyroid cancer
patients treated by head and neck surgeons is limited due to the
fact that there are <400 head and neck surgeons in China.
Although there are numerous general surgeons in general hospitals
in all medical institutions throughout the country, general
surgeons are typically not so experienced at managing the recurrent
laryngeal nerve, the parathyroid gland and neck dissection, which
may lead to tumor tissue being left behind. Addtionally,
otorhinolaryngologists have only begun treating thyroid cancer in
the past few years; clinical capacity and experience are yet to be
accumulated. Radical guidelines in China may lead to further
complications and affect the patients’ quality of life. More than
80% of PTC patients belong to the low risk group, accompanied by
controversial treatment of thyroidectomy and central compartment
dissection. However, there is a great disparity of medical levels
in different areas in China. In this study, we represent our
characteristical experience of minimally accepted surgical regimen
for PTC treatment based on our own experience of salvage surgery on
patients with residual tumor and limited surgery efficiency.
Materials and methods
Patients and inclusion criteria
Between January 2006 and December 2009, a total of
117 patients diagnosed with papillary thyroid cancer where the
tumor was located in one lobe, underwent insufficient primary
thyroid surgery that was less extensive than hemithyroidectomy at
other institutions. This study was conducted in accordance with the
declaration of Helsinki and with approval from the Ethics Committee
of Beijing Cancer Hospital and Institute. Written informed consent
was obtained from all participants. Patients were suspected to have
residual tumor tissue in the ipsilateral thyroid lobe and/or
metastasis in the ipsilateral central neck by imaging findings
including computed tomography (CT) and high-resolution neck
ultrasound examination. The characteristics of patients prior to
undergoing completion lobectomy are listed in Table I. The cohort comprised 94 females
and 23 males whose median age was 39.3 years and ranged from 16 to
72 years. Thirty-two patients had undergone prior resection of the
tumor alone, 46 had undergone prior partial thyroidectomy and 39
had undergone prior subtotal thyroidectomy. No neck dissection was
performed. Hoarseness occurred in 17 cases following the initial
surgery and vocal cord paralysis was confirmed by fiberoptic
laryngoscopy. Reoperations were scheduled a median of 1.2 months
(range, 3 days–6.5 months) after primary surgery for PTC. All
available clinical, pathological, surgical and diagnostic imaging
data were reviewed for accurate staging. Patients undergoing
completion operation for PTC were required to meet the following
criteria: i) primary tumor size <4 cm; ii) solitary tumor
located in one lobe; iii) no palpable or radiological lateral neck
lymph node metastases; iv) normal contralateral lobe by ultrasound;
v) no distant metastases and vi) no massive extrathyroidal
invasion.
 | Table ICharacteristics of patients prior to
completion surgery. |
Table I
Characteristics of patients prior to
completion surgery.
| Characteristics | No. (%) |
|---|
| Gender | |
| Female | 94 (80) |
| Male | 23 (20) |
| Initial surgery | |
| Tumor
resection | 32 (27) |
| Partial
thyroidectomy | 46 (39) |
| Subtotal
thyroidectomy | 39 (34) |
| Lymph node
dissection | |
| Compartment VI | 0 (0) |
| Other
compartment | 0 (0) |
| Complications | |
| Recurrent laryngeal
nerve damage | 17 (15) |
|
Hypoparathyroidism | 0 (0) |
| TNM stage at initial
surgery | |
| T1 | 43 (37) |
| T2 | 74 (63) |
| N0 | 0 (0) |
| N1 | 0 (0) |
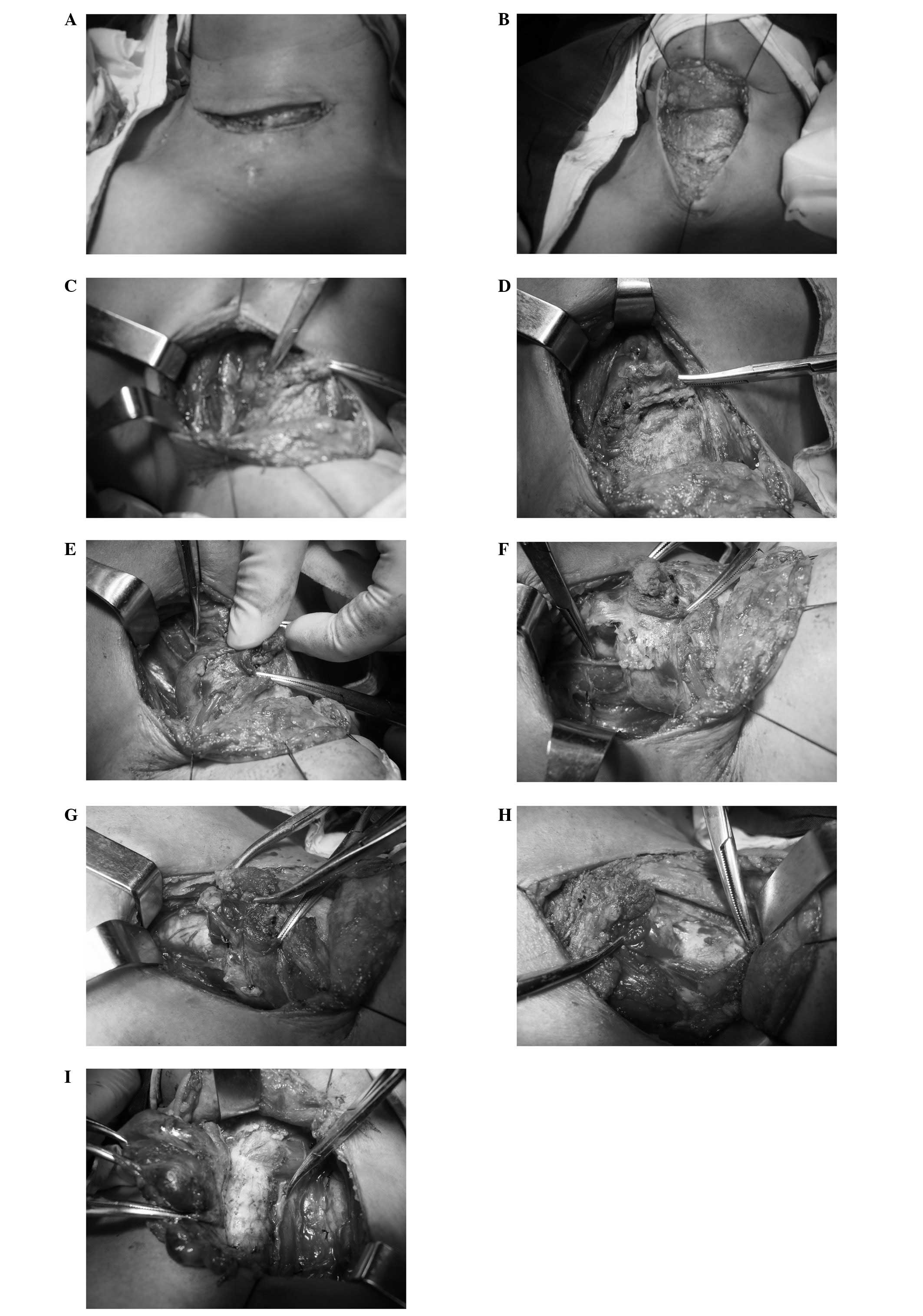
Surgical contents
The extent of surgical resection included the
residual affected lobe, the ithmus, the ipsilateral strap muscle
adhering to the former surgical area (mainly the sternothyroid
muscle and part of the sternohyoid muscle) and ipsilateral
compartment VI (the prelaryn geal, pretracheal and paratracheal
lymph nodes).
Surgical approach
A low collar incision was made on the previous
incision, with excision of the previous scar and extension into the
lower neck creases to the anterior margin of the
sternocleidomastoid muscle. A subplatysmal dissection was elevated
superiorly and inferiorly, elevating the neck flaps. The inferior
neck flap was elevated well below the sternal notch. The infrahyoid
strap musculature was cut off at the levels of the cricoid
cartilage, superiorly and the sternal notch, inferiorly. The
carotid artery was dissected from the level of the thyroid
cartilage down to the clavicle. The recurrent laryngeal nerves were
identified in areas previously lacking or with minimal dissection,
thus the laryngeal nerves were identified most inferiorly in the
tracheoesophageal groove. The nerves were meticulously
microdissected from the clavicle to the scar area. The nerves were
pulled outwards, and the lymph nodes and adipose tissue in the
tracheoesophageal groove were dissected to connect with the
residual lobe. Pretracheal tissues were also dissected to connect
with the residual lobe. Finally, the nerves in the scar tissue
regions were dissected into their laryngeal inlet, and the
frequently arborized laryngeal branches were identified and
completely spared. The lymphatic fatty tissues in compartment VI
and around the lobe, the ipsilateral residual lobe and the
ipsilateral strap muscle were cleared away according to the
continuous en bloc principle (Fig. 1). When the parathyroid tissue was
identified to be distinct from the resected tissue, it was
immediately finely minced and then the frozen section was
pathologically confirmed. Parathyroid glands confirmed by
pathological analysis were considered for autotransplantation into
the sternocleidomastoid muscle.
Results
Overall tumor residue
Among the 117 patients, pathological analysis
confirmed the presence of residual tumor in 60 patients, with a
residual rate of 51.28%. Among these 60 patients, 18 had residual
tumor in the thyroid bed alone, while 28 had residual tumor in
compartment VI alone, and 14 had residual tumor in both the thyroid
bed and compartment VI (Table
II).
 | Table IIOverall tumor residue. |
Table II
Overall tumor residue.
| Location | No. (%) |
|---|
| Thyroid bed | 18 (30) |
| Compartment VI
region | 28 (47) |
| Thyroid bed and
compartment VI region | 14 (23) |
Lymph node metastasis in compartment
VI
All 117 patients underwent compartment VI
dissection. Lymph node metastasis was confirmed in compartment VI
in 42 patients (35.90%), with an average of 6.5 nodes removed
(range, 2–14 nodes for each patient). In addition, an average of
3.14 positive lymph nodes were confirmed in each of these
patients.
Complications
The cervical part of the recurrent laryngeal nerves
was fully dissected in all 117 patients. Among the 17 patients with
hoarseness following initial surgery in other institutions, 13
patients had undergone subtotal thyroidectomy and 4 patients had
undergone partial thyroidectomy. Investigation during reoperation
revealed that the recurrent laryngeal nerves had been completely
resected in 12 patients. Of these nerves, 8 had been resected near
the interaction with the inferior thyroid artery and 4 had been
resected within 1 cm of the laryngeal inlet, while 5 had been
sutured near the laryngeal inlet.
Among the 100 patients without recurrent laryngeal
nerve damage following initial surgery, 6 patients developed
hoarseness after reoperation. Other complications included hematoma
in two patients, wound infection in one patient and transient
hypoparathyroidism in two patients.
Survival
Patients were followed up for ≥18 months (range,
18–66 months). Seven patients (5.98%) developed recurrence
following reoperation. The recurrence was observed in the
contralateral thyroid gland in two patients, in the contralateral
tracheoesophageal groove in two patients and in the ipsilateral
lateral neck in three patients. All patients with recurrence
received salvage surgery and no mortality was recorded.
Discussion
The management of papillary thyroid carcinoma
continues to be an area of debate and controversy (6,7), which
includes the extent of thyroidectomy, the extent of lymphadenectomy
and the type of postoperative treatment to be performed. The debate
concerning the extent of thyroidectomy in well-differentiated
thyroid cancer focuses on total versus less than total
thyroidectomy. As the serum thyroglobulin level may be used as a
marker of recurrence, radioactive iodine (RAI) ablation may be
performed as an adjuvant therapy and multifocality is often
observed (8,9). Western countries usually routinely
perform total thyroidectomy followed by RAI ablation and thyroid
stimulating hormone (TSH) suppression as the standard treatment
(4,10,11),
particularly in patients with a tumor size >1 cm. However, total
thyroidectomy is not accepted by all thyroid surgeons worldwide,
particularly for low-risk patients. In the past decade, the
majority of patients with primary tumors <4 cm in size, no lymph
node metastases and a normal contralateral lobe determined by
ultrasound examination have been treated with thyroid lobectomy
alone, at the Memorial Sloan-Kettering Cancer Center (12). This indicates that lobectomy has
been accepted by Western surgeons in low-risk patients with PTC.
Studies from Japan and China, which are both countries with a large
population size, demonstrate that the majority of low-risk patients
with papillary thyroid carcinoma become disease-free when they
undergo surgery that is less extensive than total thyroidectomy
(13). Additionally, recurrent
laryngeal nerve paralysis and hypoparathyroidism may be decreased,
L-thyroxine may not be administered throughout the patient’s life
and the recurrence rate of contralateral thyroid gland of patients
who underwent hemithyroidectomy has been demonstrated to be low
(only 1% for T1NOMO patients in Japan) (14). Multifocalities have been detected in
the range of 15.0–43.8% (8,9,15).
However, for patients with a solitary tumor detected by imaging
findings (the minimal focus size typically detected is ∼3 mm) and
with multifocalities detected by pathological examination, whether
it is clinically beneficial to treat these small pathological
focuses remains unclear. A study from Japan concerning
microcarcinoma helps us to understand multifocalities detected by
pathological examination from a different perspective (16). No size changes were observed in 70%
of microcarcinomas, while a size enlargement (>3 mm) was
identified in only 6.7% of the microcarcinomas and no distant
metastasis or death of the thyroid carcinoma were observed after a
5-year follow-up. The authors suggested that observation of PMC is
a reasonable strategy for microcarcinoma incidentally detected by
imaging studies. Therefore, microcarcinoma detected by pathology is
of less clinical significance than that detected by imaging.
The treatment results of total thyroidectomy and
hemithyroidectomy remain controversial for low-risk PTC (15,17). A
study by Shah et al demonstrated that no differences in
cause-specific survival, local recurrence, regional recurrence and
distant metastasis at 20 years were observed between low-risk
patients undergoing lobectomy and total thyroidectomy (18). Moreover, data from China have
demonstrated that good survival rates and low morbidities were
achieved, and that lobectomy was suggested to Chinese surgeons
(19). Medical institutions are
widely distributed in China, with a great disparity in the medical
levels of different regions. Radical surgery, as with Western
countries, may cause further complications and decrease patients’
quality of life. Therefore, according to experiences in China and
to other data, for low-risk PTC, lobectomy does not decrease
survival and increase recurrence rates, while it decreases
complications and is suitable for use in China. Due to the
aforementioned reasons, our center considers lobectomy to be the
initial treatment for low-risk PTC with a solitary tumor located in
one lobe. Additionally, we now perform completion lobectomy in such
patients who have undergone surgery that is less extensive than
lobectomy, particularly for patients who undergo nodulectomy alone
for benign disease. In our study, 32 out of 117 patients who
underwent surgery less extensive than lobectomy were observed to
have residual tumor in the left ipsilateral lobe, which indicates
that it was necessary for those patients to undergo completion
surgery.
Compartment VI dissection is another debated issue
in PTC treatment. The value of compartment VI dissection is
determined by whether it improves survival or decreases recurrence
rates; whether it increases the risk of hypoparathyroidism and
recurrent laryngeal nerve damage; and whether reoperation in
compartment VI increases the risk of hypoparathyroidism and
recurrent laryngeal nerve damage (20).
Certain authors argue that compartment VI metastasis
has no effect on long-term survival (8,21).
Sugitani and Fujimoto reported that patients with compartment VI
metastasis have a poorer prognosis than those without metastasis
(22. Vini et al confirmed that compartment VI metastasis may
have prognostic implications, particularly for those patients
>45 years of age (12). Current
evidence shows a potential decrease in local recurrence and a
possible survival benefit are associated with compartment VI
dissection (23). Compartment VI
dissection may cause a higher rate of permanent hypoparathyroidism
and unintentional permanent recurrent laryngeal nerve injury, while
experienced thyroid surgeons are able to decrease the rate of
complications. It has been demonstrated that a higher rate of
hypocalcemia and nerve damage is expected in reoperation in
patients with compartment VI recurrence (24). Additionally, the diagnostic accuracy
of pre-operative imaging for compartment VI metastasis is very low;
ultrasonography is the most important examination and is confirmed
to have a high positive predictive value and sensitivity, but a low
negative predictive value and specificity (25). For the reasons listed previously,
more surgeons are considering compartment VI dissection in the
initial treatment for PTC patients (26–29).
There continues to be considerable controversy
related to unilateral or bilateral central compartment dissection
(5). In our hospital, we take
unilateral central compartment dissection (prelaryngeal,
pretracheal and paratracheal lymph nodes) to be the standard
treatment for patients with PTC located in one lobe. The reasons
for this are as follows: i) recurrent laryngeal nerve dissection is
the basic step for both lobectomy and unilateral central
compartment dissection, and tissues in these two compartments may
be resected as a whole body according to continuous en bloc
and tumor-isolating principles; ii) complications, including
hypoparathyroidism and bilateral recurrent laryngeal nerve injury,
may be decreased or possibly avoided; iii) positive lymph nodes are
mainly distributed in the unilateral central compartment of the
tumor, and the risk of reoperation in the contralateral central
compartment would be low as no dissection would have occurred in
the initial surgical procedure.
In China, treatment of the central compartment is
not satisfactory, as numerous surgeons in Chinese community
hospitals do not consider metastasis in the central compartment to
be an important part of PTC treatment, and positive lymph nodes in
the central compartment are typically ignored, which is a potential
risk for recurrence. In the present study, none of the 117 patients
underwent compartment VI dissection, while 42 patients had
confirmed lymph node metastasis, which strongly indicates the need
for routine compartment VI dissection.
Due to the evidence discussed previously, in our
department, we now perform salvage surgery, which includes the
ipsilateral residual lobe, the isthmus and ipsilateral compartment
VI (the prelaryngeal, pretracheal and paratracheal lymph nodes), in
low-risk patients undergoing surgery that is less extensive than
hemithyroidectomy. The key problem is how to perform the surgery
according to en bloc and tumor-isolating principles
following confirmation of the extent of salvage surgery required.
The surgical approach that we adopted based on our own experience
and understanding, and that has not been demonstrated in other
studies, has been introduced in this study (detailed in Surgical
approach). This surgical approach achieves en bloc resection
of the ipsilateral residual lobe, the residual tumor, the isthmus,
ipsi-lateral compartment VI and the contaminated strap muscles,
according to the tumor-isolating principles that have become our
standard approach to salvage surgery.
Acknowledgements
The authors would like to thank all
study participants and their families.
References
|
1
|
Cooper DS, Doherty GM, Haugen BR, et al:
Management guidelines for patients with thyroid nodules and
differentiated thyroid cancer. Thyroid. 16:109–142. 2006.
View Article : Google Scholar
|
|
2
|
Sundram F, Robinson BG, Kung A, et al:
Well-differentiated epithelial thyroid cancer management in the
Asia Pacific region: a report and clinical practice guideline.
Thyroid. 16:461–469. 2006. View Article : Google Scholar
|
|
3
|
Davies L and Welch HG: Increasing
incidence of thyroid cancer in the United States, 1973–2002. JAMA.
295:2164–2167. 2006.
|
|
4
|
Cooper D, Doherty G, Haugen B, et al:
Revised American thyroid association management guidelines for
patients with thyroid nodules and differentiated thyroid cancer.
Thyroid. 19:1167–1213. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shaha AR: Prophylactic central compartment
dissection in thyroid cancer: a new avenue of debate. Surgery.
146:1224–1227. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grant CS, Stulak JM, Thompson GB, Richards
ML, Reading CC and Hay ID: Risks and adequacy of an optimized
surgical approach to the primary surgical management of papillary
thyroid carcinoma treated during 1999-006. World J Surg.
34:1239–1246. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gary LC, Shellenberger TD, Ginsberg LE, et
al: Approach and safety of comprehensive central compartment
dissection in patients with recurrent papillary thyroid carcinoma.
Head Neck. 31:1152–1163. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wada N, Duh QY, Sugino K, et al: Lymph
node metastasis from 259 papillary thyroid microcarcinomas. Ann
Surg. 237:399–407. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chow SM, Law SC, Chan JK, Au SK, Yau S and
Lau WH: Papillary microcarcinoma of the thyroid-prognostic
significance of lymph node metastasis and multifocally. Cancer.
98:31–40. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Takami H, Ito Y, Okamoto T and Yoshida A:
Therapeutic strategy for differentiated thyroid carcinoma in Japan
based on a newly established guideline managed by Japanese Society
of Thyroid Surgeons and Japanese Association of Endocrine Surgeons.
World J Surg. 35:111–121. 2011. View Article : Google Scholar
|
|
11
|
Sywak M, Pasieka JL and Oglivie T: A
review of thyroid cancer with intermediate differentiation. J Surg
Oncol. 86:44–54. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vini L, Hyer SL, Marshall J, A’Hern R and
Harmer C: Long-term results in elderly patients with differentiated
thyroid carcinoma. Cancer. 97:2736–2742. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ito Y and Miyauchi A: Prognostic factors
and therapeutic strategies for differentiated carcinomas of the
thyroid. Endocr J. 56:177–192. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ito Y, Masuoka H, Fukushima M, et al:
Excellent prognosis of patient with solitary T1N0M0 papillary
thyroid carcinoma who underwent thyroidectomy and elective lymph
node dissection without radioiodine therapy. World J Surg.
34:1285–1290. 2010. View Article : Google Scholar
|
|
15
|
Falvo L, D’Ercole C, Sorrenti S, et al:
Papillary microcarcinoma of the thyroid gland: analysis of
prognostic factors including histological subtype. Eur J Surg.
168:28–32. 2002.
|
|
16
|
Ito Y, Uruno T, Nakano K, et al: An
observation trial without surgical treatment in patients with
papillary microcarcinoma of the thyroid. Thyroid. 13:381–388. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shaha AR, Shah JP and Loree TR: Low-risk
differentiated thyroid cancer: the need for selective treatment.
Ann Surg Oncol. 4:328–333. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shah JP, Loree TR, Dharker D and Strong
EW: Lobectomy versus total thyroidectomy for differentiated
carcinoma of the thyroid: a matched-pair analysis. Am J Surg.
166:331–335. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Head and Neck Surgery Group, Editorial
Board of Chinese Journal of Otorhinolaryngology Head and Neck
Surgery: Discussion on clinical guideline of differentiated thyroid
carcinoma. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 881–886.
2011.(in Chinese).
|
|
20
|
White ML, Gauger PG and Doherty GM:
Central lymph node dissection in differentiated thyroid cancer.
World J Surg. 31:895–904. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shaha AR, Tuttle RM and Shah JP: Papillary
microcarcinoma of the thyroid. J Surg Oncol. 95:532–533. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sugitani I and Fujimoto Y: Symptomatic
versus asymptomatic papillary thyroid microcarcinoma: a
retrospective analysis of surgical outcome and prognostic factors.
Endocr J. 46:209–216. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gemsenjäger E, Perren A, Seifert B,
Schüler G, Schweizer I and Heitz PU: Lymph node surgery in
papillary thyroid carcinoma. J Am Coll Surg. 197:182–190. 2003.
|
|
24
|
Lim DJ, Baek KH, Lee YS, et al: Clinical,
histopathological, and molecular characteristics of papillary
thyroid microcarcinoma. Thyroid. 17:883–888. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ito Y, Tomoda C, Uruno T, et al:
Ultrasound-detectable and anatomopathologically-detectable node
metastasis in the lateral compartment as indicators of worse
relapse-free survival in patients with papillary thyroid carcinoma.
World J Surg. 29:917–920. 2005. View Article : Google Scholar
|
|
26
|
Ito Y, Jikuzono T, Higashiyiama T, et al:
Clinical significance of lymph node metastasis of thyroid papillary
carcinoma located in one lobe. World J Surg. 30:1821–1828. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shindo M, Wu JC, Park EE and Tanzella F:
The importance of central compartment elective lymph node excision
in the staging and treatment of papillary thyroid cancer. Arch
Otolaryngol Head Neck Surg. 132:650–654. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Machens A, Hauptmann S and Dralle H: Lymph
node dissection in the lateral neck for completion in central node
positive papillary thyroid cancer. Surgery. 145:176–181. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Swyak M, Cornford L, Roach P, Stalberg P,
Sidhu S and Delbridge L: Routine ipsilateral level VI
lymphadenectomy reduces postoperative thyroglobulin levels in
papillary thyroid cancer. Surgery. 140:1000–1007. 2006. View Article : Google Scholar
|