Introduction
Sclerosing hemangioma (SH) of the lung is an
uncommon tumor that was first described by Leibow and Hubbell in
1956 (1). SH is a lung tumor with a
distinctive constellation of histological findings, including
solid, papillary, sclerotic and hemorrhagic patterns (2). SH usually presents as a slow-growing
benign mass in the lower lobes of middle-aged females (3). Several reports have described
multicentric SHs or SHs with lymph node metastasis (4–19).
Thus, SH is not always benign and it has the potential to
metastasize.
Case report
Clinical summary
A 40-year-old female was referred to Toyooka
Hospital (Toyooka, Hyogo, Japan) after chest X-ray screening
revealed a nodule in the left lower pulmonary field. The patient
had no history of smoking. Family history was negative for relevant
diseases. Blood tests revealed no increase in concentrations of
tumor markers.
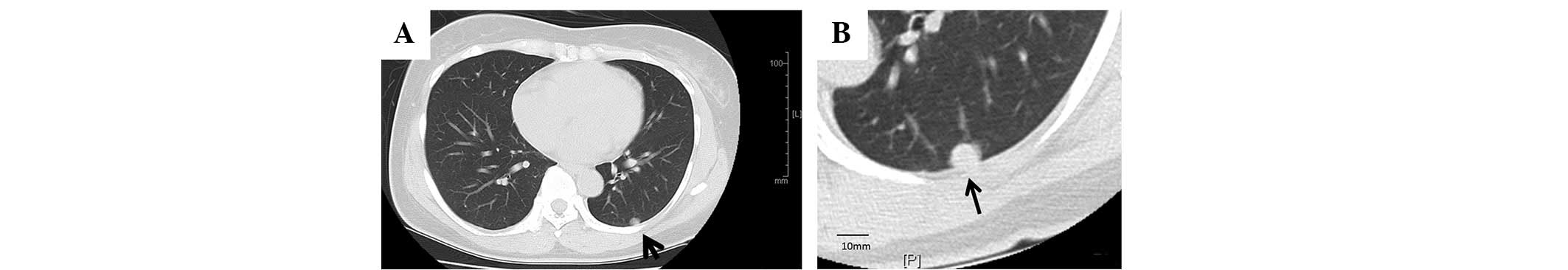
Chest computed tomography (CT) scanning revealed a
nodule ~10 mm in diameter in the left lower lung (Fig. 1), but no mediastinal or hilar lymph
node swelling. The patient underwent lobectomy of the left lower
lung with lymph node dissection.
Pathological findings
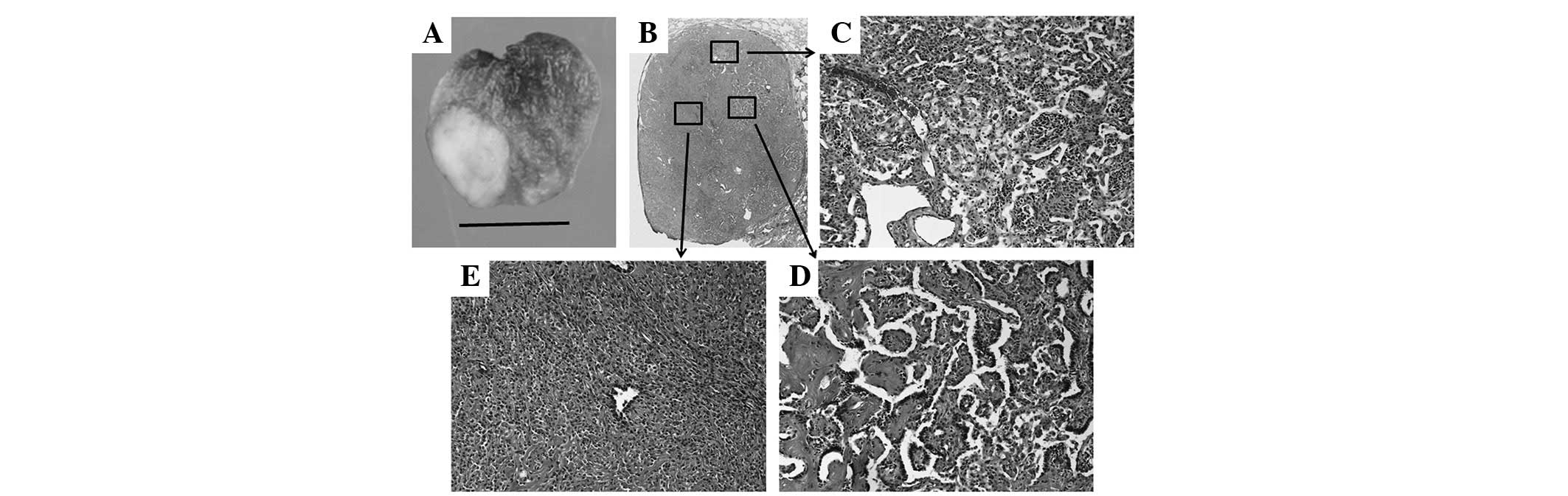
Macroscopically, the tumor was sharply demarcated
from the surrounding lung tissue and ~10×10×10 mm in size (Fig. 2A). The cut surface was whitish and
sclerotic.
Microscopically, the tumor demonstrated various
features characteristic of SH, including angiomatoid areas,
sclerosis, papillary structures lined with cuboidal cells and
sheets of round to polygonal cells with slightly eosinophilic
cytoplasms.
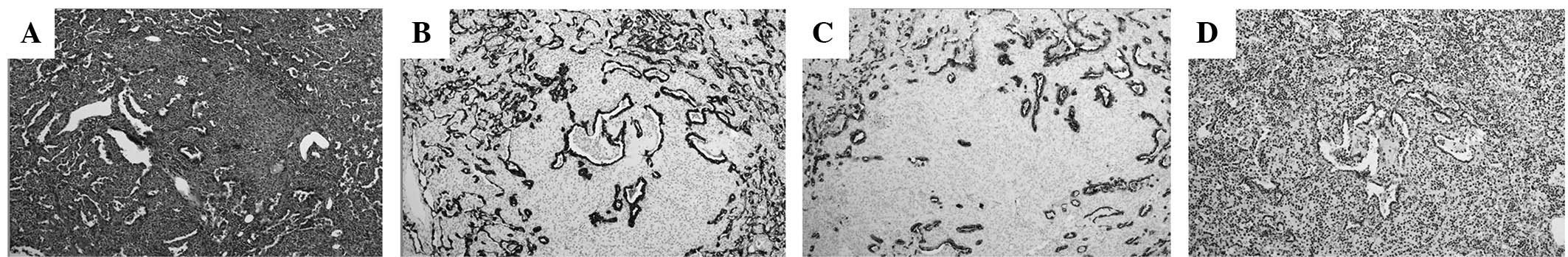
Immunohistochemically, the surface-lining cells were
positive for napsin A, cytokeratin AE1/AE3 (Fig. 3) and cytokeratin 7 (data not shown).
The other cells were negative for these markers. However, all the
tumor cells (both the surface-lining and polygonal cells) were
positive for thyroid transcription factor 1 (TTF-1), which is
expressed not only in thyroid epithelial cells but also in type II
pneumocytes and Clara cells, and epithelial membrane antigen. These
findings suggested that the tumor was an SH.
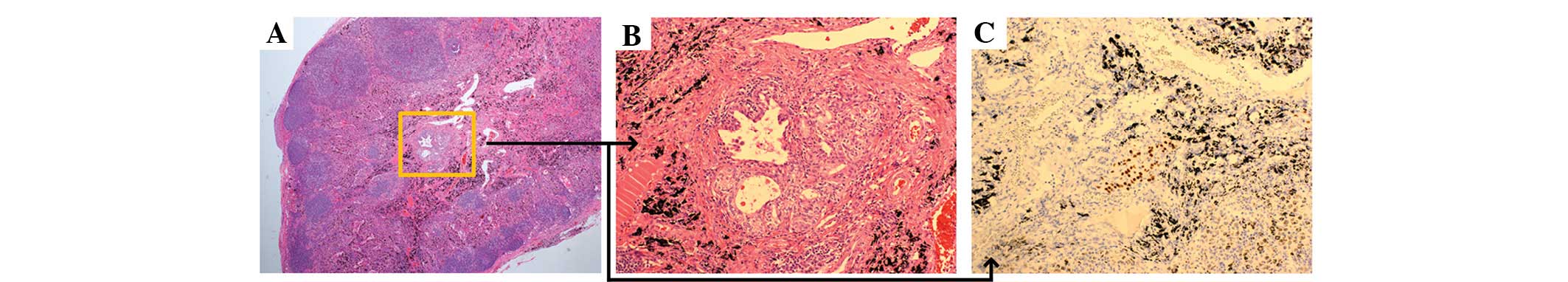
A small metastatic focus of SH was identified in one
mediastinal lymph node. This lesion shared the papillary pattern of
the primary tumor and was TTF-1-positive (Fig. 4). The patient provided written
informed consent. This study was approved by the Ethics Committee
of Toyooka Hospital (Toyooka, Japan).
After two years of follow-up the patient has not
exhibited any recurrence nor metastasis of the tumor.
Discussion
Pulmonary SH was originally thought to be derived
from the endothelium due to histological similarity to cutaneous SH
(1).
In the present literature review, PubMed and JDream
III (http://jdream3.com/) were used to search for
studies written in English or Japanese reporting cases of pulmonary
SH with metastasis in the lymph nodes, using the search terms
‘sclerosing hemangioma’, ‘lung’ and ‘metastasis’. The results of
these searches returned 17 such cases, of which 13 were in English
and 4 in Japanese. Of the 4 studies written in Japanese, 3 cases
were abstracts of congresses. Table
I lists these cases, including the present report.
 | Table ICases of pulmonary sclerosing
hemangioma with lymph node metastasis. |
Table I
Cases of pulmonary sclerosing
hemangioma with lymph node metastasis.
| | | Primary tumor | Metastases | |
|---|
| | |
|
| |
|---|
| No. | Age, years | Gender | Location | Size, mm | Lymph nodes, n | Maximum size, mm | Location | Reference |
|---|
| 1 | 22 | M | R lower | 50 | 1 | 3 | Hilum | 6 |
| 2 | 48 | M | R lower | 80 | 2 | 2 | Hilum | 7 |
| 3 | ND | ND | ND | 35 | 2 | ND | Hilum | 8 |
| 4 | 67 | F | R lower | 90 | 5 | ND | Hilum,
mediastinum | 9 |
| 5 | 10 | F | R middle | 47 | 1 | 5 | Regional | 10 |
| 6 | 45 | F | R upper | 25 | 3 | 7 | Hilum | 10 |
| 7 | 45 | M | L lower | 37 | 1 | 3 | Mediastinum | 10 |
| 8 | 50 | F | L lower | 15 | 1 | 12 | Intralobular | 10 |
| 9 | 19 | M | L upper
(lingula) | 30 | ND | ND | Intrapulmonary,
intralobular | 11 |
| 10 | 19 | F | L Lower | 100 | 11 | ND | Intrapulmonary,
interlobular, hilum | 12 |
| 11 | 37 | F | L lower | 20 | 1 | ND | Saltcellar | 13 |
| 12 | 35 | M | L lower | ND | 1 | ND | Mediastinum | 14 |
| 13 | 23 | M | R upper | 90 | Multiple | ND | Hilum | 15 |
| 14 | 24 | F | R lower | ND | ND | ND | ND | 16 |
| 15 | 35 | M | L lower | 33 | 2 | ND | Mediastinum | 17 |
| 16 | 55 | M | R lower | 22 | 1 | ND | Intrapulmonary | 18 |
| 17 | 38 | F | L lower | 33 | 1 | ND | Intralobular | 19 |
| 18 | 40 | F | L lower | 10 | 1 | 0.5 | Mediastinum | PC |
Analysis of the data provided in these reports
revealed the following about SH with lymph node metastasis: i) The
age of the patients ranged between 22 and 67 years [mean ± SD,
36±15 years]; ii) males accounted for 8/17 cases (47.1%) and
females 9/17 cases (52.9%); iii) 9/17 (52.9%) primary tumors were
found in the left lung and 8/17 (47.1%) were found in the right
lung; iv) the left upper lobe was involved in 1/17 cases (5.9%),
the left lower lobe in 8 (47.1%), the right upper lobe in 2
(11.8%), the right middle lobe in 1 (5.9%) and the right lower lobe
in 5 (29.4%); and v) the primary tumors ranged in size between 10
and 100 mm (mean, 44.8±29.1 mm).
Previously, Devouassoux-Shisheboran et al
analyzed 100 cases of SH, including one with lymph node metastasis
(8). In this study, the clinical
and pathological features of these tumors were analyzed in detail.
Patients ranged in age between 13 and 76 years (mean, 46 years).
There were 83 female and 17 male patients; thus, the female-to-male
ratio was 5:1. The left lung was the site of 46% of tumors (17% in
the left upper lobe, 25% in the left lower lobe, 1% in the fissure
between the upper and lower lobe and the specific site was unknown
in 3% of cases), and 54% were found in the right lung (9% in the
right upper lobe, 17% in the right middle lobe, 22% in the right
lower lobe, 4% in the fissure between the middle and upper lobe, 1%
in the fissure between the middle and lower lobe and the specific
site was unknown in 1% of cases). The tumors ranged in size between
3 and 70 mm (mean, 26 mm).
In the present study, the cases of SH with lymph
node metastases that we compiled were compared with the cases of SH
that Devouassoux-Shisheboran et al analyzed (8). As shown in Table II, SH with lymph node metastasis
tended to occur more often in relatively young male patients than
SH without metastasis. The mean size of primary SHs that had lymph
node metastasis was larger than the mean size of non-metastatic
primary SHs.
 | Table IISH cases and SH cases with lymph node
metastasis. |
Table II
SH cases and SH cases with lymph node
metastasis.
| Parameter | SHa | SH with lymph node
metastasisb |
|---|
| Patients, n | 100 | 18 |
| Age, years
(mean) | 13–76 (46) | 22–67 (36±15) |
| Gender, male :
female | 1:5 | 8:9 |
| Primary tumor size,
mm (mean) | 3–70 (26) | 10–100
(44.8±29.1) |
| Primary tumor
location, % |
| Left lung | 46 | 53 |
| Right lung | 54 | 47 |
| Left upper lobe | 16 | 6 |
| Left lower lobe | 25 | 48 |
| Right upper
lobe | 9 | 11 |
| Right middle
lobe | 16 | 6 |
| Right lower
lobe | 22 | 29 |
The findings that SHs with lymph node metastasis are
larger and occur in younger patients may possibly correlate with
the more rapid growth of these tumors. However, it is difficult to
explain why there is a high frequency of SHs with lymph node
metastasis in male patients and in the left lower lobe. Further
investigation is required to elucidate the mechanism of metastasis
of SH.
References
|
1
|
Liebow AA and Hubbell DS: Sclerosing
hemangioma (histiocytoma, xanthoma) of the lung. Cancer. 9:53–75.
1956. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Devouassoux-Shisheboran M, Nicholson AG,
Leslie K and Niho S: Sclerosing hemangioma. World Health
Organisation Classification of Tumours: Tumors of lung, pleura,
thymus and heart. Travis WD, Brambilla E, Muller-Hemelink HK and
Harris CC: IARC Press; Lyon: pp. 115–117. 2004
|
|
3
|
Keylock JB, Galvin JR and Franks TJ:
Sclerosing hemangioma of the lung. Arch Pathol Lab Med.
133:820–825. 2009.PubMed/NCBI
|
|
4
|
Maeda R, Isowa N, Miura H, Tokuyasu H,
Kawasaki Y and Yamamoto K: Bilateral multiple sclerosing
hemangiomas of the lung. Gen Thorac Cariovasc Surg. 57:667–670.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Joshi K, Shankar SK, Gopinath N, Kumar R
and Chopra P: Multiple sclerosing haemangiomas of the lung.
Postgrad Med J. 56:50–53. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tanaka I, Inoue M, Matsui Y, Oritsu S,
Akiyama O, Takemura T, Fujiwara M, Kodama T and Shimosato Y: A case
of pneumocytoma (so-called sclerosing hemangioma) with lymph node
metastasis. Jpn J Clin Oncol. 16:77–86. 1986.PubMed/NCBI
|
|
7
|
Chan AC and Chan JK: Pulmonary sclerosing
hemangioma consistently expresses thyroid transcription factor-1
(TTF-1): a new clue to its histogenesis. Am J Surg Pathol.
24:1531–1536. 2000. View Article : Google Scholar
|
|
8
|
Devouassoux-Shisheboran M, Hayashi T,
Linnoila RI, Koss MN and Travis WD: A clinicopathologic study of
100 cases of pulmonary sclerosing hemangioma with
immunohistochemical studies: TTF-1 is expressed in both round and
surface cells, suggesting an origin from primitive respiratory
epithelium. Am J Surg Pathol. 24:906–916. 2000. View Article : Google Scholar
|
|
9
|
Yano M, Yamakawa Y, Kiriyama M, Hara M and
Murase T: Sclerosing hemangioma with metastases to multiple nodal
stations. Ann Thorac Surg. 73:981–983. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Miyagawa-Hayashino A, Tazelaar HD, Langel
DJ and Colby TV: Pulmonary sclerosing hemangioma with lymph node
metastases: report of 4 cases. Arch Pathol Lab Med. 127:321–325.
2003.PubMed/NCBI
|
|
11
|
Chan NG, Melega DE, Inculet RI and
Shepherd JG: Pulmonary sclerosing hemangioma with lymph node
metastases. Can Respir J. 10:391–392. 2003.PubMed/NCBI
|
|
12
|
Kim KH, Sul HJ and Kang DY: Sclerosing
hemangioma with lymph node metastasis. Yonsei Med J. 44:150–154.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim GY, Kim J, Choi YS, Kim HJ, Ahn G and
Han J: Sixteen cases of sclerosing hemangioma of the lung including
unusual presentations. J Korean Med Sci. 19:352–358. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Katakura H, Sato M, Tanaka F, Sakai H,
Bando T, Hasegawa S, Nakashima Y and Wada H: Pulmonary sclerosing
hemangioma with metastasis to the mediastinal lymph node. Ann
Thorac Surg. 80:2351–2353. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vaideeswar P: Sclerosing hemangioma with
lymph nodal metastases. Indian J Pathol Microbiol. 52:392–394.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ymazaki A, Masuda S, Ose Y, Tahara M,
Nakahara K and Hayashi I: Sclerosing hemangioma in right lung with
lymph node metastasis. In: Proceedings of the 124th Kanto Branch
Congress of the Japan Lung Cancer Society; Tokyo. The Japan Lung
Cancer Society; Tokyo: pp. 2231999
|
|
17
|
Katakura H, Sakai H, Tanaka H, Chin T,
Ogawa E, Ri M, Kawashima M, Yanagihara K, Hanaoka S, Bando T,
Hasegawa S and Wada H: A case of pulmonary sclerosing hemangioma
with lymph node metastasis. In: Proceedings of the 78th Kansai
Branch Congress of the Japan Lung Cancer Society; Osaka. The Japan
Lung Cancer Society; Tokyo: pp. 7682003
|
|
18
|
Nakajima D, Sumitomo S, Matsumoto K,
Tarumi S, Mori N and Sumitomo R: A case of pulmonary sclerosing
hemangioma with lymph node metastasis (Japanese). Nippon Kokyuki
Geka Gakkai Zasshi. 24:74–77. 2010.
|
|
19
|
Kita H, Shiraishi Y, Katsushiro N,
Hyougotani A, Hiramatsu M and Shimoda K: A case of sclerosing
hemangioma with lymph node metastasis. In: Proceedings of the 52nd
Congress of the Japan Lung Cancer Society; Osaka. The Japan Lung
Cancer Society; Tokyo: pp. 6182011
|