Introduction
Prostate cancer (PCa) is the second most frequently
diagnosed type of cancer, and in 2008, it was the sixth leading
cause of cancer mortality in males worldwide (1). Although the incidence of PCa in China
is not as high as that in Europe and North America, it is currently
on the increase. Gu (2,3) evaluated the incidence of PCa at 187
hospitals based in 26 Chinese provinces. The overall incidence rate
of PCa in 1997 was 1.5% (1389/95749). Between 1951 and 1960 the
incidence rate of PCa at the Institute of Urology, Beijing
University, Beijing, China, was 0.6%. However, between 1991 and
1997 this rate has increased to 3.4% in total.
As a curative treatment for localized PCa,
laparoscopic radical prostatectomy has been performed in Western
countries for almost 15 years. However, it remains a great
challenge to many Chinese urologists. A narrower pelvis of Asian
males compared with Caucasian males increases the difficulty of
performing laparoscopic radical prostatectomy. A smaller incidence
of PCa in China compared to Western countries means that surgeons
require a longer time to become experienced. To the best of our
knowledge, published studies decribing laparoscopic radical
prostatectomy exceeding 300 Chinese cases are rare.
Between March 2005 and March 2010, we performed 329
cases of extraperitoneal laparoscopic radical prostatectomy (ELRP)
with running urethrovesical anastomosis using the single needle
method (4). In this study, we
evaluated the oncological and clinical results after ELRP.
Patients and methods
Patient characteristics
All 329 patients had been confirmed as localized PCa
by examinations using magnetic resonance images and transrectal
ultrasound guided biopsies, with negative radionuclide bone scans
(PSA ≥20 ng/ml and Gleason scores ≥7). The median age and median
initial prostate-specific antigen (PSA) levels are shown in
Table I. The percentage of initial
PSA, clinical stage and biopsy Gleason scores are shown in Table II.
 | Table IPerioperative data from present and
previous studies. |
Table I
Perioperative data from present and
previous studies.
| Present data | Rozet et al
(9) | Stolzenburg et
al (10) | Eden et al
(11) | Do et al
(12) |
|---|
| Number of
patients | 329 | 600 | 2400 | 1000 | 100 |
| Age (years)
(median) | 67 (45–78) | 62 (47–73) | 63.3 (41–81) | 62.0 (40–78) | 63.7 (43–78) |
| Initial PSA (ng/ml)
(median or mean) | 17.35
(4.58–201.85) | 7.4± 6.2 | 9.8 (0.08–93) | 7.0 (1–50) | 9.6 (1.5–59.2) |
| Biopsy Gleason score
(median) | 7 (4–10) | - | - | - | - |
| Time for anastomosis
(min) (median) | 13 (10–28) | - | - | - | - |
| Surgery time (min)
(median or mean) | 90 (80–185) | 173±85 (95–300) | 150.7 (50–340) | 177 (78–600) | 150 (75–270) |
| Estimated blood loss
(ml) (median or mean) | 75 (20–800) | 380±210
(20–3500) | 255 (20–1200) | 200 (10–1300) | 245 (30–800) |
| Blood transfusion
(ml) (median) | 600 (200–800) | - | - | - | - |
| Placement time of
retropubic drain (days) (median) | 3 (2–10) | - | - | - | - |
| Postoperative
catheterization time (days) (median) | 6 (5–14) | 7.6 (3–20) | 6.19 (3–40) | 10.0 (0.8–120) | 6.7 (4–24) |
| Time to oral intake
(days) (median) | 2 (1–4) | - | - | - | - |
| Time to ambulation
(days) (median) | 2 (2–4) | - | - | - | - |
| Postoperative
hospital stay (days) (median) | 7 (6–16) | 6.3 (4–14) | - | 3.0 (2–28) | - |
| Pathological TNM |
| pT2 (Organ
confined) | 211 (64.2%) | 432 (72%) | 1693 (70.5%) | - | - |
| pT3a (Extracapsular
extension) | 51 (15.5%) | 115 (19.2%) | 473 (19.7%) | - | - |
| pT3b (Seminal
vesicle invasion) | 60 (18.2%) | 53 (8.8%) | 226 (9.4%) | - | - |
| pT4 (Invasion of
rectum, levator muscles and/or pelvic wall) | 7 (2.1%) | - | 8 (0.3%) | - | - |
 | Table IIPercentage of initial PSA, clinical
stage and biopsy Gleason score. |
Table II
Percentage of initial PSA, clinical
stage and biopsy Gleason score.
| No. (%) |
|---|
| Initial PSA
(ng/ml) |
| <10 | 108 (32.8) |
| 10–20 | 98 (29.8) |
| >20 | 123 (37.4) |
| Clinical stage |
| T1b | 30 (9.1) |
| T1c | 38 (11.5) |
| T2a | 136 (41.3) |
| T2b | 28 (8.6) |
| T2c | 97 (29.5) |
| Biopsy Gleason
score |
| 2–6 | 135 (41.1) |
| 7 | 138 (41.9) |
| 8–10 | 56 (17.0) |
A total of 77 patients with T2 or T3a PCa clinical
stage had received neoadjuvant hormonal therapy (NHT) for 3–9
months prior to ELRP, while 94 patients had received NHT for <3
months. NHT comprised combined androgen blockade with luteinizing
hormone-releasing hormone analogue (goserelin acetate) injections
monthly and antiandrogen (bicalutamide, 50 mg) daily. A total of 30
patients had previously been treated with transurethral prostate
resection (TURP) and ELRP was performed in these patients after an
interval of 3 months.
Patients with localized PCa of clinical stage T1b-2c
(N0M0) with a life expectancy of >10 years were candidates for
ELRP. In each case, a bilateral pelvic lymph node dissection (PLND)
was performed according to these indications: enlarged lymph nodes
identified in magnetic resonance images, PSA ≥20 ng/ml, Gleason
scores ≥7 or G3 tumor. Candidates for bilateral neurovascular
bundles (NVB) sparing procedures were patients with normal
preoperative potency, T1 or T2 diseases, PSA <10 ng/ml and
Gleason scores ≤7.
All patients consented to the use of their clinical
data for this study. The Human Ethics Review Committee of Chinese
People’s Liberation Army General Hospital approved the study
protocol.
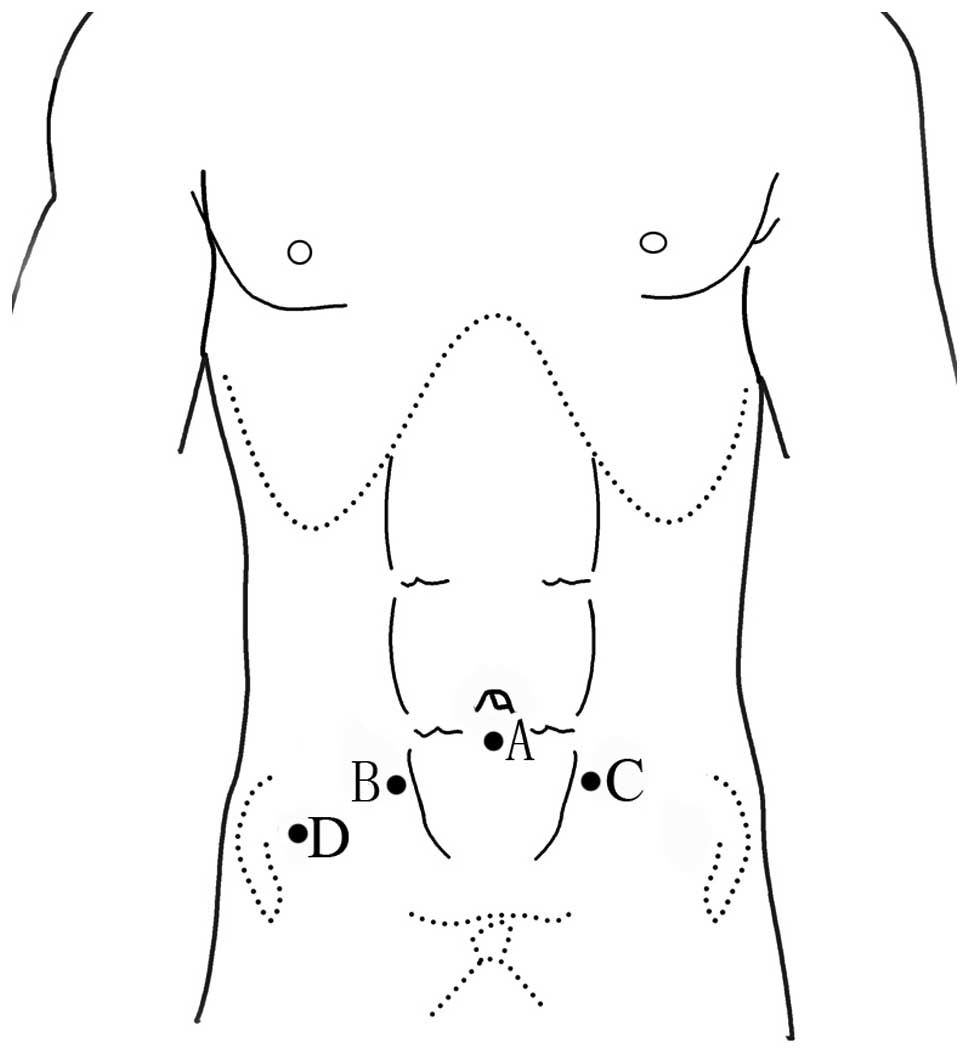
Surgical technique
ELRP was performed using the technique as described
by Stolzenburg et al (5),
but with certain modifications. While Stolzenburg et al
introduced the method of 5-trocars placement, the number and
position of the trocar placement was different in our study, in
which 4 trocars were applied to complete the surgery (Fig. 1). Stolzenburg et al used an
interrupted suture for urethrovesical anastomosis, whereas we
preferred a running urethrovesical anastomosis using a 25 cm 2–0
Monocryl suture with a UR-6 tape needle. The initial suture was
performed outside-in through the bladder neck at the 3 o’clock
position and a knot was tied with a 3-cm end outside on the
posterior lip of the bladder neck. Another suture at the nearby
position was performed outside-in through the bladder neck and
inside-out through the urethra at the corresponding position. Under
the guidance of a Foley catheter, clockwise running sutures were
performed from 3 o’clock to 9 o’clock every 1 o’clock with slight
traction. After gentle traction was applied to each suture to bring
the bladder neck in contact with the urethra without excessive
tension, the locking suture was performed at 9 o’clock. The running
sutures were continued from 10 o’clock to 2 o’clock every 2
o’clock. The needle went inside-out of the urethra near the 3
o’clock suture and a knot was tied at the tail end after completing
the full circumference. The surgeries were performed by the same
experienced surgeon (XZ).
Postoperative treatment and
follow-up
The patients were treated with antibiotics to
prevent infection until removal of the stitches approximately 7
days postoperatively. Patients received patient-controlled
intravenous analgesia for 2 or 3 days postoperatively. Different
types and doses of analgesics were applied by anesthetists
according to the different conditions of the patients. The Foley
catheter was normally retained for at least 5 days. The entire
gland was examined and the positive surgical margin (PSM) was
defined as any cancer cells in contact with ink. The specimens were
examined by an experienced pathologist. Pathological review of the
specimens was performed according to the TNM 2002 classification
for PCa. Candidates for adjuvant hormonal therapy (AHT) were
patients with PSMs, metastasis in the regional lymph node,
pathological T3 or T2 disease with Gleason scores >7 and initial
PSA>20 ng/ml. AHT comprised combined androgen blockade with
luteinizing hormone-releasing hormone analogue (goserelin acetate)
injections on a monthly basis and antiandrogen (bicalutamide, 50
mg) on a daily basis. Candidates for adjuvant external beam
radiotherapy (EBRT) were patients with PSMs, seminal vesicle
invasion, pathological T3 or T4 disease and postoperative
continuous rising PSA values. The patients required digital rectal
examination (DRE) and PSA detection postoperatively every 3 months
for 2 years, then every 6 months for 5 years and then annually.
Continence and erectile function were evaluated pre-
and postoperatively in all patients. Continence was defined when
patients did not require incontinence pads. Potency was defined by
positive answers to the following questions: ‘Could you get and
keep an erection?’, ‘how often were your erections hard enough to
be inserted into your partner’s vagina?’, ‘how often were you able
to maintain your erection after you had penetrated your partner
during sexual intercourse?’, ‘did your erections last long enough
to have sexual intercourse?’ and ‘were you satisfied with this
sexual experience?’. Patients were contacted by telephone and
answers to the above questions were recorded individually.
Questionnaires were mailed to patients without a telephone
interview.
Statistical analysis
Perioperative data were collected, while continence
and erectile function results were recorded during the follow-up.
Groups were compared using the Pearson Chi-square (χ2)
analysis. Multivariate analysis of the Cox proportional hazard
model was used to identify whether variables had significant
independent correlations with biochemical recurrence-free survival.
The Kaplan-Meier method and log-rank test were used to compare the
biochemical recurrence-free survival among the different groups. In
all analyses, P<0.05 was considered to indicate a statistically
signifcant difference, and was two-sided. The data were analyzed
using SPSS 18.0 software.
Results
Perioperative data
No conversion or re-intervention were found in the
329 cases of ELRP. Surgery time was recorded from the beginning of
subumbilical incision and ended when the specimen was removed. The
operative data are shown in Table
I, including the median times for anastomosis, surgery,
postoperative catheterization and the median estimated blood loss
and median blood transfusion.
There were 12 temporary urinary leakages requiring
prolonged catheterization to 14 days. A total of 1 case of deep
vein thrombosis occurred and was cured by non-surgical treatment 3
months postoperatively. There was 1 case of alimentary tract
hemorrhage which was controlled by the usage of antiulcerative
drugs. A total of 7 cases of anterior urethral stricture were
identified 3 months postoperatively, which were successfully
treated by endoscopic urethrotomy. No rectal injury, lymphocele,
incision infection or incision hernia were identified in our
patients.
PSM and Gleason score
The median pathological Gleason score was 7 (range,
5–10). The pathological Gleason scores could not be identified in
38 cases that had received preoperative NHT. The number of PSMs in
the no NHT group, NHT <1 month, NHT 1–3 months and NHT >3
months are shown in Table III.
The PSM rate was higher in the group without preoperative NHT.
Preoperative NHT had a significant effect on pathological Gleason
score (P<0.001) and surgical margin (P=0.027), respectively.
PSMs were identified in 55 patients (16.7%) (Table IV). Pearson Chi-square
(χ2) analysis demonstrated that PSM correlated with
pathological stage and Gleason score, respectively (both
P<0.001).
 | Table IIIPSM and pathological Gleason scores
among the differerent NHT groups. |
Table III
PSM and pathological Gleason scores
among the differerent NHT groups.
| No NHT | NHT<1 month | NHT 1–3 months | NHT >3 months | Total | P-value |
|---|
| Pathological Gleason
scores | | | | | | |
| No Gleason
score | 0 | 12 | 5 | 21 | 38 | P<0.001 |
| 2–6 | 53 | 10 | 0 | 18 | 81 | |
| 7 | 65 | 11 | 13 | 23 | 112 | |
| 8–10 | 40 | 23 | 20 | 15 | 98 | |
| Total | 158 | 56 | 38 | 77 | 329 | |
| Surgical
margin | | | | | | |
| PSM | 36 | 8 | 5 | 6 | 55 | P=0.027 |
| NSM | 122 | 48 | 33 | 71 | 274 | |
| Total | 158 | 56 | 38 | 77 | 329 | |
 | Table IVPSM among different pathological
stages and Gleason grade groups. |
Table IV
PSM among different pathological
stages and Gleason grade groups.
| PSM | NSM | Total | P-value |
|---|
| Pathological
stage |
| pT2a | 0 | 90 | 90 | |
| pT2b | 0 | 28 | 28 | |
| pT2c | 10 | 83 | 93 | P<0.001 |
| pT3a | 22 | 29 | 51 | |
| pT3b | 16 | 44 | 60 | |
| pT4 | 7 | 0 | 7 | |
| Pathological
Gleason score | | | | |
| No Gleason
score | 2 | 36 | 38 | |
| 2–6 | 3 | 76 | 79 | |
| 7 | 20 | 94 | 114 | P<0.001 |
| 8–10 | 30 | 68 | 98 | |
A total of 149 patients (45%) underwent bilateral
standard PLND. Unilateral metastases in the regional lymph nodes
were identified in 5 T3a and 3 T3b patients. Bilateral metastases
in the regional lymph nodes were identified in 3 T3b patients.
Postoperatively, 125 (40.0%) patients had undergone AHT and 35
(11.2%) patients had received both AHT and adjuvant
radiotherapy.
A total of 17 patients were lost during the
follow-up period. Slight stress urinary incontinence was identified
in almost every patient after the catheter was removed. In a
minimum follow-up of 12 months (range, 12–72), 216 and 74 patients
were completely continent after 3 months and 4–12 months,
respectively. A total of 22 patients used 1 precautionary pad daily
after 12 months postoperatively and achieved full continence
several months later. Neither postoperative persistent urinary leak
nor anastomotic stricture had occurred. A total of 139 patients had
undergone bilateral NVB sparing procedures and 132 were
followed-up. Overall, 29 patients were satisfied with their
erection, hardness and duration 12 months postoperatively. During
the same postoperative period of time, 17 patients had an erection
with inadequate hardness and duration. Younger patients (≤67 years
of age) had a more rapid continence recovery and a better
postoperative potency (Table
V).
 | Table VReturn of continence and potency are
age-related and better in younger males. |
Table V
Return of continence and potency are
age-related and better in younger males.
| Age ≤67 years | Age >67
years | Total | P-value |
|---|
| Complete
continence | | | | P<0.001 |
| 3 months
postoperatively | 120 | 96 | 216 | |
| 3–12 months
postoperatively | 22 | 52 | 74 | |
| Total | 142 | 148 | 290 | |
| Potency at 12
months postoperatively | | | | P<0.001 |
| Erectile
dysfunction | 33 | 53 | 86 | |
| Erection with
inadequate hardness and duration | 13 | 4 | 17 | |
| Satisfied
erection, hardness and duration | 22 | 7 | 29 | |
| Total | 68 | 64 | 132 | |
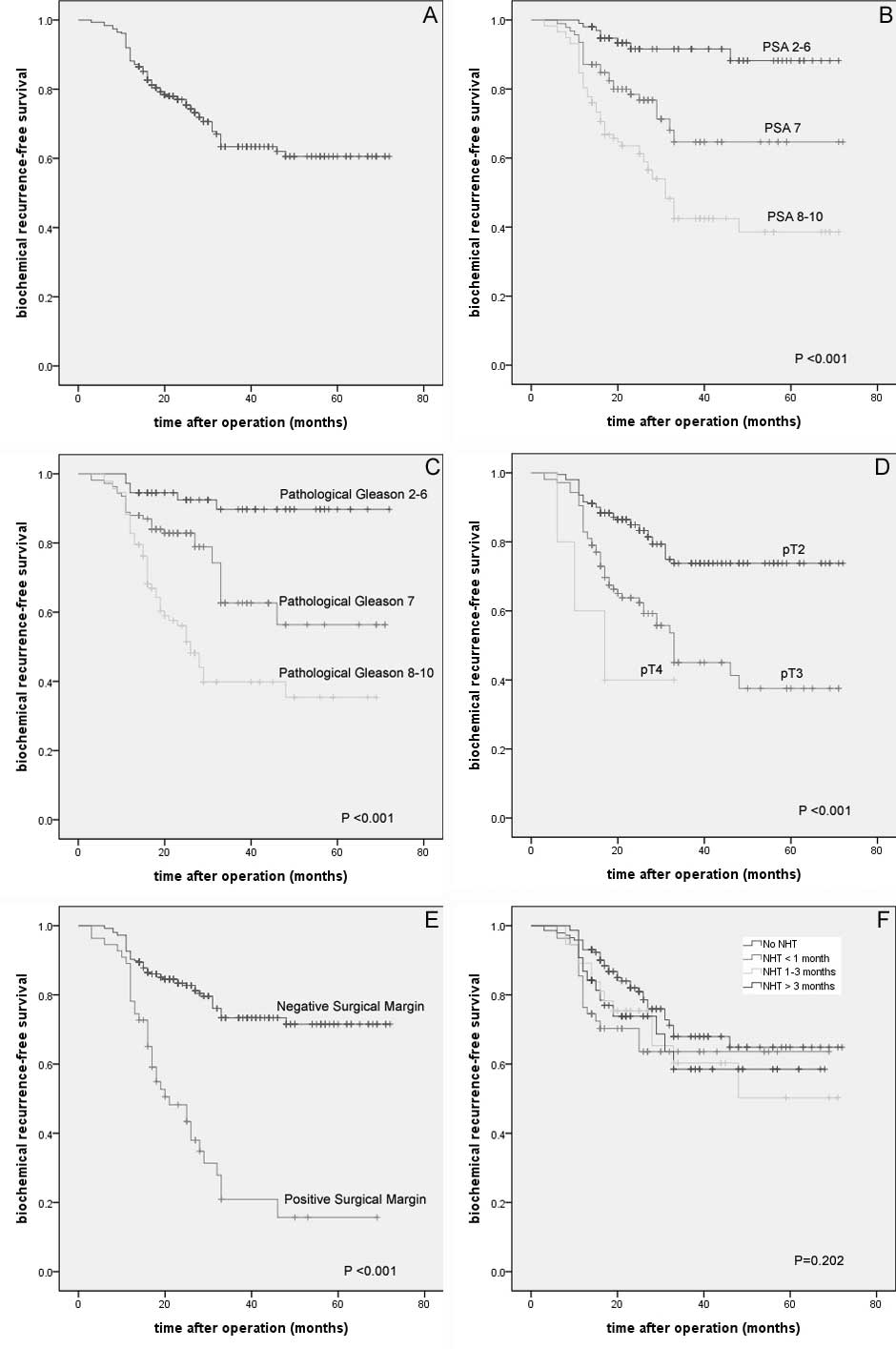
During the follow-up period of 12–72 months, the
patients survived and 89 (28.6%) patients were diagnosed with
biochemical recurrence for 2 consecutive PSA values ≥0.2 ng/ml. The
overall biochemical recurrence-free survival decreased during the
follow-up period. Multivariate analyses using the Cox proportional
hazard model identified the initial PSA value, PSM, pathological
stage and Gleason score as independent prognostic factors for
biochemical recurrence-free survival (Fig. 2A-E).
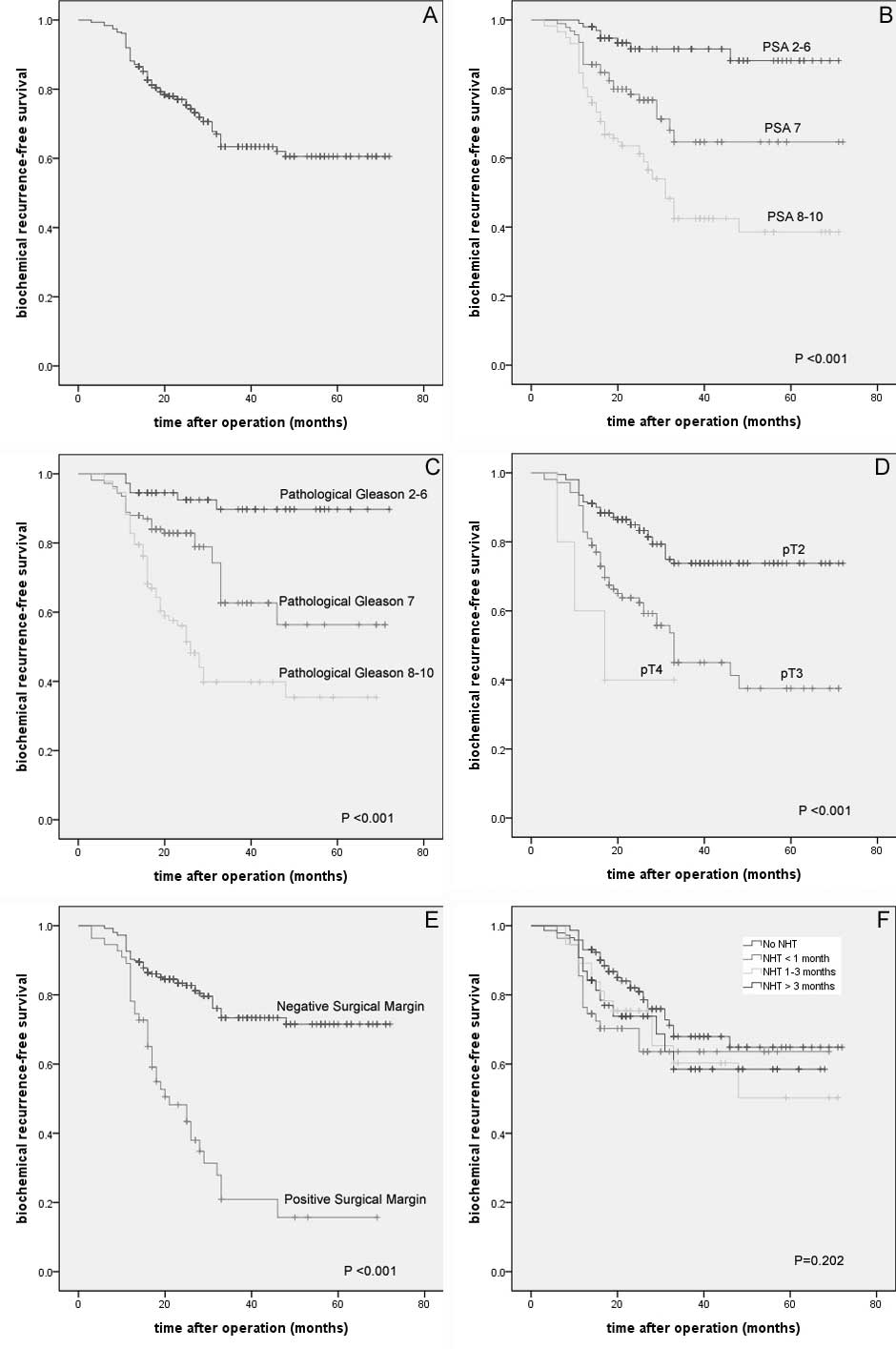 | Figure 2(A) The overall biochemical
recurrence-free survival. Biochemical recurrence-free survival
according to (B) initial PSA value (P<0.001, log-rank test), (C)
Gleason score (P<0.001, log-rank test), (D) pathological stage
(P<0.001, log-rank test), (E) surgical margin (P<0.001,
log-rank test) and (F) preoperative NHT (P=0.202, log-rank test).
PSA, prostate-specific antigen; NHT, neoadjuvant hormonal
therapy. |
Discussion
In 1997, the first studies of transperitoneal
laparoscopic radical prostatectomy (TLRP) and the initial
experience of ELRP were reported by Schuessler et al
(6) and Raboy et al
(7), respectively. In 2002,
Stolzenburg et al (5)
introduced their technique and experience of the endoscopic
extraperitoneal radical prostatectomy (EERPE). These authors
reported that extraperitoneal endoscopic access was able to prevent
intra-abdominal complications, including bowel injury, ileus or
intestinal adhesions, and combined the advantages of minimally
invasive laparoscopy and retropubic open prostatectomy.
Our initial 20 cases of laparoscopic radical
prostatectomy were performed using the transperitoneal approach in
2003. Although neither bowel injury nor ileus occurred, the
interference of the bowel and prevention of intraperitoneal
complications resulted in the extraperitoneal approach being
selected. There were enough cases of transperitoneal approach to
compare with the extraperitoneal approach. Our 329 cases of
successfully performed ELRP proves that the extraperitoneal
approach is a feasible and reproducible technique.
The initial 23 cases of running urethrovesical
anastomosis were performed using the single knot method (SKM)
(8). We found that the two suture
lines were easily interacted in the narrow Chinese pelvic section.
When the transperitoneal approach was adopted, intestinal canals
made the condition increasingly difficult. We adopted the single
needle method (SNM) (4) to
successfully perform the running urethrovesical anastomosis. We
used a UR-6 taper needle with 5/8 radian; this suitable needle was
small enough, allowing for easier rotation in the narrow pelvis.
Due to the low friction characteristic of the Monocryl, the sutures
glided smoothly under traction, and the poliglecaprone was strong
enough when the urethral stump and the bladder neck were brought
together with traction. Until the 8 o’clock position of the
posterior was sutured, we had not pulled the bladder neck with the
urethra immediately after every suture. The tension of anastomosis
was shared by several sutures, therefore dilaceration of the
bladder or the urethra was avoided. Correct tension of traction on
each suture followed with the locking suture at 9 o’clock was a key
point.
The majority of the temporary urinary leakages were
identified in the initial cases. Upon increasing experience,
temporary urinary leakage seldom occurred. The details of SNM and
initial results compared with the results of several other methods
of urethrovesical anastomosis that have been published (4). A short median time for anastomosis, a
short median placement time of the retropubic drain, no
postoperative persistent urinary leakage and no anastomotic
stricture indicated that SNM was a simple and efficient method.
Rozet et al (9), Stolzenburg et al (10), Eden et al (11) and Do et al (12) have reported their encouraging
experiences and results of laparoscopic radical prostatectomy. The
majority of our perioperative results were analogical with data
from the European studies (Table
I). In China, PSA monitoring has not been regularly inspected
in older males, thus a quantity of Chinese PCas were identified
with high PSA values and late-stages. The median PSA of 17
demonstrated in our study is a little higher than that in a number
of other published studies, we consider that this may be due to the
fact that there are higher proportions of pT3b and pT4 cases in our
patients.
The median age of our patients was 67 years old,
thus patients were divided into two groups at the age of 67. Our
follow-up data demonstrated that return of continence and potency
are age-related and yield better results in younger males (≤67
years of age), which is in accordance with other studies by
Stolzenburg et al (10), Hu
et al (13) and Mendiola
et al (14).
A number of Chinese urologists prefer to adopt
preoperative NHT in the interval between TURP or biopsy and radical
prostatectomy. In our study, over half of the patients had received
preoperative NHT for less or more than 3 months. Statistical
analysis demonstrated that preoperative NHT had a significant
effect on the pathological Gleason score and surgical margin, but
not on biochemical recurrence. This result is in accordance with
the 2011 EAU guidelines on PCa, which indicates that preoperative
NHT prior to radical prostatectomy does not provide a significant
overall survival advantage or a significant advantage in
disease-free survival over prostatectomy alone. However, NHT
substantially improves local pathological variables, including
pathological down-staging and PSMs.
Multivariate analyses using the Cox proportional
hazard model in this study demonstrated that biochemical
recurrence-free survival was statistically significantly correlated
with the initial PSA value, pathological Gleason score,
pathological stage and PSM. No significant correlation was
identified between biochemical recurrence-free survival, body mass
index, NHT, AHT and adjuvant radiotherapy, respectively. Since
bilateral standard PLND was not performed in all patients, we did
not analyse whether lymph node metastasis had a significant
independent correlation with biochemical recurrence-free survival.
A limitation of our study is that the sample size was small, and
that the study was a retrospective analysis with a short
postoperative follow-up period, which allowed for potential
selection bias. Large, prospective studies and long-term follow-up
are required to evaluate oncological and functional results of
Chinese patients.
In their study, Jemal et al (1) reported that the incidence of PCa in
Eastern Asia was 8.2 per 100,000 according to global cancer
statistics. A recent unpublished study in Beijing revealed that the
incidence of PCa may have been severely underestimated in China. A
total of 3,359 males with a mean age of 65±10 years received DRE
and PSA detection. Overall, 87 cases were identified with abnormal
DRE and/or PSA values and 61 cases received transrectal
ultrasound-guided biopsy. A total of 19 cases of PCa were diagnosed
and 11 cases were late-stage. The authors suggested that PSA
monitoring should be applied more widely in large- and medium-sized
cities of China. Due to the increase in Chinese PCa cases the
application of PSA detection may aid in the diagnosis of PCa, thus
an increasing number of urologists may employ ELRP in the
future.
Acknowledgements
This study was supported by the 50th General
Financial Grant from China Postdoctoral Science Foundation (Grant
no. 201150M1535) and the National Natural Science Foundation for
Distinguished Young Scholar (no. 30725040), China.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2
|
Gu FL: The incidences of benign prostatic
hyperplasia and prostatic cancer in China. Zhonghua Wai Ke Za Zhi.
31:323–326. 1993.PubMed/NCBI
|
|
3
|
Gu F: Epidemiological survey of benign
prostatic hyperplasia and prostatic cancer in China. Chin Med J
(Engl). 113:299–302. 2000.PubMed/NCBI
|
|
4
|
Zhang X, Ju Z, Wang C, et al: The single
needle method for urethrovesical anastomosis with strengthened
posterior fixation during laparoscopic radical prostatectomy. J
Huazhong Univ Sci Technolog Med Sci. 29:745–749. 2009. View Article : Google Scholar
|
|
5
|
Stolzenburg JU, Do M, Pfeiffer H, König F,
Aedtner B and Dorschner W: The endoscopic extraperitoneal radical
prostatectomy (EERPE): technique and initial experience. World J
Urol. 20:48–55. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schuessler WW, Schulam PG, Clayman RV and
Kavoussi LR: Laparoscopic radical prostatectomy: initial short-term
experience. Urology. 50:854–857. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Raboy A, Ferzli G and Albert P: Initial
experience with extraperitoneal endoscopic radical retropubic
prostatectomy. Urology. 50:849–853. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Van Velthoven RF, Ahlering TE, Peltier A,
Skarecky DW and Clayman RV: Technique for laparoscopic running
urethrovesical anastomosis: the single knot method. Urology.
61:699–702. 2003.PubMed/NCBI
|
|
9
|
Rozet F, Galiano M, Cathelineau X, Barret
E, Cathala N and Vallancien G: Extraperitoneal laparoscopic radical
prostatectomy: a prospective evaluation of 600 cases. J Urol.
174:908–911. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stolzenburg JU, Kallidonis P, Minh D, et
al: Endoscopic extraperitoneal radical prostatectomy: evolution of
the technique and experience with 2400 cases. J Endourol.
23:1467–1472. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Eden CG, Neill MG and Louie-Johnsun MW:
The first 1000 cases of laparoscopic radical prostatectomy in the
UK: evidence of multiple ‘learning curves’. BJU Int. 103:1224–1230.
2009.PubMed/NCBI
|
|
12
|
Do M, Haefner T, Liatsikos E, et al:
Endoscopic extraperitoneal radical prostatectomy after previous
transurethral resection of prostate: oncologic and functional
outcomes of 100 cases. Urology. 75:1348–1352. 2010. View Article : Google Scholar
|
|
13
|
Hu JC, Elkin EP, Pasta DJ, Lubeck DP,
Kattan MW, Carroll PR and Litwin MS: Predicting quality of life
after radical prostatectomy: results from CaPSURE. J Urol.
171:703–707. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mendiola FP, Zorn KC, Mikhail AA, Lin S,
Orvieto MA, Zagaja GP and Shalhav AL: Urinary and sexual function
outcomes among different age groups after robot-assisted
laparoscopic prostatectomy. J Endourol. 22:519–524. 2008.
View Article : Google Scholar
|