Introduction
Endometrial carcinoma affects older females, with
∼75% of the cases occurring after the onset of the menopause, and
is the third most common gynecological malignant tumor. Its
incidence has increased markedly and it is estimated that ∼43,470
new cases of endometrial carcinoma were diagnosed and 7,950
mortalities occurred in the USA in 2010 (1,2).
Surgery, chemotherapy and radiation approaches (3,4) have
been established for the treatment of endometrial carcinoma.
However, the recurrent cases that have acquired radio- or
chemoresistance pose a major challenge for healthcare
professionals. It is therefore necessary to identify new, effective
and comprehensive treatments.
Angiogenesis is a physiological process that
normally occurs in fetal development, wound healing and in the
female reproductive tract. It has been reported that the growth of
new blood vessels has pathological and beneficial roles in human
diseases and the growth of tumors also relies on adequate blood
supplies. Angiogenesis is considered to be crucial for tumor
malignant biological characteristics, such as invasion, recurrence
and metastasis (2,5) and its importance in solid tumor growth
and metastasis has been widely recognized by multiple studies.
Studies concerning blocking angiogenesis to treat tumors have drawn
much attention and become one of the most promising and active
fields in anticancer research (6–9). The
present study investigated the effect of siRNA targeted against the
tyrosine kinase receptor 2 (Tie2) gene in combination with
carboplatin in a mouse model of endometrial carcinoma in an attempt
to elucidate the role of Tie2 in the carcinogenesis and progression
of endometrial carcinoma via angiogenesis, in order to establish a
basis for the development of complementary molecule targeting and
chemotherapeutic actions.
Materials and methods
Cell culture
Ishikawa cells, a human endometrial carcinoma cell
line, were generously provided as a gift by Professor L.H. Wei
(Peking University People’s Hospital, Beijing, China) and cultured
in α-Modified Eagle’s medium (α-MEM; Gibco, Carlsbad, CA, USA)
supplemented with 10% heat-inactived fetal bovine serum (FBS,
Gibco), penicillin (100 IU/ml) and streptomycin (100 μg/ml).
All cultures were incubated in a 5% CO2 humidified
incubator at 37°C and experiments were performed using subconfluent
cells in the exponential growth phase.
Nude mouse tumor xenograft model
The animal care procedures conformed with the
institutional guidelines in compliance with the national and
international laws and policies. Female 3–4-week-old athymic nude
mice (BALB/c-nu/nu; n=25), obtained from Shanghai Animal Center
(Shanghai, China), were used for all experiments. The mice were
housed and maintained in laminar flow cabinets under specific
pathogen-free conditions.
Following the construction of the nude mouse tumor
xenograft model with Ishikawa cells, all the injected nude mice
with tumors were randomly divided into five groups, with five mice
in each group as follows, when the volume of the xenografts reached
50 mm3 (∼2 weeks): i) blank (5% glucose; G) group; ii)
pRNAT-CMV3.2-Neo carrying negative siRNA (N) group; iii)
carboplatin (C) group; iv) pRNAT-CMV3.2-Neo carrying Tie2-siRNA (T)
group; v) Tie2-siRNA in combination with carboplatin (A) group. The
five groups received intra-tumor injections of 5% glucose (0.2
ml·mouse−1), N-siRNA (20 μg·mouse−1),
carboplatin (25.0 mg·kg−1, 5% glucose dilution),
Tie2-siRNA (20 μg·mouse−1) and Tie2-siRNA (20
μg·mouse−1) in combination with carboplatin (25.0
mg·kg−1, 5% glucose dilution), respectively, every three
days for five cycles. The grafts were measured with a sliding
caliper and the tumor sizes were caculated using the equation:
tumor size =[length (mm) × width (mm)2] / 2. The
inhibitory rates of the primary tumors were calculated as: (Tumor
sizecontrol − tumor sizetreatment) / tumor
sizecontrol ×100. All mice were sacrificed following the
last administration.
Real-time PCR assay
The total RNA was isolated from the tumor tissue
samples using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) and
the amount and purity of the extracted RNA was quantitated by
absorbance analysis at 260 nm using an Eppendorf biophotometer
(Hamburg, Germany). The total RNA was reverse transcribed using
murine leukemia virus reverse transcriptase (Takara, Ōtsu, Japan).
GAPDH primer was used as an internal standard. PCR reactions were
performed using the SYBR PrimeScript RT-PCR kit (Takara) and the
following primers: for Tie2: forward, 5′-GTTCTGTCTCCCTGACCCCTAT-3′
and reverse, 5′-TAAGCTTACAATCTGGCCCGTA-3′; and for GAPDH, forward,
5′-ATTCCATGGCACCGTCAAGGCTG-3′ and reverse,
5′-GTGGTGAAGACGCCAGTGGACT-3′. To ensure the specificity of the Tie2
primer set, the amplicons generated from the PCR reactions were
evaluated in terms of specific melting point temperatures using the
first derivative primer melting curve software (Applied Biosystems,
Foster City, CA, USA). The expression level of Tie2 mRNA was
normalized to the expression of the control gene GAPDH and the
relative quantification of Tie2 mRNA was performed using the
comparative cycle threshold method (2−ΔΔCT) (10). All PCR experiments were repeated
three times.
Western blot analysis
The tumor tissue samples were homogenized in RIPA
buffer with a protease and phosphatase cocktail (Roche, Mannheim,
Germany). The proteins underwent 10% SDS-PAGE and were then
transferred onto nitrocellulose membranes (Millipore, Billerica,
MA, USA). After incubation with the primary antibody (1:1,000; CST)
at 4°C overnight, the membranes were washed with Tris-buffered
saline Tween-20 (TBST), then incubated with a goat anti-mouse-HRP
secondary antibody (1:5,000 dilution, Abcam, Cambridge, MA, USA)
and visualized using ECL chemoluminescence (Millipore). GAPDH
(Abcam) was used as an internal standard. The relative intensity of
the target blots was analyzed using Quantity One software (Bio-Rad,
Hercules, CA, USA).
Immunohistochemical assessment of vessel
density
The tumor tissues were paraffin-embedded and
sectioned (4-μm thickness) after being fixed in formalin for
24 h. The slides were deparaffined and microwaved at 98°C for 10
min in citrate buffer, then rehydrated through descending grades of
ethanol. Endogenous peroxidase activity was quenched by immersion
in 3% H2O2 for 10 min. The sections were then blocked
with 10% FBS (Gibco) and incubated with appropriately diluted
(1:150) rabbit CD34 monoclonal antibody (one type of blood vessel
marker; Abcam) at 4°C overnight. The primary antibody was removed
and washed with TBS and FITC-conjugated goat-anti-rabbit IgG
antibody (Zhongshan Bio-tech Co., Ltd., Zhongshan, China) was then
added, incubated at 37°C for 30 min. The sections were then
visualized using DAB coloration fluid (Zhongshan Bio-tech Co.,
Ltd.). Finally, the sections were stained with hematoxylin and
washed with distilled water. Quantification of blood vessels was
performed as described previously (11). A negative control was included for
each tissue section by substituting the primary antibody for a
matching concentration of goat or rabbit IgG.
The brown-stained single endothelial cell or cell
clusters distinct from adjacent microvessels, tumor cells or other
stromal cells were considered as single countable microvessels. The
areas with the highest microvessel density (MVD) were identified in
a low-power field (magnification, ×100) and vessels were counted in
five high-power fields (magnification, ×200). The average numbers
of microvessels were presented as the mean ± SEM. To minimize
subjectivity, the process was performed by blinded
pathologists.
Statistical analysis
All values were presented as the mean ± SEM and
analyzed for significance by one-way analysis of variance (ANOVA).
The SPSS 16 statistical software (SPSS, Chicago, IL, USA) was used
for the analyses. P<0.05 was considered to indicate
statistically significant differences.
Results
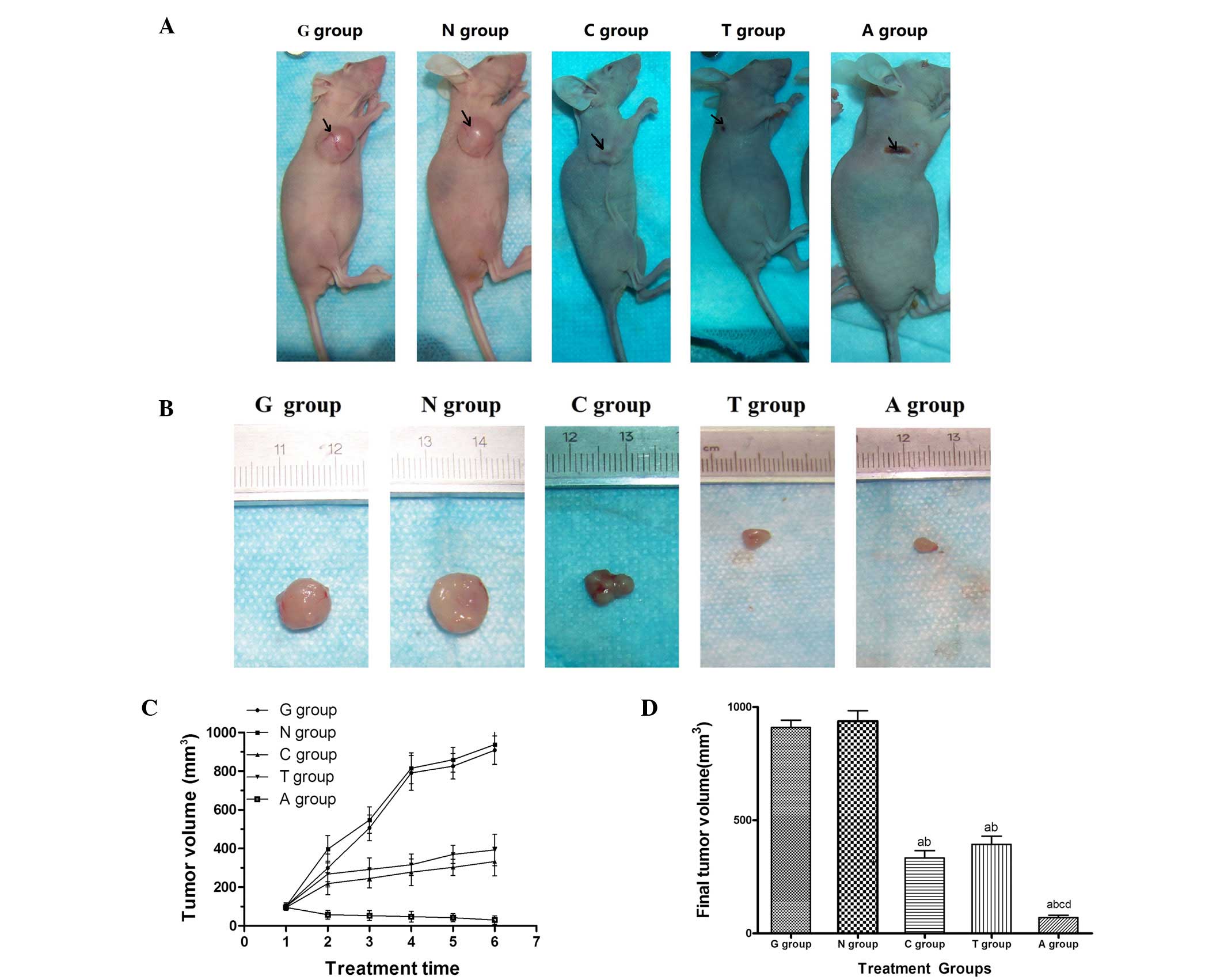
Difference in tumor growth following
treatment with Tie2-siRNA and/or carboplatin
The effect of Tie2 gene silencing with or without
carboplatin was investigated in the Ishikawa cell tumor xenograft
model in vivo. The control and experimental mice developed
tumors at the site of injection. Typically, 10–14 days were
required after cell transplantation for the volume of the xenograft
to reach 100 mm3. The representative images of mice
(outline with arrow, Fig. 1A) and
excised tumors (Fig. 1B) from each
group are shown in Fig. 1A and B.
The mice which received intratumor treatment with carboplatin,
Tie2-siRNA and combined therapy exhibited reductions in tumor size
in comparison with the G or N group mice. The treatment had
significant effects on tumor growth beginning on the second
treatment and continued to be significant throughout the study
(Fig. 1C). During the treatment
period, the tumor growth curves were essentially the same in the G
and N group mice (Fig. 1C).
However, while carboplatin and Tie2-siRNA significantly slowed
tumor growth (Fig. 1C), the
combination of carboplatin and Tie2-siRNA resulted in a greater
retardation of tumor growth than single administrations (Fig. 1C). The final average tumor volumes
were smaller in the carboplatin (332.99±73.91 mm3),
Tie2-siRNA (392.78±81.74 mm3) and combined
administration (70.11±22.09 mm3) groups than those in
the G (909.05±73.42 mm3) or N (937.65±103.09
mm3) groups, and the differences were statistically
significant (Fig. 1D). The combined
administration was significantly different compared with the
carboplatin and Tie2-siRNA groups (Fig.
1D). The mean tumor inhibition rates in the carboplatin,
Tie2-siRNA and combined administration groups were 62.91±4.50,
75.18±8.39 and 85.93±5.35%, respectively compared with those of the
G and N (0.8±5.86%) groups, and the differences were statistically
significant.
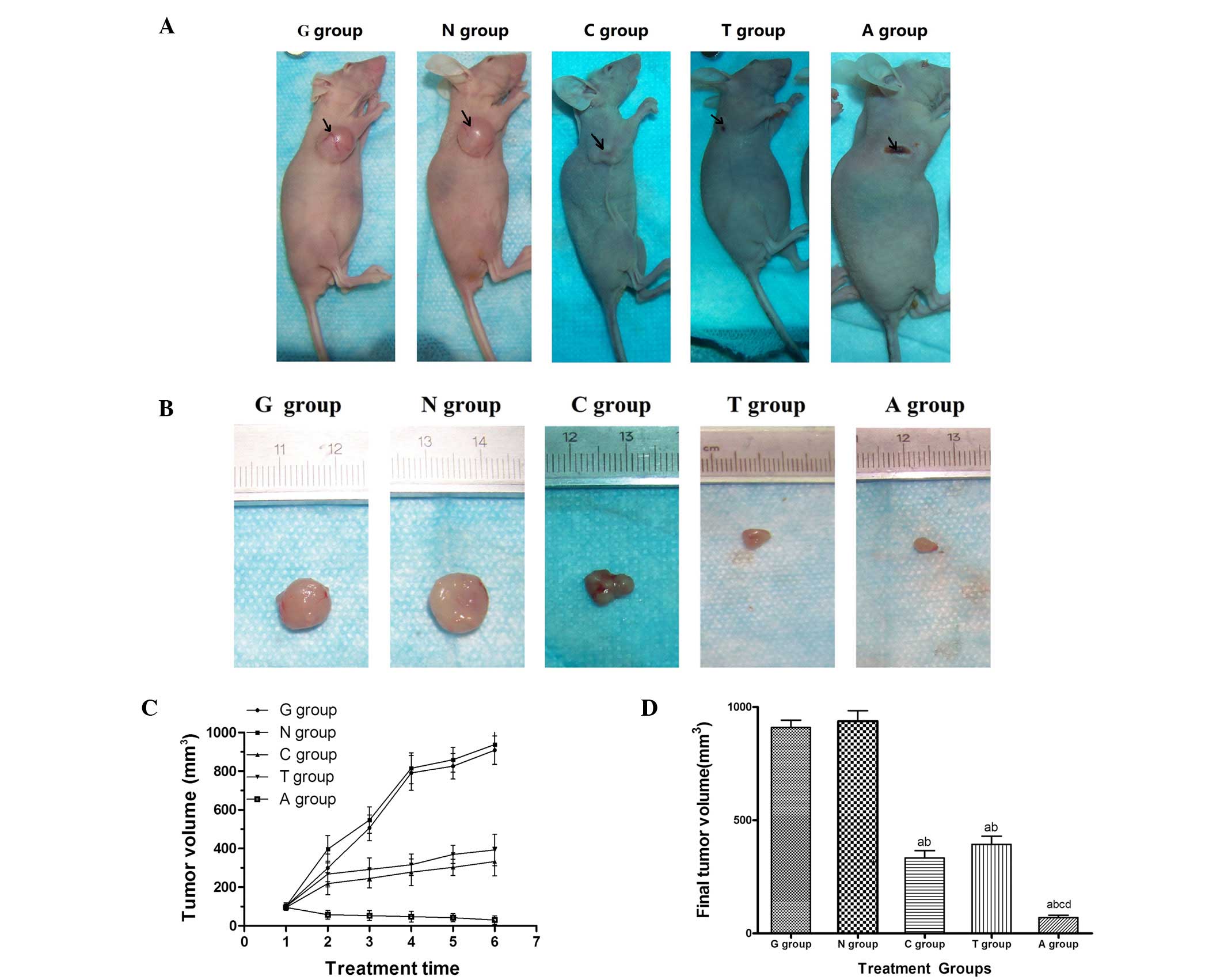 | Figure 1Tie2-siRNA and/or carboplatin affects
tumor growth in vivo. (A) Macroscopic appearance of tumors
in nude mice 30 days after the transplantation of human endometrial
carcinoma Ishikawa cells. Arrows outline the representative tumors
in the right scapular region of the mice. (B) Images of
representative excised tumors from each group. (C) Tumor volumes
were averaged for each treatment group and time point over the
course of the study. (D) Final tumor volumes of the isolated tumors
were averaged for each group (mean ± SEM). The tumor volumes of
mice treated with of carboplatin, Tie2-siRNA and the combined
administration were significantly different, compared with the G or
N group, beginning at the third treatment and continuing to be
significant throughout the study (P<0.05 respectively).
aCompared with G group, there was a statistically
significant difference; bCompared with N group, there
was a statistically significant difference; cCompared
with C group, there was a statistically significant difference;
dCompared with T group, there was a statistically
significant difference. Tie2, tyrosine kinase receptor 2; G,
glucose treatment; N, pRNAT-CMV3.2-Neo carrying negative siRNA
treatment; C, carboplatin treatment; T, pRNAT-CMV3.2-Neo carrying
Tie2-siRNA treatment; A, Tie2-siRNA in combination with carboplatin
treatment. |
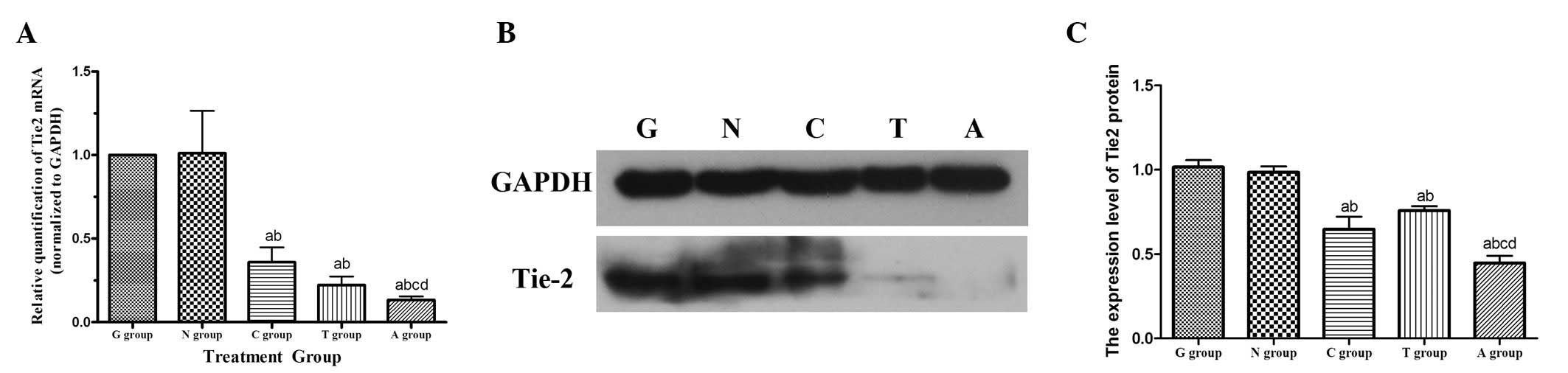
Difference in Tie2 mRNA expression
following treatment with Tie2-siRNA and/or carboplatin
The antitumor treatment had significant effects on
tumor growth in the present study and subsequently Tie2 gene
expression was investigated by real-time PCR. The amount of Tie2
mRNA was normalized to the expression of the control gene GAPDH and
relative quantification was performed using the 2−ΔΔCT
method. The expression of Tie2 mRNA was significantly reduced
following treatment with carboplatin (0.36±0.23), Tie2-siRNA
(0.22±0.14) and the combined administration of the two (0.13±0.05)
compared with the G (1.00±0.00) or N (1.01±0.67) groups. Compared
with the administration of carboplatin or Tie2-siRNA alone, the
reduction of Tie2 mRNA expression level in the the combined
administration group was statistically significant (P<0.05;
Fig. 2A).
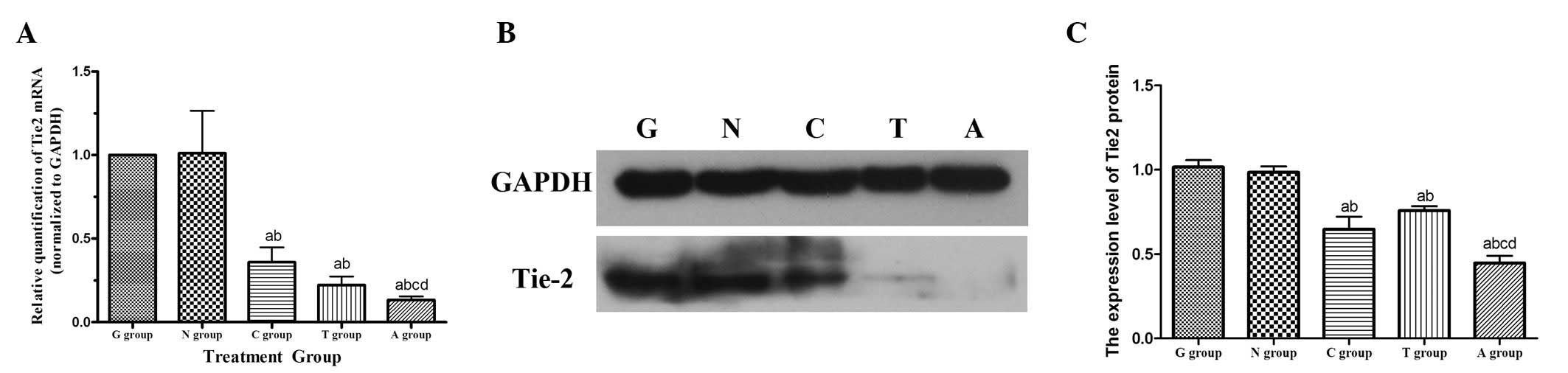 | Figure 2Tie2-siRNA and/or carboplatin
decreases Tie2 expression in the tumor tissues of the groups. (A)
Total RNA was isolated from tumor tissues and relative Tie2 mRNA
expression was analyzed with real-time PCR. (B) Western blot
analysis of Tie2 protein expression in five groups and (C)
quantification of relative Tie2 protein expression tumor tissues of
every group (P<0.05). aCompared with G group, there
was a statistically significant difference; bCompared
with N group, there was a statistically significant difference;
cCompared with C group, there was a statistically
significant difference; dCompared with T group, there
was a statistically significant difference. Tie2, tyrosine kinase
receptor 2; G, glucose treatment; N, pRNAT-CMV3.2-Neo carrying
negative siRNA treatment; C, carboplatin treatment; T,
pRNAT-CMV3.2-Neo carrying Tie2-siRNA treatment; A, Tie2-siRNA in
combination with carboplatin treatment. |
Difference in expression level of Tie2
protein following treatment with Tie2-siRNA and/or carboplatin
Since the expression of Tie2 mRNA was significantly
reduced following treatment with Tie2-siRNA and/or carboplatin, the
effects of this treatment on Tie2 protein expression levels in the
present treatment groups was investigated next. Xenograft
homogenates were analyzed by western blotting and probed with
anti-Tie2 antibody and GAPDH was used as a loading control. The
results of the blotting revealed that the Tie2 protein levels were
significantly reduced in the C (0.805±0.085), T (0.670±0.109) and A
(0.590±0.135) groups compared with the G (1.059±0.085) or N
(1.018±0.069) groups (Fig. 2B and
C). The protein level in the A group exhibited the most marked
reduction and was significantly different compared with treatment
using carboplatin or Tie2-siRNA alone (P<0.05). Taken together
with the real-time PCR data, it may be suggested that silencing the
Tie2 gene enhances the the antitumor activity of carboplatin. This
may be through the normalization of tumor vessels during the
chemotherapy period.
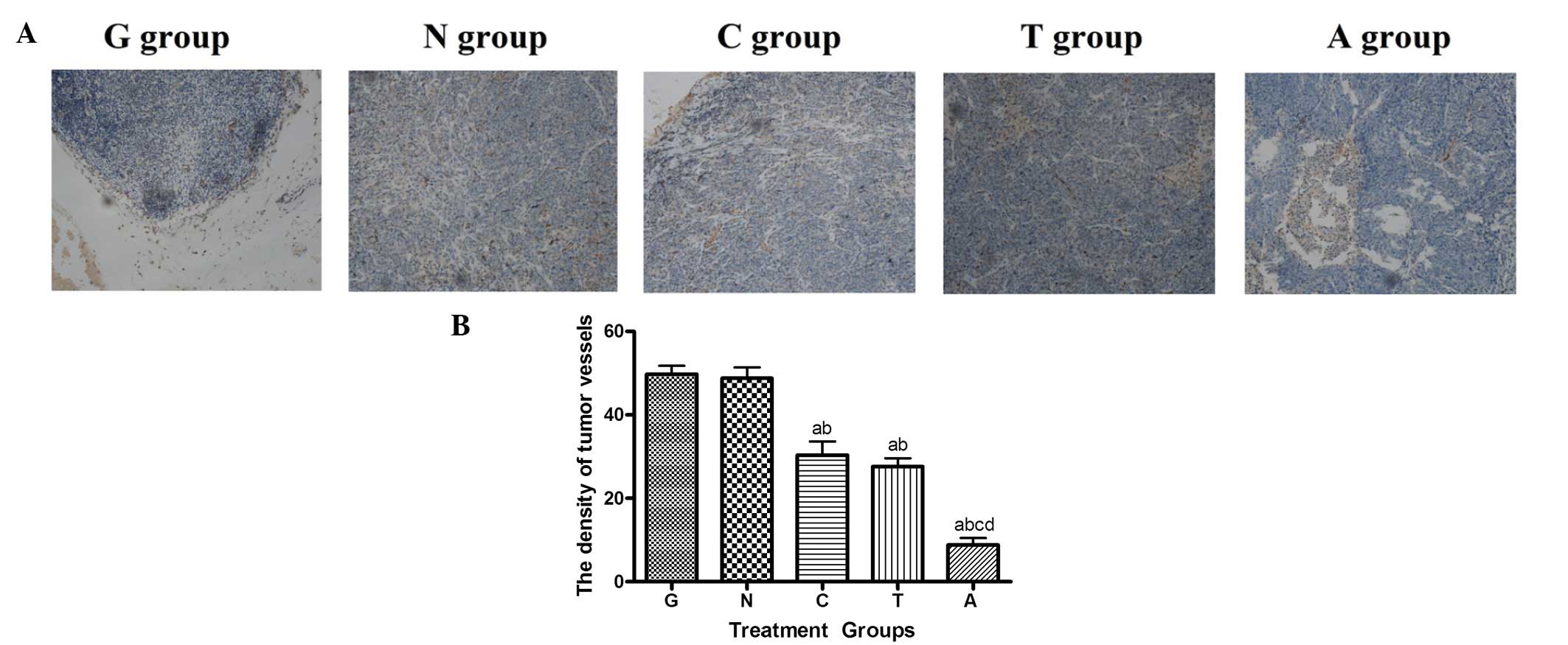
Differences in tumor vascularity
following treatment with Tie2-siRNA and/or carboplatin
The growth of new blood vessels has an important
role in tumor progression. To determine whether Tie2 siRNA-mediated
downregulation of Tie2 was involved in the inhibition of
angiogenesis, the density of tumor vessels was investigated by
immunohistochemical assessment and probed with anti-CD34 antibody.
The expression of CD34 in the tumor tissues of T (27.60±4.56)
group, C (35.80±2.17) and A (15.40±2.07) group was poor, but was
high in the G (49.80±4.44) and N groups (48.80±5.81). Microvessel
counting showed that the MVD was higher in the G and N groups
compared with the T group (Fig.
3A).
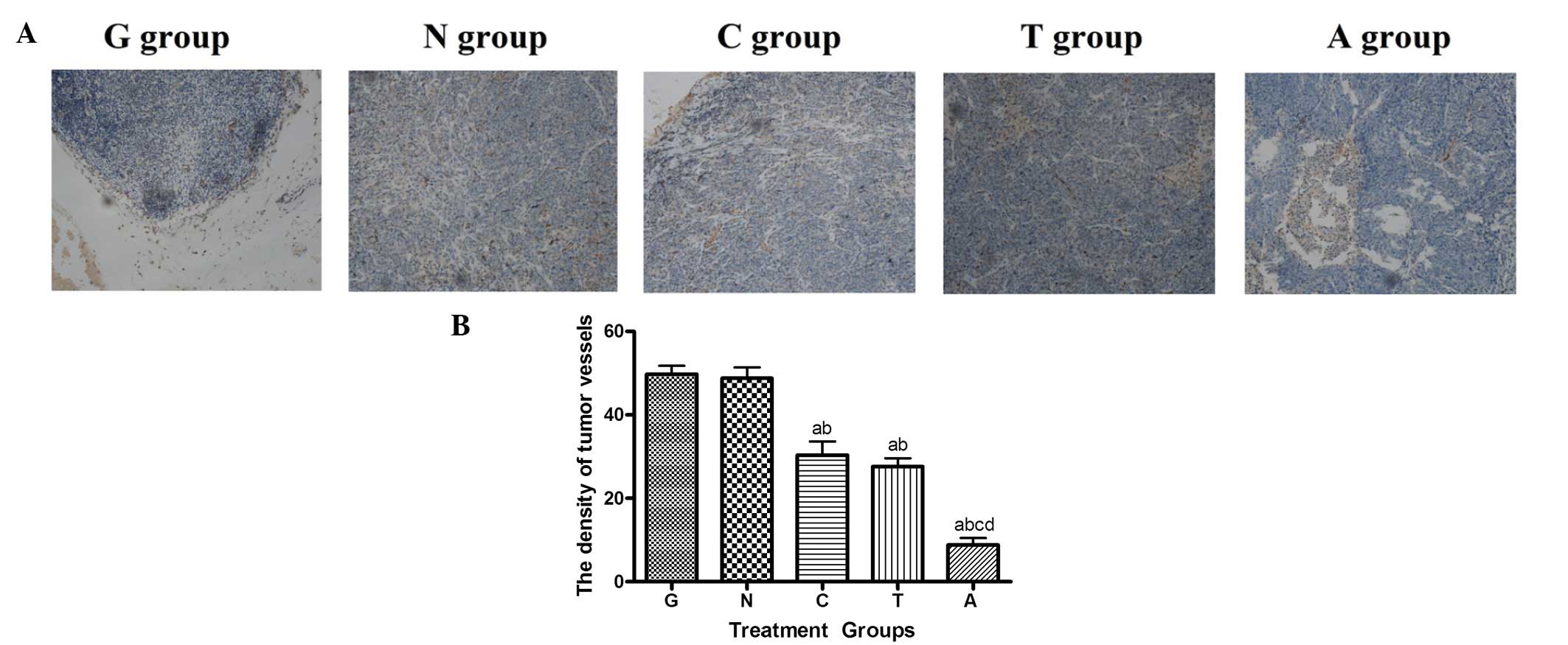 | Figure 3Inhibition of tumor angiogenesis
following treatment. (A) Immunohistochemical staining of tumor
xenografts probed with anti-CD34 antibody after adminastration to
visualize endothelial cells and tumor vascular formation. The
images of the microvessel density and vessel characteristics of the
treatment groups are shown (magnification, ×200). (B) Results of
immunohistochemical staining. The densitiy of tumor vessels were
lower in the carboplatin, Tie2-siRNA and the combined
administration groups than those in the G and N groups (P<0.05).
The combined administration group showed the greatest reduction in
the number of tumor vessels and the reduction was significantly
different compared with the other groups (P<0.05).
aCompared with G group, there was a statistically
significant difference; bCompared with N group, there
was a statistically significant difference; cCompared
with C group, there was a statistically significant difference;
dCompared with T group, there was a statistically
significant difference. Tie2, tyrosine kinase receptor 2; G,
glucose treatment; N, pRNAT-CMV3.2-Neo carrying negative siRNA
treatment; C, carboplatin treatment; T, pRNAT-CMV3.2-Neo carrying
Tie2-siRNA treatment; A, Tie2-siRNA in combination with carboplatin
treatment. |
Discussion
Angiogenesis is a key element for the development of
tumors as it provides new blood supplies and subsequently allows
malignant progression. This suggests a new strategy for the
treatment of carcinoma. The critical role of angiogenesis in
ovarian and endometrial function has been demonstrated previously
(12). During tumor angiogenesis,
vascular quiescence and stabilization are regulated by different
signal molecules. It is generally accepted that tumor angiogenesis
is the result of unbalanced expression of angiogenic factors.
Angiogenesis also involves an extremely complicated
network and is modulated by numerous growth factors. Vascular
endothelial growth factor (VEGF), expressed predominantly on
vascular endothelial cells, is one of the most important regulators
of vascularization and an attractive target for anti-angiogenic
therapy. VEGF is the most importaint angiogenic regulator that
increases vascular permeability and promotes endothelial
proliferation (12). Agents such as
endostatin and anti-VEGF antibodies that inhibit the VEGF receptor
have been developed and may result in effective inhibition of solid
tumor growth in vivo(13–16).
However, VEGF-targeted therapy is restricted by its transient
responses in the clinic due to drug resistance and it has been
reported that the agents were not effective for all tumor types,
indicating that blocking VEGF activation alone may not be
sufficient to completely halt tumor angiogenesis, since
angiopoietin and other factors are also involved.
Tie and angiopoietin (Ang) are involved in another
signaling system which is not only crucial for angiogenesis and
vascular homeostasis, but is also vital in the progression of
numerous types of cancer (17–19).
Ang1 is produced by pericytes and other cells, whereas Ang2 and
Tie2 are expressed mainly on endothelial cells. Tie2 was originally
identified as the second member of an orphan RTK subfamily and is
an Ang-specific receptor with a critical role in the modulation of
vascular generation and remodeling (20–22).
It has been reported that Tie2 is critical in tumor-induced
angiogenesis (23). The suppression
of Tie2 signaling caused by the use of specific blocking agents may
be able to suppress the growth of tumors and several studies have
shown that interfering with the Tie2 receptor pathway resulted in
the inhibition of tumor angiogenesis and growth (24–27).
The expression of Tie2 in tumor vessels may also indicate a role
for Tie2 in tumor angiogenesis and the pathological angiogenesis
contributing to the progression of diseases. Thus this strategy may
be used for anti-angiogenesis treatment in anticancer therapy. The
Tie/Ang system is important for endometrial vessel development
during the postovulatory phase and has a critical association with
the initiation of endometrial diseases. Thus the potential for
inhibiting angiogenesis is likely to have implications for the
treatment of endometrial cancer.
Chemotherapy is an important and complementary
treatment for advanced and recurrent patients with endometrial
cancer and platinum-based chemotherapy has been an important
treatment for these patients. Carboplatin is cis-diammine
(1,1-cyclobutanedicarboxylate) platinum which has an effective
activity against human tumors. It has little renal toxicity,
ototoxicity or neurotoxicity compared with cisplatin in clinical
studies. Early studies have shown that carboplatin acts through the
inhibition of DNA replication and transcription and by shielding
the repair of damaged DNA. However, the mechanisms of carboplatin
action may be more complicated, and research concerning the
anticancer mechanism of carboplatin is scarce.
The present study aimed to elucidate the role of
Tie2 in the carcinogenesis and progression of endometrial carcinoma
via angiogenesis, with a focus on establishing a basis for the
development of complementary molecule targeting action. The
experiments showed that the treatment of endometrial cacinoma in
nude mice with carboplatin and Tie2-siRNA, alone or in combination,
resulted in delays in tumor growth and reductions in tumor size and
vascularity (Figs. 1 and 3). Tie2 expression was significantly
silenced in the tumor tissues of the combined therapy, Tie2-siRNA
and carboplatin treatment groups, which was consistent with
previous studies (28). This may
indicate that Tie2 is important in the carcinogenesis and
progression of cancer via angiogenesis.
It is well known that tumor vessels are structurally
and functionally abnormal. Tumor vessels may be tortuous and leaky,
lacking the hierarchical arrangement of arterioles, capillaries and
venules and existing in a constantly dynamic state, which becomes
increasingly resistent to conventional chemotherapy due to the slow
proliferation of cells (29). The
vessel number and normalized tumor vessels are enough to maintain
tumor growth (20). Current
anticancer therapies use normalized tumor vessels to deliver
chemotherapeutics or other cancer cell-targeting drugs more
efficiently (30). In the present
study, during the combined administration, the expression of Tie2
was silenced first in order to normalize the tumor vascularity,
followed by the administration of the chemotherapeutic drug
carboplatin, so carboplatin was able to affect all areas of the
tumors. The combined administration exhibited more noticeable
effects in delaying tumor growth and reducing tumor size and
vascularity compared with carboplatin or Tie2-siRNA administration
alone, and the difference was significant. This was in accordance
with previous studies (31) and
also showed a role for Tie2 in tumor angiogenesis.
The growth and maintenance of tumor blood vessels
depend on multiple growth factors. Making use of the effect of the
interplay among the growth factors is required in order to advance
growth factor-targeted cancer therapies. Thus, agents that block
multiple angiogenesis targets are being developed for the treatment
of tumors. In the present study, a nude mouse endometrial carcinoma
model was successfully constructed and the critical role of the
Tie2 gene in tumor angiogenesis and endometrial carcinoma was
demonstrated. It is the first time that the inhibition of the Tie2
gene has been used in combination with carboplatin to suppress
tumor growth in endometrial carcinoma by interrupting tumor
angiogenesis in xenograft models. The present findings revealed
that local administration of Tie2-siRNA is able to mediate
effective knockdown of the target protein and suppress tumor growth
in vivo. Together with the other results of the present
study, this may suggest that intratumor injections of
pRNAT-CMV3.2-Tie2 may silence the expression of Tie2, subsequently
eliminate the tumor angiogenesis and metastasis pathway regulated
by Tie2 and increase the efficiency of chemotherapy for endometrial
carcinoma using carboplatin. However, siRNAs are not an optimal
treatment due to their short half lives and transient effects
(32,33). Other anti-Tie2 treatment modalities
more suitable for therapy, such as modified RNAi or an antibody,
should be developed in the future. At present, little is known with
regard to the abnormal stucture and function and the hierarchical
arrangement of arterioles, capillaries and venules of tumor
vessels. Microangiography may be useful for structural and
functional studies of tumor vessels in future. In summary, the
findings of the present study reveal a new direction for the
rational design and scheduling of siRNA-based molecular targeting
therapeutic strategies in combination with anti-angiogenic drugs
and/or other therapies.
Acknowledgements
The present study was supported by a
grant (ZKX09023) awarded by the Health Department of Nanjing
(Jiangsu, China). The authors gratefully acknowledge Professor L.H.
Wei (Peking University People’s Hospital, Beijing, China) for
providing the Ishikawa cell line.
References
|
1
|
National Cancer Institute at the National
Institutes of Health: Endometrial Cancer Home Page. http://seer.cancer.gov/statfacts/html/corp.html
Accessed November 10, 2010.
|
|
2
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
3
|
Myatt SS, Wang J, Monteiro LJ, Christian
M, Ho KK, Fusi L, Dina RE, Brosens JJ, Ghaem-Maghami S and Lam EW:
Definition of microRNAs that repress expression of the tumor
suppressor gene FOXO1 in endometrial cancer. Cancer Res.
70:367–377. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ray M and Fleming G: Management of
advanced-stage and recurrent endometrial cancer. Semin Oncol.
36:145–154. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Poon RT, Lau CP, Ho JW, Yu WC, Fan ST and
Wong J: Tissue factor expression correlates with tumor angiogenesis
and invasiveness in human hepatocellular carcinoma. Clin Cancer
Res. 9:5339–5345. 2003.PubMed/NCBI
|
|
6
|
Carmeliet P: Angiogenesis in life, disease
and medicine. Nature. 438:932–936. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sistla A, Kertelj A and Shenoy N:
Development of an intravenous formulation of SU010382 (prodrug of
SU5416, an anti-angiogenesis agent). PDA J Pharm Sci Technol.
62:200–210. 2008.PubMed/NCBI
|
|
8
|
Griffioen AW: Anti-angiogenesis: making
the tumor vulnerable to the immune system. Cancer Immunol
Immunother. 57:1553–1558. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kimura Y, Sumiyoshi M and Baba K:
Anti-tumor actions of major component 3′-O-acetylhamaudol of
Angelica japonica roots through dual actions,
anti-angiogenesis and intestinal intraepithelial lymphocyte
activation. Cancer Lett. 265:84–97. 2008.PubMed/NCBI
|
|
10
|
Schmittgen TD and Livak KJ: Analyzing
real-time PCR data by the comparative C(T) method. Nat Protoc.
3:1101–1108. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Weidner N: Current pathologic methods for
measuring intratumoral microvessel density within breast carcinoma
and other solid tumors. Breast Cancer Res Treat. 36:169–180. 1995.
View Article : Google Scholar
|
|
12
|
Klauber N, Rohan RM, Flynn E and D’Amato
RJ: Critical components of the female reproductive pathway are
suppressed by the angiogenesis inhibitor AGM-1470. Nat Med.
3:443–446. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamaguchi R, Yano H, Nakashima Y,
Ogasawara S, Higaki K, Akiba J, Hicklin DJ and Kojiro M: Expression
and localization of vascular endothelial growth factor receptors in
human hepatocellular carcinoma and non-HCC tissues. Oncol Rep.
7:725–729. 2000.PubMed/NCBI
|
|
14
|
Miller K, Wang M, Gralow J, Dickler M,
Cobleigh M, Perez EA, Shenkier T, Cella D and Davidson NE:
Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic
breast cancer. N Engl J Med. 357:2666–2676. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gerber HP and Ferrara N: Pharmacology and
pharmacodynamics of bevacizumab as monotherapy or in combination
with cytotoxic therapy in preclinicals studies. Cancer Res.
65:671–680. 2005.PubMed/NCBI
|
|
16
|
Ferrara N and Kerbel RS: Angiogenesis as a
therapeutic target. Nature. 438:967–974. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sandler A, Gray R, Perry MC, Brahmer J,
Schiller JH, Dowlati A, Lilenbaum R and Johnson DH:
Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell
lung cancer. N Engl J Med. 355:2542–2550. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sugimachi K, Tanaka S, Taguchi K, Aishima
S, Shimada M and Tsuneyoshi M: Angiopoietin switching regulates
angiogenesis and progression of human hepatocellular carcinoma. J
Clin Pathol. 56:854–860. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hu B, Guo P, Fang Q, Tao HQ, Wang D,
Nagane M, Huang HJ, Gunji Y, Nishikawa R, Alitalo K, Cavenee WK and
Cheng SY: Angiopoietin-2 induces human glioma invasion through the
activation of matrix metalloprotease-2. Proc Natl Acad Sci USA.
100:8904–8909. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yang H, Yang K, Hu JK, Tang H, Zhang B,
Chen ZX, Wang YJ and Chen JP: Eukaryotic expression of
extracellular ligand binding domains of murine Tie-2 and its
anti-angiogenesis effect in SGC-7901 cell lines. J Gastroenterol
Hepatol. 25:345–351. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dumont DJ, Yamaguchi TP, Conlon RA,
Rossant J and Breitman ML: tek, a novel tyrosine kinase gene
located on mouse chromosome 4, is expressed in endothelial cells
and their presumptive precursors. Oncogene. 7:1471–1480.
1992.PubMed/NCBI
|
|
22
|
Sato TN, Tozawa Y, Deutsch U,
Wolburg-Buchholz K, Fujiwara Y, Gendron-Maguire M, Gridley T,
Wolburg H, Risau W and Qin Y: Distinct roles of the receptor
tyrosine kinases Tie-1 and Tie-2 in blood vessel formation. Nature.
376:70–74. 1995. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Suri C, Jones PF, Patan S, Bartunkova S,
Maisonpierre PC, Davis S, Sato TN and Yancopoulos GD: Requisite
role of angiopoietin-1, a ligand for the TIE2 receptor, during
embryonic angiogenesis. Cell. 87:1171–1180. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Eklund L and Olsen BR: Tie receptors and
their angiopoietin ligands are context-depedent regulators of
vascular remodeling. Exp Cell Res. 312:630–641. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mori Y, Sahara H, Matsumoto K, Takahashi
N, Yamazaki T, Ohta K, Aoki S, Miura M, Sugawara F, Sakaguchi K and
Sato N: Downregulation of Tie2 gene by a novel antitumor
sulfolipid, 3′-sulfoquinovosyl-1′-monoacylglycerol, targeting
angiogenesis. Cancer Sci. 99:1063–1070. 2008.PubMed/NCBI
|
|
26
|
Mai J, Song S, Rui M, Liu D, Ding Q, Peng
J and Xu Y: A synthetic peptide mediated active targeting of
cisplatin liposomes to Tie2 expressing cells. J Control Release.
139:174–181. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yamakawa D, Kidoya H, Sakimoto S, Jia W
and Takakura N: 2-Methoxycinnamaldehyde inhibits tumor angiogenesis
by suppressing Tie2 activation. Biochem Biophys Res Commun.
415:174–180. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tournaire R, Simon MP, le Noble F,
Eichmann A, England P and Pouysségur J: A short synthetic peptide
inhibits signal transduction, migration and angiogenesis mediated
by Tie2 receptor. EMBO Rep. 5:262–267. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Maschek G, Savaraj N, Priebe W,
Braunschweiger P, Hamilton K, Tidmarsh GF, De Young LR and Lampidis
TJ: 2-deoxy-D-glucose increases the efficacy of adriamycin and
paclitaxel in human osteosarcoma and non-small cell lung cancers
in vivo. Cancer Res. 64:31–34. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sennino B, Falcón BL, McCauley D, Le T,
McCauley T, Kurz JC, Haskell A, Epstein DM and McDonald DM:
Sequential loss of tumor vessel pericytes and endothelial cells
after inhibition of platelet-derived growth factor B by selective
aptamer AX102. Cancer Res. 67:7358–7367. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jain RK: Normalization of tumor
vasculature: an emerging concept in antiangiogenic therapy.
Science. 307:58–62. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Devroe E and Silver PA: Therapeutic
potential of retroviral RNAi vectors. Expert Opin Biol Ther.
4:319–327. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Behlke MA: Chemical modification of siRNAs
for in vivo use. Oligonucleotides. 18:305–319. 2008.
View Article : Google Scholar : PubMed/NCBI
|