Introduction
Giant cell tumor of the tendon sheath (GCTTS) is a
benign lesion of uncertain etiology that involves inflammation,
trauma, toxin, allergy, clonal chromosomal abnormalities and
aneuploidy (1–2). Jaffe et al originally described
the condition in 1941 (3).
Approximately 85% of GCTTS occurs in the fingers, while 12% of
tumors are located in the knee, elbow, hip and ankle (4). GCTTS may occur at any age but most
typically occurs between the ages of 30 and 50, with a 2:1 female
predominance (5). GCTTS in the knee
is extremely rare, particularly in a 15-year-old boy. Most often,
GCTTS is small (average tumor size, 2.0 cm) (5), although the mass in this case,
measuring 3.8×2.0×1.7 cm was much larger than average. There are
few reports in the literature of cases occurring in males, in
younger age groups, tumor located in the knee and of greater tumor
size. Antecedent trauma has been reported, but only 15% of cases
have a definite history of trauma (6). Our patient reported a trauma while
playing basketball at school 6 months previously. Treatments
consist of careful local excision, particularly microscopic
excision, and postoperative radiotherapy. GCTTS may recur following
excision.
One of the most important clinical features is that
the symptoms of GCTTS are non-specific. We report a valuable case
that was not initially regarded as GCTTS. Following excision
biopsy, the diagnosis of GCTTS was made. We believe that this study
may assist clinicians in making a proper diagnosis and
administering correct treatment.
Case report
The research findings are presented with the consent
of the boy's parents and ethics committee approval. A 15-year-old
boy presented with an occult growing swelling and a 2-month history
of pain in the left knee at the Provincial Hospital Affiliated to
Shandong University, China. Strenuous exercise aggravated the pain,
which was felt at the infra-patellar region of the left knee. The
skin temperature of the left knee was higher than the right one.
The patient reported a trauma when playing basketball at school 6
months previously. Physical examination revealed local tenderness
of the fibular and tibial collateral ligament. The range of motion
was limited. Hyperextension and hyperflexion tests of the left knee
were positive. There were no constitutional symptoms such as night
sweats, fever or weight loss. The patient had previously been
healthy, and no enlarged inguinal lymph nodes were detected.
Analysis of the patient's blood was normal.
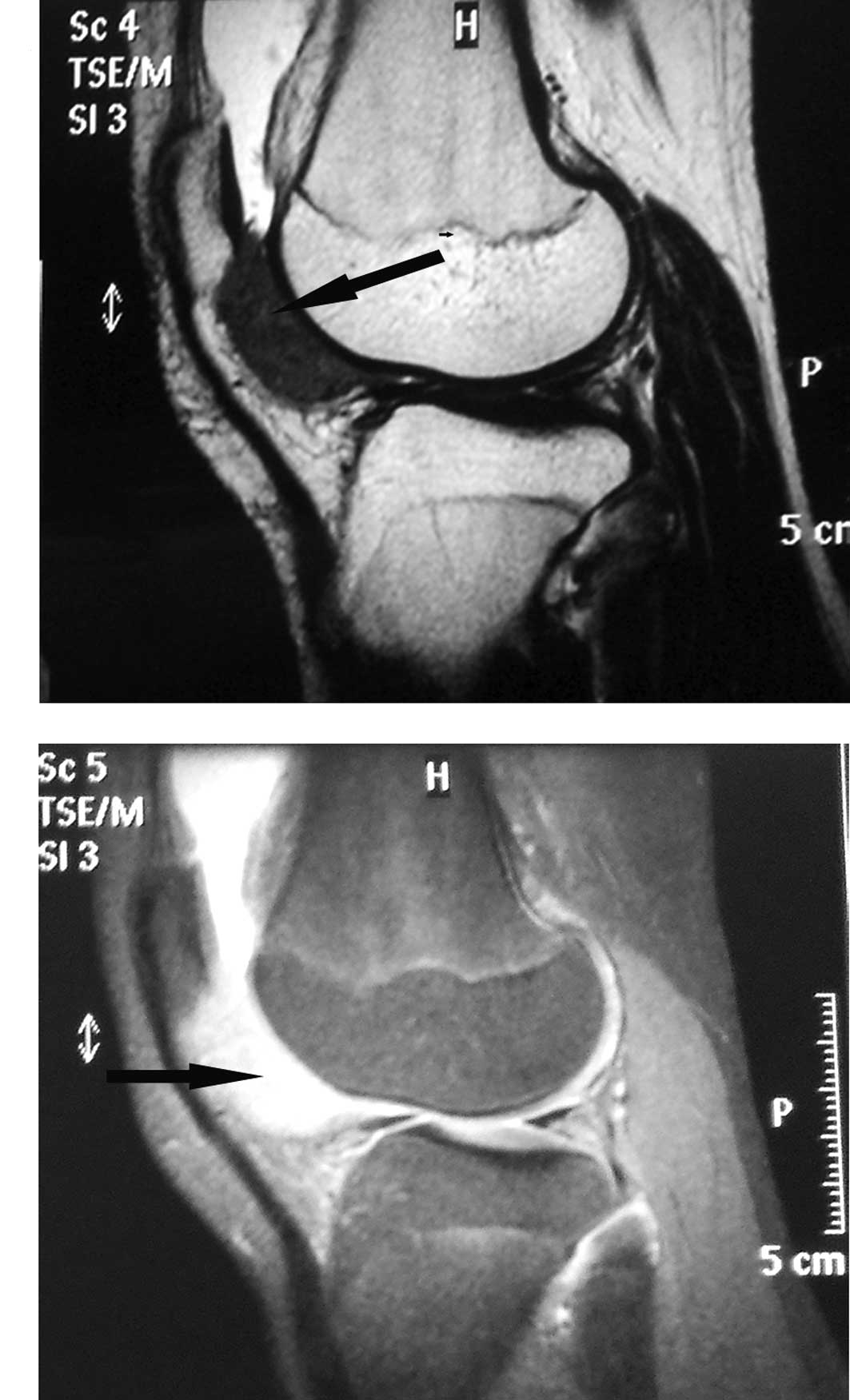
Plain radiography and magnetic resonance imaging
(MRI) were obtained. Plain anteroposterior and lateral radiographs
revealed no bone erosion of the left knee joint (Fig. 1). MRI demonstrated an encapsulated
soft tissue lump in the infra-patellar fat pad, posterior to the
patella tendon (Fig. 2). Initially,
we regarded the neoplasm as an intra-articular lipoma, synovial
sarcoma or fibroma of the tendon. Excision biopsy was performed by
surgical removal, and an irregular shaped mass measuring
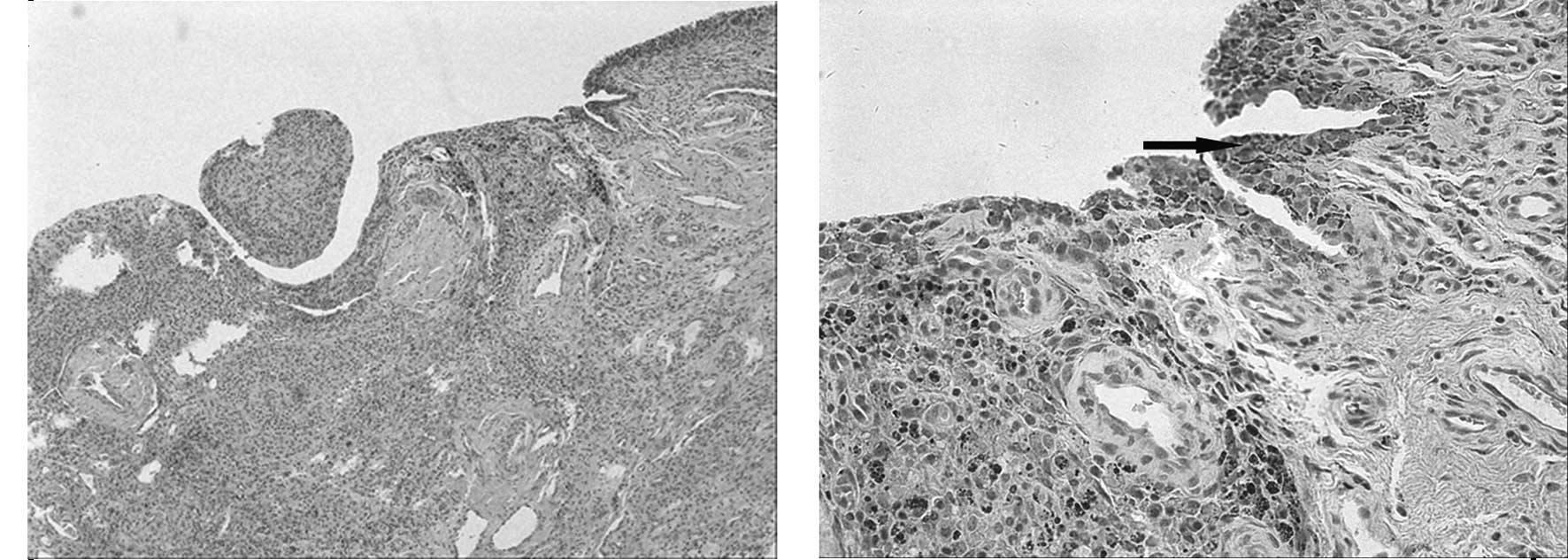
3.8×2.0×1.7 cm was removed. Histopathological examination of the
specimen revealed prominent mononuclear cells, accompanied by a
variable number of foamy histiocytes, hemosiderin-laden macrophages
and multinucleated giant cells (Fig.
3). No mitotic activity or malignant feature was reported. A
diagnosis of GCTTS was finally made.
The recovery following surgery was propitious. There
was no local tenderness of the left knee and the skin temperature
of the knee was normal. The patient had full range of motion of the
knee joint and returned to school life with no difficulty. During
the 5 month follow-up period there was no evidence of local tumor
recurrence.
Discussion
The diffuse and localized extra-articular forms of
pigmented villonodular synovitis (PVNS) are presently referred to
as diffuse-type giant cell tumor and giant cell tumor of the tendon
sheath (GCTTS), respectively (7),
and were originally alluded to by Jaffe et al in 1941
(3). Most localized giant cell
tumors are small (average tumor size, 2.0 cm) (5), although lesions of greater size may be
found in large joints such as the knee and elbow. Tumors are
well-circumscribed and typically lobulated, and white to gray in
color, with yellowish and brown areas. Most diffuse-type giant cell
tumors are infiltrative and grow as diffuse, expansile sheets.
These entities are now classified as ‘fibriohistiocytic tumors’ in
the World Health Organization system of classification of bone and
soft tissue tumors (4). GCTTS
occurs in the digits of the hands and feet more frequently than in
the large joints of the knee, elbow and ankle (8); 85% of GCTTS is observed in fingers,
while 12% is observed in large joints (4). GCTTS in the knee is rare.
The etiology of GCTTS remains uncertain. A variable
number of factors have been described as possible causes of GCTTS.
These include inflammation, trauma, toxin, allergy, clonal
chromosomal abnormalities and aneuploidy (1–2). GCTTS
was initially regarded as an inflammatory disease; however, the
finding of aneuploidy in certain cases and the demonstration of
clonal chromosomal abnormalities strongly support a neoplastic
origin (4).
The diagnosis of GCTTS may be difficult. Patients
typically present with a painless mass in the digits or large
joints. The lesions are usually well-circumscribed and localized,
and infrequently erode or infiltrate the nearby bone (6). In large joints, the symptoms are
non-specific and few, thus the diagnosis is difficult to make. The
soft tissue mass grows and expands into areas of least resistance,
such as the tendon sheath (8).
Plain radiographs are usually not helpful in the diagnosis of the
disease. Bone erosions or soft tissue swelling is occasionally
found in plain radiographs.
Magnetic resonance imaging (MRI) is an effective and
highly sensitive tool for diagnosis. Typically, MRI features T1-
(T1WI) and T2-weighted (T2WI) images, which may present with a
homogeneous low signal intensity in GCTTS. The reason for this is
that tumors contain dense collagen and hemosiderin-laden
macrophages (9).
Treatments consist of careful and complete local
excision and postoperative radiotherapy. Surgical removal is the
standard treatment of GCTTS. Adequate initial local excision may
effectively limit the risk of local recurrence (10). Recently, microscopic excision has
been prescribed to prevent recurrence. Ikeda et al (11) treated 18 patients with microscopic
excision, and of the 18 patients which only one case recurred. The
reason for this recurrence was that the microscope excision was not
used in this diffuse-type patient. As an adjuvant therapy,
postoperative radiotherapy had been indicated to prevent recurrence
following surgery. Kotwal et al (12) published a prospective study in which
the recurrence rate was only 4%. This rate was much lower than
previously reported incidences of between 25 and 45%.
Although GCTTS is a benign type of tumor, it has a
high incidence of recurrence. Recurrence following resection has
been a consistent problem, and occurs in 9 to 44% of cases
(13). Lowyck and De Smet (13) retrospectively reviewed 49 patients
and reported the rate of recurrence to be 16%.
In conclusion, the concurrence of GCTTS occurring in
a younger male, occurring in the knee and being of greater than
average size is unique to our patient, making this an exceptional
case to those reported in previous literature. It is extremely
difficult to make a proper diagnosis during the earlier stages of
GCTTS. As the condition always presents with a painful lump, it
should be considered as a differential diagnosis if the mass is
found in the knee, particularly in younger males and when the tumor
is of greater size. MRI may be useful for diagnosis when the
symptoms of GCTTS are non-specific and few. To make a definite
diagnosis, histopathological examination is required. If a possible
diagnosis of GCTTS is suspected, excision biopsy should be carried
out as early as possible in the same manner that the present case
was treated. Finally, the purpose for which we report this case is
to emphasize the possibility of GCTTS, even when the painless or
painful mass accompanied with non-specific symptoms are found in
the knee of a younger patient, and to avoid misdiagnosis wherever
possible.
References
|
1
|
Reilly KE, Stern PJ and Dale JA: Recurrent
giant cell tumors of the tendon sheath. J Hand Surg. 24:1298–1302.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Abdul-Karim FW, el-Naggar AK, Joyce MJ,
Makley JT and Carter JR: Diffuse and localized tenosynovial giant
cell tumor and pigmented villonodular synovitis: a
clinicopathologic and flow cytometric DNA analysis. Hum Pathol.
23:729–735. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jaffe HL, Lichtenstein L and Sutro CJ:
Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch
Pathol. 31:731–765. 1941.
|
|
4
|
Fletcher CDM, Krishnan Unni K and Mertens
F: Giant cell tumour of tendon sheath. World Health Organization
Classification of Tumors, Pathology and Genetics of Tumors of Soft
Tissue and Bone. IARC Press; Lyon: pp. 110–111. 2002
|
|
5
|
Ushijima M, Hashimoto H, Tsuneyoshi M and
Enjoji M: Giant cell tumor of the tendon sheath (nodular
tenosynovitis): a study of 207 cases to compare the large joint
group with the common digit group. Cancer. 57:875–884. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Uriburu IJ and Levy VD: Intraosseous
growth of giant cell tumors of the tendon sheath (localized nodular
tenosynovitis) of the digits: report of 15 cases. J Hand Surg.
23:732–736. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sanghvi DA, Purandare NC, Jambhekar NA,
Agarwal MG and Agarwal A: Diffuse-type giant cell tumor of the
subcutaneous thigh. Skeletal Radiol. 36:327–330. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Relwani J, Factor D, Khan F and Dutta A:
Giant cell tumor of the patellar tendon sheath-an unusual cause of
anterior knee pain: a case report. Knee. 10:145–148. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cheng XG, You YH, Liu W, Zhao T and Qu H:
MRI features of pigmented villonodular synovitis (PVNS). Clin
Rheumatol. 23:31–34. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Monaghan H, Salter DM and Al-Nafussi A:
Giant cell tumour of tendon sheath (localized nodular
tenosynovitis): clinicopathological features of 71 cases. J Clin
Pathol. 54:404–407. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ikeda K, Osamura N and Tomita K: Giant
cell tumor in the tendon sheath of the hand: importance of the type
of lesion. Scand J Plast Reconstr Surg Hand Surg. 41:138–142. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kotwal PP, Gupta V and Malhotra R:
Giant-cell tumor of the tendon sheath: is radiotherapy indicated to
prevent recurrence after surgery? J Bone Joint Surg Br. 82:571–573.
2000.PubMed/NCBI
|
|
13
|
Lowyck H and De Smet L: Recurrence rate of
giant cell tumors of the tendon sheath. Eur J Plast Surg.
28:385–388. 2006. View Article : Google Scholar
|