Introduction
Gastric cancer is the second most common cancer and
the third leading cause of mortality from cancer in China (1). There are more new cases diagnosed in
China than in any other country each year. Complete surgical
resection is the only potential curative treatment for gastric
cancer. Nonetheless, the long-term results of resectable gastric
cancer are still poor. More than 50% of patients will develop
locoregional recurrences and/or distant metastases within 1–3 years
of curative surgery and patients with serosa-infiltrating and/or
node-positive cancer are at a particularly high risk of recurrence
(2,3). Levels of interest in adjuvant
treatment have increased in the past few decades. In spite of the
notable improvement demonstrated by Intergroup 116 (adjuvant
chemoradiation) (4), MAGIC
(neoadjuvant and adjuvant chemotherapy) (5) and ACTS-GC (adjuvant S1) trials
(6), almost half of gastric cancer
patients will succumb to the condition within three years of
surgery. These trials all showed the same pattern of cancer
recurrence. The patients were treated either by surgery alone or
surgery plus peri- or postoperative chemoradiotherapy; however,
peritoneal failure remained the most common pattern of first
recurrence (7). Therefore, it is
essential to reinforce efforts to find more effective adjuvant
treatment modalities.
Systemic chemotherapy (SCT) possesses the
theoretical advantage of treating undetectable cancer cells that
have spread systemically at the time of surgery and will ultimately
represent a major source of treatment failure for patients with
resectable gastric cancer. Recent meta-analyses (8–10) have
demonstrated that adjuvant SCT is effective in treating gastric
cancer. In addition, intraperitoneal chemotherapy (IPCT) has
several unique pharmacokinetic advantages which are able to
eradicate free cancer cells and micrometastatic or microscopic
residual focus in the peritoneal cavity. IPCT also reduces
recurrence and therefore combines the effects of intraportal
chemotherapy on the liver with a direct effect on the peritoneum
and the resection site. Adjuvant IPCT has also been shown to be a
valuable strategy in treating gastric cancer (11–13).
Therefore, cumulative data suggests that benefits may be obtained
by combining SCT and IPCT to decrease both local and distant
metastases simultaneously with different targets, different times
of effect and non-overlapping side effects. Taken together, SCT and
IPCT appear well-suited for combined use; therefore, it is rational
to combine SCT with IPCT in an adjuvant setting for gastric cancer
(13). Moreover, the benefit of
this combined strategy has been verified by many convincing
clinical trials in ovarian cancer (14).
Therefore, we conducted a study to evaluate the
efficacy and feasibility of this novel adjuvant chemotherapy
approach in high-risk patients with locally advanced gastric
cancer. This study was approved by the ethics committees of The
First Affiliated Hospital of Wenzhou Medical College.
Materials and methods
Patients
All patients enrolled were required to have
adenocarcinoma of the stomach confirmed histologically and undergo
a curative resection with D2 lymphadenectomy and negative margins
(R0 resection). Enrolled patients were also required to have
serosa-infiltrating (pT3+ stage) and/or regional lymph
node-positive (pN+) cancer with no distant metastases (stage II
through IVM0, according to the 2002 staging criteria of the
American Joint Commission on Cancer) (15). Eligibility was determined by
reviewing the study forms, operative and pathology reports
carefully. Patients with any overt evidence of peritoneal spread
were excluded. Additional requirements for eligibility were an
Eastern Cooperative Oncology Group performance status ≤1; age of
20–80 years; adequate hematological levels (neutrophils
≥2×109/l; hemoglobin ≥900 g/l; platelets
≥100×109/l); hepatic function (bilirubin ≤25
μmol/l; aspartate aminotransferase and alanine
aminotransferase ≤2.5 × upper normal limit); renal function
(creatinine ≤130 μmol/l); cardiac function (New York Heart
Association class <II); no previous malignancies other than
superficial skin cancer or in situ cervical carcinoma and no
previous treatments such as neoadjuvant chemotherapy or
radiotherapy. Patients were enrolled in this study no earlier than
1 week and no later than 3 weeks after surgery. Metastatic disease
was ruled out by computed tomography (CT) scans of the brain, chest
and whole abdomen prior to surgery. All patients signed an informed
consent prior to treatment.
Treatment
ACSIP started within 1–3 weeks of surgery. The
course of treatment was repeated every 28 days for up to 6 cycles.
SCT consisted of intravenous oxaliplatin 85 mg/m2 on day
1 over a 2-h period followed by LV 200 mg/m2 and 5-FU
450 mg/m2 for 3 days (days 1 to 3). Prior to every IPCT,
peritoneal catheterization was performed blindly under local
anesthesia using the Seldinger technique based on previous
ultrasonography localization of the puncture site. Intraperitoneal
drug delivery was administered through a single-lumen central
venous catheter (Arrow International, Inc., Reading, PA, USA)
inserted into the abdominal cavity. IPCT consisted of 5-FU 600
mg/m2 on days 4 to 5 followed by CDDP 40
mg/m2 on day 5. Prior to IPCT, 100 ml 0.9% normal saline
with 10 mg dexamethasone was instilled into the peritoneal cavity.
5-FU and CDDP were diluted in 1,000 ml and 500 ml 0.9% normal
saline, respectively. Patients were asked to change their body
position every 15 min for 2 h following the intraperitoneal
administration. The fluid was left in the peritoneal cavity until
the next infusion. The catheter was removed 24 h after the last
infusion. If grade 3–4 hematological toxicity occurred, the doses
of SCT were decreased by 20%. If grade 3–4 non-hematological
toxicity occurred, or if toxicity (hematological or
non-hematological) persisted for more than 2 weeks, the doses of
SCT and IPCT were both decreased by 20%.
Follow-up evaluation
Comprehensive baseline assessments, including a
complete medical history, physical examination, complete blood cell
count, blood chemistries, tumor markers (CEA, CA19.9 and CA125),
and brain, chest and whole abdomen CT scans were conducted prior to
both surgery and treatment for every patient. During the treatment,
patients were checked from weekly to monthly intervals by physical
examination, toxicity assessment and blood examination. Toxicities
were evaluated following the National Cancer Institute Common
Toxicity Criteria, version 2.0. Follow-up was performed at 3-month
intervals for 2 years, 6-month intervals for 3 years and yearly
thereafter. Follow-up examinations consisted of physical
examination, complete blood cell count, blood chemistries, tumor
markers and abdomino-pelvic ultrasonography and/or CT. Chest X-rays
or CT scans, if indicated clinically, were performed every 6 months
in the first 3 years then yearly to ensure recurrence data
collection. A radionuclide bone scan and endoscopy were performed
if clinically indicated. The sites and date of first relapse and
the date of death, if the patient succumbed to their condition,
were recorded. Recurrence was confirmed by clinical, radiological
and histological examinations (whenever feasible). Typical nodules
in liver or lung with imaging studies or typical lesions in the
radionuclide bone scan and MRI or plain X-ray were accepted as
relapse without histological confirmation. Patterns of recurrence
reported in this study represent first sites of documented
recurring disease following curative resection, including
locoregional, peritoneal, hepatic and other distant metastasis.
Disease-free survival (DFS) and overall survival (OS) rates were
measured from the date of surgery. DFS was measured to the date of
recurrence and OS was defined as the time from surgery to the date
of death from any cause. DFS and OS rates were estimated using the
Kaplan-Meier method.
Results
Patient characteristics
Between June 2003 and December 2008, a total of 67
patients were enrolled in the study. Five patients (7.5%) were
excluded from the analysis: one had a positive surgical margin; one
refused to start treatment; two were lost to follow-up evaluation
during ACSIP and one had protocol violation, thus the analyses were
carried out in the remaining 62 eligible patients. For the 62
patients, the median age was 56 years (range 32–77) with 45 males
and 17 females. The majority of patients had serosa-infiltrating
(83.9%) and/or node-positive (87.1%) cancer (Table I).
 | Table I.Patient and tumor characteristics
(n=62). |
Table I.
Patient and tumor characteristics
(n=62).
|
Characteristics | No. of patients
(%) |
|---|
| Gender | |
| Male | 45 (72.6) |
| Female | 17 (27.4) |
| Age (years) | |
| Median | 56 |
| Range | 32–77 |
| Tumor location | |
| Upper third of
stomach | 12 (19.4) |
| Middle third of
stomach | 39 (62.9) |
| Lower third of
stomach | 11 (17.7) |
| Type of
gastrectomy | |
| Subtotal | 42 (67.7) |
| Total | 20 (32.3) |
| Histological
type | |
|
Well-differentiated | 2 (3.2) |
| Moderately
differentiated | 16 (25.8) |
| Poorly
differentiated | 44 (71.0) |
| Pathological T
stage | |
| pT1 | 1 (1.6) |
| pT2 | 9 (14.5) |
| pT3 | 51 (82.3) |
| pT4 | 1 (1.6) |
| Pathological node
status | |
| N0 | 8 (12.9) |
| N1 | 41 (66.1) |
| N2 | 9 (14.5) |
| N3 | 4 (6.5) |
| AJCC stage
(2002) | |
| II | 19 (30.6) |
| IIIA | 30 (48.4) |
| IIIB | 8 (12.9) |
| IV | 5 (8.1) |
Survival
At the time of survival analysis, the median
follow-up time for this study was 45 months (range 7–101). At
present, 37 patients are still alive, with 35 of them free of
recurrence. There are 2 patients with documented recurrence who are
still alive. During follow-up, 25 patients succumbed to their
condition and 2 of them succumbed without evidence of recurrence or
metastasis (one from cardiovascular disease and the other for
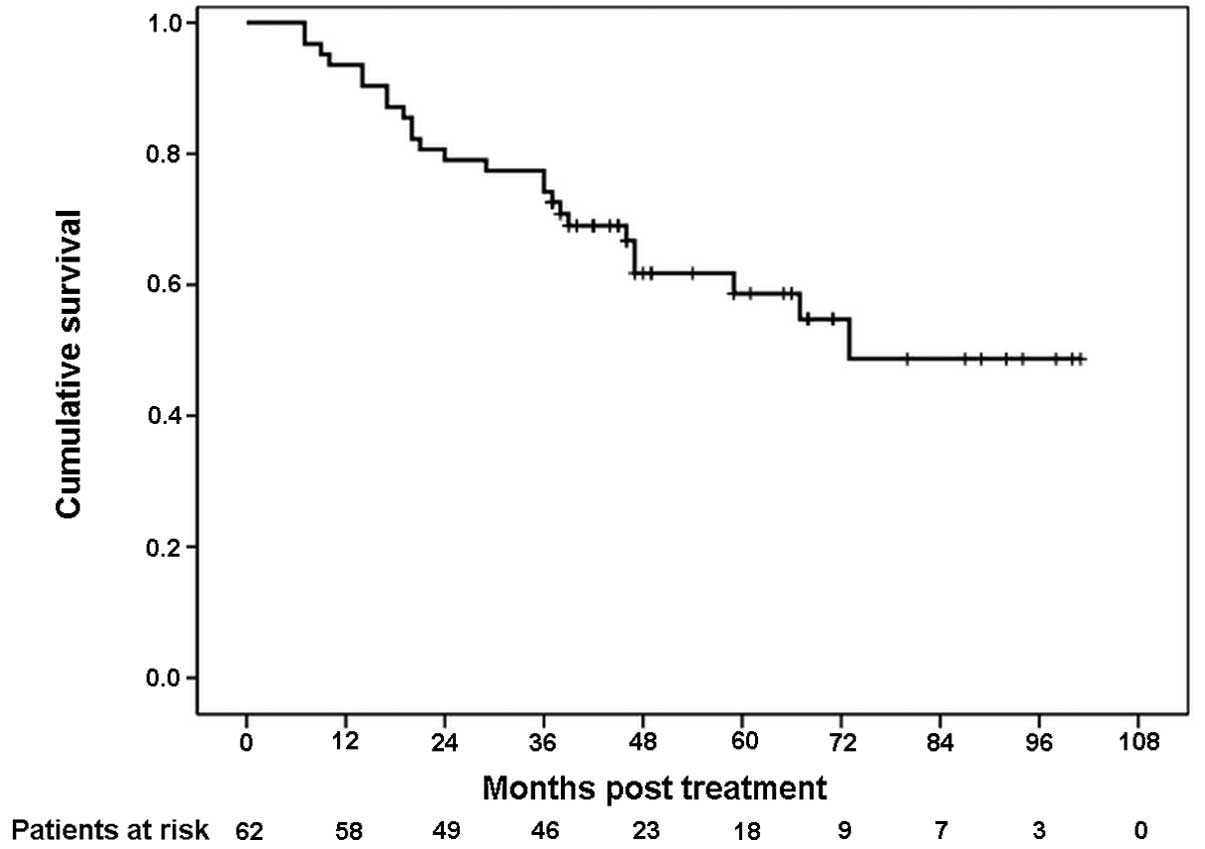
unknown reasons). The 3-year DFS rate was 66.1% (Fig. 1). The 3-year OS rate was 74.2%
(Fig. 2).
Relapse
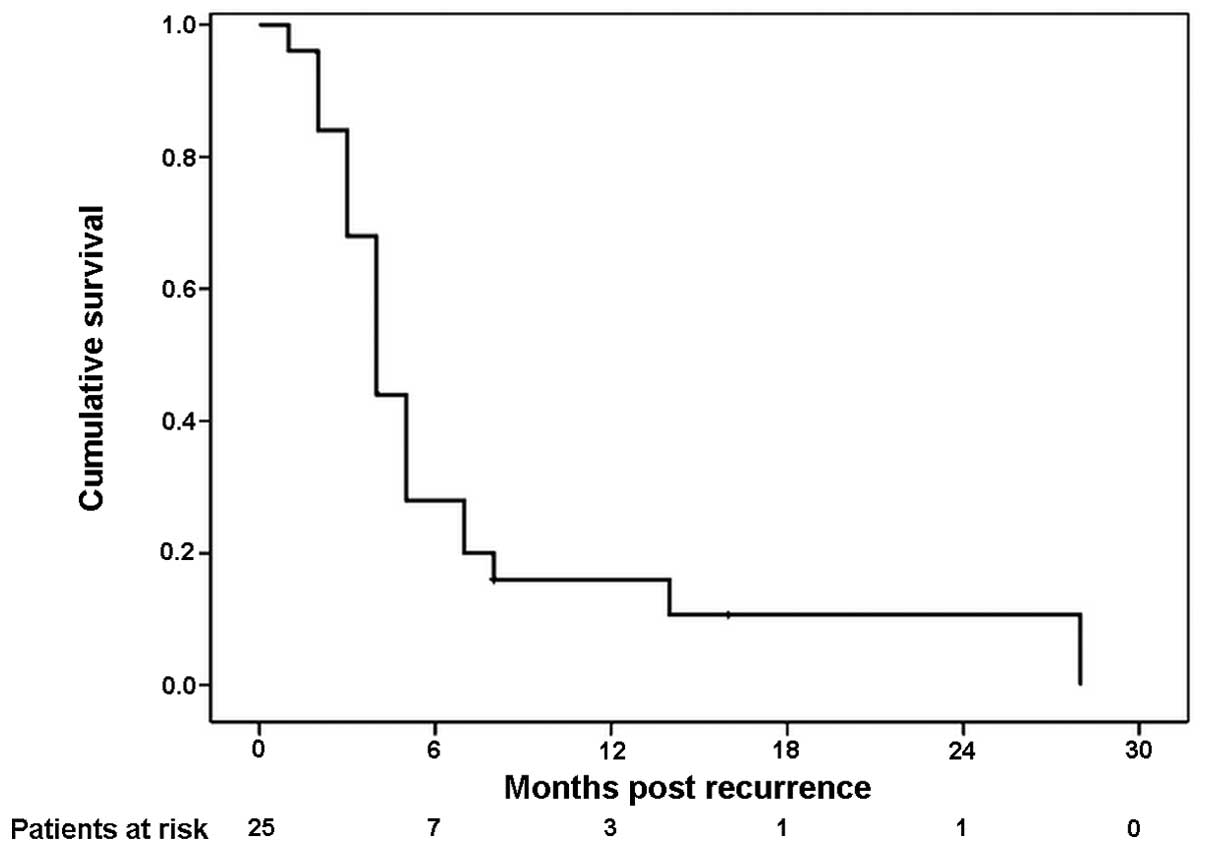
During follow-up, 25 patients (40.3%) eventually
relapsed and 23 patients succumbed to disease recurrence. As it
concerns the sites of first treatment failure, among the 25
patients, 6 (24.0%) and 3 (12.0%) of them experienced initial
peritoneal and hepatic recurrence, respectively, 5 patients (20.0%)
had locoregional relapse and 11 patients (44.0%) had other distant
metastases (Table II). Twenty-one
patients (91.3%) succumbed to their condition within 1 year of the
diagnosis of recurrence. The median time from recurrence to death
was 4 months (Fig. 3).
 | Table II.Sites of first treatment failure
(n=25). |
Table II.
Sites of first treatment failure
(n=25).
| Sites | No. of patients
(%) |
|---|
| Locoregional | 5 (20.0) |
| Peritoneal | 6 (24.0) |
| Hepatic | 3 (12.0) |
| Other distant
metastases | 11 (44.0) |
Toxicity and surgical complications
Overall, adverse toxicities were relatively uncommon
and they were generally mild to moderate. Neutropenia (8.1%),
diarrhea (4.8%), nausea (1.6%), vomiting (1.6%) and peripheral
neuropathy (1.6%) were the most common grade 3–4 toxicities. No
treatment-related mortality was observed (Table III). Surgical complications were
observed in 5 out of 62 patients (8.1%): anastomotic leakage in 2;
intra-abdominal abscess in 1; wound infection in 1 and pancreatitis
in 1. Treatment was delayed in 6 of the 62 patients (9.7%) due to
toxicities and/or surgical complications; however, the toxicities
and surgical complications were all manageable. Fifty-five (88.7%)
out of the 62 patients completed more than 4 cycles of ACSIP and 48
patients (77.4%) completed 6 cycles. In addition, 4 patients
completed 3 cycles of ACSIP, and 3 patients completed 2 cycles. The
primary reasons for 14 patients (22.6%) not completing 6 cycles of
ACSIP were patient refusal (6 patients), disease progression (2
patients), toxicities (1 patient), surgical complications (1
patient), catheter-related complications (1 patient) and other
reasons (3 patients).
 | Table III.Toxicities from treatment (n=62). |
Table III.
Toxicities from treatment (n=62).
| Toxicities | Grade 1–2, n
(%) | Grade 3–4, n
(%) | All,n (%) |
|---|
| Hematological | | | |
| Neutropenia | 9 (14.5) | 5 (8.1) | 14 (22.6) |
| Anemia | 11 (17.7) | 0 | 11 (17.7) |
|
Thrombocytopenia | 10 (16.1) | 0 | 10 (16.1) |
|
Non-hematological | | | |
| Stomatitis | 4 (6.5) | 0 | 4 (6.5) |
| Diarrhea | 5 (8.1) | 3 (4.8) | 8 (12.9) |
| Nausea | 4 (6.5) | 1 (1.6) | 5 (8.1) |
| Vomiting | 5 (8.1) | 1 (1.6) | 6 (9.7) |
| Distention | 3 (4.8) | 0 | 3 (4.8) |
| Abdominal
pain | 1 (1.6) | 0 | 1 (1.6) |
| Impaired liver
function | 3 (4.8) | 0 | 3 (4.8) |
| Impaired renal
function | 2 (3.2) | 0 | 2 (3.2) |
| Peripheral
neuropathy | 6 (9.7) | 1 (1.6) | 7 (11.3) |
Discussion
In the past decades, studies on adjuvant SCT for the
treatment of resectable gastric cancer have shown conflicting
results (8). Adjuvant SCT has not
become the standard of care for gastric cancer except with S1 in
Japan following the publication of the results of the ACTS-GC trial
(6,16). In addition, there is limited good
quality evidence to determine the role of adjuvant IPCT in gastric
cancer (17). The optimal adjuvant
chemotherapy approach for gastric cancer such as SCT, IPCT alone or
in combination has not yet been well-defined and there is no widely
accepted chemotherapeutic regimen. Based on the recurrence patterns
following curative resection, the rationale and advantage for
combined SCT and IPCT in an adjuvant setting for gastric cancer is
evident. In addition, the efficacy and feasibility of combined SCT
and IPCT have been well-established in other intra-abdominal
malignancies including colon (18)
and ovarian cancer (14),
particularly in the latter, for which convincing clinical trials
have confirmed the improvement in survival.
Despite the attractive rationale for the combination
of adjuvant SCT and IPCT, clinical experience with this treatment
modality in gastric cancer is limited. To our knowledge, there were
only a few earlier studies available exploring the use of ACSIP in
gastric cancer. The earliest was by Atiq et al (19), published in 1993. This group
assessed postoperative adjuvant intraperitoneal CDDP and 5-FU and
systemic 5-FU chemotherapy in patients with resected gastric
cancer. In that study, 16 out of 35 patients experienced
recurrence, and 18 remained alive free of disease with a 3-year
survival rate of 50.0%. The treatments were also associated with
altered metastatic patterns (decreased incidence of peritoneal
spread and liver metastases). In another study by Zuo et al
(20), a statistically significant
improvement in 3-year survival was reported for the adjuvant
intraperitoneal hyperthermic chemoperfusion combined with
intravenous chemotherapy group; the 3-year survival rate was 83.0%
in the combined group compared with 61.0% in the adjuvant
intravenous chemotherapy alone group (P<0.05). Recently, a
retrospective study by Shi et al (21) revealed that the 5-year OS rate in
the adjuvant systemic chemotherapy combined with intraperitoneal
perfusion chemotherapy (IP+) group was significantly better than
that in the systemic chemotherapy only (IP-) group (60.4 vs. 42.9%;
P= 0.001). In addition, the average progression-free survival in
the IP+ group was significantly longer than that in the IP- group
(60.5 vs. 46.2 months; P=0.001). Although the different patient
selection criteria and chemotherapy regimens tested make the
comparison between these studies and the present study difficult,
the results of these studies and ours are both encouraging, as the
3-year DFS rate was 66.1% and the 3-year OS rate was 74.2% in the
present study. However, the benefit of this promising combined
adjuvant treatment modality should be confirmed in prospective
randomized controlled trials.
The incidences of hepatic and peritoneal failure
were relatively low in this study. An initial intraperitoneal and
hepatic relapse was noted in 6 (24.0%) and 3 (12.0%) out of 25
patients with recurrence in this study, respectively, thus the
incidences are lower than those revealed in the study of Wu et
al (2), which addressed
recurrence patterns following intended curative surgery in 611
patients with gastric cancer. In that study, 38.2 and 17.9%
patients experienced peritoneal and hepatic recurrence,
respectively. The low incidence of hepatic and peritoneal failure
in this study is possibly related to the additive effects of
systemic, intravenous and intraperitoneal drug administration.
However, in the present study, 91.3% of patients succumbed to their
condition within 1 year of the diagnosis of recurrence being made,
and the median time from recurrence to mortality was only 4 months.
These results are poorer than those of D’Angelica et al
(22). They reported that 70.0% of
patients succumbed to their condition within 1 year of the
diagnosis of recurrence and the median time from recurrence to
mortality was 6 months. In multivariate analysis, they demonstrated
that shortened median time until mortality was significantly
correlated with a higher T stage (4 vs. 7 months, P=0.007) and
involved lymph nodes (5 vs. 9 months, P=0.01). In the present
study, 83.9% of patients had serosa-infiltrating cancer and 87.1%
of them were lymph node-positive, which may be the main causes of
the short time to death following recurrence.
Patient tolerance of ACSIP was excellent in this
study. On the whole, toxicities were mild to moderate. Neutropenia,
gastrointestinal side effects and peripheral neuropathy were the
most common grade 3–4 toxicities; however, they were all infrequent
and manageable. There were no treatment-related mortalities.
Chemical peritonitis had been reported in patients with
intra-abdominal cancer receiving intraperitoneal high doses of 5-FU
and CDDP for long periods (23);
however, this did not occur in the present study as 5-FU and CDDP
were administered for a shorter period of time. Several studies
have suggested that there was an increase in morbidity and
mortality with adjuvant perioperative intraperitoneal chemotherapy
in gastric cancer. Yu et al (24) reported that the overall morbidity
and mortality rates in patients receiving early postoperative IPCT
starting on postoperative day 1 (the study group) were both higher
than in those who underwent surgery only (the control group),
although the difference was not significant (28 vs. 20.3%, P=0.121;
5.6 vs. 0.8%, P= 0.299, respectively). By contrast, intra-abdominal
sepsis without anastomotic leakage (P=0.008) and bleeding (P=0.002)
occurred significantly more often in the study group compared with
the control group. In a study by Rosen et al (25), significantly higher postoperative
complication and mortality rates were also observed in patients
receiving intraperitoneal mitomycin bound to activated carbon
particles compared with the surgical control group (35 vs. 16.0%;
11 vs. 2.0%, respectively), thus the protocol committee decided to
stop further recruitment of patients into that particular study.
However, the incidence of surgical complications was only 8.1% in
the present study, which was much lower than that in the
above-mentioned studies. The difference in incidence between these
studies and ours may be related to the different cancer stage, type
of surgery, timing of IPCT commencement and the chemotherapeutic
agents intraperitoneally administered. This study indicates that
adjuvant intraperitoneal 5-FU and CDDP delivered at 1–3 weeks
postoperatively may not increase the rates of surgical
complications and mortality in patients with gastric cancer. In
addition, 55 patients (88.7%) completed more than 4 cycles of ACSIP
and 48 patients (77.4%) completed 6 cycles in the present study. It
is possible that the benefit of ACSIP may be greater if more
patients successfully complete 6 cycles of treatment; however, the
effect of the duration of treatment on clinical outcome has not
been confirmed by any study.
A considerable amount of research into adjuvant
chemotherapy in gastric cancer is still necessary. Further
improvements will require the development of more effective
treatment modalities and chemotherapeutic regimens. During the last
decade, several new agents including paclitaxel, docetaxel,
oxaliplatin, irinotecan, capecitabine and S1 have shown promising
activity in gastric cancer. From a theoretical point of view,
regimens with higher activity may have more efficacy as adjuvant
therapies (26,27). However, the selection, dosage,
combination, schedule of chemotherapy agents and the route and
timing of administration need extensive testing in confirmatory
studies.
In conclusion, the results of this study indicate
that ACSIP is effective and feasible in high risk patients with
locally advanced gastric cancer following curative gastrectomy
under D2 lymphadenectomy and has encouraging 3-year DFS and OS
rates. Failure pattern data suggest possible decreased peritoneal
and hepatic recurrences. The benefit of this promising combined
adjuvant treatment modality for this challenging disease warrants
further studies.
Acknowledgements
The authors acknowledge Dr Jing Zhao
for her assistance in the statistical analysis of the data, as well
as Mr. Xian-Ce Jin for his revision of the manuscript.
References
|
1.
|
P ZhaoM DaiW ChenN LiCancer trends in
ChinaJpn J Clin Oncol40281285201010.1093/jjco/hyp187
|
|
2.
|
CW WuSS LoKH ShenIncidence and factors
associated with recurrence patterns after intended curative surgery
for gastric cancerWorld J Surg27153158200312616428
|
|
3.
|
PH SugarbakerW YuY YonemuraGastrectomy,
peritonectomy, and perioperative intraperitoneal chemotherapy: the
evolution of treatment strategies for advanced gastric cancerSemin
Surg Oncol21233248200310.1002/ssu.10042
|
|
4.
|
JS MacdonaldSR SmalleyJ
BenedettiChemoradiotherapy after surgery compared with surgery
alone for adenocarcinoma of the stomach or gastroesophageal
junctionN Engl J Med345725730200110.1056/NEJMoa010187
|
|
5.
|
D CunninghamWH AllumSP
StenningPerioperative chemotherapy versus surgery alone for
resectable gastroesophageal cancerN Engl J
Med3551120200610.1056/NEJMoa05553116822992
|
|
6.
|
M SasakoS SakuramotoH KataiFive-year
outcomes of a randomized phase III trial comparing adjuvant
chemotherapy with S-1 versus surgery alone in stage II or III
gastric cancerJ Clin Oncol2943874393201122010012
|
|
7.
|
XJ YangCQ HuangT SuoCytoreductive surgery
and hyperthermic intraperitoneal chemotherapy improves survival of
patients with peritoneal carcinomatosis from gastric cancer: final
results of a phase III randomized clinical trialAnn Surg
Oncol1815751581201110.1245/s10434-011-1631-5
|
|
8.
|
GASTRIC (Global Advanced/Adjuvant Stomach
Tumor Research International Collaboration) GroupX PaolettiK
ObaBenefit of adjuvant chemotherapy for resectable gastric cancer:
a meta-analysisJAMA30317291737201010.1001/jama.2010.53420442389
|
|
9.
|
P SunJB XiangZY ChenMeta-analysis of
adjuvant chemotherapy after radical surgery for advanced gastric
cancerBr J Surg962633200910.1002/bjs.640819016271
|
|
10.
|
TS LiuY WangSY ChenYH SunAn updated
meta-analysis of adjuvant chemotherapy after curative resection for
gastric cancerEur J Surg
Oncol3412081216200810.1016/j.ejso.2008.02.00218353606
|
|
11.
|
DZ XuYQ ZhanXW SunSM CaoQR
GengMeta-analysis of intraperitoneal chemotherapy for gastric
cancerWorld J Gastroenterol1027272730200415309728
|
|
12.
|
TD YanD BlackPH SugarbakerJ ZhuY YonemuraG
PetrouDL MorrisA systematic review and meta-analysis of the
randomized controlled trials on adjuvant intraperitoneal
chemotherapy for resectable gastric cancerAnn Surg
Oncol1427022713200710.1245/s10434-007-9487-4
|
|
13.
|
PH SugarbakerAdjuvant intraperitoneal
chemotherapy for advanced primary gastric cancerScand J
Surg95270273200617249276
|
|
14.
|
DK ArmstrongB BundyL WenzelIntraperitoneal
cisplatin and paclitaxel in ovarian cancerN Engl J
Med3543443200610.1056/NEJMoa05298516394300
|
|
15.
|
American Joint Committe on Cancer
(AJCC)Cancer staging handbook: TNM classification of malignant
tumours6th editionSpringerNew York991062002
|
|
16.
|
T SanoT AikoNew Japanese classifications
and treatment guidelines for gastric cancer: revision concepts and
major revised pointsGastric
Cancer1497100201110.1007/s10120-011-0040-621573921
|
|
17.
|
G MatharuO TuckerD AldersonSystematic
review of intraperitoneal chemotherapy for gastric cancerBr J
Surg9812251235201110.1002/bjs.758621644239
|
|
18.
|
W ScheithauerGV KornekA MarczellCombined
intravenous and intraperitoneal chemotherapy with fluorouracil +
leucovorin vs fluorouracil + levamisole for adjuvant therapy of
resected colon carcinomaBr J Cancer77134913541998
|
|
19.
|
OT AtiqDP KelsenMH ShiuPhase II trial of
postoperative adjuvant intraperitoneal cisplatin and fluorouracil
and systemic fluorouracil chemotherapy in patients with resected
gastric cancerJ Clin Oncol114254331993
|
|
20.
|
Y ZuoM XuD ShenWD LuJF LuPostoperative
intraperitioneal hyperthermic chemoperfusion combined with
intravenous chemotherapy for 82 advanced gastric cancer
patientsZhonghua Zhong Liu Za Zhi262472492004
|
|
21.
|
C ShiB YangQ ChenJ YangN FanRetrospective
analysis of adjuvant intraperitoneal chemotherapy effect prognosis
of resectable gastric
cancerOncology80289295201110.1159/000329075
|
|
22.
|
M D’AngelicaM GonenMF BrennanAD TurnbullM
BainsMS KarpehPatterns of initial recurrence in completely resected
gastric adenocarcinomaAnn Surg240808816200415492562
|
|
23.
|
RL SchilskyKE ChoiJ GrayhackD GrimmerC
GuarnieriL FullemPhase I clinical and pharmacologic study of
intraperitoneal cisplatin and fluorouracil in patients with
advanced intraabdominal cancerJ Clin Oncol8205420611990
|
|
24.
|
W YuI WhangA AverbachD ChangPH
SugarbakerMorbidity and mortality of early postoperative
intraperitoneal chemotherapy as adjuvant therapy for gastric
cancerAm Surg641104110819989798779
|
|
25.
|
HR RosenG JatzkoS RepseAdjuvant
intraperitoneal chemotherapy with carbon-adsorbed mitomycin in
patients with gastric cancer: results of a randomized multicenter
trial of the Austrian Working Group for Surgical OncologyJ Clin
Oncol16273327381998
|
|
26.
|
F De VitaL VecchioneG GaliziaPerspectives
in adjuvant therapy of gastric cancerOncology773842200920130430
|
|
27.
|
A BittoniE MaccaroniM ScartozziR BerardiS
CascinuChemotherapy for locally advanced and metastatic gastric
cancer: state of the art and future perspectivesEur Rev Med
Pharmacol Sci14309314201020496540
|