Introduction
Primary squamous cell carcinoma of the liver is
rare. More than 20 cases have been reported since the first case
was described in 1934 by Imai (1).
The pathogenesis of the disease is undetermined. Previous studies
have reported that potentially related diseases, including
congenital cyst of the liver (2–8),
calculus of the intrahepatic duct (9), hepatic cirrhosis (10,11),
Caroli’s disease (12) and hepatic
teratoma (1), are rare. However,
hepatic primary squamous carcinoma without latent hepatic injury
has also been reported (13). This
disease has a high malignancy rate and poor prognosis, and survival
is typically no longer than one year (12). In the present case study, a patient
suffered from biliary calculosis for over 20 years. The patient
underwent chest, abdominal and pelvic CT scans and gynecological
examination to preclude other primary foci. The study was approved
by the Ethics Committee of Shandong Cancer Hospital, Jinan, China.
Written informed consent was obtained from the patient. The
postoperative pathology and immunohistochemistry confirmed the
disease as liver primary squamous cell carcinoma. Combined with the
patient’s history of calculosis of the biliary tree for 20 years,
we determined that the mechanism of carcinogenesis was correlated
with persistent stimulation induced by chronic biliary infection
caused by calculus of the intrahepatic duct. However, the
transformation mechanism from cholangiocellular carcinoma to
squamous carcinoma is undetermined and requires further study. In
the present study, the patient underwent liver tumor radiofrequency
ablation, but the abdominal pain remained evident following the
surgery. As the patient’s physical condition was too weak to
tolerate generalized chemotherapy, local radiotherapy and
supportive therapy is being conducted, and the patient’s pain has
already been relieved.
Case report
A 60-year-old female patient underwent
cholecystectomy due to cholecystolithiasis with chronic
cholecystitis in 1988. In May 2010, the patient experienced
repeated pain without obvious cause in the right upper quadrant,
accompanied by fever, nausea without vomiting, hypodynamia,
anorexia, abdominal distension, diarrhea, shivers, jaundice and
lumbar-dorsal radiating pain. A CT examination revealed a calculus
of the intrahepatic duct and chronic cholangitis. A partial
resection of the hepatic left lobe was carried out on July 29th,
2010. The postoperative pathology indicated left hepatic
cholangeitis and calculus of the bile duct. A magnetic resonance
imaging (MRI) examination performed in December 2010 indicated that
the primary focus was in the left liver at a size of 4.0×3.0×3.0
cm, with reinforcement in the arterial phase. The examination of
tumor biomarkers revealed 7.6 μg/l AFP, 1.1 μg/l CEA
and 275.9 U/ml CA19-9. The tumor resection of the left hepatic
external lobe, exploration of the biliary tract and T-tube drainage
were performed on December 31st, 2010. A calculus with a diameter
of 0.2 cm and a grey tumor 2.0×1.5 cm in the cross section without
peplos in the surroundings of the tumor were observed and the
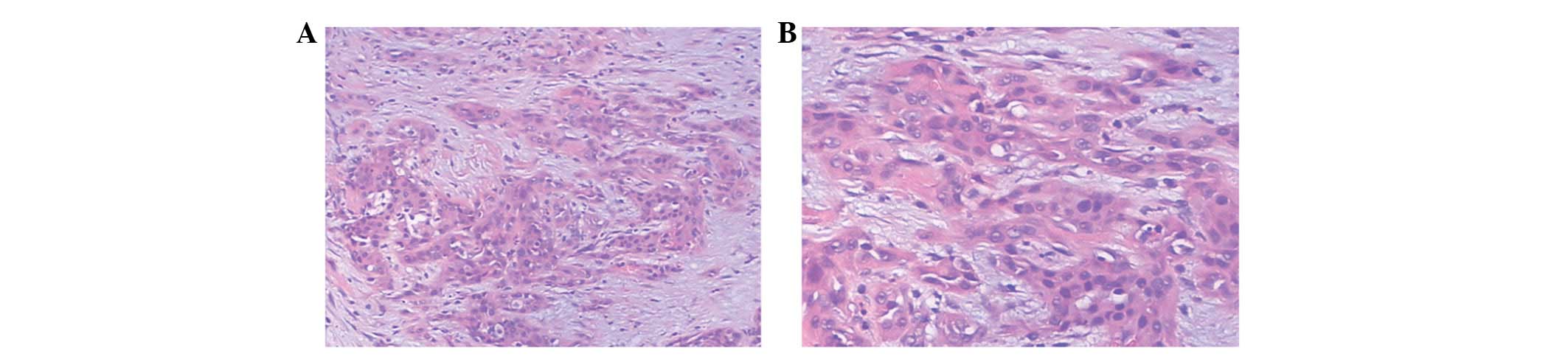
texture was hard. Microscopically (Fig.
2), the tumor tissue was accumulated in the glandular tube, the
lumens contained mucilage, the cancer cells were cubic or columnar,
the nuclei were round or orbicular-ovate, there was karyomegaly and
anachromasis, evident atypia and the surroundings indicated
infiltrative growth affecting the nerves. Tumor growth was not
observed in cancerous tissue, and there was no pseudo-lobule
structure in the remaining liver. Masson (+), AB (+) and reticulum
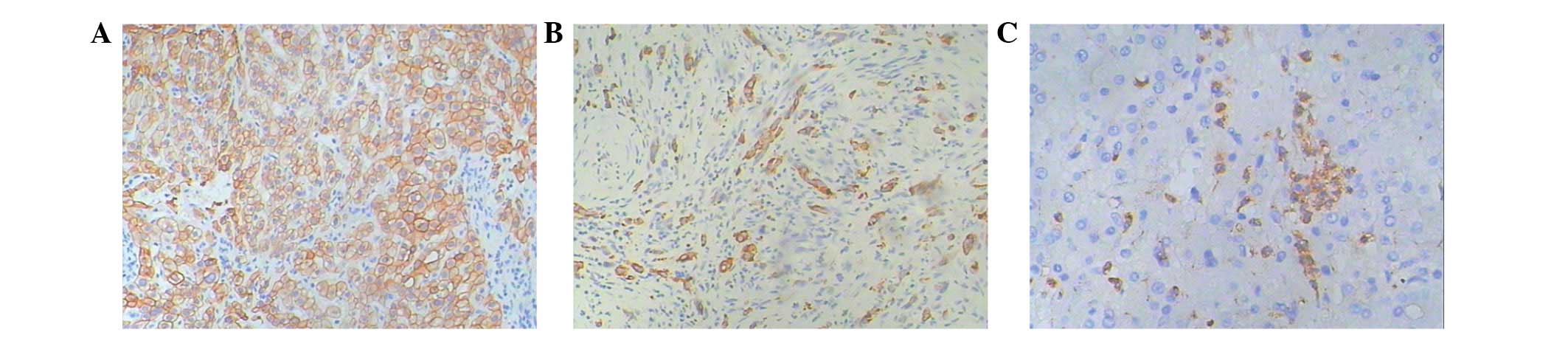
staining (−) were performed. The immunohistochemistry results were
as follows (Fig. 3): Hep-1(+++),
HBsAg(−), CK18(+), CK19(++), CD34(−), HbeAg(−), pCEA(+++),
β-catenin(−), MUC-1(−), myoglobin(−), Gly-3(−) and MAT1(−). The
pathological diagnosis was intrahepatic cholangiocarcinoma of the
hepatic left lobe with mild differentiation and calculus of the
bile duct. The patient’s symptoms were relieved following the
surgery. In June 2011, the patient experienced pain in the right
upper quadrant without any evident cause, and the pain started to
radiate to the back, accompanied by nausea, vomiting, hypodynamia
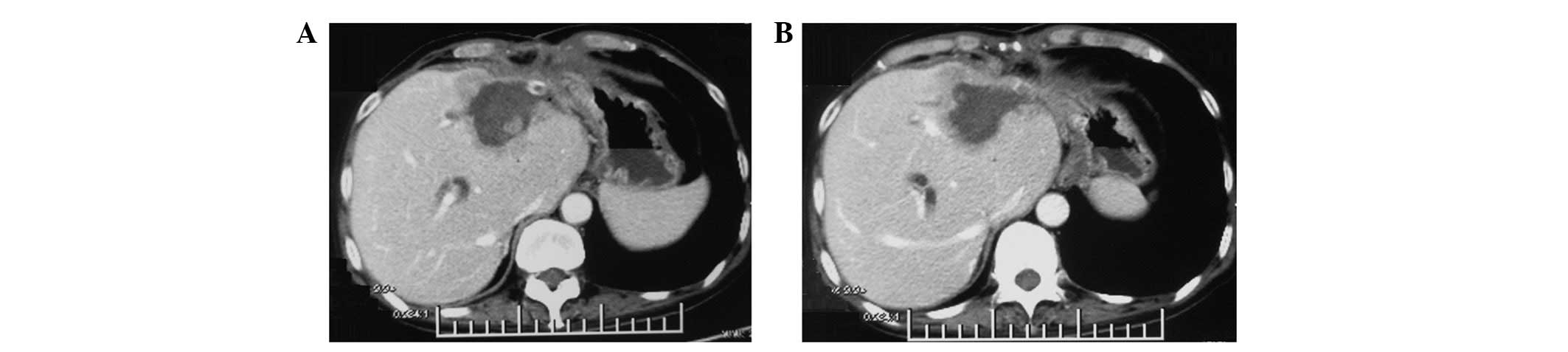
and anorexia. An abdominal CT examination (Fig. 1) was performed and revealed an
abnormal density shadow in the medial segment of the left lobe of
the liver following the tumor resection of the hepatic left lobe,
which was considered to be the postoperative recurrence of
cholangiocellular carcinoma of the hepatic left lobe. Examination
of the tumor markers indicated 4.63 μg/l AFP, 191.5 U/ml
CA125 and 1557.8 U/ml CA19-9. The patient underwent hepatic tumor
biopsy and hepatic tumor radiofrequency ablation on July 4th, 2011.
The tumor was located in the junctional zone of the hepatic left
internal lobe and right anterior lobe with a hard texture at a size
of 1.5×1.2×0.5 cm, which was closely adhered to partial gastric
serous tunic and peripheral abdominal wall. Considering the extra
hepatic encroachment of the tumor, the location and surroundings of
the tumor made surgical separation and radical resection difficult;
therefore, radiofrequency ablation of the left hepatic tumor was
carried out. Postoperative pathology revealed a mass of
grayish-white and grayish-yellow tissue with a hard texture and a
size of 1.2×1.2×0.4 cm. Microscopically, infiltration of poorly
differentiated carcinoma tissue in the proliferative fibrous tissue
and interaction between foam cells and multinucleated giant cells
in the mesenchyme were observed (Fig.
4). The immunohistochemical staining of the tumor cells
revealed CD68(−), Ki-67(+, <25%), CK(+), CK590(+) (Fig. 5), which is consistent with liver
squamous cell carcinoma.
Currently, the patient continues to feel pain in the
right upper quadrant of the abdomen, accompanied by fever, nausea,
vomiting, hypodynamia, anorexia without jaundice, abdominal
distension and diarrhea, with poor diet and sleeping. The patient’s
weight has reduced by ∼15 kg in 1 year. Nutritional therapy was
administered, and radiotherapy of the hepatic tumor focus and the
periphery of the invaded structure were performed at a total dose
of 36 Gy 20 times. The patient’s abdominal pain was markedly
relieved and the abdominal mass was reduced to a size of 4.0×5.0
cm, and we are currently following up the patient.
Discussion
Incidence of primary squamous cell carcinoma of the
liver is rare and the pathogenesis of the disease is undetermined.
Previous studies have reported that potentially related diseases,
including congenital cyst of the liver (7,8),
calculus of the intrahepatic duct (9), hepatic cirrhosis (11), Caroli’s disease (12) and hepatic teratoma (1), are also rare.
In the present study, the patient underwent chest,
abdominal and pelvic CT scans and gynecological examination to
preclude other primary foci. The postoperative pathology and
immunohistochemistry confirmed the disease as liver primary
squamous cell carcinoma. The patient’s primary operative pathology
revealed hepatic cholangiocellular carcinoma. The tumor recurrence
occurred in half a year, and tumor pathological biopsy and
immunohistochemistry revealed the tumor to be hepatic primary
squamous carcinoma. The transformation from hepatic
cholangiocellular carcinoma to liver squamous carcinoma is
extremely rare, and there are no similar studies. Combined with the
patient’s history of calculosis of the biliary tree for 20 years,
we determined that the mechanism of carcinogenesis was correlated
with persistent stimulation induced by chronic biliary infection
caused by calculus of the intrahepatic duct. However, the
transformation mechanism from cholangiocellular carcinoma to
squamous carcinoma is undetermined and requires further study.
The morbidity of hepatic primary squamous has no
evident gender differentiation and mainly occurs in 50–70-year-old
patients. The clinical symptoms are commonly reported as stomach
ache or jaundice, accompanied by anorexia, hypodynamia, nausea,
vomiting and physical athrepsia. Swelling of the liver may be
palpable in the physical examination. Currently, the definitive
diagnosis mainly relies on pathology and immunohistochemistry.
In cases of liver primary squamous carcinoma, due to
its high malignancy, poor prognosis and late definitive diagnosis,
survival is generally no longer than 1 year (11). As the incidence of liver primary
squamous carcinoma is extremely low, its therapeutic regime has not
been agreed. Reported therapeutic methods include surgical
resection, generalized chemotherapy, radiotherapy, hepatic arterial
chemoembolization (HACE) and combinations of these therapies. In
the present study, the patient underwent liver tumor radiofrequency
ablation, but the patient’s abdominal pain continued after the
surgery. As the patient’s physical condition was too weak to
tolerate generalized chemotherapy, local radiotherapy and
supportive therapy is being carried out, and the patient’s pain has
already been relieved. The current viewpoint is that HACE combined
with radiotherapy or generalized chemotherapy may extend survival
in patients with primary squamous carcinoma, whereas the timely
total surgical resection of tumor is the key to preventing invasive
tumor growth and further surgical resection, systematic generalized
chemotherapy or HACE may be used for patients with postoperative
recurrence of the disease. We determined that local radiotherapy
may be used to relieve symptoms in patients who are unable to
undergo resection of the tumor or tolerate generalized
chemotherapy.
Acknowledgements
This study was financially supported
by grant no. 2011CB504302 from the 973 Program of China and grant
nos. ZR2010HL018 and Y2008C30 from the Natural Science Foundation
of Shandong. We appreciate the valuable comments from other members
of our laboratories.
References
|
1.
|
T ImaiEin Fall von zystischem Teratom der
Leber, in welchem Plattenepithelkrebs entstandTrans Soc Pathol
Jap245785801934(In German).
|
|
2.
|
MJ LynchMK McLeodL WeatherbeeJR GilsdorfKS
GuiceFE EckhauserSquamous cell cancer of the liver arising from a
solitary benign nonparasitic hepatic cystAm J
Gastroenterol8342643119883279761
|
|
3.
|
J BanburyKC ConlonR GhosseinMF
BrennanPrimary squamous cell carcinoma within a solitary
nonparasitic hepatic cystJ Surgl
Oncol57210212199410.1002/jso.29305703167967614
|
|
4.
|
M MonteagudoG VidalM MorenoSquamous cell
carcinoma and infection in a solitary hepatic cystEur J
Gastroenterol
Hepatol1010511053199810.1097/00042737-199812000-000129895053
|
|
5.
|
DJ VickZD GoodmanKG IshakSquamous cell
carcinoma arising in a ciliated hepatic foregut cystArch Pathol Lab
Med12311151117199910539920
|
|
6.
|
A FurlanettoAP Dei TosSquamous cell
carcinoma arising in a ciliated hepatic foregut cystVirchows
Archiv441296298200210.1007/s00428-002-0668-z12242527
|
|
7.
|
H YagiM UedaS KawachiSquamous cell
carcinoma of the liver originating from non-parasitic cysts after a
15 year follow-upEur J Gastroenterol
Hepatol1610511056200415371931
|
|
8.
|
X ZhangZ WangY DongSquamous cell carcinoma
arising in a ciliated hepatic foregut cyst: case report and
literature reviewPathol Res
Pract205498501200910.1016/j.prp.2008.12.00319410383
|
|
9.
|
E SongMC KewT GrieveC IsaacsonJA
MyburghPrimary squamous cell carcinoma of the liver occurring in
association with
hepatolithiasisCancer53542546198410.1002/1097-0142(19840201)53:3%3C542::AID-CNCR2820530328%3E3.0.CO;2-36692259
|
|
10.
|
Y AraseY EndoM HaraH KumadaK IkedaA
YoshibaHepatic squamous cell carcinoma with hypercalcemia in liver
cirrhosisActa Pathol Jpn3864365019882463731
|
|
11.
|
N YukiY HijikataM KatoK KawaharaK
WakasaSquamous cell carcinoma as a rare entity of primary liver
tumor with grave prognosisHepatol
Res36322327200610.1016/j.hepres.2006.08.00416978916
|
|
12.
|
M SpaggiariF Di BenedettoR BallarinPrimary
squamous cell carcinoma of the liver associated with Caroli’s
disease: a case reportOnkologie34193195201121447978
|
|
13.
|
R KajiN SasakiI TateishiA case report of
primary hepatic squamous cell carcinoma that remarkably responded
to low dose arterial injection of anti-cancer drugsKurume Med
J507175200310.2739/kurumemedj.50.7112971268
|