Introduction
Hepatocellular carcinoma (HCC) is one of the most
common types of malignant liver tumor, which is the third leading
cause of cancer mortality worldwide (1–3).
Studies have demonstrated that countries in Asia, particularly
China, have a high incidence rate of HCC, due to endemic hepatitis
B and C (4,5). Surgeries, including complete surgical
resection and liver transplantation, offer the best prognosis for
HCC (6,7). However, 70–85% of patients with HCC
are not surgical candidates due to advanced liver disease or
extrahepatic metastases (8,9). Metastatic right atrial (RA) tumor
thrombus is rare in advanced HCC patients, but the prognosis is
poor (10,11). Transcatheter arterial
chemoembolization (TACE) is the most widely used primary treatment
for patients with HCC who are considered unsuitable candidates for
surgery (12,13).
We present a case of an HCC patient with metastatic
RA tumor thrombus who presented with secondary Budd-Chiari
syndrome. The patient underwent effective TACE therapy and remains
alive after 3 years and 10 months.
Patients and methods
The patient was a 45-year-old man with a one-month
history of edema in the lower extremities and recurrent episodes of
chest distress. Examination revealed no abdominal pain, abdominal
distension, or other manifestations of liver cancer.
Upon admission, a physical examination was
conducted.It was discovered that both legs had marked edema, but no
further abnormalities, including hepatosplenomegaly and ascites,
were observed. Laboratory examinations revealed that the level of
α-fetoprotein was 2041.3 ng/ml (normal value, <20.0 ng/ml). The
levels of glutamate oxaloacetic transaminase 44 U/l (<40 U/l),
glutamate pyruvate transaminase 34 U/l (<50 U/l), total
bilirubin 18.0 μmol/l (<22 μmol/l), and albumin 31.4 g/l (35–55
g/l) were elevated. The viral marker tests demonstrated that HBsAg
was positive.
A chest X-ray revealed a moderate right pleural
effusion, but no abnormalities were observed from the ECG. The
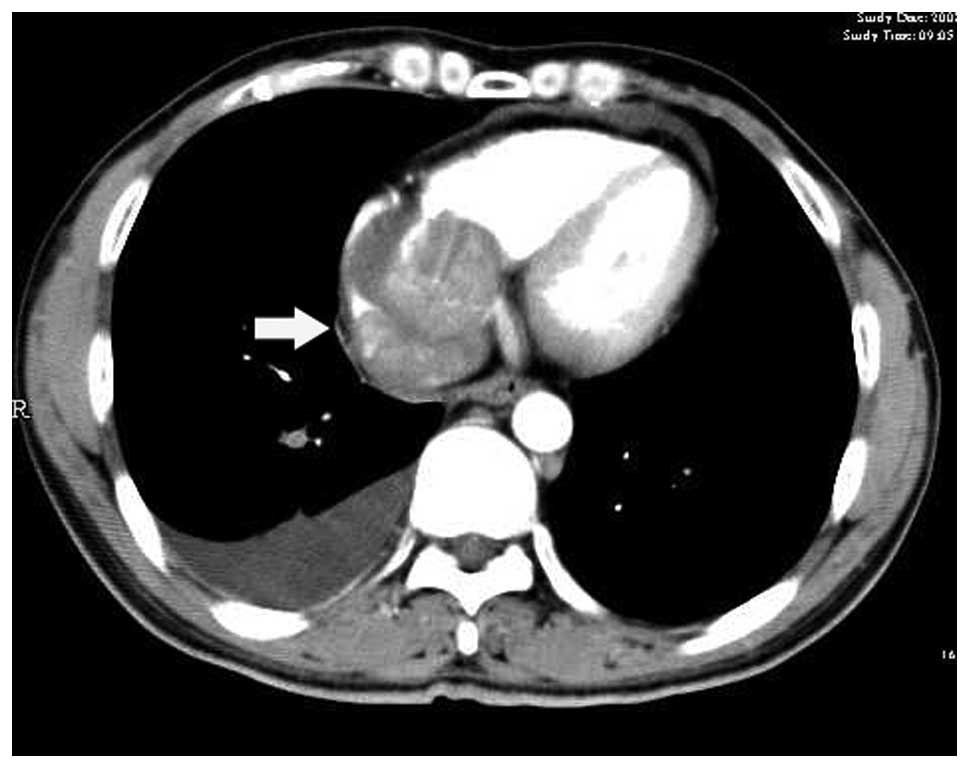
abdominal-enhanced CT scan, which was performed on admission,
demonstrated an arterial-phase enhancing mass in the left lobe
which was found to have extended into the inferior vena cava (IVC)
and RA (Fig. 1). The tumor and the
RA tumor thrombus demonstrated an enhancing pattern of HCC.
Therefore, a diagnosis of HCC with RA tumor thrombus was
established based on the high level of plasma α-fetoprotein
(>400 ng/ml) combined with typical CT appearances. The CT images
also revealed a moderate right pleural effusion.
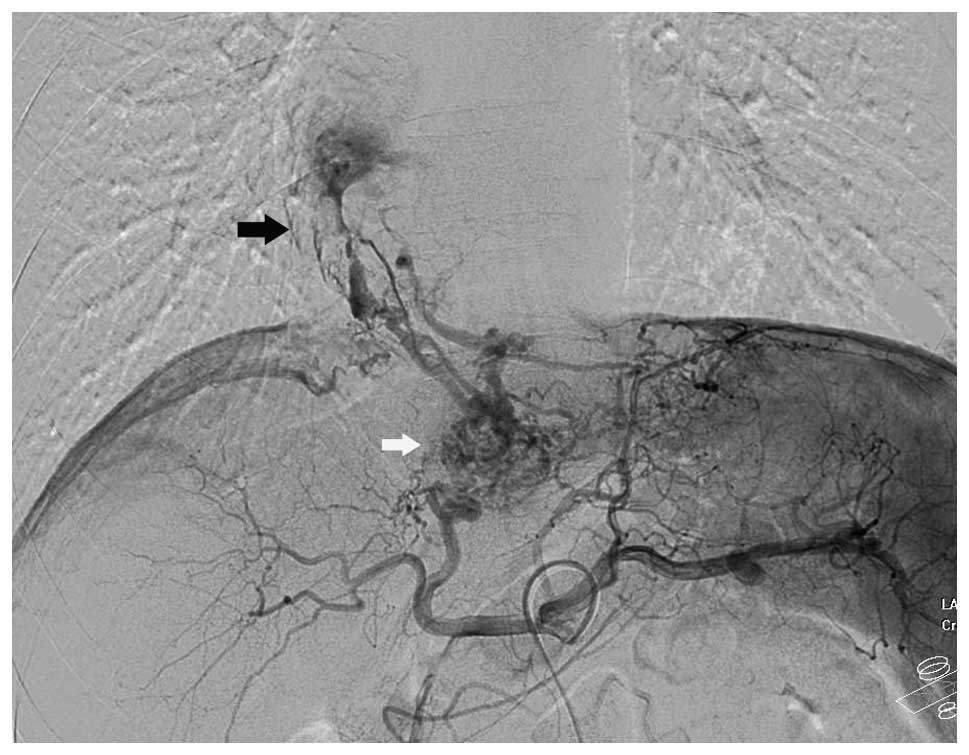
Selective hepatic angiography (Fig. 2) showed hypervascular tumor staining
of the left hepatic lobe, which was typical of HCC, and extended
into the IVC and RA through the hepatic vein. The feeding arteries
of the tumor and tumor thrombus were derived from the left hepatic
artery. A filling defect of the IVC and RA, and upward collateral
veins, were revealed by inferior vena cavography. Therefore, the
patient was diagnosed with HCC complicated by secondary Budd-Chiari
syndrome, resulting from tumor thrombus of the venous system.
Following diagnosis, the patient underwent 2
sessions of TACE therapy over a period of 3 months. Depending on
the arterial supply of the tumor identified by the arteriographies,
a 2.7 French microcatheter (Terumo, Tokyo, Japan) was
superselectively placed into the feeding arteries of the tumor and
the tumor thrombus for selective embolization which was carried out
with an embolization suspension consisting of pirarubicin (30 mg),
oxaliplatin (200 mg), hydroxycamptothecine (20 mg) and iodized-oil
(Lipiodol; Guerbet, Aulnay-sous-Bois, France).
The study was approved by the ethics committee of
the First Affiliated Hospital, School of Medicine, Zhejiang
University. Consent was obtained from the patient in this
study.
Results
Following TACE therapy, the pleural effusion and
edema of the lower extremities disappeared. The level of
α-fetoprotein gradually decreased to a normal level (<20 ng/ml).
A CT scan was performed 2 years later (Fig. 3), which revealed that the tumor
thrombus within the IVC and RA had shrunk and almost disappeared.
The liver tumor also markedly decreased in size and almost
disappeared on the CT images. Following therapy, the patient has
been regularly followed up and demonstrates no signs of tumor
progression and has continued to experience quality of life 3 years
and 10 months following treatment.
Discussion
The incidence of HCC is on the increase worldwide
due to the rise in hepatitis B and C infection (2,4).
Hepatic resection or liver transplantation is restricted to a small
minority of patients with HCC (8,9).
Greatly-advanced HCC with involvement of the heart is rare
(14,15). The early diagnosis of HCC with tumor
thrombus extending into the heart is occasionally difficult,
particularly when patients do not demonstrate abdominal
manifestations of liver cancer (16). In this case study, the patient had
tumor thrombus within the IVC and RA, which caused secondary
Budd-Chiari syndrome, and which was identified as a presenting
feature of HCC. Despite progress in the treatment of liver cancer,
greatly-advanced HCC with metastatic IVC and RA tumor thrombus has
an extremely poor prognosis (14,15).
The median survival of patients with metastatic IVC and RA tumor
thrombus, without effective therapy, is only 2–3 months (17). For HCC with metastatic IVC and RA
tumor thrombus, no effective therapy has yet been reported. For
these patients, surgical resection is often not complete or
impossible. Previous studies on surgery for HCC with metastatic IVC
and RA tumor thrombus have demonstrated disappointing results with
a mean survival time of approximately 8 months (18).
TACE has become the most widely used and effective
treatment in patients with advanced HCC, and provides a survival
benefit for selective patients (19). It is also the most extensively used
treatment for patients on the waiting list for liver
transplantation (13). Following
selective catheterization of the feeding artery of the tumor, a
suspension consisting of iodized-oil and anticancer drugs was
slowly injected into the target vessel to fulfill the
microcirculation of the tumor, and remained there to prevent the
blood flow causing tumor necrosis (13). TACE therapy has already become a
significant and commonly used non-surgical treatment for HCC
(12,13,19).
However, there is a lack of large sample sizes in
studies that have demonstrated the safety and efficacy of TACE in
patients with greatly-advanced HCC with metastatic IVC and RA tumor
thrombus. There have only been some case studies that have examined
TACE therapy for HCC with metastatic IVC and RA tumors (20,21).
In this case study, celiac angiography and inferior vena cavography
revealed that the feeding artery of the tumor thrombus associated
with HCC was derived from the tumor vessels from the hepatic
artery. Following selective chemoembolization, the decrease of the
tumor thrombus and the liver tumor was clearly demonstrated by a CT
scan. Additionally, the secondary Budd-Chiari syndrome of the
patients due to the tumor thrombus disappeared.
In conclusion, our long-term survival case indicates
that TACE therapy is not only an effective treatment against
secondary Budd-Chiari syndrome due to tumor thrombus, but is also
an effective treatment for advanced HCC with metastatic IVC and RA
tumor thrombus, and is beneficial to long-term survival.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (No. 30901446), the Medical Health Fund
of Zhejiang Province (No. 2008A053), the Programme of Chinese
Medical Science of Zhejiang Province (No. 2009CB040), the Program
for Innovative Research Team of Science and Technology of Zhejiang
Province (No. 2009R50038), the Major Program of the Science and
Technology Bureau of Zhejiang Province (No. 2009C03012-1) and the
National Major Program of Science and Technology of China (No.
2012ZX10002-17).
References
|
1
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Estimating the world cancer burden: Globocan 2000. Int J Cancer.
94:153–156. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
He J, Gu D, Wu X, et al: Major causes of
death among men and women in China. N Engl J Med. 353:1124–1134.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
El-Serag HB: Hepatocellular carcinoma and
hepatitis C in the Ued States. Hepatology. 36:S74–S83. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Taura N, Hamasaki K, Nakao K, et al: Aging
of patients with hepatitis C virus-associated hepatocellular
carcinoma: Long-term trends in Japan. Oncol Rep. 16:837–843.
2006.PubMed/NCBI
|
|
5
|
Llovet JM, Fuster J and Bruix J: Prognosis
of hepatocellular carcinoma. Hepatogastroenterology. 49:7–11.
2002.
|
|
6
|
Kawano Y, Sasaki A, Kai S, et al: Short-
and long-term outcomes after hepatic resection for hepatocellular
carcinoma with concomitant esophageal varices in patients with
cirrhosis. Ann Surg Oncol. 15:1670–1676. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Saab S, Yeganeh M, Nguyen K, et al:
Recurrence of hepatocellular carcinoma and hepatitis B reinfection
in hepatitis B surface antigen-positive patients after liver
transplantation. Liver Transpl. 15:1525–1534. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tsuzuki T, Sugioka A, Ueda M, Iida S,
Kanai T, Yoshii H and Nakayasu K: Hepatic resection for
hepatocellular carcinoma. Surgery. 107:511–520. 1990.PubMed/NCBI
|
|
9
|
Fan HL, Chen TW, Hsieh CB, et al: Liver
transplantation is an alternative treatment of hepatocellular
carcinoma beyond the Milan criteria. Am J Surg. 200:252–257. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Florman S, Weaver M, Primeaux P, et al:
Aggressive resection of hepatocellular carcinoma with right atrial
involvement. Am Surg. 75:1104–1108. 2009.PubMed/NCBI
|
|
11
|
Lazaros G, Samara C, Nikolakopoulou Z and
Tassopoulos N: Growth of hepatocellular carcinoma into the right
atrium. A case of antemortem diagnosis with magnetic resonance
imaging of the heart. Acta Cardiol. 58:563–565. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Scartozzi M, Baroni GS, Faloppi L, et al:
Trans-arterial chemoembolization (TACE), with either lipiodol
(traditional TACE) or drug-eluting microspheres (precision TACE,
pTACE) in the treatment of hepatocellular carcinoma: efficacy and
safety results from a large mono-institutional analysis. J Exp Clin
Cancer Res. 29:1642010. View Article : Google Scholar
|
|
13
|
Baur M, Walter R, Gebauer A, et al:
Chemoembolization with cisplatin, lipiodol and Gelfoam and
subsequent systemic chemotherapy with cisplatin and interferon in
patients with hepatocellular carcinoma: A non-randomized
prospective study. Int J Oncol. 23:811–819. 2003.
|
|
14
|
Nam SW, Baek JT, Kang SB, et al: A case of
the hepatocellular carcinoma during the pregnancy and metastasis to
the left atrium. Korean J Hepatol. 11:381–385. 2005.PubMed/NCBI
|
|
15
|
Chong VH, Jamaludin AZ, Lim KS, Abdullah
HM and Nair RT: Hepatocellular carcinoma with intravascular and
right atrial extension. Indian J Gastroenterol.
27:2552008.PubMed/NCBI
|
|
16
|
Lazopoulos GL, Manns-Kantartzis M and
Kantartzis MN: Severe right atrial obstruction due to cardiac
extension of a hepatic carcinoma. Ann Thorac Surg. 87:6452009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zeng Z, Fan J, Tang Z, et al: A comparison
of treatment combinations with and without radiotherapy for
hepatocellular carcinoma with portal vein and/or inferior vena cava
tumor thrombus. Int J Radiat Oncol Biol Phys. 61:432–443. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Asahara T, Itamoto T, Katayama K, et al:
Hepatic resection with tumor thrombectomy for hepatocelluar
carcinoma with tumor thrombi in the major vasculatures.
Hepatogastroenterology. 46:1862–1869. 1999.PubMed/NCBI
|
|
19
|
Takayasu K, Arii S, Ikai I, et al:
Prospective cohort study of transarterial chemoembolization for
unresectable hepatocellular carcinoma in 8510 patients.
Gastroenterology. 131:461–469. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dazai Y, Katoh T, Katoch I, Sueda S and
Yoshida R: Effectiveness of chemoembolization therapy for
metastatic right atrial tumor thrombus associated with
hepatocellular carcinoma. Chest. 96:434–436. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kashima Y, Miyazaki M, Kaiho T, et al: A
successful treatment for hepatocellular carcinoma with atrial tumor
thrombus. Hepatogastroenterology. 43:1040–1045. 1996.
|