Introduction
Mature cystic teratomas (MCTs) are germ cell tumors
that commonly occur in the ovaries, accounting for 10% of all
ovarian tumors (1). Ovarian MCTs
are usually located in the uterine adnexa and pouch of Douglas,
where the tumors arise from the nervous system (i.e. chordoma and
schwannoma) or from the intestinal tract (i.e. colorectal carcinoma
and mesenchymoma) in the presacral region. Teratomas, particularly
ovarian MCTs, rarely occur at presacral locations (2). Transsacral surgery is a routine
procedure for presacral tumor management. The current study
presents an extremely rare case of transsacral abdominal ovarian
MCT and describes the surgical removal of this tumor.
Case report
Clinical presentation and diagnosis
A 24-year-old Mongolian female was referred to the
outpatient clinic at Huashan Hospital (Shanghai, China) with mild
sacrococcygeal pain that had been present for two months with no
obvious causation. The individual had no fever, abdominal pain or
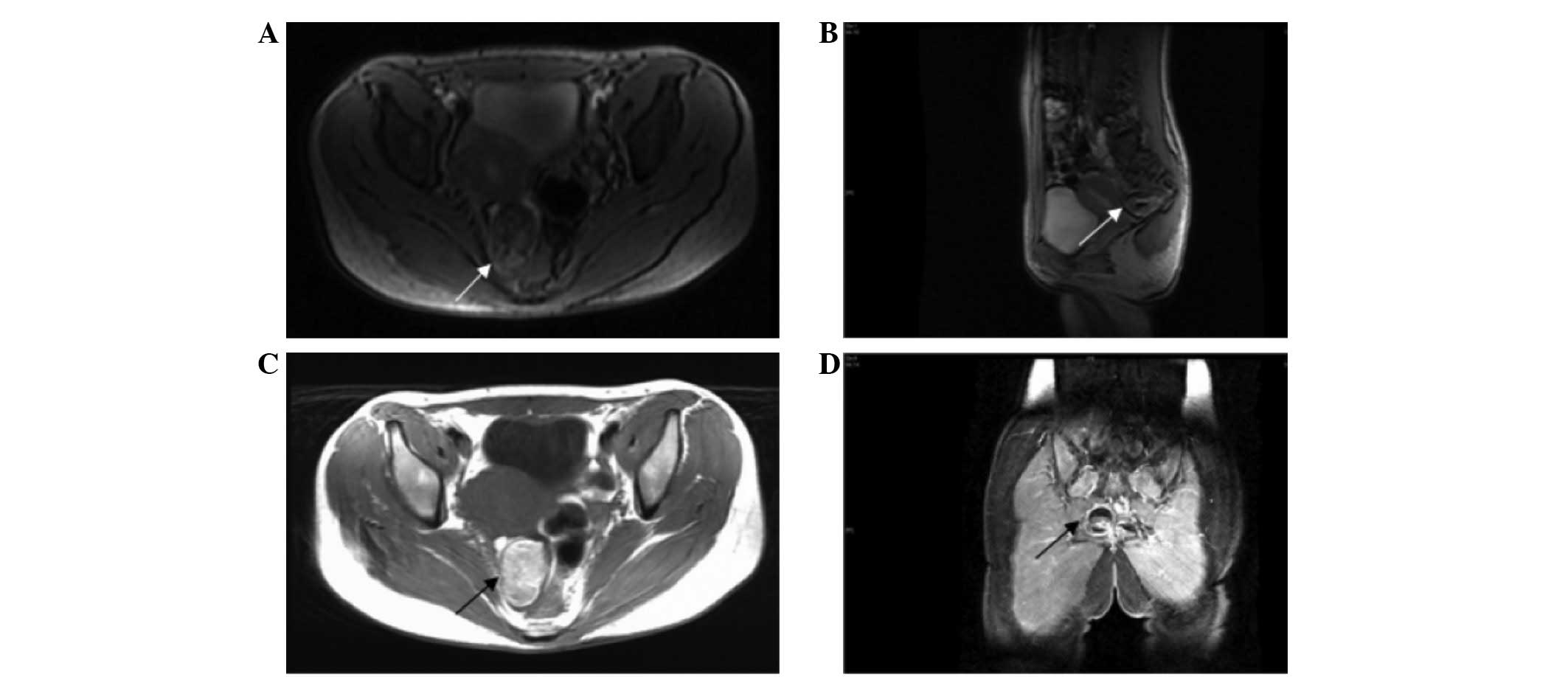
changes in habitual normal bowel movement and urination. Magnetic
resonance imaging (MRI) of the patient’s pelvis revealed a
53×40×33-mm pelvic mass, posterior to the sacrum and at the right
side of the rectum (Fig. 1). An
enhanced MRI showed that the mass, a possible teratoma, was under
the sacrum (Fig. 2). Based on the
radiological features, the mass was located at the posterior of the
rectum towards the right side and was extended near the sacrum with
clear boundaries without evidence of sacral invasion. A laboratory
examination of the tumor section, including an analysis for tumor
markers CA 19-9 and CA 125, revealed results within the normal
ranges. The patient’s medical history included a coccyx fracture in
2002 and a sacral epidermal cystectomy in 2004.
Upon admission to the hospital, no abdominal
tenderness, rebound pain or palpable masses were identified by a
physical examination. The initial rectal exam detected the inferior
end of a non-mobile, non-tender and smooth-edged mass attached to
the right posterior side of the rectum.
Surgical procedure
The patient was scheduled for surgical treatment
under general anesthesia two days after admission.
Intraoperatively, the patient was placed in the prone jack-knife
position. The surgery was performed with a 10-cm incision at the
inferior margin of the fifth sacrum. The coccyx and the inferior
margin of the fifth sacrum were removed. The right side of the wall
of the rectum was dissociated from the presacral rectum by an
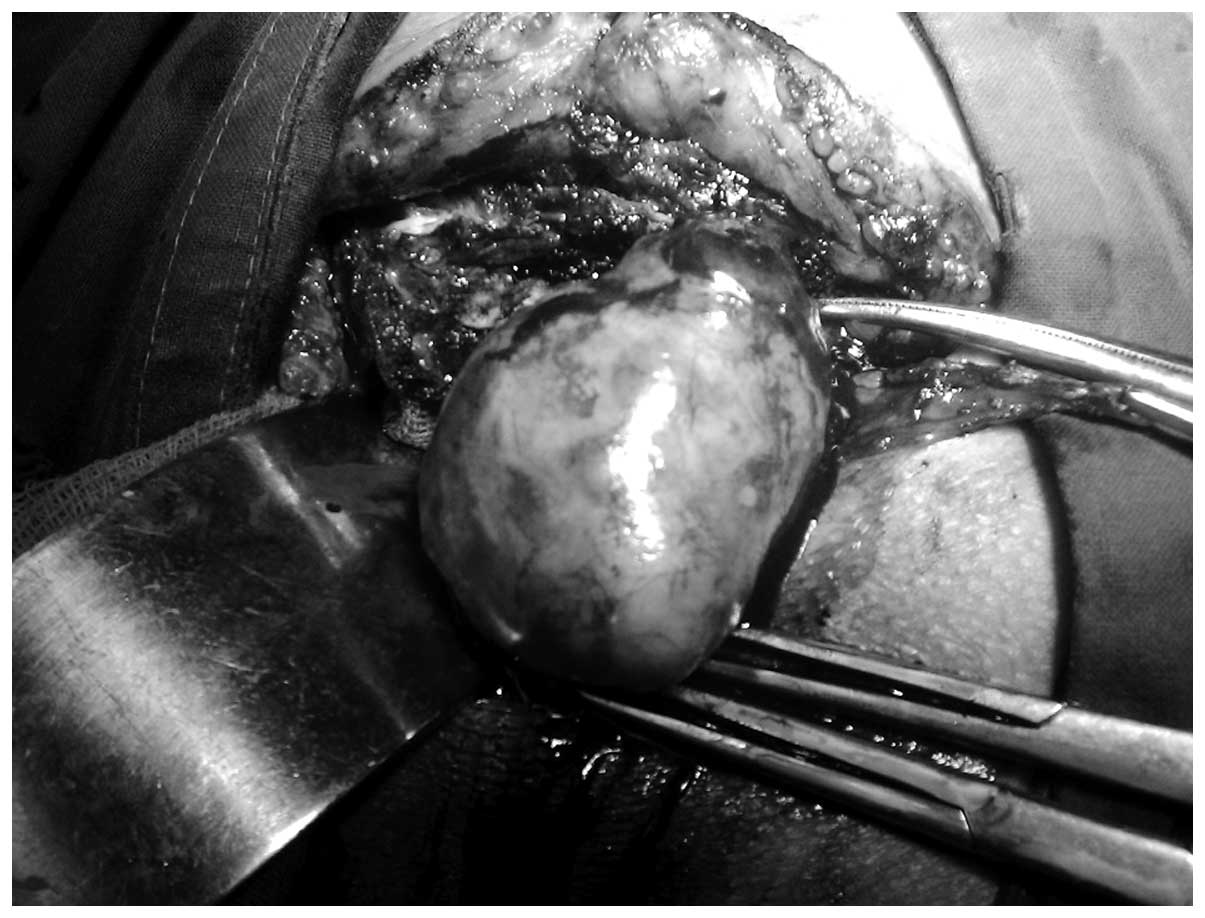
incision into the gorge of the sacrum. No tumor mass was located by
laparotomy or the initial examination during surgery. Next, an
ultrasound examination was performed and the mass was visualized at
the right side of rectum, posterior to the uterus. The right ovary
was not located at its normal anatomical site. The peritoneum was
opened and the enlarged right ovary was identified as a presacral
mass with an irregular appearance. The mass had a diameter of 5 cm
and its outer boundary was smooth with no feeding vessel or
ligamentous connection to the surrounding organs, including the
rectum, uterus, cervix and vagina. The sacrum and coccyx were
unaffected (Fig. 3). The left ovary
was normal in appearance and located at its usual anatomical
site.
The right ovary tumor mass was resected and removed
from the normal ovarian tissue by a gynecologist. The examination
of an intraoperative frozen section indicated a possible diagnosis
of a presacral MCT (dermoid cyst). A further pathological
examination confirmed the diagnosis of a presacral MCT. The patient
recovered uneventfully and was discharged 6 days after the surgery.
Written informed consent was obtained from the patient for the
publication of this case report.
Discussion
Teratomas arise mainly from totipotential gonadal
cells, and while a number of them may have malignant potential, the
majority are benign at the time of identification. The cause of
teratomas remains unknown (3).
These masses are encapsulated tumors with components that resemble
normal derivatives of all three germ layers and they appear
completely different to the normal tissue in which they are
embedded. Teratomas represent 10–15% of the total number of
recorded ovarian tumors and are commonly found in young patients
(4). MCTs are the most common type
of teratoma, accounting for the majority of germ cell tumors. These
tumors generally develop as a single mass away from the midline
(5). The symptoms of teratomas vary
between individuals, but these tumors are mainly identified as a
result of organ occupation and compression by the mass. Presacral
masses arise from the nervous system or intestinal tract. In
contrast to the current case report, primary presacral MCTs are one
of the most common types of tumor to be found in infants and are
rarely reported in adults (6).
Primary presacral MCTs occur more frequently in females, and the
female-to-male ratio is 10:1 (7).
An accurate diagnosis of a presacral mass prior to
surgical removal is extremely important. A number of standard
diagnostic imaging methods, including ultrasonography (transvaginal
and transrectal), computed tomography (CT) and MRI, are readily
available and must be used to generate a detailed image of the mass
to facilitate pre-operative planning (8,9).
Although presacral ovarian MCTs are extremely rare, to avoid any
diagnostic dilemma, a gynecological ultrasound examination via the
vagina and/or rectum is an important routine examination.
Sonographically, an MCT may present predominantly as a cyst,
containing a solid or complex tumor mass (10). Gynecological ultrasound examinations
are able to reveal the anatomical location of the tumor and its
relationship to the adnexa uteri. This technique is the most
commonly employed imaging method for the assessment of pathological
conditions associated with the adnexa uteri. Regardless of whether
transsacral or transabdominal surgery is performed, an ultrasound
may be useful for monitoring and adjusting the surgical
approach.
Radiological visualization techniques, including CT
and MRI, enable us to generate a pre-operative diagnosis for
presacral tumors (11,12). CT scans are useful for determining
the size and density of the lesion and its spatial relations,
however, they lack the specificity to differentiate the types of
presacral tumors (13). MCTs
typically show various CT-based attenuations. The considerably
variable MRI signal intensities generated by the various tissue
contents of the mass within the cystic lesion, including fat and
bone, are characteristic of MCTs. MRI has also been used to
evaluate presacral tumors and is known to be able to define the
type of tumor as well as visualize and screen for meningeal and
bone invasion (14).
In the current patient, MRI showed the fat-like and
soft tissue components within the presacral mass. Since a diagnosis
of a primary presacral MCT could not be ruled out, particularly due
to the patient’s medical history and physical examination results,
the transsacral approach was selected for the surgery.
Surgical resection is the standard curative
treatment for the majority of MCTs. For patients who are otherwise
healthy and whose lesions appear resectable, the management of such
lesions is almost always surgical resection. The approach depends
on the nature and location of the lesion. Previous studies have
reported that lesions which do not extend below S4 should be
resected transabdominally, while lesions below S4 and <8 cm in
diameter should be resected transsacrally and larger lesions or
those in an intermediate position may require a combined abdominal
and sacral surgical procedure (15,16).
According to the MRI results in the present study, the lesion of
the patient was >5 cm in diameter and below S5. Therefore, the
transsacral approach was selected to access and remove the
tumor.
The final diagnosis for this patient was a
transsacral ovarian MCT in the presacral region. Ovarian MCTs
mostly occur in the pelvic cavity and are commonly observed in the
pouch of Douglas and occasionally in the uterosacral ligament
(17). In rare cases, masses have
been identified in the presacral region (18,19).
The location of a mass in the presacral region is likely to be due
to gravitational effects on the relatively large mass size, the
heterogeneous content of the mass that enables it to be squeezed
and reshaped along with the surroundings during exogenic movements
or compressions and the presence of a smooth outer layer with
limited attachments, together with the heterotypic or displaced of
the ovary. In the current case, the MCT had a diameter of 5 cm and
exhibited heterogeneous density. The mass was tucked into the right
inferior of the sacrum, which may have been due to gravitational
pull and the compression force of bowel movements. Several
radiological examinations did show that the tumor was at this
location. We hypothesized that the supine position assumed during
the examination may have also contributed to such a result; the
mass was eventually located in the position it had descended to in
the presacral region. These effects contributed to the prediction
of the derivation and location of the tumor.
In addition, the most frequent symptom of MCT is
lower abdominal pain (20), while
the most common symptoms of patients with presacral masses are
suppuration and sacrococcygeal pain (21). The current patient reported symptoms
similar to those caused by a presacral mass, an additional
contribution to the misdiagnosis.
Performing a laparotomy with an uncertain target and
an unplanned surgical approach must be prevented to limit
surgery-related trauma and complications. During transsacral
surgery to remove a presacral mass, ultrasonography must be
performed if the mass cannot be located initially.
In the present case, no mass was located by the
laparotomy or initial examination during the surgery. An ultrasound
examination was performed, confirming that the mass was at the
right side of rectum, posterior to the uterus and embedded in the
predicted right ovary, which was not at its normal anatomical
location. Since the tumor was covered by normal smooth ovarian
tissue and had no adhesion to other organs and as the patient was
in the prone jack-knife position, the likelihood that the tumor may
have moved and descended into the abdominal cavity must be
considered.
We resected and dissociated the tumor mass from the
ovary through the sacral region and returned the ovary to the
normal anatomical location. The organs posterior to the bladder
were exposed in a clear view to avoid injuring the ureters. As MCTs
are curable in the majority of cases by a complete surgical
resection of the tumor alone (22),
and as the surgery is also sonographically monitored, operating
through the sacral region is likely to have no negative impact on
the outcome and prognosis of this case.
Ovarian MCTs commonly occur in the pelvic cavity and
are rarely identified in the presacral position. In cases where
ultrasound and radiological examinations strongly indicate the
presence of a teratoma, a diagnosis of a prescacral ovarian MCT
must be taken into consideration.
Pre-operative ultrasound and radiographic
examinations must be performed in the supine and prone positions to
assess the firmness and mobility of the presacral mass, as well as
its derivation and relationship to the surroundings. Based on these
efforts, the most efficient and least trauma-inflicting surgical
approach must be determined prior to surgery.
To dissect a transsacral abdominal mass, an
ultrasound examination must be performed during the surgery to
assist in the identification of the mass if it is not firmly
attached, movable or is not able to be located directly during
surgery initially. If the transsacral laparotomy fails to locate
the mass, an additional surgical procedure, such as a transparietal
laparotomy, should be performed. To assess a transsacral mass, it
is feasible that, during transsacral abdominal surgery, the
peritoneum is opened from the pelvic floor. By contrast, for a
common MCT that may be curatively managed by complete surgical
resection transabdomenally, the transsacral approach is unnecessary
and may be relatively more traumatic.
References
|
1
|
Peterson WF: Malignant degeneration of
benign cystic teratomas of the ovary; a collective review of the
literature. Obstet Gynecol Surv. 12:793–830. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Heller DS, Keohane M, Bessim S, Jagirdar J
and Deligdisch L: Pituitary-containing benign cystic teratoma
arising from the terosacral ligament. Arch Pathol Lab Med.
113:802–804. 1989.PubMed/NCBI
|
|
3
|
Jucá M, de Oliveira FF, Gomes EG and Le
Campion E: Sacrococcygeal teratoma in adult. Report of a case. Int
J Gastrointest Canc. 37:91–93. 2006.
|
|
4
|
Jeffcoate N: Jeffcoate’s Principles of
Gynaecology. Tindal VR: 5th edition. Butterworth-Heinemann Ltd;
Oxford: pp. 4661987
|
|
5
|
Krnojelac D, Hadzić B, Curcin N, Dolai M
and Bogdanović G: Malignant transformation of thyroid tissue in an
ovarian dermoid cyst: case report. Med Pregl. 52:395–398. 1999.(In
Croatian).
|
|
6
|
Moawad NS, Starks D and Ashby K: Ectopic
ovarian teratoma of the uterosacral ligament associated with a
large ovarian dermoid. J Minim Invasive Gynecol. 15:523–524. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Al-Essa AA, Malik TA, Baghdadi MK and El
Tayeb AA: Adult sacrococcygeal teratomas. Saudi Med J. 25:367–369.
2004.
|
|
8
|
Pidala MJ, Eisenstat TE, Rubin Rj and
Salvati EP: Presacral cysts: transrectal excision in select
patients. Am Surg. 65:112–115. 1999.PubMed/NCBI
|
|
9
|
Negro F, Mercuri M, Ricciardi V, et al:
Presacral epidermoid cyst: a case report. Ann Ital Chir. 77:75–77.
2005.
|
|
10
|
Saba L, Guerriero S, Sulcis R, Virgilio B,
Melis G and Mallarini G: Mature and immature ovarian teratomas: CT,
US and MR imaging characteristics. Eur J Radiol. 72:454–463. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Davidson AJ, Hartman DS and Goldman SM:
Mature teratoma of the retroperitoneum: radiologic, pathologic, and
clinical correlation. Radiology. 172:421–425. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pereira JM, Sirlin CB, Pinto PS and Casola
G: CT and MR imaging of extrahepatic fatty masses of the abdomen
and pelvis: techniques, diagnosis, differential diagnosis, and
pitfalls. Radiographics. 25:69–85. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang DM, Yoon MH, Kim HS, et al: Presacral
epidermoid cyst: imaging findings with histopathologic correlation.
Abdom Imaging. 26:79–82. 2001. View Article : Google Scholar
|
|
14
|
Riojas CM, Hahn CD and Johnson EK:
Presacral epidermoid cyst in a male: a case report and literature
review. J Surg Educ. 67:227–232. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bullard Dunn K: Retrorectal tumors. Surg
Clin North Am. 90:163–171. 2010.
|
|
16
|
Du F, Jin K, Hu X, Dong X and Cao F:
Surgical treatment of retrorectal tumors: a retrospective study of
a ten-year experience in three institutions.
Hepatogastroenterology. 59:1374–1377. 2012.PubMed/NCBI
|
|
17
|
Koo YJ, Im KS, Jung HJ and Kwon YS: Mature
cystic teratoma of the uterosacral ligament successfully treated
with laparoendoscopic single-site surgery. Taiwan J Obstet Gynecol.
51:86–88. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Afuwape OO, Ogundoyin OO, Ogunlana D and
Adeleye A: Adult sacrococcygeal teratoma: a case report. Ghana Med
J. 43:40–42. 2009.PubMed/NCBI
|
|
19
|
Monteiro M, Cunha TM, Catarino A and Tomé
V: Case report: sacrococcygeal teratoma with malignant
transformation in and adult female: CT and MRI findings. Br J
Radiol. 75:620–623. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Papadias K, Kairi-Vassilatou E,
Kontogiani-Katsaros K, Argeitis J, Kondis-Pafitis A and Greatsas G:
Teratomas of the ovary: a clinico-pathological evaluation of 87
patients from one institution during a 10-year period. Eur J
Gynaecol Oncol. 26:446–448. 2005.PubMed/NCBI
|
|
21
|
Canelles E, Roig JV, Cantos M, García
Armengol J, Barreiro E, Villalba FL, Ruiz MD and Pla V: Presacral
tumors. Analysis of 20 surgically treated patients. Cir Esp.
85:371–377. 2009.(In Spanish).
|
|
22
|
Luk SY, Tsang YP, Chan TS, Lee TF and
Leung KC: Sacrococcygeal geratoma in adults: case report and
literature review. Hong Kong Med J. 17:417–20. 2011.PubMed/NCBI
|