Introduction
Primary effusion lymphoma (PEL) is a rare type of
large B-cell lymphoma characterized by lymphomatous effusion of
body cavities without lymphadenopathy or organomegaly. PEL often
occurs in patients with human immunodeficiency virus (HIV) and/or
human herpes virus type 8 (HHV-8) infections (1). However, patients have been reported
with HHV-8-negative and HIV-negative PEL with high expression of B
cell markers. This is described as HHV-8-unrelated PEL-like
lymphoma (2). To date, only one
case report has described the presentation of PEL using
fluorodeoxyglucose (FDG) positron emission tomography
(PET)/computer tomography CT) (3),
and there has been no such study for PEL-like lymphoma. To the best
of our best knowledge, all cases of PEL or PEL-like lymphoma
reported in the literature were diagnosed by ascitic cytology. This
report presents a case of PEL-like lymphoma with negative ascitic
cytology, which was identified by FDG PET/CT and ultimately
confirmed by laparoscopic biopsy of the greater omentum. Written
informed consent was obtained from the patient’s family.
Case report
A 39-year-old male was referred to the First
Affiliated Hospital of Wenzhou Medical College (Wenzhou, China)
with a one-week history of abdominal pain and distension.
Laboratory tests revealed a white blood cell (WBC) count of
10.1×109 cells/l and hemoglobin levels of 12.8 g/dl.
Aspartate aminotransferase levels were 14 U/l and alanine
aminotransferase levels were 70 U/l. Tests for hepatitis markers,
Epstein-Barr virus (EBV), HHV-8, HIV and tumor markers were
negative.
The WBC count of the ascitic fluid was 640,000
cells/ml: 5% polymorphonuclear leukocytes, 71% lymphocytes and 24%
abdominal cells. Bacterial cultures were negative. The ascitic
effusion test for HHV-8 using polymerase chain reaction was also
negative. Ascitic cytology was performed three times but no
malignant cells were found. Gastroscopy and colonoscopy were also
normal.
Enhanced abdominal CT scan showed massive ascites
and enhanced peritoneum, mesenterium and greater omentum but no
detectable mass or lymphadenopathy. Therefore, the patient
underwent FDG PET/CT examination. FDG PET/CT showed FDG uptake in
the peritoneum, mesenterium and greater omentum (Fig. 1). No mass or lymphoma cells were
detected by whole-body CT, FDG PET or bone marrow biopsy.
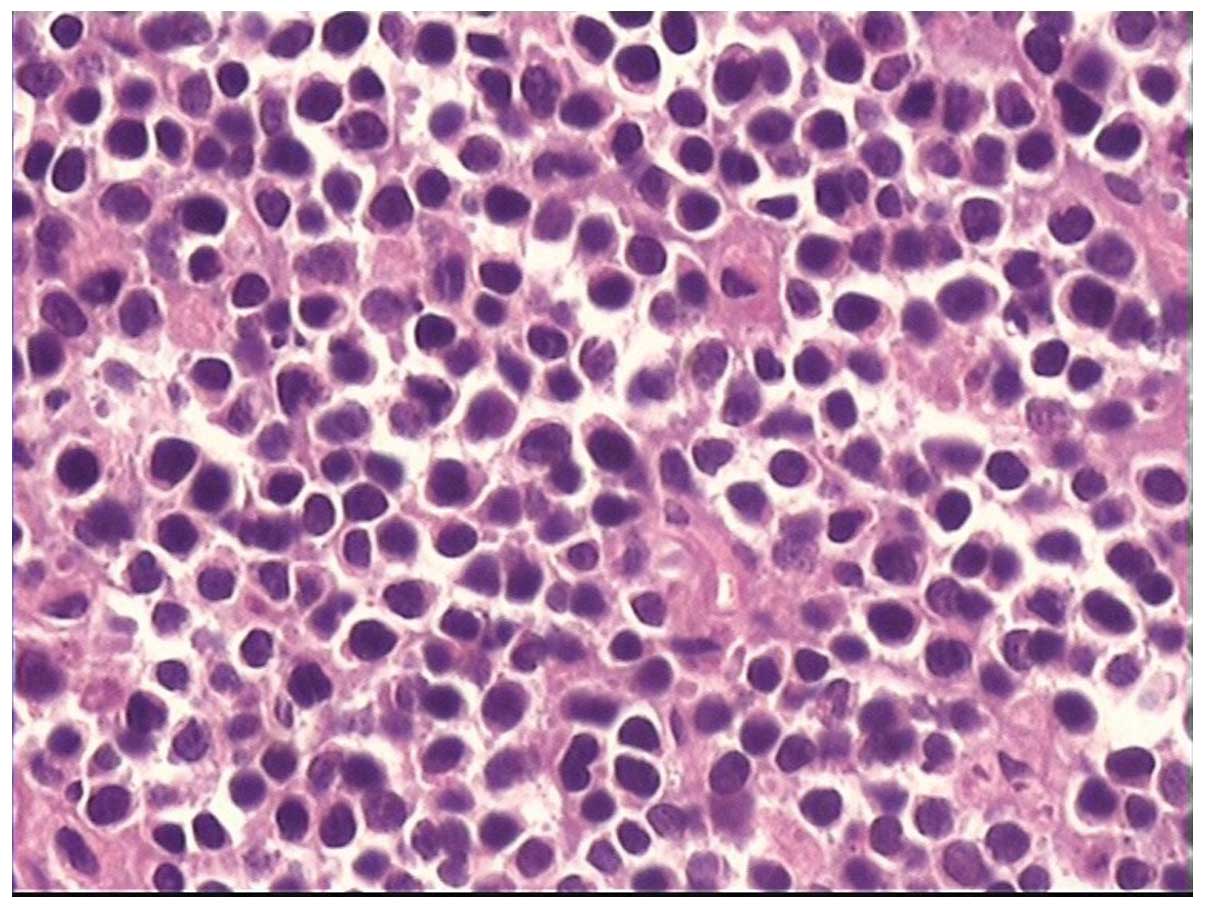
A laparoscopic biopsy of the greater omentum was
performed, revealing lymphoma cells with large nuclei and abundant
cytoplasm which exhibited a B-cell phenotype (Fig. 2). Immunohistochemical staining
revealed that the large atypical cells were positive for cluster of
differentiation (CD) 10 (+), CD20 (++++), CD79a (++++), Ki67
(95%+), multiple myeloma oncogene 1 (++) and paired box 5 (++), but
negative for anaplastic lymphoma kinase, B cell lymphoma (Bcl) 2,
Bcl-6, CD2, CD117, CD21, CD3, CD30, CD34, CD43, CD5, CD56, CD68,
CD7, CD99, CD1A, creatine kinase, cyclin-D1, Epstein Barr
virus-encoded RNA, epithelial membrane antigen, granzyme B,
myeloperoxidase, perforin and terminal deoxynucleotidyl
transferase.
The patient was diagnosed with HHV-8-unrelated
HIV-negative PEL-like lymphoma (indeterminate phenotype). The
patient and his relatives refused chemotherapy and the patient
succumbed to PEL-like lymphoma one month later.
Discussion
PEL is often associated with HHV-8 and occurs most
frequently in immunodeficient states (1). However, the etiology of
HHV-8-unrelated PEL-like lymphoma is unknown. Hepatitis C virus
(HCV) infection has been suggested to induce persistent antigenic
stimulation that results in B-cell clonal expansion (4). The reported rate of association of
PEL-like lymphoma with HCV is 30–40% (5). However, in the majority of patients
with HHV-8-unrelated PEL-like lymphoma, as was the case in the
present study, no known pathogens, including HIV, EBV, HCV, or
iatrogenic immunodeficiency, can be identified (4).
The diagnosis of PEL-like lymphoma is primarily
based on cytological evaluation of fluid material by
immunohistochemistry or flow cytometry. However, no malignant cells
were found despite the fact that ascitic cytology had been
performed three times in the current case study. Therefore, this
patient underwent FDG PET/CT examination and laparoscopic omentum
biopsy. As a useful non-invasive diagnostic tool, FDG PET
supplements conventional imaging in diagnosis of peritoneal
disease, as this technique can detect lesions not identified by CT
(6). Makis et al(3) first described the appearance of F-18
FDG PET/CT in a patient with hepatitis C-related PEL. Results
showed a marked increased F-18 FDG uptake in the pleura and
peritoneum on the left side. The current case report demonstrates
increased F-18 FDG uptake in the peritoneum, mesenterium and
greater omentum. As FDG is taken up by macrophages, granulation
tissues and inflammatory tissues, in addition to tumor cells,
intense F-18 FDG uptake in the peritoneum may also occur in
tuberculous peritonitis, peritoneal carcinomatosis, and peritoneal
mesothelioma (3). To date, no
reliable PET/CT criteria have been established for differential
diagnosis of these diseases (6).
There is no consensus on the optimal treatment of
HHV-8-unrelated PEL-like lymphoma due to the small number of
published reports. Cyclophosphamide hydroxydaunorubicin oncovin
prednisone-like regimen (1) or rituximab-containing regimen (2)
have frequently been administered in these cases. Although the
prognosis of HIV-negative HHV-8-unrelated PEL-like lymphoma
patients is better than the HIV-positive PEL group (1), in this case, the prognosis was still
poor and the patient succumbed to PEL-like lymphoma one month
following diagnosis.
In conclusion, PET/CT and laparoscopic biopsy may be
useful diagnostic tools for PEL-like lymphoma when the origins of
ascites cannot be determined by general ascitic examination or
conventional imaging tests, such as CT scans.
References
|
1
|
Adiguzel C, Bozkurt SU, Kaygusuz I, et al:
Human herpes virus 8-unrelated primary effusion lymphoma-like
lymphoma: report of a rare case and review of the literature.
APMIS. 117:222–229. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Takahashi T, Hangaishi A, Yamamoto G, et
al: HIV-negative, HHV-8-unrelated primary effusion lymphoma-like
lymphoma: report of two cases. Am J Hematol. 85:85–87. 2010.
|
|
3
|
Makis W and Stern J: Hepatitis C-related
primary effusion lymphoma of the pleura and peritoneum, imaged with
F-18 FDG PET/CT. Clin Nucl Med. 35:797–799. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang T, Nava VE, Schechter GP, et al:
Human herpes virus 8-unrelated primary effusion lymphoma-like
lymphoma: a patient successfully treated with pleurodesis. J Clin
Oncol. 29:e747–e750. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kobayashi Y, Kamitsuji Y, Kuroda J, et al:
Comparison of human herpes virus 8 related primary effusion
lymphoma with human herpes virus 8 unrelated primary effusion
lymphoma-like lymphoma on the basis of HIV: report of 2 cases and
review of 212 cases in the literature. Acta Haematol. 117:132–144.
2007. View Article : Google Scholar
|
|
6
|
Anthony MP, Khong PL and Zhang J: Spectrum
of (18)F-FDG PET/CT appearances in peritoneal disease. AJR Am J
Roentgenol. 193:W523–W529. 2009. View Article : Google Scholar : PubMed/NCBI
|