Introduction
Plasmacytoma is an extremely rare and discrete
solitary mass of neoplastic monoclonal plasma cells, which was
first described by Schridde in 1905 (1). Extramedullary plasmacytoma (EMP) has
been seldom reported and accounts for 4% of all non-epithelial
tumors of the upper respiratory tract (2). While occasionally localized to the
gastrointestinal tract, lungs, mammae, testes and skin, it has been
previously reported that 80% of EMPs are localized in the head and
neck region (3,4). Common clinical symptoms include
epistaxis, rhinorrhea, a sore throat, dysphonia and hemoptysis
(5,6). EMP is usually managed through
radiotherapy, with or without surgery. The current study presents
the case of a young male patient with EMP of the nasopharynx who
was treated successfully with surgery and radiotherapy. Written
informed consent was obtained from the patient.
Case report
A 15-year-old male was referred to the Department of
Otolaryngology, Cathay General Hospital (Taipei, Taiwan) due to
intermittent epistaxis lasting for 2 weeks. In addition, the
patient reported a 3-year history of persistent nasal obstruction.
A physical examination revealed an extremely large tumor in the
center of the nasopharynx that bled easily when touched. Computed
tomography revealed a mass occupying almost the entire
nasopharyngeal space without involvement of the bony structures
(Fig. 1). Surgical treatment was
arranged and the tumor was excised completely using a transpalatal
approach. Microscopically, the tumor showed sheets of monomorphic
round-to-oval cells with eccentric nuclei and a dense infiltration
of plasmacytoid cells (Fig. 2).
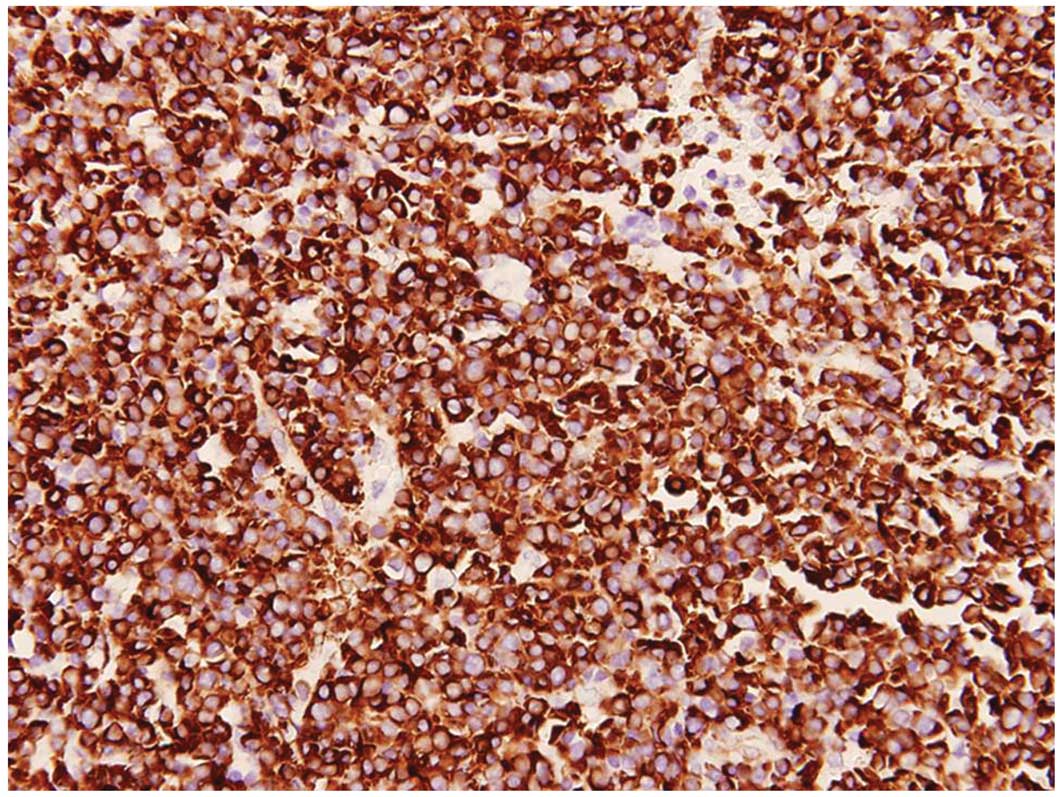
Significant nuclear pleomorphism was also noted (Fig. 3). Immunohistochemical staining
showed that the tumor cells were positive for the plasma cell
markers, Mum-1 and VS38c (Fig. 4),
and negative for CD3 and CD20. In addition, expression was was
positive for heavy chain immunoglobulin M. The complete blood cell
count and serum levels of calcium, creatinine, uric acid and β2
microglobulin were within normal limits. Electrophoresis of serum
and urine specimens did not reveal any monoclonal paraprotein and a
whole-body bone survey revealed no detectable osteolytic lesions. A
bone marrow aspiration was arranged and a plasma cell count of
<1% was noted. A few enlarged cervical lymph nodes were also
noted bilaterally, and the biopsy of the cervical lymph nodes
showed non-specific inflammatory reactions. A final diagnosis of
EMP of the nasopharynx was determined, and following tumor
excision, the patient underwent radiotherapy with 5,040 cGy in 28
fractions in the nasopharyngeal field. Repeated serum and urine
electrophoresis subsequent to 3 months revealed no M protein.
Discussion
Plasmacytomas have been classified into 3 subtypes.
The most common type is multiple myeloma, which is usually a
disseminated disease and is characterized by abnormal M protein.
The other 2 types, solitary plasmacytoma of the bone and EMP of the
soft tissue, are considerably less common. EMPs present in <5%
of plasma cell neoplasms and often (>80%) originate in the head
and neck region (7). EMPs represent
~4% of nasal cavity tumors and 0.4% of all head and neck
malignancies. The diagnosis of EMP of the soft tissue has been
based on the following criteria: i) Pathological tissue evidence of
monoclonal plasma cells involving a single extramedullary site; ii)
no bone marrow involvement; iii) negative skeletal survey results;
iv) no anemia, hypercalcemia or renal impairment caused by plasma
cell dyscrasia; and v) low serum or urinary levels of monoclonal
immunoglobulin (8). The M protein
is detected in the serum and/or urine of <25% of patients. There
is a greater male preponderance (male:female ratio, 3:1), and EMP
tends to occur during the fifth and seventh decades of life, rarely
being diagnosed in younger patients. In the head and neck region,
the majority of EMPs occur as a solitary tumor and ~10% are
multiple. Only four cases of EMP have been previously reported in
relatively young patients: i) Two 3.5-year-old males with
unexpected EMP following adenoidectomy for chronic rhinosinusitis
(9); ii) a 12-year-old female who
presented with progressive hoarseness and was subsequently found to
have EMP coexisting with localized amyloidosis involving the larynx
(10); and iii) an 11-year-old male
who presented with an EMP of the orbit (11). In the present patient, the tumor was
localized in the nasopharynx. There was no involvement of the bony
structure or bone marrow and the diagnosis of solitary EMP of the
nasopharynx was confirmed. To the best of our knowledge, this is
the youngest case of nasopharyngeal EMP to be reported in the
literature.
The etiology of this disease remains unknown, but
factors such as viral pathogenesis and chronic irritation from
inhaled irritants have been previously indicated (12–14).
Radiotherapy remains the mainstay for the management of EMP.
Previously, Susnerwala et al proposed a pathological grading
system based on the multiple myeloma grading criteria; tumors
classified into low, intermediate and high grades, which have been
found to correlate closely with outcomes. The study recommended the
use of adjuvant chemotherapy in patients with higher-grade disease
(14). In general, EMPs are
considered radiosensitive, with a local control rate of 90–100%
(15). A radiation dose of 40–50 Gy
delivered to the primary site of the EMP in the nasopharynx is
usually recommended (8).
Irradiation to the neck is required only in cases with clinically
positive cervical node metastasis. In a recent study by Sasaki
et al, it was found that radiotherapy was quite effective
and safe for patients with EMP in the head and neck region.
Moreover, radiotherapy combined with surgery produced an improved
outcome, as determined by survival rates (12). Although the role of chemotherapy in
EMP treatment has not been established, chemotherapy is usually
considered for EMPs with high risk factors for local treatment
failure (tumor size of >5 cm) and in cases of refractory disease
(8). Follow-up radiological and
electrophoresis assessment is required following treatment to
detect recurrence and progression to multiple myeloma, which occurs
in 10–30% of cases. The overall 10-year survival rate is ~70%
(7,8).
A literature search revealed no publications
supporting the use of surgery alone to treat EMP. In the current
case, although the tumor was well defined and thus completely
excised, and the patient recovered from the surgery smoothly,
subsequent irradiation was recommended. Only four cases of EMP have
been previously reported in relatively young patients. To the best
of our knowledge, the present case is the youngest case of
nasopharyngeal EMP to be reported in the literature.
References
|
1
|
Schridde H: Weitere Untersuchungen uber
die Kornelungen der Plasmazellen. Centralbl Allg Pathol Anat.
16:433–435. 1905.(Article in German).
|
|
2
|
Fu YS and Perzin KH: Nonepithelial tumors
of the nasal cavity, paranasal sinuses, and nasopharynx. A
clinicopathologic study VI Fibrous tissue tumors (fibroma,
fibromatosis, fibrosarcoma). Cancer. 37:2912–2928. 1976. View Article : Google Scholar
|
|
3
|
Knowling MA, Harwood AR and Bergsagel DE:
Comparison of extramedullary plasmacytomas with solitary and
multiple plasma cell tumors of bone. J Clin Oncol. 1:255–262.
1983.PubMed/NCBI
|
|
4
|
Galieni P, Cavo M, Pulsoni A, et al:
Clinical outcome of extramedullary plasmacytoma. Haematologica.
85:47–51. 2000.
|
|
5
|
Miller FR, Lavertu P, Wanamaker JR,
Bonafede J and Wood BG: Plasmacytomas of the head and neck.
Otolaryngol Head Neck Surg. 119:614–618. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nofsinger YC, Mirza N, Rowan PT, Lanza D
and Weinstein G: Head and neck manifestations of plasma cell
neoplasms. Laryngoscope. 107:741–746. 1997. View Article : Google Scholar
|
|
7
|
Straetmans J and Stokroos R:
Extramedullary plasmacytomas in the head and neck region. Eur Arch
Otorhinolaryngol. 265:1417–1423. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Soutar R, Lucraft H, Jackson G, et al:
Guidelines on the diagnosis and management of solitary plasmacytoma
of bone and solitary extramedullary plasmacytoma. Br J Haematol.
124:717–726. 2004. View Article : Google Scholar
|
|
9
|
Mann G, Trebo MM, Minkov M, Simonitsch I,
Chott A and Gadner H: Extramedullary plasmacytoma of the adenoids.
Pediatr Blood Cancer. 48:361–362. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nagasaka T, Lai R, Kuno K, Nakashima T and
Nakashima N: Localized amyloidosis and extramedullary plasmacytoma
involving the larynx of a child. Hum Pathol. 32:132–134. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sharma MC, Mahapatra AK, Gaikwad S and
Biswal A: Primary extramedullary orbital plasmacytoma in a child.
Childs Nerv Syst. 12:470–472. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sasaki R, Yasuda K, Abe E, et al:
Multi-institutional analysis of solitary extramedullary
plasmacytoma of the head and neck treated with curative
radiotherapy. Int J Radiat Oncol Biol Phys. 82:626–634. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sasaki S, Hashimoto K, Nakatsuka S, et al:
Plasmablastic extramedullary plasmacytoma associated with
Epstein-Barr virus arising in an immunocompetent patient with
multiple myeloma. Intern Med. 50:2615–2620. 2011. View Article : Google Scholar
|
|
14
|
Susnerwala SS, Shanks JH, Banerjee SS,
Scarffe JH, Farrington WT and Slevin NJ: Extramedullary
plasmacytoma of the head and neck region: clinicopathological
correlation in 25 cases. Br J Cancer. 75:921–927. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chao MW, Gibbs P, Wirth A, Quong G, Guiney
MJ and Liew KH: Radiotherapy in the management of solitary
extramedullary plasmacytoma. Intern Med J. 35:211–215. 2005.
View Article : Google Scholar : PubMed/NCBI
|