Introduction
Angiomatoid fibrous histiocytoma (AFH) is a very
rare mesenchymal neoplasm of uncertain differentiation, a small
number of which recur locally. Rare cases have been known to
metastasize (1). It is often
initially misdiagnosed as individuals often present a clinical
picture resembling other diseases. AFH most often presents in
children and young adults and occurs most commonly within the
extremities (2–4). Previous reports have shown that AFH
may occur in the extremities and the trunk. Here, a case of
angiomatoid fibrous histiocytoma located in the retroperitoneum is
presented. The diagnosis was established based on pathological
review with immunohistochemistry. The study was approved by the
Ethics Committee of Suzhou University, Suzhou, Jiangsu, China.
Case report
A 25-year-old male was presented for evaluation with
a fever and cough which had initiated 4 months previously and had
become aggravated during the past 3 days. The patient noticed
weight loss and denied hemoptysis, chest pain, dyspnea, fatigue or
night sweats. The patient was previously healthy and had no history
of smoking. His family history was negative for hereditary
diseases.
On examination, the patient had a fever of 38.6°C
with normal blood pressure and regular pulse. He had moderate
anemia. Everything else was otherwise normal. Laboratory studies
revealed anemia with a hemoglobin (Hb) of 57.9 g/l (normal adult
male level 120.0–160.0 g/l), a white blood cell count (WBC) of
12.24×109/l (normal level 4–10×109/l) and a
platelet count of 755×109/l (normal level
100–300×109l). His C reactive protein was 49.9 mg/l
(normal level 0.0–10.0 g/l) and he had an erythrocyte sedimentation
rate of 23 mm/h (normal rate 0–21 mm/h). Tests for liver function
revealed severe hypoalbuminemia with an albumin level of 17.5 g/l
(35.0–55.0 g/l) and a globulin level of 56.3 g/l (19.0–38.0 g/l).
His prothrombin time was 18.5 sec (9.0–13.0 sec) and activated
partial thromboplastin time was 41.0 sec (19.0–34.5 sec). Tests for
blood and sputum culture were negative. There was no monoclonal
protein on serum electrophoresis. A bone marrow blood smear
demonstrated nucleated cells, myeloid and erythroid were actively
hyperplastic, and a lymphocyte count of 28%. The morphology of
cells were regular and thrombocytosis. Bone marrow biopsy did not
demonstrate any abnormal cells. Flow cytometry of bone marrow blood
did not demonstrate any monotypic cell population or increase in
blast cells.
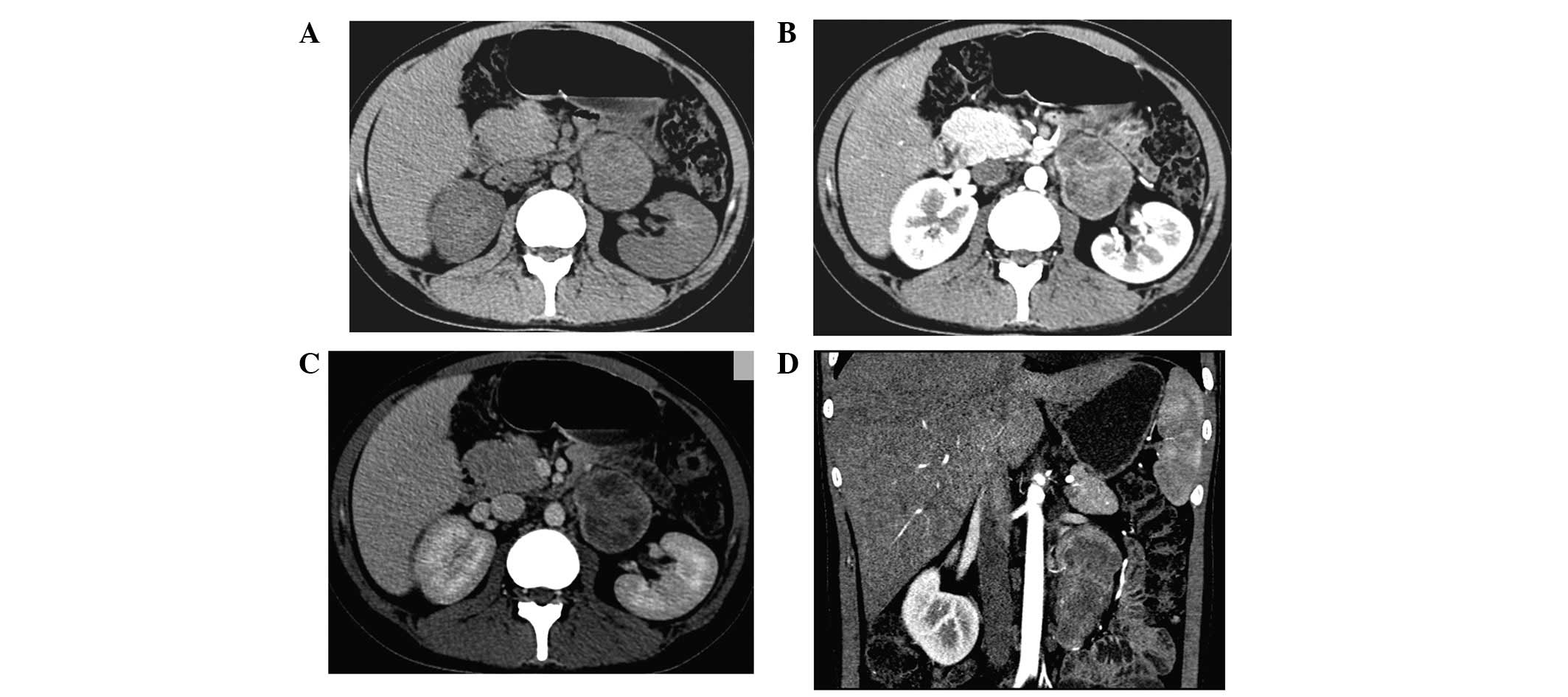
A high resolution computed tomography (HRCT) of the
chest was normal. A CT scan of the abdomen showed an indeterminate
5.7×4.7-cm retroperitoneal soft tissue mass with an appearance
suggestive of neurogenic tumor (Fig.
1). Positron emission tomography (PET)/CT revealed that the
metabolism of fludeoxyglucose (FDG) had increased abnormally, prone
to malignant disease (Fig. 2).
Treatment options were discussed with the patient.
Retroperitoneal tumor resection was performed and a hemorrhagic
firm mass measuring 8.0×5.0×5.0 cm was resected. Pathology revealed
an AFH (Fig 3). Eight days after
the operation, peripheral blood was Hb 120 g/l, WBC
8.20×109/l and platelets 495×109/l. Liver
function examination showed an albumin level of 29.2 g/l and a
globulin level of 44.9 g/l. Tests for coagulation function showed a
prothrombin time of 15.7 sec and activated partial thromboplastin
time of 37.5 sec. A month later, tests for peripheral blood, liver
and coagulation function were normal. The patient had gained 5 kg
in weight. Three months later his abdomen CT was normal. To date,
the condition of the patient is stable.
Discussion
AFH is a very rare mesenchymal neoplasm of uncertain
differentiation, initially described as angiomatoid ‘malignant’
fibrous histiocytoma (5). It
normally affects children and young adults. It typically occurs in
the extremities of the deep dermis and subcutaneous tissue,
followed by the trunk and the head and neck. Rare cases involve
bone (6). Here, a case of
retroperitoneal AFH is presented. This presentation is not unusual
for patients with AFH. The clinical features of AFH may present
systemic symptoms, such as fever, anemia, weight loss, polyclonal
gammopathy and a Castleman disease-like lymphadenopathy (7). It is often misdiagnosed initially. A
small number of AFH cases recur locally and rare cases have been
known to metastasize. The best therapy for AFH is surgery together
with a wide local excision. Comprehensive treatment such as
radiation and chemical therapy can be used when wide excision
margins are not feasible (1,8,9).
According to one pathological review, AFH usually demonstrates four
features: a fibrohistiocytic cell proliferation, a
pseudoangiomatous pattern, a plasmalymphocytic infiltrate and a
fibrous pseudocapsule (10). The
immunohistochemical features present a unique immunophenotype. In
one immunohistochemical review, 50–60% of cases had coexpression of
desmin, epithelial membrane antigen, CD68 and CD99 but no samples
were positive for CD21, CD35, clusterin or S100 (7). The diagnosis of AFH was made based on
these studies. Although thorough pathologic review is critical for
diagnosis, techniques such as fluorescence in situ
hybridization (FISH) have been used to confirm cases of AFH with
pleomorphic features. AFH has been found to harbor three related
translocations at (12;16) (q13;p11), (12;22)(q13;q12) and
(2;22)(q33;q12), resulting in an FUS/ATF1, a EWSR1/ATF1 and an
EWSR1/CREB1 fusion gene, respectively (11–13).
AFH is a rare disease that occurs most commonly
within the extremities and the trunk. It may also present in other
parts of the body, such as the retroperitoneum in our patient. This
is the first report of retroperitoneal AFH. Patients may present a
clinical picture suggestive of other diseases. Pathological review
is necessary to diagnose AFH. Most patients recover with wide local
excision alone, but radiotherapy and chemotherapy may be utilized
when wide excision margins are not feasible. AFH has a good
prognosis except when it occurs in the head and neck. The recovery
of our patient was good and there was no evidence of recurrence and
metastasis at follow-up.
References
|
1
|
Costa MJ and Weiss SW: Angiomatoid
malignant fibrous histiocytoma: A follow-up study of 108 cases with
evaluation of possible histologic predictors of outcome. Am J Surg
Pathol. 14:1126–1132. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weiss SW and Goldblum JR: Enzinger and
Weiss’ Soft Tissue Tumors. Mosby Elsevier; Philadelphia: pp.
390–394. 2008
|
|
3
|
Fletcher CDM, Unni KK and Mertens F:
Pathology and genetics of tumours of soft tissue and bone WHO. IARC
Press. Lyon: 194–195. 2002.
|
|
4
|
Fletcher CDM: Soft tissue tumors.
Diagnostic Histopathology of Tumors. Churchill Livingstone,
Elsevier; Philadelphia: pp. 1574–1575. 2007
|
|
5
|
Enzinger FM: Angiomatoid malignant fibrous
histiocytoma: a distinct fibrohistiocytic tumor of children and
young adults simulating a vascular neoplasm. Cancer. 44:2147–2157.
1979. View Article : Google Scholar
|
|
6
|
Hallor KH, Micci F, Meis-Kindblom JM, et
al: Fusion genes in angiomatoid fibrous histiocytoma. Cancer Lett.
251:158–163. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
García JJ and Folpe AL: The impact of
advances in molecular genetic pathology on the classification,
diagnosis and treatment of selected soft tissue tumors of the head
and neck. Head Neck Pathol. 4:70–76. 2010.PubMed/NCBI
|
|
8
|
Davis AM, O’Sullivan B, Turcotte R, et al:
Late radiation morbidity following randomization to preoperative
versus postoperative radiotherapy in extremity soft tissue sarcoma.
Radiother Oncol. 75:48–53. 2005. View Article : Google Scholar
|
|
9
|
Matsumura T, Yamaguchi T, Tochigi N, et
al: Angiomatoid fibrous histiocytoma including cases with
pleomorphic features analysed by fluorescence in situ
hybridisation. J Clin Pathol. 63:124–128. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Grossman LD, White RR and Arber DA:
Angiomatoid fibrous histiocytoma. Ann Plast Surg. 36:649–651. 1996.
View Article : Google Scholar
|
|
11
|
Waters BL, Panagopoulos I and Allen EF:
Genetic characterization of angiomatoid fibrous histiocytoma
identifies fusion of the FUS and ATF-1 genes induced by a
chromosomal translocation involving bands 12q13 and 16p11. Cancer
Genet Cytogenet. 121:109–116. 2000. View Article : Google Scholar
|
|
12
|
Antonescu CR, Dal Cin P, Nafa K, et al:
EWSR1-CREB1 is the predominant gene fusion in angiomatoid fibrous
histiocytoma. Genes Chromosomes Cancer. 46:1051–1060. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rossi S, Szuhai K, Ijszenga M, et al:
EWSR1-CREB1 and EWSR1-ATF1 fusion genes in angiomatoid fibrous
histiocytoma. Clin Cancer Res. 13:7322–7328. 2007. View Article : Google Scholar : PubMed/NCBI
|