Introduction
Desmoid tumors (DTs), also known as aggressive
fibromatoses, are benign myofibroblastic neoplasms originating from
muscular aponeuroses that are also classified as deep fibromatoses
(1). They constitute 3% of all soft
tissue tumors and 0.03% of all neoplasms (2). Despite their aggressive local
infiltration, DTs lack metastatic potential (3). However, the local infiltrations and
compressions of surrounding structures demonstrate a high
recurrence rate, and in anatomic locations with restricted access
to surgical resection, may lead to fatalities (4). DTs usually occur in fertile females
and are uncommon during the menopause; during pregnancy an increase
in volume occasionally occurs in already existing tumors. This
corroborates the estrogen-stimulated tumor growth hypothesis
(5). Numerous studies have
demonstrated that 37–50% of DTs are initiated in the abdominal area
(6). Abdominal DTs occur
sporadically or are associated with certain familial syndromes,
such as familial adenomatous polyposis (FAP) (7).
This report presents the case of this rare
fibromatosis in a 17-year-old female who had no history of trauma,
abdominal surgery or childbearing. The appearance of the tumor was
analyzed using computed tomography (CT). Informed consent was
obtained from the patient prior to the study.
Case report
A 17-year-old female was admitted to the Department
of General Surgery, The Second Affiliated Hospital of Dalian
Medical University (Dalian, Liaoning, China) with a painless mass
in the left anterolateral abdomen. During a physical examination,
the mass was observed to be firm, lacking tenderness and fixed to
the abdominal wall. The patient stated that the mass was gradually
increasing in size. The patient had no relevant family history and
no history of smoking, drinking alcohol or taking any medication.
The analyzed blood parameters were within the normal range and the
tumor marker results were negative. The patient had no history of
trauma, surgery or childbearing.
Pre-operative CT scans revealed a large mass
(9.3×6.1 cm) with unclear borders of attenuation equal to that of
muscle. The mass originated from the left rectus abdominis muscle
and, following intravenous administration of contrast medium,
demonstrated mild enhancement, even in the delayed images (Fig. 1).
Radical resection of the affected abdominal wall
musculature was performed down to the peritoneum, and including a
peripheral margin of 3 cm of healthy tissue. Following the
resection of the DT, the abdominal wall defect was replaced with a
Bard Composix EX Mesh (Bard Inc., Cranston, RI, USA).
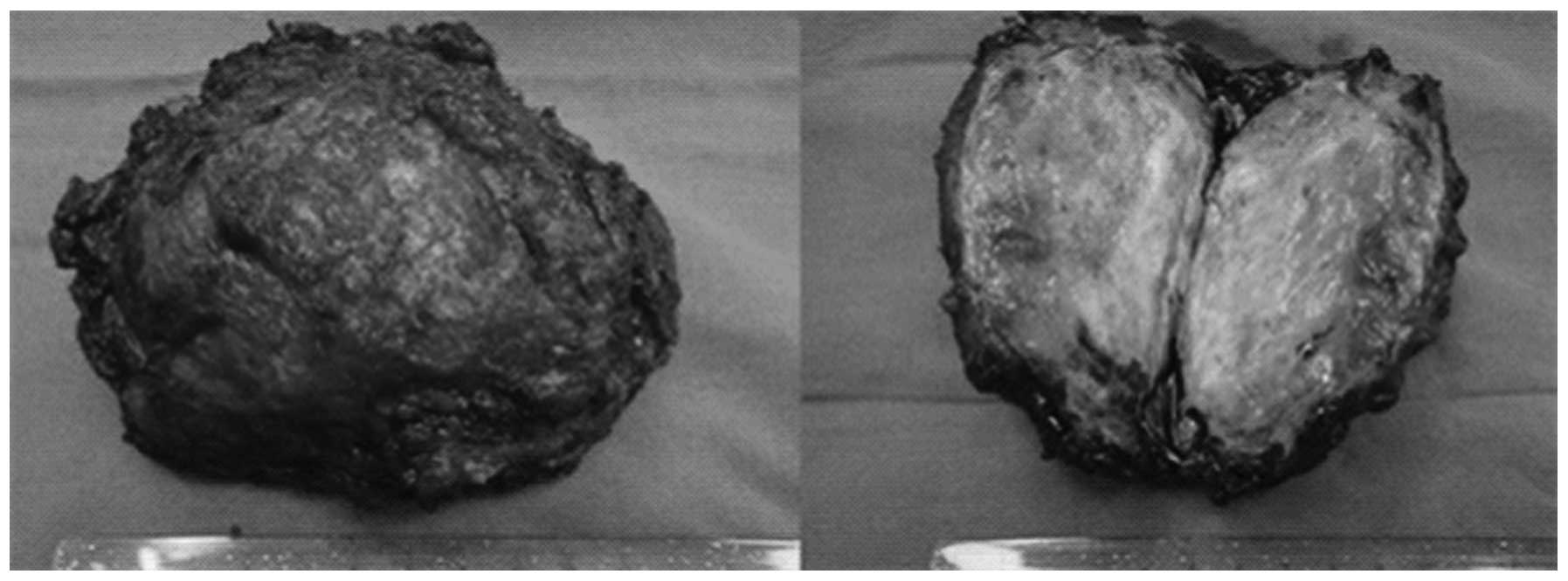
Macroscopically, the tumor had a firm texture. On the cut surface,
it was pale and certain areas had the appearance of fish meat. The
tumor has no confirmed capsule, and its margin was ill-defined
(Fig. 2). The histological
diagnosis was of a DT (Fig. 3). The
post-operative course was uneventful and the patient was discharged
on the ninth post-operative day. After a follow-up of 5 months from
the end of surgery, the patient remains in good health and complete
remission without any other treatment.
Discussion
DTs are benign deep fibromatoses that originate from
fascia and muscular aponeuroses, with an infiltrating growth
pattern (8). DTs are rare tumors
with ∼3.7 new cases occurring per one million individuals each year
(9). Primarily located abdominally
or intra-abdominally (1), DTs have
been correlated with the female gender, FAP (10) and occasionally with surgical trauma
(11). They have a higher
prevalence in females who have experienced pregnancy (12). In the present case, the patient had
no history of trauma, surgery or childbearing. Despite their
aggressive local infiltration, DTs do not metasta-size to other
parts of the body (13–15). Depending on the tumor size, the
chosen therapy and the negative resection margins, recurrence is
present in ≤45% of cases (16).
Several modern imaging methods, including abdominal
ultrasonography, CT and magnetic resonance imaging (MRI), are used
for the diagnosis of DTs (17). In
ultrasonography, desmoids have a variable echogenicity, with
smooth, well-defined margins. In contrast-enhanced CT scans, the
tumors are generally characterized by high attenuation (relative to
muscle) and have either ill- or well-defined margins. A CT scoring
system has been developed, characterizing specimens according to
the presence of desmoid precursor lesions (‘mesenteric fibrosis’)
and true DTs. This has provided further evidence for a stepwise
progression in desmoid development (18). In MRI scans, DTs have a low signal
intensity relative to muscle on T1-weighted images, and a variable
signal intensity on T2-weighted images (19). MRI scans indicate how the tumors are
likely to behave, with a bright signal indicating a high water
content, which has been correlated with rapid growth (20). Although there are no specific
imaging features to distinguish DTs from other solid masses, the
diagnosis of DTs should be considered in patients with an abdominal
mass, a history of previous abdominal surgery or injury and where
there may be an association with FAP. A definitive diagnosis must
be established with a histopathological analysis (21). Characteristically, there is diffuse
cell infiltration of the adjacent tissue structures. In addition,
the immunohistochemical response for actin may be partially
positive, and immunohistochemical muscle cell markers may delimit
DTs from fibrosarcoma (22).
The treatment of neoplasms, such as DTs, is guided
by their clinical and evolutive characteristics. Radical therapy
consists of wide tumor and adjoining tissue resections (23). Surgery has a key role in the
management of abdominal DTs; the resection of abdominal wall
(superficial) DTs is simple and may be performed safely when the
lesion is growing and possesses clear margins (24,25).
Incomplete resection is correlated with high recurrence rates.
Abdominal wall reconstruction may be achieved by direct repair
(with sutures), or by using synthetic materials (meshes) or
myocutaneous flaps when the defect is extensive (26–28).
In the present case, the peritoneal defect was replaced with a Bard
Composix mesh. Prosthetic materials are more susceptible to
bacterial infection and other complications (29,30),
although newly developed materials have exhibited encouraging
experimental results (31).
Radiation therapy has been used predominantly for the treatment of
extra-abdominal DTs, and has resulted in an improvement in the
local control of DTs by reducing local recurrence rates (32). External beam irradiation or
brachytherapy may be used alone, predominantly in patients with
inoperable lesions (33), although
they are correlated with high failure rates (34). They may also be used either prior to
surgery, or as adjuvant therapies following incomplete
(non-radical) surgical resection.
In conclusion, the optimal treatment for DTs remains
unclear. Surgery is the primary treatment option, although it
carries a risk of local recurrence. A radical resection with clear
margins remains the principal determinant of outcome. The repair of
abdominal wall defects may be achieved with prosthetic mesh
reconstruction, which leads to good functional results.
Non-surgical treatments result in diverse and unpredictable
outcomes, but are considered as an option for adjuvant therapy in
patients with unresectable lesions.
Acknowledgements
This study was supported by a grant
from the National Natural Science Foundation of China (no.
81250025).
References
|
1
|
Fletcher CD: Myofibroblastic tumours: an
update. Verh Dtsch Ges Pathol. 82:75–82. 1998.
|
|
2
|
Kiel KD and Suit HD: Radiation therapy in
the treatment of aggressive fibromatoses (desmoid tumors). Cancer.
54:2051–2055. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lewis JJ, Boland PJ, Leung DH, Woodruff JM
and Brennan MF: The enigma of desmoid tumors. Ann Surg.
229:866–873. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Merchant NB, Lewis JJ, Woodruff JM, Leung
DH and Brennan MF: Extremity and trunk desmoid tumors: a
multifactorial analysis of outcome. Cancer. 86:2045–2052. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Enzinger FM and Weiss SW: Soft Tissue
Tumours. 3rd edition. Mosby; St Louis, MO: pp. 201–229. 1995
|
|
6
|
Lefevre JH, Parc Y, Kernéis S, Goasguen N,
Benis M, Parc R and Tiret E: Risk factors for development of
desmoids tumours in familial adenomatous polyposis. Br J Surg.
95:1136–1139. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lips DJ, Barker N, Clevers H and Hennipman
A: The role of APC and beta-catenin in the aetiology of aggressive
fibromatosis (desmoid tumors). Eur J Surg Oncol. 35:3–10. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hasegawa SL and Fletcher CDM: Fibromatosis
in the adult. Adv Pathol. 9:259–275. 1996.
|
|
9
|
Economou A, Pitta X, Andreadis E,
Papapavlou L and Chrissidis T: Desmoid tumor of the abdominal wall:
a case report. J Med Case Rep. 5:3262011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Soravia C, Berk T, McLeod RS and Cohen Z:
Desmoid disease in patients with familial adenomatous polyposis.
Dis Colon Rectum. 43:363–369. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Cian F, Delay E, Rudigoz RC, Ranchère D
and Rivoire M: Desmoid tumor arising in a cesarean section scar
during pregnancy: monitoring and management. Gynecol Oncol.
75:145–148. 1999.PubMed/NCBI
|
|
12
|
Gansar GF, Markowitz IP and Cerise EJ:
Thirty years of experience with desmoid tumors at Charity Hospital.
Am Surg. 53:318–319. 1987.PubMed/NCBI
|
|
13
|
Kumar V, Khanna S, Khanna AK and Khanna R:
Desmoid tumors: experience of 32 cases and review of the
literature. Indian J Cancer. 46:34–39. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Overhaus M, Decker P, Fischer HP, Textor
HJ and Hirner A: Desmoid tumors of the abdominal wall: A case
report. World J Surg Oncol. 1:112003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lahat G, Nachmany I, Itzkowitz E,
Abu-Abeid S, Barazovsky E, Merimsky O and Klauzner J: Surgery for
sporadic abdominal desmoid tumor: is low/no recurrence an
achievable goal? Isr Med Assoc J. 11:398–402. 2009.PubMed/NCBI
|
|
16
|
Nuyttens JJ, Rust PF, Thomas CR Jr and
Turrisi AT III: Surgery versus radiation therapy for patients with
aggressive fibromatosis or desmoid tumors: A comparative review of
22 articles. Cancer. 88:1517–1523. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Church J, Berk T, Boman BM, Guillem J,
Lynch C, Lynch P, Rodriguez-Bigas M, Ruslin L and Weber T;
Collaborative Group of the Americas on Inherited Colorectal Cancer:
Staging intra-abdominal desmoid tumors in familial adenomatous
polyposis: a search for a uniform approach to a troubling disease.
Dis Colon Rectum. 48:1528–1534. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Middleton SB, Clark SK, Matravers P, Katz
D, Reznek R and Phillips RK: Stepwise progression of familial
adenomatous polyposis-associated desmoid precursor lesions
demonstrated by a novel CT scoring system. Dis Colon Rectum.
46:481–485. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Healy JC, Reznek RH, Clark SK, Phillips RK
and Armstrong P: MR appearances of desmoid tumors in familial
adenomatous polyposis. AJR Am J Roentgenol. 169:465–472. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cassilas J, Sais GJ, Greve JL,
Iparraguirre MC and Morillo G: Imaging of intra- and extraabdominal
desmoid tumors. Radiographics. 11:959–968. 1991. View Article : Google Scholar
|
|
21
|
Teo HE, Peh WC and Shek TW: Case 84:
desmoid tumor of the abdominal wall. Radiology. 236:81–84. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mentzel T and Katenkamp D: Myofibroblastic
tumors. Brief review of clinical aspects, diagnosis and
differential diagnosis. Pathologe. 19:176–186. 1998.(In
German).
|
|
23
|
Catania G, Ruggeri L, Iuppa G, Di Stefano
C, Cardi F and Iuppa A: Abdominal wall reconstruction with
intraperitoneal prosthesis in desmoid tumors surgery. Updates Surg.
64:43–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Latchford AR, Sturt NJ, Neale K, Rogers PA
and Philips RK: A 10-year review of surgery for desmoid disease
associated with familial adenomatous polyposis. Br J Surg.
93:1258–1264. 2006.
|
|
25
|
Sturt NJ and Clark SK: Current ideas in
desmoid tumors. Fam Cancer. 5:275–285; discussion 287–288. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Brenner P and Rammelt S: Abdominal wall
and foot reconstruction after extensive desmoid tumor resection
with free tissue transfer. Langenbecks Arch Surg. 386:592–597.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rohrich RJ, Lowe JB, Hackney FL, Bowman JL
and Hobar PC: An algorithm for abdominal wall reconstruction. Plast
Reconstr Surg. 105:202–216. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bauer JJ, Salky BA, Gelernt IM and Kreel
I: Repair of large abdominal wall defects with expanded
polytetrafluoroethylene (PTFE). Ann Surg. 206:765–769. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Disa JJ, Klein MH and Goldberg NH:
Advantages of autologous fascia versus synthetic patch abdominal
reconstruction in experimental animal defects. Plast Reconstr Surg.
97:801–806. 1996. View Article : Google Scholar
|
|
30
|
Leber GE, Garb JL, Alexander AI and Reed
WP: Long-term complications associated with prosthetic repair of
incisional hernias. Arch Surg. 133:378–382. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Disa JJ, Chiaramonte MF, Girotto JA, Klein
MH and Goldberg NH: Advantages of autologous fascia versus
synthetic patch abdominal reconstruction in experimental animal
defects. Plast Reconstr Surg. 108:2086–2087. 2001. View Article : Google Scholar
|
|
32
|
Micke O and Seegenschmiedt MH; German
Cooperative Group on Radiotherapy for Benign Diseases: Radiation
therapy for aggressive fibromatosis (desmoid tumors): results of a
national Patterns of Care Study. Int J Radiat Oncol Biol Phys.
61:882–891. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sherman NE, Romsdahl M, Evans H, Zagars G
and Oswald MJ: Desmoid tumors: a 20-year radiotherapy experience.
Int J Radiat Oncol Biol Phys. 19:37–40. 1990.PubMed/NCBI
|
|
34
|
Moslein G and Dozois RR: Desmoid tumors
associated with familial adenomatous polyposis. Perspect Colon
Rectal Surg. 10:109–126. 1998.
|