Introduction
With the development of computed tomogrphy (CT), an
increasing number of lung lesions are detected. It has been
reported that >50% of resected pulmonary nodular lesions are
related to malignancy; therefore, the requirement for rapid and
definite diagnoses of lung lesions has been stressed (1)CT-guided needle biopsy has become the
dominant method for obtaining tissue samples from lung lesions in
order to obtain a pathological diagnosis (2). The procedure is generally regarded as
safe, but pneumothorax, hemorrhage and other rare complications may
occur. In addition, the reliability of a benign result remains
controversial (3). The objective of
the current study was to determine the diagnostic accuracy of
CT-guided core needle biopsy (CNB) and to retrospectively analyze
the correlation between factors and complications of the
procedure.
Materials and methods
Study population
Between January 2009 and June 2010, a CNB was
performed on a total of 343 patients with 345 lung lesions in 345
sessions. Among them, two patients received a second CNB, as the
size of the tissue sample was not large enough to obtain
pathological results. These patients were then followed up for at
least two years. The enrolled population consisted of 228 males
(66.5%) and 115 females (33.5%). The patient age ranged between 17
and 86 years old (mean age, 60±18.3 years old). The study was
approved by the ethics committee of Fudan University (Shanghai,
China).
Procedure
Prior to the procedure, the risks and benefits were
explained to each patient and informed consent was obtained. Three
interventional physicians, each with >5 years experience of
needle biopsies, performed the procedures. All cases were performed
using the Philips 64-slice spiral CT (120 kV, 250 mA and a 3-mm
thickness; Philips Healthcare, Andover, MA, USA) for imaging
guidance. The biopsy tool that was used was an automated biopsy gun
(SuperCore™, Angiotech Pharmaceuticals, Inc., Vancouver, BC,
Canada) with an 18-gauge needle. The patient lay on the CT table
and the puncture point and access routine were determined by CT
scan. Following local anesthesia, the needle was inserted through
the skin and advanced to the lesion. Intra-operative CT scans were
performed to confirm the position of the lesion and needle. Once
the needle was located in an appropriate position within or near
the lesion, the operator triggered the cannula to close, trapping
the specimen in the sample notch. Next, the tissue specimen was
removed from the notch and sent to the Department of Pathology
(Fudan University, Shanghai, China). Immediately after the
procedure, a chest CT scan was performed to evaluate procedural
complications, including pneumothorax and hemorrhage. In addition,
a chest radiograph was obtained the following morning. The baseline
characteristics of the lesions and procedures are summarized in
Table I.
 | Table ICharacteristics of lesions and
procedures. |
Table I
Characteristics of lesions and
procedures.
| Characteristic | n (range) |
|---|
| Maximal diameter,
mm | 41.4 (8–134) |
| Lesion location |
| Lobe |
| Upper | 178 |
| Middle | 28 |
| Lower | 139 |
| Zone |
| Outer | 54 |
| Middle | 114 |
| Inner | 177 |
| Patient position |
| Supine | 106 |
| Prone | 192 |
| Decubitus | 45 |
| Frequency of needle
adjustments | 1.6 (1–7) |
| Distance from skin
puncture to needle tip, mm | 73.0 (4.8–139.6) |
| Distance from pleural
puncture to needle tip, mm | 34.4 (8.9–87.8) |
| Length of needle
through normal parenchyma, mm | 14.8 (0.0–59.7) |
Classification of diagnoses and
complications
The CNB results were divided into 4 categories:
Atypical adenomatous hyperplasia (AAH), malignant, benign and
undetermined (3). AAH is a
premalignant lesion of lung adenocarcinoma. Although AAH is not
ranked as malignant, this category commonly undergoes carcinomatous
change.
Final diagnoses were divided into 3 categories:
Malignant, benign and undetermined. Malignant tumors were defined
by: i) Cancer-associated mortality occurring during the follow-up
period; ii) lesions representing complete response, partial
response or progressive disease to chemotherapy according to the
Response Evaluation Criteria in Solid Tumors (4); and iii) a histopathological
examination showing malignant tumor tissue in the specimen received
at surgical resection. Benign tumors were defined by: i) Lesions
that disappeared or decreased in size with conservative treatment;
ii) patient exhibited a positive microbiological conclusion
(3,5); or iii) a histopathological examination
showing no malignant tumor tissue in the specimen from surgical
resection. Undetermined tumors were defined as: i) Lesions treated
by radiofrequency ablation or stereotactic irradiation (6); ii) a lesion that was stable in size at
follow-up; or iii) a patient that could not be contacted for
follow-up (Table II).
 | Table IICNB and final diagnosis. |
Table II
CNB and final diagnosis.
| Final diagnosis |
|---|
|
|
|---|
| CNB diagnosis | Benign | Malignant | Undetermined |
|---|
| Benign | 50 | 7 | 9 |
| AAH | 0 | 3 | 0 |
| Malignant | 0 | 250 | 6 |
| Undetermined | 2 | 7 | 11 |
AAH and malignant were considered to be positive
results and benign was considered a negative result. Positive CNB
results were considered true positives if the final diagnosis was
malignant or AAH. By contrast, results were considered false
positives if the final diagnosis was benign. Negative CNB results
were considered true negatives if the final diagnosis was benign
and false negatives if the final diagnosis was malignant or AAH
(Table III).
 | Table IIIPositive and negative diagnosis. |
Table III
Positive and negative diagnosis.
| Final diagnosis |
|---|
|
|
|---|
| CNB diagnoses | Positive | Negative | Total |
|---|
| Positive | 253 | 0 | 253 |
| Negative | 7 | 50 | 57 |
| Total | 260 | 50 | 310 |
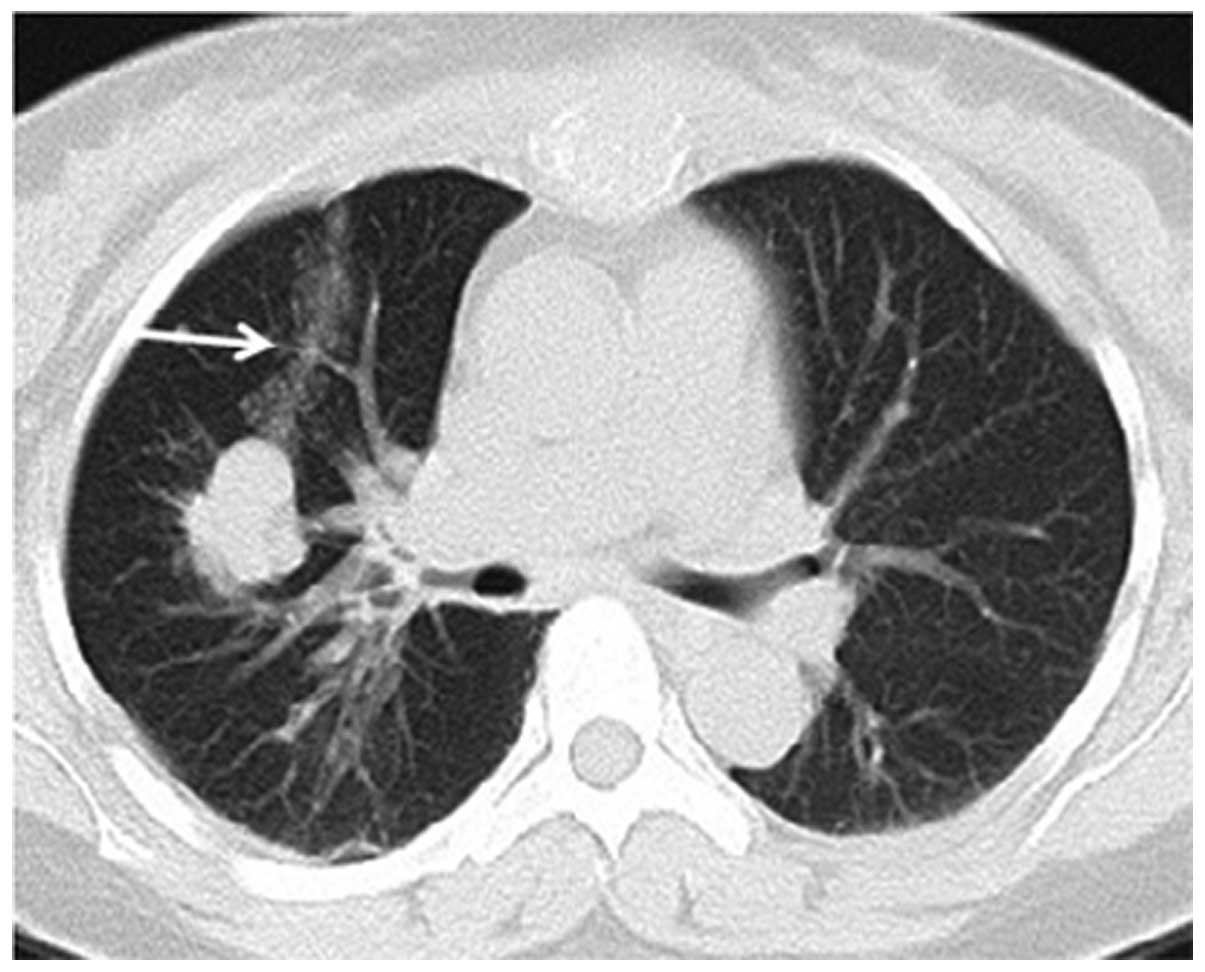
Pneumothorax was graded as mild (lung surface
retraction of ≤2 cm; Fig. 1),
moderate (lung surface retraction of 2–4 cm) and severe (lung
surface retraction of ≥4 cm) (7).
Hemorrhage was graded as mild (presenting as haziness along the
needle tract; Fig. 2), moderate
(hemoptysis of <30 ml or occurrence of patchy haziness around
the lesion in CT; Fig. 3) and
severe (hemoptysis of ≥30 ml or hemothorax).
Statistical analysis
Data were analyzed with SPSS 19.0; the χ2
test was used for the statistical analysis. The analysis of
pneumothorax and hemorrhage was based on the 345 CNB sessions not
the 343 patients. P<0.05 was considered to indicate a
statistically significant difference.
Results
CNB diagnoses included 66 benign cases, 3 AAH cases,
256 malignant cases and 20 undetermined cases; final diagnoses
consisted of 52 benign cases, 267 malignant cases and 26
undetermined cases. Final diagnoses were obtained based on the
following characteristics: 11 (3.2%) patients succumbed to
cancer-associated mortalities; 64 (18.7%) surgical specimens, 12
(3.5%) positive cultures; 193 (56.2%) positive responses to
chemotherapy; 37 (10.8%) tumors disappeared or decreased in size
with conservative treatment; 8 (2.3%) lesions were treated with
radiofrequency ablation (n=2) or stereotactic irradiation (n=6); 5
(1.5%) lesions were stable during the follow-up period; and 13
(3.8%) patients could not be contacted for follow-up. Following
exclusion of the undetermined CNB and final diagnoses (n=35)
(8), the number of true positives,
false positives, true negatives and false negatives were 253, 0, 50
and 7, respectively. The sensitivity, specificity, accuracy,
positive predictive value (PPV) and negative predictive value (NPV)
were 97.3, 100, 97.7, 100 and 87.7%, respectively.
In the present study, the overall complication rate
was 50.4%. There was a total of 60 (17.5%) cases of pneumothorax in
the 343 patients. Among those, 52 (15.2%) were mild, 6 (1.7%) were
moderate and 2 (0.6%) were severe. Only 5 (1.5%) required placement
of chest tubes. There were 113 (32.9%) cases of hemorrhage in this
study. Of those, 78 (22.7%) were mild hemorrhage, 35 (10.2%) were
moderate hemorrhage. No severe hemorrhage occurred. One of the
patients with moderate hemorrhage complained of chest pain and
chest tightness 8 h after the biopsy; the chest radiograph
indicated a parenchymal hemorrhage and hemocoagulase was
administrated. Another patient developed hypotension with syncope,
and resuscitation and hemocoagulase administration improved the
individual’s condition. All other hemorrhages were
self-limited.
The correlation between factors and complications
was determined, and a statistically significant correlation was
found between pneumothorax and the factors of smoking and the
position and length of the needle in the normal parenchyma
(P=0.011). In addition, a statistically significant correlation
existed between hemorrhage and the maximal diameter (P=0.005) and
length of the needle in the normal parenchyma (P<0.01) and the
frequency of needle adjustments (P<0.01). The correlations
between factors and complications are shown in Tables IV and V.
 | Table IVCorrelation between factors and
pneumothorax. |
Table IV
Correlation between factors and
pneumothorax.
| Characteristic | Pneumothorax, n | Non-pneumothorax,
n | P-value |
|---|
| Gender | | | 0.956 |
| Male | 40 | 189 | |
| Female | 21 | 95 | |
| Age, years | | | 0.986 |
| 17–49 | 12 | 58 | |
| 50–69 | 34 | 146 | |
| 70–86 | 15 | 80 | |
| Smoking status | | | 0.015a |
| Non-smoker | 17 | 44 | |
| Current or
ex-smoker | 20 | 126 | |
| Unknown | 24 | 114 | |
| Patient position | | | 0.000a |
| Supine | 16 | 89 | |
| Prone | 25 | 170 | |
| Decubitus | 20 | 25 | |
| Lesion location | | | |
| Lobe | | | 0.568 |
| Upper | 29 | 158 | |
| Middle | 5 | 25 | |
| Lower | 27 | 101 | |
| Zone | | | 0.115 |
| Outer | 14 | 41 | |
| Middle | 24 | 86 | |
| Inner | 23 | 157 | |
| Effusion | | | 0.181 |
| No | 56 | 246 | |
| Yes | 5 | 38 | |
| Maximal diameter,
cm | | | 0.605 |
| ≤1 | 2 | 4 | |
| 1–3 | 22 | 89 | |
| 3–5 | 26 | 107 | |
| >5 | 11 | 84 | |
| Length of needle
through normal parenchyma, mm | | | 0.011a |
| <1 | 14 | 124 | |
| 1–3 | 31 | 102 | |
| ≥3 | 16 | 58 | |
| Needle-hilus angle,
° | | | 0.156 |
| 0–30 | 22 | 95 | |
| 30–60 | 32 | 125 | |
| 60–90 | 7 | 63 | |
| Needle
adjustments | | | 0.285 |
| 1 | 38 | 176 | |
| 2–3 | 14 | 83 | |
| ≥4 | 9 | 25 | |
| Operator/s | | | 0.210 |
| 1 | 34 | 136 | |
| 2 | 15 | 60 | |
| 3 | 12 | 88 | |
 | Table VCorrelation between factors and
hemorrhage. |
Table V
Correlation between factors and
hemorrhage.
| Characteristic | Hemorrhage, n | Non-hemorrhage,
n | P-value |
|---|
| Gender | | | 0.747 |
| Male | 75 | 154 | |
| Female | 40 | 76 | |
| Age, years | | | 0.455 |
| 17–49 | 27 | 43 | |
| 50–69 | 55 | 125 | |
| 70–86 | 33 | 62 | |
| Smoking status | | | 0.697 |
| Non-smoker | 20 | 41 | |
| Current or
ex-smoker | 52 | 94 | |
| Unknown | 43 | 95 | |
| Patient
position | | | 0.211 |
| Supine | 32 | 73 | |
| Prone | 72 | 123 | |
| Decubitus | 11 | 34 | |
| Lesion
location |
| Lobe | | | 0.466 |
| Upper | 65 | 122 | |
| Middle | 7 | 23 | |
| Lower | 43 | 85 | |
| Zone | | | 0.336 |
| Outer | 14 | 41 | |
| Middle | 36 | 74 | |
| Inner | 65 | 115 | |
| Effusion | | | 0.134 |
| No | 10 | 33 | |
| Yes | 105 | 197 | |
| Maximal diameter,
cm | | | 0.005a |
| ≤1 | 5 | 1 | |
| 1–3 | 43 | 68 | |
| 3–5 | 45 | 88 | |
| >5 | 22 | 73 | |
| Length of needle
through normal parenchyma, mm | | | 0.000a |
| <1 | 18 | 120 | |
| 1–3 | 49 | 84 | |
| ≥3 | 48 | 26 | |
| Needle-hilus angle,
° | | | 0.465 |
| 0–30 | 36 | 81 | |
| 30–60 | 55 | 102 | |
| 60–90 | 23 | 47 | |
| Needle
adjustments | | | 0.000a |
| 1 | 53 | 161 | |
| 2–3 | 48 | 59 | |
| ≥4 | 14 | 20 | |
| Operator/s | | | 0.797 |
| 1 | 55 | 115 | |
| 2 | 24 | 51 | |
| 3 | 36 | 64 | |
Discussion
In the present study, the incidence of pneumothorax
was 17.5%, with 1.5% requiring chest tube drainage. These results
are comparable to prior studies (9–11). The
decubitus position was found to result in more pneumothoraxes than
the supine and prone positions. We hypothesize that the decubitus
position separates the parietal and visceral pleura more than the
other positions and therefore, air is more likely to enter the
pleural cavity as the needle is taken out. Moreover, the majority
of lung lesions were found to be located in the middle or inner
zone of the lung in the present study. In the biopsy of lesions
located in the middle or inner zone of the lung, it is more
difficult to keep away from the interlobar pleural; if it is
damged, it is more likely to result in pneumothorax. O’Neill et
al(12) reported that rapidly
(within 10 sec) rolling the patient over to the biopsy-side-down
position following needle-out reduced the rate of overall
pneumothorax and pneumothorax necessitating a drainage catheter.
Moreover, smoking, the decubitus position and a longer length
needle in the normal parenchyma were risk factors for a
pneumothorax. It is generally considered that a pneumothorax is the
most common complication of a needle biopsy of the lung (11,13).
However, in the present study, the incidence of hemorrhage (32.9%)
was higher than pneumothorax (17.5%) and also higher than the 1–27%
reported in the literature (7,11,14).
This may be since a pneumothorax is easier to identify in chest
radiographs and its obvious symptoms are apt to attract notice. By
contrast, mild hemorrhage is difficult to identify in chest
radiographs. Furthermore, the current data was based on the
presence of haziness on CT images and hemoptysis, instead of
hemoptysis only. The results showed that a small diameter and
longer length of the needle in the normal parenchyma and more
frequent adjustments of the needle were poor predictive factors of
hemorrhage.
With regard to pathological yield, in the present
study, the false positive and false negative rates and the PPV and
NPV were 0, 2.7, 100 and 87.7%, respectively. When a malignant
diagnosis is identified by needle biopsy, the clinical
decision-making process is generally straightforward due to the
extremely low false-positive rates (0.0–1%) (3,15).
However, when a benign diagnosis is obtained, there is clinical
uncertainty over how to proceed, as a number of these lesions may
prove to be malignant (false negatives). Previous studies have
evaluated the outcomes following a benign biopsy and have found
false negative rates that vary widely (2–54%) (16–18).
Combining the results of the present and relevant previous studies,
we recommend that patients with benign CNB diagnoses undergo repeat
imaging for ≥2 years to document the stability or resolution of the
lesions. If the nodule grows, a repeat biopsy (19–21) or
resection (22) may be required to
obtain a definitive diagnosis.
The main limitations of the present study were as
follows: Firstly, in the analysis of the correlation between
factors and complications, single factors were considered
individually without excluding the affect of other factors.
Secondly, a small number of patients were lost for follow-up and a
two-year follow-up may not have been sufficient.
In conclusion, CT-guided core needle biopsy of the
lung lesions provides a high diagnostic yield. Smoking, the
decubitus position and a longer length of needle in the normal
parenchyma were risk factors for pneumothorax. In addition, small
diameter, a longer length of needle in the normal parenchyma and
more frequent adjustments of the needle were poor predictive
factors of hemorrhage.
Acknowledgements
This study was supported by grants from the Science
Technology Commission of Shanghai Municipality (nos. 0952nm03400
and 11nm0504000).
References
|
1
|
Shah PL, Singh S, Bower M, Livni N, Padley
S and Nicholson AG: The role of transbronchial fine needle
aspiration in an integrated care pathway for the assessment of
patients with suspected lung cancer. J Thorac Oncol. 1:324–327.
2006. View Article : Google Scholar
|
|
2
|
Zhou Y, Thiruvalluvan K, Krzeminski L, et
al: CT-guided robotic needle biopsy of lung nodules with
respiratory motion - experimental system and preliminary test. Int
J Med Robot. 9:317–330. 2013. View
Article : Google Scholar
|
|
3
|
Gelbman BD, Cham MD, Kim W, et al:
Radiographic and clinical characterization of false negative
results from CT-guided needle biopsies of lung nodules. J Thorac
Oncol. 7:815–820. 2012. View Article : Google Scholar
|
|
4
|
Padhani AR and Ollivier L: The RECIST
(Response Evaluation Criteria in Solid Tumors) criteria:
implications for diagnostic radiologists. Br J Radiol. 74:983–986.
2001. View Article : Google Scholar
|
|
5
|
Jae LI, June IH, Miyeon Y, et al:
Percutaneous core needle biopsy for small (≤10 mm) lung nodules:
accurate diagnosis and complication rates. Diagn Interv Radiol.
18:527–530. 2012.
|
|
6
|
Inoue D, Gobara H, Hiraki T, et al: CT
fluoroscopy-guided cutting needle biopsy of focal pure ground-glass
opacity lung lesions: diagnostic yield in 83 lesions. Eur J Radiol.
81:354–359. 2012. View Article : Google Scholar
|
|
7
|
Yildirim E, Kirbas I, Harman A, et al:
CT-guided cutting needle lung biopsy using modified coaxial
technique: factors effecting risk of complications. Eur J Radiol.
70:57–60. 2009. View Article : Google Scholar
|
|
8
|
Kim GR, Hur J, Lee SM, et al: CT
fluoroscopy - guided lung biopsy versus conventional CT-guided lung
biopsy: a prospective controlled study to assess radiation doses
and diagnostic performance. Eur Radiol. 21:232–239. 2011.
View Article : Google Scholar
|
|
9
|
Tomiyama N, Yasuhara Y, Nakajima Y, et al:
CT-guided needle biopsy of lung lesions: a survey of severe
complication based on 9783 biopsies in Japan. Eur J Radiol.
59:60–64. 2006. View Article : Google Scholar
|
|
10
|
Laurent F, Montaudon M, Latrabe V and
Bégueret H: Percutaneous biopsy in lung cancer. Eur J Radiol.
45:60–68. 2003. View Article : Google Scholar
|
|
11
|
Wu CC, Maher MM and Shepard JA:
Complications of CT-guided percutaneous needle biopsy of the chest:
prevention and management. AJR Am J Roentgenol. 196:W678–W682.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
O’Neill AC, McCarthy C, Ridge CA, et al:
Rapid needle-out patient-rollover time after percutaneous CT-guided
transthoracic biopsy of lung nodules: effect on pneumothorax rate.
Radiology. 262:314–319. 2012.
|
|
13
|
Wu RH, Tzeng WS, Lee WJ, et al: CT-guided
transthoracic cutting needle biopsy of intrathoracic lesions:
comparison between coaxial and single needle technique. Eur J
Radiol. 81:e712–e716. 2012. View Article : Google Scholar
|
|
14
|
Wiener RS, Schwartz LM, Woloshin S and
Welch HG: Population-based risk of complications following
transthoracic needle lung biopsy of a pulmonary nodule. Ann Intern
Med. 155:137–144. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Manhire A, Charig M, Clelland C, et al:
Guidelines for radio-logically guided lung biopsy. Thorax.
58:920–936. 2003. View Article : Google Scholar
|
|
16
|
Schreiber G and McCrory DC: Performance
characteristics of different modalities for diagnosis of suspected
lung cancer: summary of published evidence. Chest. 123(1 Suppl):
115S–128S. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Savage C, Walser EM, Schnadig V, et al:
Transthoracic image-guided biopsy of lung nodules: when is benign
really benign? J Vasc Interv Radiol. 15:161–164. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Anderson JM, Murchison J and Patel D:
CT-guided lung biopsy: factors influencing diagnostic yield and
complication rate. Clin Radiol. 58:791–797. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee YJ, Hwang Y, Kim TJ, et al:
Inconclusive result from CT guided transthoracic needle aspiration
and biopsy: affecting factors and final outcome. J Lung Cancer.
10:94–101. 2011. View Article : Google Scholar
|
|
20
|
Lee IJ, Bae YA, Kim DG, et al:
Percutaneous needle aspiration biopsy (PCNAB) of lung lesions: 5
years results with focusing on repeat PCNAB. Eur J Radiol.
73:551–554. 2010.
|
|
21
|
Khouri NF, Stitik FP, Erozan YS, et al:
Transthoracic needle aspiration biopsy of benign and malignant lung
lesions. AJR Am J Roentgenol. 144:281–288. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lee WT, Wang Y, He XH, et al: Combination
of CT-guided hookwire localization and video-assisted thoracoscopic
surgery for pulmonary nodular lesions: Analysis of 103 patients.
Oncology Letters. 4:824–828. 2012.
|