Introduction
Malignant mesotheliomas are a rare form of cancer
derived from pleural mesothelial cells. In contrast to diffuse
mesothelioma, localized malignant mesothelioma is uncommon and
localized malignant mesothelioma in the mediastinum is extremely
rare (1). Malignant mesotheliomas
have been described under a variety of names, including benign
mesothelioma, localized mesothelioma, fibrous mesothelioma,
subpleural fibroma and localized fibrous tumor of the pleura. The
majority of malignant mesotheliomas are benign; however, diffuse
mesotheliomas are malignant. Approximately 60% of cases occur in
the pleura and ∼35% in the peritoneum. They are usually
asymptomatic, although occasionally patient present with coughing,
pain, dyspnea and pulmonary osteoarthropathy. The tumor is not
associated with asbestosis. Mesotheliomas may be confused with
other spindle cell tumors, including fibrosarcoma, smooth muscle
tumors and neurogenic tumors. Immunohistochemical examination is
useful in the differential diagnosis and classification of
mesothelioma. The main treatment methods of malignant mesothelioma
are wide resection of the border, chemotherapy and combined
therapy. Prognosis is extremely poor (2).
To the best of our knowledge, only a few cases of
localized malignant mesothelioma have been reported in the
English-language literature. The present study reports a new case
of localized malignant mesothelioma in the upper mediastinum. This
study was approved by the ethics committee of Shandong Tumor
Hospital, Jinan, China. Written informed consent was obtained from
the patient’s family.
Case report
A 29-year-old female patient was admitted to
Shandong Tumor Hospital and Institute (Jinan, China) on July 17,
2012, due to coughing that had lasted for one month and a fever
that had been present for seven days. The patient had no history of
any remarkable asbestos exposure. No abnormalities were noted upon
physical examination and the patient exhibited no heart-involved
symptoms. Furthermore, no heart abnormalities were detected by
electrocardiogram and color ultrasonography studies. Laboratory
tests showed that the leukocyte level was 7.8×109/l and
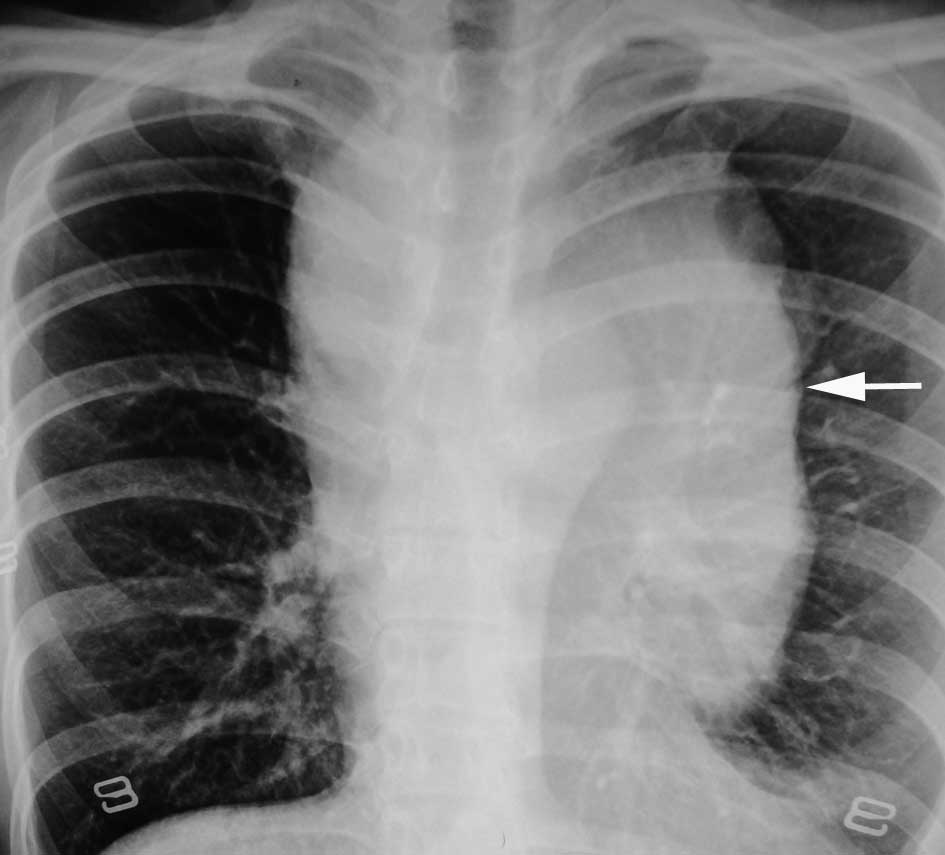
the level of carcinoembryonic antigen (CEA) was 1.7 ng/ml. A chest
radiograph revealed a projecting abnormal giant upper mediastinal
shadow (Fig. 1). A
contrast-enhanced computed tomography (CT) scan revealed an upper
mediastinal tumor, 9.0×10.0 cm in size, adjacent to the aortic
arch, trachea, superior vena cava and left pulmonary artery. The
vessels in the mediastinum were compressed and shifted to the lower
right. The trachea became stenotic, but there was no evidence of
invasion. Although a small amount of bilateral pleural effusion was
observed, there was no pericardial effusion. The mass was
relatively well encapsulated. There was no pleural thickening or
clearly swollen lymph nodes in the mediastinum. Heterogeneous and
weak enhancement was observed during the arterial and delayed
phases (Fig. 2).
A detailed general examination showed no other
metastatic or primary lesions. A CT-guided puncture biopsy of the
mediastinal mass failed to provide a pathological diagnosis. Based
on the suspicion of a mediastinal tumor, thoracoscopic surgery and
surgical biopsies of the mass were performed. During surgery, it
was observed that the mass was located in the upper mediastinum
under the normal mediastinal pleura and convex to the left chest
cavity. The surface of the tumor was smooth and uneven, and the
tumor was an elastic-hard mass, measuring 8.0×9.0 cm. Furthermore,
the tumor was in a frozen state with the mediastinal tissue, with
no metastatic nodules in the pleural membrane and mediastinal
pleura, and a small number of light-yellow pleural effusions. Four
sections were cut and sent for pathological examination. In the
macroscopic analysis, the soft tissue sections were pale and the
quality of the material was fine. Through microscopic analysis, it
was observed that the large atypical mesothelial tumor cells
proliferated in a diffuse or nodular pattern. Frequent mitoses and
small foci of tumor necrosis were also observed.
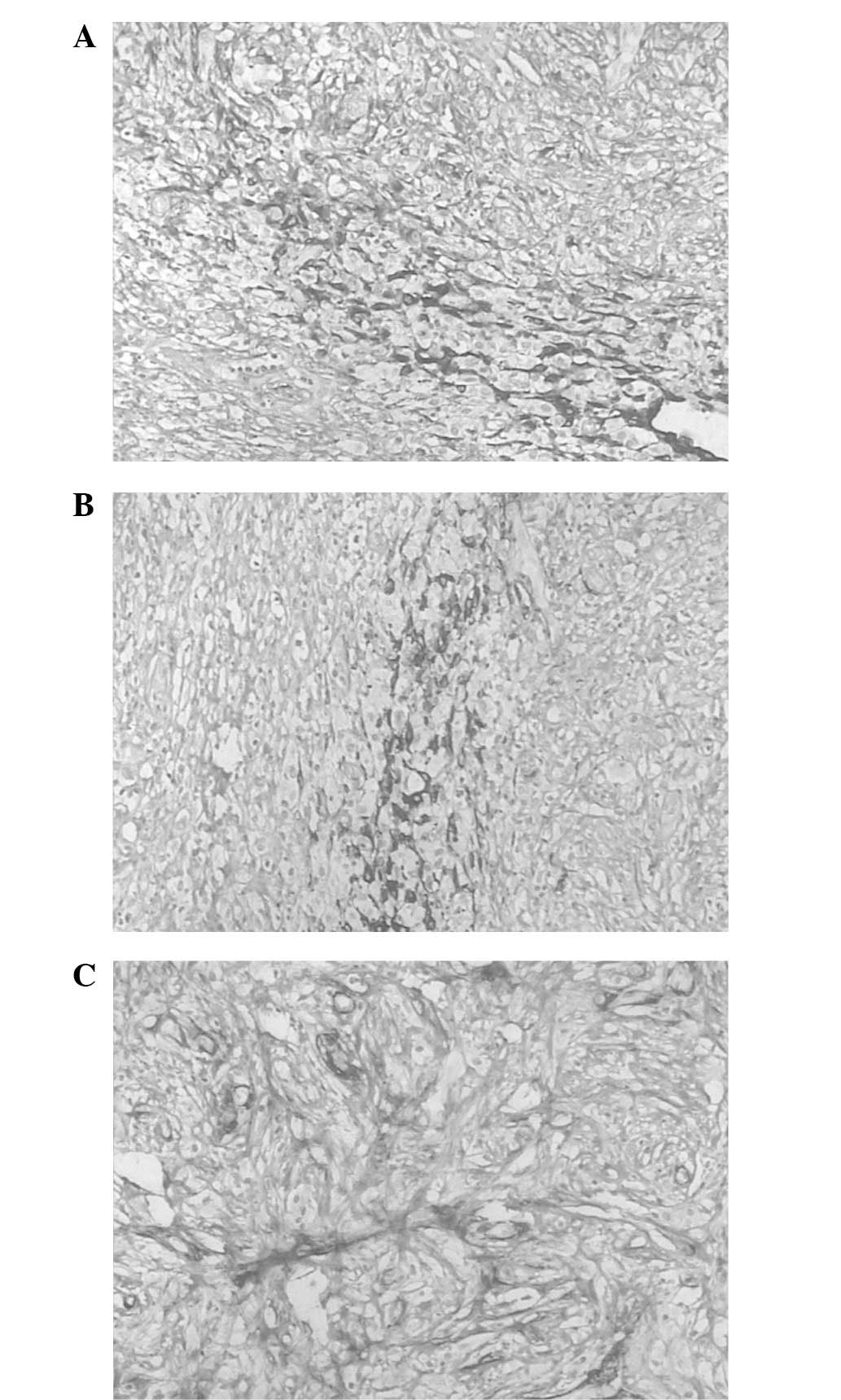
Immunohistochemical analysis showed that the tumor cells were
positive for cytokeratin (CK; Fig.
3A), CAM5.2 (Fig. 3B), smooth
muscle actin (SMA; Fig. 3C), CK19,
calretinin (CR) and CD34. The markers for CEA, bcl-2, placental
alkaline phosphatase (PLAP), CD117, S-100, CD20, CD79a, CD45RO,
CD15 and CD30 were negative. Focal tumor necrotic foci and mitoses
were also observed (identified in 1–2 of the 10 high-power fields
examined). Based on these findings, the tumor was diagnosed as a
malignant mesothelioma arising from the mediastinal mesothelial
cells. The patient received pemetrexed (500 mg/m2) and
cisplatin (75 mg/m2) combination chemotherapy for four
cycles (administered on the first day of the cycle, 21 days for
each cycle). At present, the patient, showing no symptoms, is
undergoing follow-up.
Discussion
Pleural mesotheliomas, which usually originate from
the mesothelial cells of the pleura and peritoneum, were once rare
(3). However, at present, the
incidence of this type tumor is increasing worldwide (4). The two types of mesothelioma are
localized and diffuse, with the majority of the former being benign
and the latter being malignant. The majority of malignant
mesotheliomas occur in adults, with few observed in children
(5). Malignant mesotheliomas appear
in ∼60% of cases in the pleura and ∼35% of cases in the peritoneum,
with sporadic cases arising in the mediastinum (6). The pathogenesis of the disease remains
unclear, and the role of asbestos exposure in the development of
malignant mesothelioma cannot be defined as the information with
regard to asbestos exposure is not available for the majority of
cases (7). The present case had no
history of asbestos exposure.
Malignant mediastinal mesotheliomas are uncommon and
are generally considered to arise from the mesothelial cells of the
pericardium; the majority of cases have been reported as
‘pericardial mesothelioma’ (1). The
largest series of these cases demonstrated that chest pain,
dyspnea, coughing or a combination of all these were the initial
symptoms of malignant pleural mesotheliomas, which accounted for
90% of all cases (8). Compared to
previous studies, in which the majority of cases had a large
quantity of pleural effusion, the present study case had only a
small amount of light yellow pleural effusion, without pericardial
effusion. This indicates that the present case may have no clear
association with the pericardium and that the pathogenesis of the
disease may have originated from the mesothelial cells of the
mediastinal pleura. Malignant pleural mesotheliomas usually develop
diffusely along the parietal and visceral pleura. In the present
case, the tumor formed a mass in the upper mediastinum, the vessels
in the mediastinum were compressed and shifted to the lower right
and the trachea became stenotic, without mucosal invasion. In
contrast to diffuse mesothelioma, localized malignant mesothelioma
is considered to be a distinct rare variant of malignant
mesothelioma (1). Mesothelioma has
a propensity to spread within tissue planes; this aspect may
explain the clinical presentation and tumor growth of the present
case. Only a few case reports of localized mesothelioma in the
mediastinum are found upon review of the English-language
literature (9–12).
In contrast to diffuse mesothelioma, the majority of
forms of localized pleural mesothelioma have been reported to be
benign, although the malignant potential of localized mesothelioma
remains unclear due to its rarity. Allen et al (7) reviewed cases of localized malignant
mesothelioma and proposed that it should be a separate entity from
diffuse malignant mesothelioma, due to its superior prognosis and
localized presentation in comparison with diffuse mesothelioma.
At present, three types of pathological cell have
been reported in malignant mesothelioma: epithelial,
fibrosarcomatous and mixed-type. The majority of reported cases
have been of the epithelial type. Immunohistochemical examination
is useful in the differential diagnosis and classification of
mesothelioma. The European Society of Thoracic Surgeons recommended
that mesothelioma be diagnosed by a panel and including a
combination of immunohistochemical positive and negative markers;
tumor cells in malignant mesothelioma have been reported to be
positive for calretinin, vimentim, keratin and epithelial membrane
antigen (EMA), while the markers for adenocarcinoma, CEA and
thyroid transcription factor 1 (TTF-1) were negative (13). Calretinin is the most sensitive of
the positive mesothelial markers. However, the choice of a
mesothelioma antibody panel remains controversial (14). The tumor cells in the present case
were positive for CK, CAM5.2, SMA, CK19, CR and CD34, while the
markers for bcl-2, PLAP, CD117, S-100, CD20, CD79a, CD45RO, CD15,
CD30 were negative.
In the present study, the patient’s mass was
initially considered to be a metastatic tumor, although no primary
lesions were detected and the mass did not have the typical imaging
characteristics of lymphoma. The mass was finally demonstrated to
be a primary mediastinal tumor. The differential diagnosis of
localized mesothelioma includes lymphoma and thymic carcinoma.
However, the imaging and clinical findings are generally unhelpful
in the differential diagnosis and tumors may only be differentiated
by histopathological and immunohistochemical examinations (1).
There has been significant progress in the treatment
of malignant mesothelioma, although it remains extremely difficult
to treat. Pemetrexed in combination with cisplatin has been
approved as a chemotherapy regimen for the treatment of malignant
mesothelioma in America and Europe (15). This regimen has been shown to
prolong the survival time of patients and improve their quality of
life. However, its effectiveness in the treatment of localized
mesothelioma remains controversial (16). Despite wide resection of the border
in cases of localized mesothelioma, metastasis or the local
recurrence of malignant mesothelioma occurs frequently and the
resultant prognosis is poor.
The tumor in the present study was finally diagnosed
as a malignant mesothelioma occurring in the mediastinum. To the
best of our knowledge, only a few cases have been reported in the
English-language literature. This type of mesothelioma is extremely
difficult to treat at an advanced stage, even if patients receive
comprehensive treatment. In addition, it is difficult to reach a
final diagnosis at the early stages.
References
|
1.
|
Erdogan E, Demirkazik FB, Gulsun M,
Ariyurek M, Emri S and Sak SD: Incidental localized (solitary)
mediastinal malignant mesothelioma. Br J Radiol. 78:858–861. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Cardinale L, Cortese G, Familiari U, Perna
M, Solitro F and Fava C: Fibrous tumour of the pleura (SFTP): a
proteiform disease. Clinical, histological and atypical
radiological patterns selected among our cases. Radiol Med.
114:204–215. 2009. View Article : Google Scholar
|
|
3.
|
Boutin C and Rey F: Thoracoscopy in
pleural malignant mesothelioma: a prospective study of 188
consecutive patients. Part 1: diagnosis. Cancer. 72:389–393. 1993.
View Article : Google Scholar
|
|
4.
|
Robinson BWS and Lake RA: Advances in
malignant mesothelioma. N Engl J Med. 353:1591–1603. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Lee YC, Thompson RI, Dean A and Robinson
BWS: Clinical and palliative care aspects of malignant
mesothelioma. Mesothelioma. Robinson BWS and Chahinian AP: Martin
Dunitz; London: pp. 111–126. 2002
|
|
6.
|
Antman KH: Current concepts: malignant
mesothelioma. N Engl J Med. 303:200–202. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Allen TC, Cagle PT, Churg AM, et al:
Localized malignant mesothelioma. Am J Surg Pathol. 29:866–873.
2005. View Article : Google Scholar
|
|
8.
|
Ruffie P, Feld R, Minkin S, et al: Diffuse
malignant mesothelioma of the pleura in Ontario and Quebec: a
retrospective study of 332 patients. J Clin Oncol. 7:1157–1168.
1989.PubMed/NCBI
|
|
9.
|
Shimazaki H, Aida S, Iizuka Y, Yoshizu H
and Tamai S: Vacuolated cell mesothelioma of the pericardium
resembling liposarcoma: a case report. Hum Pathol. 31:767–770.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Val-Bernal JF, Figols J and Gómez-Román
JJ: Incidental localized (solitary) epithelial mesothelioma of the
pericardium: case report and literature review. Cardiovasc Pathol.
11:181–185. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Bierhoff E and Pfeifer U: Malignant
mesothelioma arising from a benign mediastinal mesothelial cyst.
Gen Diagn Pathol. 142:59–62. 1996.PubMed/NCBI
|
|
12.
|
Sane AC and Roggli VL: Curative resection
of a well-differentiated papillary mesothelioma of the pericardium.
Arch Pathol Lab Med. 119:266–267. 1995.PubMed/NCBI
|
|
13.
|
Scherpereel A, Astoul P, Baas P, et al
European Respiratory Society/European Society of Thoracic Surgeons
Task Force: Guidelines of the European Respiratory Society and the
European Society of Thoracic Surgeons for the management of
malignant pleural mesothelioma. Eur Respir J. 35:479–495. 2010.
View Article : Google Scholar
|
|
14.
|
Amatya VJ, Takeshima Y, Aoe K, et al: CD9
expression as a favorable prognostic marker for patients with
malignant mesothelioma. Oncol Rep. 29:21–28. 2013.PubMed/NCBI
|
|
15.
|
Zucali PA and Giaccone G: Biology and
management of malignant pleural mesothelioma. Eur J Cancer.
42:2706–2714. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Kitazono-Saitoh M, Takiguchi Y, Kitazono
S, et al: Interaction and cross-resistance of cisplatin and
pemetrexedin in malignant pleural mesothelioma cell lines. Oncol
Rep. 28:33–40. 2012.PubMed/NCBI
|