Introduction
Gastrointestinal stromal tumors (GIST) are
mesenchymal tumors of the digestive tract that originate from
interstitial Cajal cells and account for 0.1–3% of all
gastrointestinal tumors. They are usually located in the stomach
and small intestine (1), but they
can be located anywhere in the gastrointestinal tract, including
the omentum and peritoneum. Generally, GISTs have a silent behavior
and are diagnosed incidentally. Approximately 40% of GIST cases
cause intestinal bleeding (2).
Perforation is rarely observed in GISTs; however, we present a case
of perforated GIST located in the jejunum as a rare cause of acute
abdomen.
Case report
A 59-year-old male was admitted to the emergency
department of the Bezmialem Faculty of Medicine Hospital with acute
abdominal pain during the previous 20 h. The patient had no
complaint of nausea or vomiting; however, the patient did have a
history of diabetes mellitus type II and had undergone a coronary
artery bypass surgery 6 years previously. On admission, the
patient’s vital signs were stable, while his physical examination
revealed abdominal distention, generalized tenderness and guarding.
No palpable mass was revealed on physical examination due to
abdominal guarding, and bowel sounds were hypokinetic. Blood cell
count was 9,800 cells/μl (normal range, 4,000–11,000
cells/μl) and the C-reactive protein value was 6.5 mg/dl,
which was 13 times the upper range (normal range, <0.5).
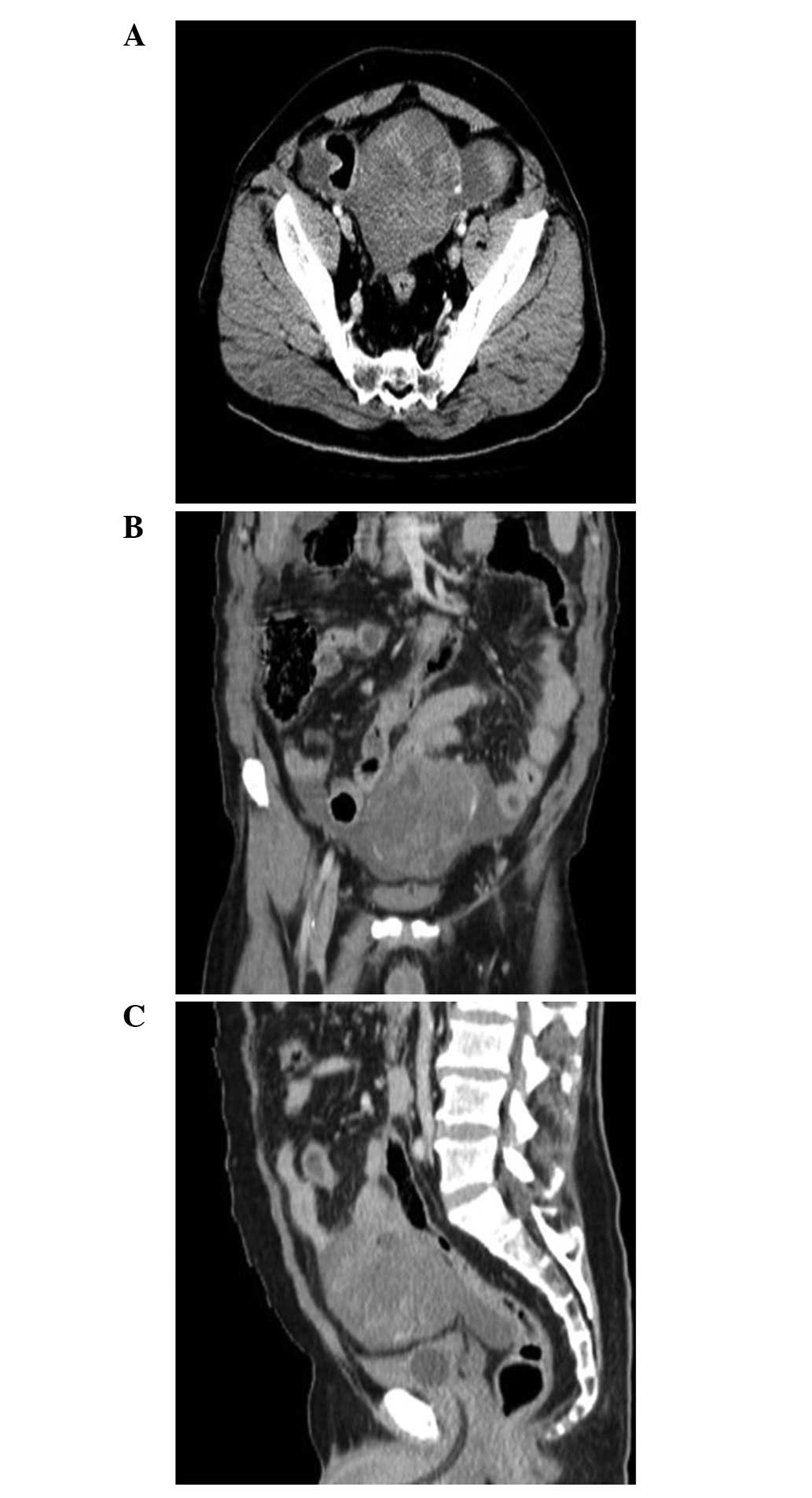
A contrast enhanced computed tomography (CT) scan
revealed a 12x10x9-cm mass located at the level of the pelvic inlet
on the midline posterosuperior to the urinary bladder with a solid
character containing centrally necrotic areas and well-vascularized
periphery (Fig. 1). Free fluid was
identified around the mass, and nearby intestinal structures were
inflamed. A laparotomy was conducted immediately. Subsequently a
12-cm diameter mass was identified in the jejunum located 150 cm
from the Treitz’s ligament, and a small perforation area was
observed at the medial side of the mass (Fig. 2). Generalized free fluid colored by
bile was detected in the abdomen, while fibrinous inflammation and
pseudomembranous colitis were identified around the mass,
particularly on the intestinal structures in the pelvis. Segmentary
jejunal resection, including the mass lesion, with clear
macroscopical margins was conducted (Fig. 3). Handling was avoided to prevent
the risk of having to conduct end to end anastomosis due to the
dirty content of the abdomen and to maintain a safer approach to
the patient. We anastomosed the posterior walls of each side and
made a loop jejunostomy from the right lower quadrant.
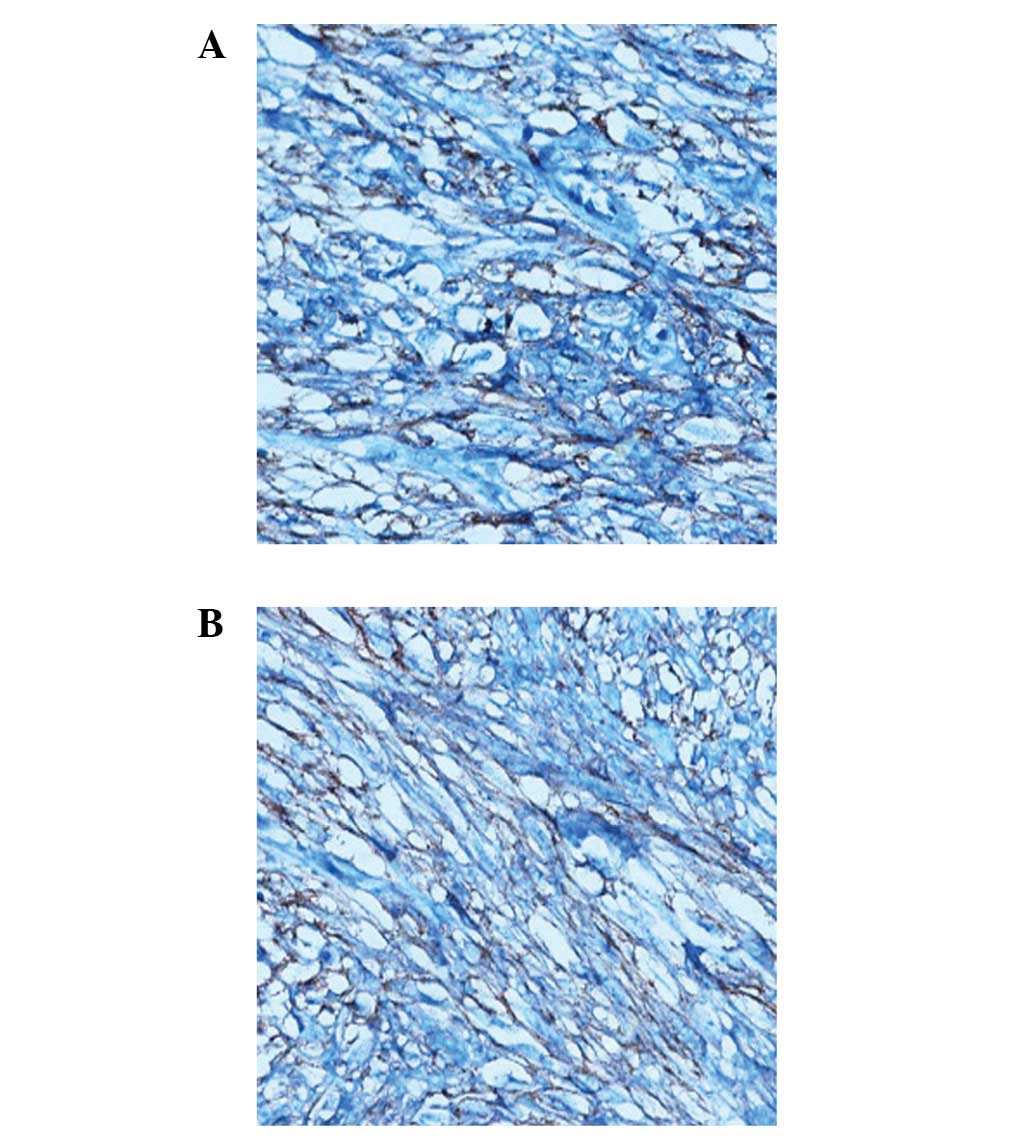
Histopathological investigation of the specimen revealed interlaced
bundles of spindle-like tumor cells with high mitotic figures [7/50
high-power field (HPF)], and a Ki-67 value of 8%.
Immunohistochemical results were C-KIT (Fig. 4A) and DOG1 positive (Fig. 4B), CD34 focally positive, S-100
positive, and smooth muscle actin (SMA) and desmin negative. As a
result of these findings, the tumor was diagnosed as a GIST. A
total of 6 lymph nodes were harvested, of which all were
nonspecific. Surgical margins were confirmed as clear and the
postoperative period was uneventful, so the patient was discharged
on the 10th postoperative day.
Discussion
GIST is a visceral tumor arising from any site of
the gastrointestinal tract. Approximately 60–70% of cases occur in
the stomach, 25–35% in the small intestine and 10% in the jejunum,
while the esophagus, colon, rectum and appendix are rarely affected
(1). Approximately 10–30% of
patients with GISTs may be asymptomatic. The most common symptoms
associated with jejunal GISTs are vague, non-specific abdominal
pain or discomfort. Patients who have jejunal GIST usually suffer
from abdominal pain or palpable mass, and also complain of early
satiety or abdominal fullness. Jejunal GISTs may cause symptoms
secondary to obstruction or hemorrhage. Pressure necrosis and
ulceration of the overlying mucosa may cause gastrointestinal
bleeding, and patients who experience significant blood loss may
suffer from malaise and fatigue. Obstruction may result from the
intraluminal growth of the tumor or luminal compression from an
exophytic lesion. Fever, anorexia and weight loss are rarely
observed (2) and GISTs originating
from the jejunum seldom cause perforation and acute diffuse
peritonitis (3–6).
It is difficult to diagnose a jejunal GIST
preoperatively due to the nonspecific and variable clinical
symptoms, and it is also difficult to distinguish the tumor based
solely on images. Although a CT scan is a commonly offered imaging
modality for patients with suspected abdominal GISTs, magnetic
resonance imaging (MRI) provides better information than CT in the
preoperative workup (7). The
definitive diagnosis of the majority of jejunal GISTs is revealed
by histopathological examination of the specimen. Approximately 95%
of GISTs express CD117, which is part of the KIT receptor tyrosine
kinase. Additionally, DOG1, a recently defined monoclonal antibody
against a chloride channel protein expressed by GIST, is positively
expressed in 95% of GISTs (8). DOG1
is a novel marker of GISTs as it has a higher sensitivity and
specificity compared with CD34, particularly in the detection of
moderate and high risk GIST. Therefore, the present case was
diagnosed by immunohistochemical examination of C-KIT and DOG1
positivity.
To date, surgery is the only potentially curative
therapy for patients with primary, resectable GIST. Nonmetastatic
GISTs greater than 2 cm should be resected. A lymphadenectomy is
not conducted because lymph node metastases are rare (9). Although the size of tumor in this case
was large, there were no harvested positive lymph nodes in the
present case. The management of GIST has undergone significant
revolution over last decade. Tyrosine kinase inhibitor therapy has
significantly improved overall survival in patients with advanced
disease and should be continued indefinitely. Prior to the
development of imatinib, recurrences were common even in patients
undergoing surgery. Adjuvant imatinib for 3 years should be
considered in patients undergoing resection for primary disease
(10).
In conclusion, we report a case of a male with a
perforated GIST in the jejunum causing acute diffuse peritonitis.
The clinical outcome is worse when this tumor presents with bowel
perforation and peritonitis; therefore, if an abdominal mass
presents with diffuse peritonitis, the possibility of jejunal GIST
perforation should be considered, even though it is extremely rare.
A high degree of suspicion is necessary in view of the high
morbidity rates resulting from a delayed diagnosis of the
disease.
References
|
1.
|
EM ConnollyE GaffneyJV
ReynoldsGastrointestinal stromal tumorsBr J
Surg9011781186200310.1002/bjs.435214515284
|
|
2.
|
T TranJA DavilaHB El-SeragThe epidemiology
of malignant gastrointestinal stromal tumors: analysis of 1,458
cases from 1992 to 2000Am J
Gastroenterol100162168200510.1111/j.1572-0241.2005.40709.x15654796
|
|
3.
|
F FengF ChenY ChenJ LiuA rare perforated
gastrointestinal stromal tumor in the jejunum: a case reportTurk J
Gastroenterol22208212201121796562
|
|
4.
|
E KaragülleE TürkE YildirimHS GõktürkH
KiyiciG MorayMultifocal intestinal stromal tumors with jejunal
perforation and intra-abdominal abscess: report of a caseTurk J
Gastroenterol19264267200819119486
|
|
5.
|
EI EfremidouN LiratzopoulosMS
PapageorgiouK RomanidisPerforated GIST of the small intestine as a
rare cause of acute abdomen: surgical treatment and adjuvant
therapy. Case reportJ Gastrointestin Liver Dis152972992006
|
|
6.
|
V ÖzbenS ÇarkmanD AtasoyG DoğusoyE
EyüboğluA case of gastrointestinal stromal tumor presenting with
small bowel perforation and internal herniaTurk J
Gastroenterol21470471201021332009
|
|
7.
|
M AmanoT OkudaY AmanoT TajitiT
KumazakiMagnetic resonance imaging of gastrointestinal stromal
tumor in the abdomen and pelvisClin
Imaging30127131200610.1016/j.clinimag.2005.09.02516500544
|
|
8.
|
S GroverSW AshleyCP RautSmall intestine
gastrointestinal stromal tumorsCurr Opin
Gastroenterol28113123201210.1097/MOG.0b013e32834ec15422157511
|
|
9.
|
Y FongDG CoitJM WoodruffMF BrennanLymph
node metastasis from soft tissue sarcoma in adults. Analysis of
data from a prospective database of 1772 sarcoma patientsAnn
Surg2177277199310.1097/00000658-199301000-000128424704
|
|
10.
|
M MiettinenJ LasotaGastrointestinal
stromal tumors: pathology and prognosis at different sitesSemin
Diagn Pathol237083200610.1053/j.semdp.2006.09.00117193820
|