Introduction
Imatinib mesylate (IM) is a first-generation
tyrosine kinase inhibitor used in the treatment of chronic myeloid
leukemia (CML), gastrointestinal stromal tumors and other types of
cancer (1). In CML, IM inhibits the
oncoprotein breakpoint cluster region-abelson 1 (BCR-ABL1) from
phosphorylating subsequent proteins and initiating the signaling
cascade necessary for CML development (2). The long-term follow-up results of the
International Randomized Study of Interferon and STI-571 trial have
confirmed the benefits of IM and the durable response of the drug.
Following eight years of IM treatment, no disease progression was
identified in patients who achieved complete cytogenetic response
(CCyR) and major molecular response (MMR) (3). Therefore, achieving and maintaining
such responses are essential for the survival of CML patients
treated with IM.
Despite the high efficacy of IM treatment in CML,
some patients fail to achieve optimal response. Mutations in the
kinase domain of BCR-ABL1 are the main causes of resistance to IM
treatment. The mutations interfere with the binding of IM to its
target, which subsequently decreases the efficacy of the drug
(4). However, accumulating data
have indicated a contributing role of pharmacokinetics in IM
efficacy, as well as in the initial therapeutic response and time
to progression. Variations in drug uptake and efflux transporter
activity may affect IM absorption, distribution and excretion,
thereby influencing the pharmacokinetics (5).
Several previous studies have demonstrated that IM
is a substrate of membrane transporters, such as the ATP-binding
cassette subfamily B member 1 [ABCB1; also termed
P-glycoprotein(P-gp) and multidrug resistance protein 1 (MDR1)] and
solute carrier family 22 member 1 [SLC22A1; also termed human
organic cation transporter type 1 (hOCT1)] (6–8). The
ABCB1 gene is located in the 7q21.1 chromosome (9) and encodes a glycoprotein of 170 KDa
(P-gp and MDR1) (10). The
structure of P-gp is comprised of a transmembrane domain with six
hydrophobic segments and a cytoplasmic domain with a binding site
for ATP, which is responsible for the ATP-dependent movement of a
wide variety of xenobiotics (including drugs), lipids and metabolic
products across the plasma and intracellular membranes (11). Since P-gp is involved in the efflux
of a broad spectrum of drugs, variations in protein expression or
activity may affect the pharmacokinetics of IM by reducing or
increasing its bioavailability.
The ABCB1 gene is highly polymorphic and >1,200
single nucleotide polymorphisms (SNPs) have been identified within
this gene, of which 50 are found within the coding region (12). Three of these SNPs have been
particularly investigated: Two silent polymorphisms, c.1236C>T
and c.3435C>T; and one polymorphism in the promoter region,
c.2677G>T/A, which results in two different amino acid changes
(Ala893Ser/Thr). These polymorphisms are in strong linkage
disequilibrium and form the three most common haplotypes
(1236CC/3435CC/2677GG, 1236CT/3435CT/2677GT and
1236TT/3435TT/2677TT) (13). In the
cell lines expressing wild-type and mutant haplotypes with
c.1236C>T, c.3435C>T and c.2677G>T/A polymorphisms, no
alterations have been previously observed in the mRNA expression of
ABCB1 and P-gp protein length. However, it has been demonstrated
that haplotypes containing the mutated alleles show major
structural modifications that result in changes in the conformation
of the binding sites and a subsequent decrease in P-gp activity
(12–14).
In our previous study, the ABCB1
1236CT/3435CT/2677GT haplotype was found to correlate with MMR in
patients responsive to a standard dose of IM (15). However, the haplotype formed by the
c.1236C>T, c.3435C>T and c.2677G>T/A polymorphisms in the
ABCB1 gene may be associated with the variability of responses to
IM due to changes in the functionality of the P-gp efflux pump.
Therefore, the aim of the present study was to evaluate the
functional activity of P-gp in order to assess the effect of the
ABCB1 1236CC/3435CC/2677GG, 1236CT/3435CT/2677GT and
1236TT/3435TT/2677TT haplotypes on the efflux capacity mediated by
P-gp. In addition, the possible impact on the plasma concentration
of IM and molecular responses in patients with CML treated with a
standard dose of IM (400 mg/day) were investigated.
Materials and methods
Subjects
In total, 28 patients with chronic-phase CML were
selected according to the haplotypes of ABCB1 with
c.1236C>T, c.3435C>T and c.2677G>T polymorphisms at the
Santa Casa Medical School and Hospital Brigadeiro (both São Paulo,
Brazil). A total of 10 patients were identified with the
1236CC/3435CC/2677GG haplotype of ABCB1 and placed into the
wild-type group and 18 patients were identified as carriers of
haplotypes with at least one mutated allele in each genotype of the
three previously described ABCB1 polymorphisms (10 patients
with the 1236CT/3435CT/2677GT haplotype and eight patients with the
1236TT/3435TT/2677TT haplotype) were placed into the mutated group.
The patients were matched for the duration of IM treatment. In
addition, all patients were in the chronic phase of CML, were
treated with a standard dose of IM (400 mg/day) for an average time
period of 60.3±12.6 months and achieved CCyR.
The study protocol was approved by the
Investigational Review Board of the University of São Paulo (São
Paulo, Brazil), the Hospital Brigadeiro and the Santa Casa Medical
School. Written informed consent was obtained from all
participants.
Analysis of ABCB1 polymorphisms
Genomic DNA was isolated from the peripheral blood
using a QIAamp DNA blood mini kit (PreAnalytiX GmbH,
Feldbachstrasses, Switzerland) according to the manufacturer’s
instructions. ABCB1 genotyping was performed using
quantitative polymerase chain reaction (qPCR) followed by
restriction fragment length polymorphism analysis, as described
previously for the c.3435C>T, c.2677G>T/A (16) and c.1236C>T (17) polymorphisms. The accuracy of the
genotyping was evaluated by performing a duplicate analysis of 20%
of the randomly selected samples. Furthermore, 10% of the genotypes
were confirmed by DNA sequencing.
Isolation of peripheral blood
mononucleated cells (PBMCs)
Isolation of the PBMCs was performed by collecting
peripheral blood in Vacutainer® CPT™ tubes (BD
Biosciences, Franklin Lakes, NJ, USA). The tubes were inverted five
times and centrifuged at 1,720 × g for 20 min at room temperature.
Following centrifugation, PBMCs (monocytes and lymphocytes) remain
above the gel barrier and, thus, were suspended in the plasma by
inverting the tubes. Next, the tubes were centrifuged at 300 × g
for 10 min at room temperature, the supernatant was discarded and
the pellet was suspended in phosphate-buffered saline (PBS).
Isolation of mRNA and cDNA synthesis
PBMC mRNA was extracted using a RNeasy mini kit
(PreAnalytiX GmbH) according to the manufacturer’s instructions.
The concentration and purity of the isolated mRNA was measured
using Nanodrop™ ND-1000 (Nanodrop Technologies, Wilmington, ME,
USA) and the cDNA was synthesized from 500 ng of RNA using the
High-Capacity RNA-to-cDNA™ kit (Invitrogen Life Technologies,
Carlsbad, CA, USA).
BCR-ABL1 mRNA levels
BCR-ABL1 transcripts were measured by qPCR,
as previously described (18). MMR
and complete molecular response (CMR) were defined as a reduction
of BCR-ABL1 transcript levels to <0.1 and 0.0032%,
respectively, in the peripheral blood samples which were
standardized according to the international scale (4).
ABCB1 and SLC22A1 mRNA expression
The mRNA expression of ABCB1 and SLC22A1 was
determined by qPCR using TaqMan™ assays (Hs00184500_m1 and
Hs00427552_m1, respectively; Applied Biosystems, Inc. Foster City,
CA, USA). A total of five genes (B2M, GAPDH, HMBS,
HPRT1 and SDHA) were analyzed using geNorm™ software
(Biogazelle, Zwijnaarde, Belgium)(19) and GAPDH was selected as the
reference gene. The relative quantification value of each gene was
analyzed using a comparative CT method. The following formula was
used to calculate the relative level of transcripts in the sample,
normalized to the reference gene, GAPDH: Gene expression =
2−ΔCT, where ΔCT = CT of the gene of interest - CT of
the reference gene.
All reactions were duplicated and each reaction
plate was performed without a sample as a negative control to
assess the possible contamination of reagents.
Flow cytometric assessment of P-gp
activity [rhodamine 123 (Rh123) efflux]
P-gp functional activity was assessed by the ability
of cells to induce the cellular efflux of Rh123, a P-gp substrate,
using flow cytometry (20). The
PBMCs (1×106) were incubated with Rh123 (1 μM) in PBS at
37°C for 15 min in the dark. The cells were then incubated in the
presence and absence of a P-gp inhibitor, PSC-833 (50 μM), for 1 h
at 37°C. At 0 and 60 min of incubation, cells were washed twice
with PBS. Next, the cell pellet was suspended in 300 μl PBS and
immediately used for the flow cytometric analysis of Rh123
retention. The Rh123 fluorescence was determined by flow cytometry
using the FACSCanto II flow cytometer (BD Biosciences) at a
wavelength of 525 nm. Lymphocytes were gated by forward and side
scatter, excluding cell debris and other blood cells. In total,
10,000 cells were counted in each sample. The P-gp mediated efflux
was calculated using the following formulae: Rh123 efflux (%) =
([Rh123] at 0 min - [Rh123] at 60 min)/[Rh123] at 0 min; and P-gp
mediated efflux (%) = Rh123 efflux in the absence of PSC-833 (%) -
Rh123 efflux in the presence of PSC-833 (%).
Determination of P-gp expression
The PBMCs of all patients were tested for P-gp
expression, which was quantified using mouse anti-human P-gp
monoclonal antibody (17F9; Santa Cruz Biotechnology Inc., Santa
Cruz, CA, USA). The protocol was adapted from that of Rodrigues
et al (21). Briefly, the
PBMCs (1×106) were washed with PBS and fixed with 1%
formaldehyde for 15 min at room temperature. Following one wash
with PBS, the cells were incubated with the primary anti-human
monoclonal P-gp antibody, 17F9 (1:50 dilution in PBS), overnight at
4°C. Following incubation, the cells were washed with PBS and
incubated with the secondary antibody (1:50 dilution in PBS), goat
anti-IgG antibody conjugated with fluorescein isothiocyanate
(FITC), for 40 min at 4°C. Following incubation, the cells were
suspended in 300 μl PBS for flow cytometric analysis using the
FACSCanto II flow cytometer (BD Biosciences). Lymphocytes were
gated as previously described and a total of 10,000 cells were
counted in each sample. As a negative control, PBS was used instead
of the primary antibody.
The results were expressed as the ratio between the
mean fluorescence intensity (MFI) of cells treated with the 17F9
primary antibody and FITC-labeled secondary antibody, divided by
the MFI of cells treated with the secondary antibody only (negative
control). Values >1.1 were considered positive for P-gp
expression (20).
Imatinib plasma levels
Blood samples were collected 24 h (±2 h) following
the administration of the IM dose, according to the instructions of
Larson et al (22). Plasma
concentrations of IM and its metabolite, CGP74588, were measured
using capillary electrophoresis with lidocaine (Sigma-Aldrich, St.
Louis, MO, USA) as the internal standard, according to the
instructions of Ajimura et al (23), with minor modifications. The limit
of quantification was 0.125 μg/ml, and the precision and accuracy
(coefficient of variation) at concentrations between 0.125 and 5.00
μg/ml were >15%.
Statistical analysis
The database and statistical analysis were performed
using the SPSS software, version 17.0 (SPSS, Inc., Chicago, IL,
USA) and graphs were obtained with GraphPad, version 5.04 (GraphPad
Software, San Diego, CA, USA). Numerical variables were compared
using the Student’s t-test or Mann-Whitney U test. Comparison of
categorical variables was performed by the χ2 or
likelihood ratio tests. The non-parametric Mann-Whitney U test was
used to evaluate the differences in the mRNA expression of the
ABCB1 and SLC22A1 genes, IM plasma levels and P-gp activity among
the groups with different haplotypes. Spearman’s correlations were
conducted to assess the associations between the patient variables
(P-gp activity, P-gp expression, ABCB1 and SLC22A1 mRNA expression,
BCR-ABL1 transcripts and IM plasma levels). Values >0.7 were
considered to indicate a strong correlation, 0.3–0.7 a moderate
correlation and <0.3 a weak correlation. P<0.05 was
considered to indicate a statistically significant difference.
Results
Clinical results
The patients included in the present study had
similar distributions in age, blood cell counts (erythrocytes,
leukocytes and platelets), time of diagnosis, treatment prior to IM
and initiation of IM treatment (P>0.05), according to the
different haplotype groups. All patients achieved complete
hematologic response and CCyR (Table
I). In addition, the frequencies of MMR and CMR in the
wild-type and mutated groups were comparable (80 vs. 88.9% for MMR;
and 20 vs. 17.7% for CMR; P>0.05).
 | Table IDistribution of a number of variables
between the CML patients. |
Table I
Distribution of a number of variables
between the CML patients.
| Haplotype | |
|---|
|
| |
|---|
| Variables | Wild-type
(n=10) | Mutated (n=18) | P-value |
|---|
|
Agea | 51.2
(30.2–57.0) | 53.7
(33.8–68.0) | 0.627 |
| Erythrocytes
(x106/mm3)a | 4.59
(4.21–5.12) | 4.3
(3.98–5.10) | 0.885 |
| Leukocytes
(x103/mm3)a | 5.10
(4.30–5.80) | 4.22
(3.92–6.57) | 0.797 |
| Platelets
(x103/mm3)a | 200 (180–237) | 193 (178–248) | 0.795 |
| Time of diagnoses
(months)a | 62.5
(59.7–100) | 65.5
(59.0–109.2) | 0.832 |
| Preview treatment
to IMb |
| Interferon-α | 4 (40.0) | 9 (50.0) | 0.879 |
| None | 6 (60.0) | 9 (50.0) | |
| Time period of IM
use (months)a | 59.5
(53.7–72.0) | 60.5
(52.1–75.3) | 0.901 |
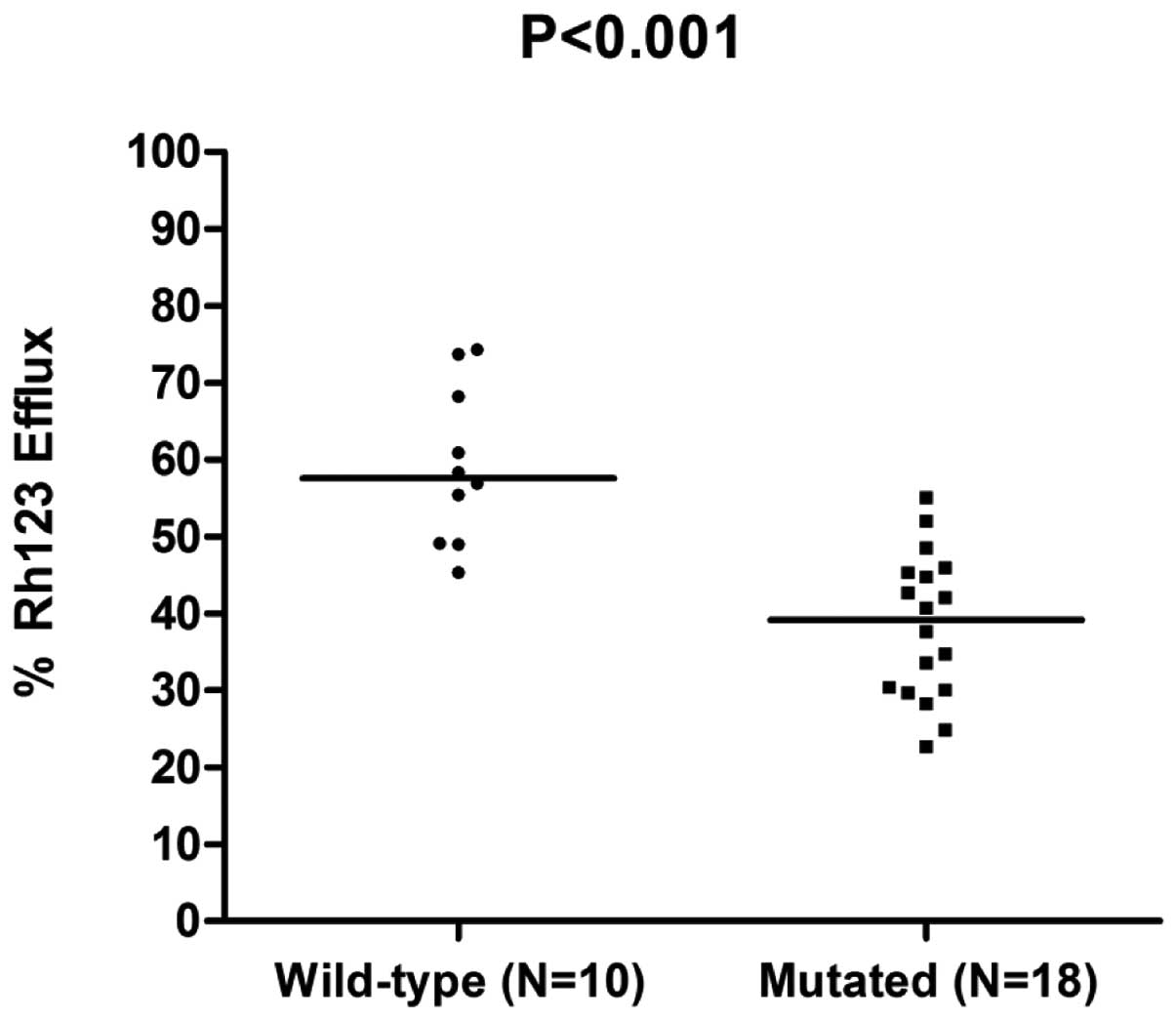
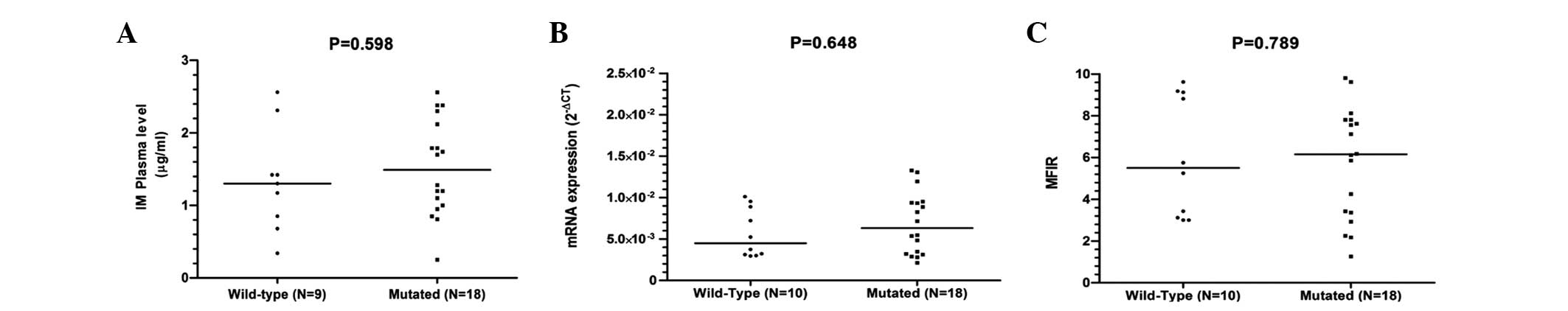
P-gp activity and IM response
The median Rh123 efflux in the wild-type and mutated
groups was 59.1 (range, 54.8–69.5) and 38.3 (range, 27.4–47.9),
respectively. A higher rate of P-gp activity was observed in
patients carrying the wild-type haplotype compared with those
carrying the mutated allele (P<0.001; Fig. 1). The different haplotypes showed no
influence on ABCB1 mRNA expression, P-gp expression and IM plasma
levels (Fig. 2).
A strong and direct correlation was identified
between ABCB1 mRNA expression and P-gp expression (r=0.747;
P=0.001). In addition, P-gp activity was found to positively and
moderately correlate with BCR-ABL1 transcript levels
(r=0.570; P=0.001), whereas SLC22A1 mRNA expression was found to
negatively and moderately correlate with BCR-ABL1 transcript
levels (r=-0.407; P=0.032).
The patients who did not achieve MMR showed a higher
rate of efflux mediated by P-gp compared with those individuals who
achieved MMR (64.7 vs. 45.7%; P=0.001). Furthermore, the
individuals who achieved MMR and CMR had a higher median rate of
SLC22A1 mRNA expression when compared with individuals who did not
achieve MMR and CMR (P<0.05). All patients without MMR showed
effluxes of >60%. However, no association was found between P-gp
activity and CMR (Table II).
Additionally, patients without MMR exhibited lower plasma
concentrations of IM when compared with those who achieved MMR
(0.51 vs. 1.42 μg/ml; P=0.001). However, no association was
observed between the plasma concentrations of IM and CMR (Table II).
 | Table IICorrelations between P-gp activity,
ABCB1 and SLC22A1 mRNA expression, P-gp expression and IM plasma
levels in individuals with or without MMR and CMR. |
Table II
Correlations between P-gp activity,
ABCB1 and SLC22A1 mRNA expression, P-gp expression and IM plasma
levels in individuals with or without MMR and CMR.
| MMR | | CMR | |
|---|
|
| |
| |
|---|
| Yes (n=24) | No (n=4) | P-valueb | Yes (n=5) | No (n=23) | P-valueb |
|---|
| P-gp activity | 45.7
(32.7–57.2) | 64.7
(47.5–73.2) | 0.001 | 45.1
(29.1–59.3) | 46.0
(31.3–62.8) | 0.890 |
| ABCB1 mRNA | 5.31
(3.31–9.47) | 8.41
(4.41–9.27) | 0.205 | 8.33
(3.20–10.10) | 6.41
(2.11–9.12) | 0.447 |
| P-gp
expressiona | 6.0 (3.0–7.6) | 6.4 (2.3–8.1) | 0.989 | 6.6 (3.0–8.6) | 5.7 (2.3–9.0) | 0.713 |
| SLC22A1 mRNA | 0.95
(0.68–1.59) | 0.54
(0.43–0.82) | 0.042 | 1.80
(1.40–2.90) | 0.81
(0.40–1.10) | 0.001 |
| IM plasma levels,
μg/ml | 1.42
(1.11–2.12) | 0.51
(0.27–1.01) | 0.001 | 1.56
(1.25–1.73) | 1.28
(0.85–2.30) | 0.753 |
Discussion
The ABCB1 c.1236C>T, c.3435C>T and
c.2677G>T/A polymorphisms have been associated with cancer risk,
as well as the variability of response to chemotherapy treatments
(24,25). It has been previously demonstrated
that the three polymorphisms are in strong linkage disequilibrium.
Considering the various haplotypes of ABCB1 with
c.1236C>T, c.3435C>T and c.2677G>T/A polymorphisms, it has
been reported that ~60% of the population, regardless of ethnicity,
carry at least one of the following three haplotypes:
1236CC/3435CC/2677GG, 1236CT/3435CT/2677GT and 1236TT/3435TT/2677TT
(26).
Dulucq et al (27) previously observed that CML patients
treated with a standard dose of IM (400 mg/day) and who were
carriers of the 1236C/3435C/2677G haplotype achieved MMR less often
than patients carrying other haplotypes (44.6 vs. 70%). In
addition, the authors demonstrated that the 1236T/3435T/2677T
haplotype was associated with MMR and serum concentrations of IM
>1.0 μg/ml.
In the present study, patients who did not achieve
MMR were observed to exhibit a higher P-gp retention (measured by
Rh123 efflux), which was associated with the wild-type haplotype
(1236CC/3435CC/2677GG). Previous studies have also associated P-gp
activity with the ABCB1 haplotypes (12,14)
and, subsequently, the 1236CC/3435CC/2677GG haplotype has been
associated with failure of treatment with antiepileptic drugs
(28). An additional study that
investigated patients with various types of cancer, including CML,
demonstrated that the rate of elimination of the P-gp substrate,
sestamibi (99mTc), was higher in individuals who carried the
3435CC/2677GG haplotype, suggesting a higher P-gp activity in such
patients (29). Other studies have
shown that subjects with the 1236TT/3435TT/2677TT haplotype have a
higher plasma concentration of digoxin, simvastatin, atorvastatin
and anthracycline compared with subjects carrying the other
haplotypes (30–33). Recently, the 1236T/3435T/2677T
haplotype has been associated with an improved response to
treatment with anthracyclines in patients with breast cancer
(33). In a previous study, an
increased serum concentration of digoxin was found in 195 patients
with congestive heart failure carrying the 1236TT/3435TT/2677TT
haplotype (30). Furthermore, a
comparable effect was observed in Chinese patients treated with
digoxin (32). Keskitalo et
al (31) also showed that
individuals carrying the 1236T/3435T/2677T haplotype had a higher
plasma concentration of simvastatin and atorvastatin.
By contrast, Kim et al (34) showed that carriers of the
1236CC/3435CC/2677GG haplotype exhibited ~40% higher area under the
plasma level-time curve values for fexofenadine compared with
individuals carrying the heterozygous and mutated haplotypes.
However, other studies have found no correlation between the
c.1236C>T, c.3435C>T and c.2677G>T/A polymorphisms and the
pharmacokinetics of aliskiren, methadone, nortriptyline, docetaxel
and paclitaxel (35–37).
These contrasting results suggest that the influence
of P-gp transport may be specific for each substrate. To date, the
mechanisms involving the drug structure and the interaction with
P-gp have not yet been elucidated. Furthermore, the majority of
studies have evaluated their results according to the associations
observed between the phenotype and genotypes of the c.1236C>T,
c. 3435C>T and c.2677G>T/A polymorphisms. However, these
studies have not performed P-gp activity tests to confirm whether
these genotypes are associated with changes in the rate of the P-gp
efflux pump or whether the transporter alone is involved in the
response or change in drug concentration.
The results of the current study are consistent with
results previously presented by Dulucq et al (27), and Vivona et al (15) revealed an association between the
presence of at least one mutant allele in the three previously
described polymorphisms and MMR. The lower efflux mediated by the
ABCB1 haplotypes suggests that reduced P-gp activity is associated
with higher IM intracellular concentrations, which is likely to
result in MMR.
IM plasma levels may affect the response to this
drug and, subsequently, it has been suggested that the IM
concentration of 1.0 μg/ml is optimal for achieving MMR (38–40).
Notably, in the present study, patients who achieved MMR had higher
IM plasma concentrations compared with those without MMR (1.42 vs.
0.51 μg/ml); however, no association was observed between the IM
plasma levels and CMR. In addition, all patients included in the
present study achieved CCyR, even with IM concentrations <1.0
μg/ml. These results are similar to those of two previous studies
in which no correlation was identified between the IM plasma
concentration and CCyR (39,40).
Conflicting results regarding the association of the
c.1236C>T, c.3435C>T and c.2677G>T/A polymorphisms with
the elimination of IM, as measured by renal clearance, have been
observed in certain previous studies (40–42). A
study conducted on 34 CML patients that evaluated the effect of the
ABCB1 c.3435C>T polymorphism on IM pharmacokinetics
showed that individuals carrying the 3435CC genotype had a higher
renal clearance of IM than individuals carrying the 3435CT and
3435TT genotypes (41). By
contrast, an additional study on 22 CML patients showed that
carriers of the 1236TT/3435TT/2677TT haplotype had a higher renal
clearance of IM compared with patients carrying the other
haplotypes (42). However, in this
study, only four patients were carriers of the 1236TT/3435TT/2677TT
haplotype. In the present study, no correlation was found between
the 1236CC/3435CC/2677GG, 1236CT/3435CT/2677GT and
1236TT/3435TT/2677TT haplotypes and IM plasma concentration. These
results are consistent with an additional study that found no
correlation between the c.1236C>T, c.3435C>T and
c.2677G>T/A polymorphisms and IM plasma levels (40). These results suggest the requirement
for further studies with a larger number of individuals to
characterize the correlations between c.1236C>T, c.3435C>T
and c.2677G>T/A polymorphisms and the pharmacokinetics of
IM.
Previous studies analyzing the manner in which the
c.1236C>T, c.3435C>T and c.2677G>T/A polymorphisms alter
the interaction between P-gp and its substrates are limited.
Several studies have shown that each substrate can interact with
different binding sites of P-gp (43,44);
however, it is difficult to determine in advance which binding
sites are important for each drug class. Fung and Gottesman
(12) used the UIC2 monoclonal
antibody directed against the extracellular epitope of P-gp in
vitro and demonstrated that the conformation of the wild-type
haplotype for the c.1236C>T, c.3435C>T and c.2677G>T/A
polymorphisms is different from that of the mutated haplotypes.
This change was demonstrated to be dependent on the presence of the
c.3435C>T polymorphism in the haplotype. This study suggested
that synonymous mutations at the ABCB1 haplotype produce a subtle
change in the substrate binding site.
The changes in protein function caused by synonymous
ABCB1 polymorphisms may not be explained by the amino acid
sequence of the protein. However, the in vitro and in
vivo observations from previous studies suggest that the
c.3435C>T polymorphism affects protein folding and function
(13,45) when it appears in a haplotype with
the c.1236C>T and c.2677G>T/A polymorphisms. Tsai et
al (46) suggested that the
synonymous c.3435C>T polymorphism causes the ribosome to pause
in the reading of codons, which subsequently affects protein
translation.
In the present study, the reduced P-gp activity in
patients carrying the heterozygous and mutated haplotypes compared
with those carrying the wild-type haplotype may be explained by a
possible conformational change in the carrier, but not by changes
in the expression of the ABCB1 mRNA or P-gp expression. This
modification leads to a decreased efflux of IM, which changes the
intracellular concentration of IM. The results of the present study
suggest that changes in the intracellular concentration may be
crucial for MMR, although all patients included achieved complete
hematologic response and CCyR. The achievement of molecular
responses appears to be a complex process, which is dependent on
higher intracellular concentrations of IM and altered
pharmacokinetics associated with low SLC22A1 mRNA expression and
hOCT1 activity. Additionally, increased efflux associated with the
presence of the ABCB11236CC/3435CC/2677GG haplotype may
substantially impact the molecular response to IM treatment.
The aim of the present study was to assess the
expression of SLC22A1 mRNA in order to evaluate the possible
combined action of SLC22A1 with P-gp activity. A higher expression
of SLC22A1 mRNA was observed in patients with MMR and CMR compared
with those without molecular response. The results are consistent
with the results of a previous study that found higher levels of
SLC22A1 transcripts in patients with MMR and CMR following
six years of IM treatment (39).
In conclusion, the present study demonstrated that
the ABCB1 1236CT/3435CT/2677GT and 1236TT/3435TT/2677TT
haplotypes are associated with lower P-gp activity and MMR in
chronic-phase CML patients treated with a standard dose of IM (400
mg/day). However, additional factors, such as other pharmacokinetic
and genetic polymorphisms in the ABCB1 and SLC22A1 genes, and the
expression of metabolizing enzymes (such as CYP3A4 and CYP3A5) and
other carriers (for example SLCO1A2 and ABCA3), may interact and
explain the variability of the IM response. Prospective studies
involving larger numbers of patients and numerous pharmacogenetic
markers are required to definitively elucidate the influence of
these factors on the pharmacokinetics of IM.
Acknowledgements
The present study was supported financially by the
São Paulo Research Foundation, Brazil (grant no. 09/54184-0) and
the National Council for Scientific and Technological Development,
Brazil. The authors would also like to thank all patients who
participated in the present study. The abstract was presented at
the American Society of Hematology meeting (ASH 2013) and published
as Poster 604. Molecular Pharmacology, Drug Resistance: Poster III
in Blood 122: 2013.
References
|
1
|
Thanopoulou E and Judson I: The safety
profile of imatinib in CML and GIST: long-term considerations. Arch
Toxicol. 86:1–12. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Druker BJ and Lydon NB: Lessons learned
from the development of an abl tyrosine kinase inhibitor for
chronic myelogenous leukemia. J Clin Invest. 105:3–7. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deininger MOBS, Guilhot F, Goldman JM,
Hochhaus A, Hughes TP, Radich JP, Hatfield AK, Mone M, Filian J,
Reynolds J, Gathmann I, Larson RA and Druker BJ: International
randomized study of interferon vs STI571 (IRIS) 8-year follow up:
sustained survival and low risk for progression or events in
patients with newly diagnosed chronic myeloid leukemia in chronic
phase (CML-CP) treated with imatinib. Blood (ASH Annual Meeting
Abstracts). 114:4622009.
|
|
4
|
Branford S, Rudzki Z, Walsh S, et al: High
frequency of point mutations clustered within the adenosine
triphosphate-binding region of BCR/ABL in patients with chronic
myeloid leukemia or Ph-positive acute lymphoblastic leukemia who
develop imatinib (STI571) resistance. Blood. 99:3472–3475. 2002.
View Article : Google Scholar
|
|
5
|
Eechoute K, Sparreboom A, Burger H, et al:
Drug transporters and imatinib treatment: implications for clinical
practice. Clin Cancer Res. 17:406–415. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hegedus T, Orfi L, Seprodi A, Váradi A,
Sarkadi B and Kéri G: Interaction of tyrosine kinase inhibitors
with the human multidrug transporter proteins, MDR1 and MRP1.
Biochim Biophys Acta. 1587:318–325. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hamada A, Miyano H, Watanabe H and Saito
H: Interaction of imatinib mesilate with human P-glycoprotein. J
Pharmacol Exp Ther. 307:824–828. 2003. View Article : Google Scholar
|
|
8
|
Thomas J, Wang L, Clark RE and Pirmohamed
M: Active transport of imatinib into and out of cells: implications
for drug resistance. Blood. 104:3739–3745. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Callen DF, Baker E, Simmers RN, Seshadri R
and Roninson IB: Localization of the human multiple-drug resistance
gene, MDR1, to 7q21.1. Human Genet. 77:142–144. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bodor M, Kelly EJ and Ho RJ:
Characterization of the human MDR1 gene. AAPS J. 7:E1–E5. 2005.
View Article : Google Scholar
|
|
11
|
Fletcher JI, Haber M, Henderson MJ and
Norris MD: ABC transporters in cancer: more than just drug efflux
pumps. Nat Rev Cancer. 10:147–156. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fung KL and Gottesman MM: A synonymous
polymorphism in a common MDR1 (ABCB1) haplotype shapes protein
function. Biochim Biophys Acta. 1794:860–871. 2009. View Article : Google Scholar
|
|
13
|
Kimchi-Sarfaty C, Marple AH, Shinar S, et
al: Ethnicity-related polymorphisms and haplotypes in the human
ABCB1 gene. Pharmacogenomics. 8:29–39. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kimchi-Sarfaty C, Oh JM, Kim IW, et al: A
‘silent’ polymorphism in the MDR1 gene changes substrate
specificity. Science. 315:525–528. 2007.
|
|
15
|
Vivona D, Bueno CT, Lima LT, et al: ABCB1
haplotype is associated with major molecular response in chronic
myeloid leukemia patients treated with standard-dose of imatinib.
Blood Cells Mol Dis. 48:132–136. 2012. View Article : Google Scholar
|
|
16
|
Rodrigues AC, Rebecchi IM, Bertolami MC,
Faludi AA, Hirata MH and Hirata RD: High baseline serum total and
LDL cholesterol levels are associated with MDR1 haplotypes in
Brazilian hypercholesterolemic individuals of European descent.
Braz J Med Biol Res. 38:1389–1397. 2005. View Article : Google Scholar
|
|
17
|
Cascorbi I, Gerloff T, Johne A, et al:
Frequency of single nucleotide polymorphisms in the P-glycoprotein
drug transporter MDR1 gene in white subjects. Clin Pharmacol Ther.
69:169–174. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Branford S and Hughes T: Diagnosis and
monitoring of chronic myeloid leukemia by qualitative and
quantitative RT-PCR. Methods Mol Med. 125:69–92. 2006.PubMed/NCBI
|
|
19
|
Vandesompele J, De Preter K, Pattyn F, et
al: Accurate normalization of real-time quantitative RT-PCR data by
geometric averaging of multiple internal control genes. Genome
Biol. 3:RESEARCH00342002. View Article : Google Scholar
|
|
20
|
Albermann N, Schmitz-Winnenthal FH,
Z’graggen K, et al: Expression of the drug transporters MDR1/ABCB1,
MRP1/ABCC1, MRP2/ABCC2, BCRP/ABCG2, and PXR in peripheral blood
mononuclear cells and their relationship with the expression in
intestine and liver. Biochem Pharmacol. 70:949–958. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rodrigues AC, Curi R, Britto LR, et al:
Down-regulation of ABCB1 transporter by atorvastatin in a human
hepatoma cell line and in human peripheral blood mononuclear cells.
Biochim Biophys Acta. 1760:1866–1873. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Larson RA, Druker BJ, Guilhot F, et al:
Imatinib pharmacokinetics and its correlation with response and
safety in chronic-phase chronic myeloid leukemia: a subanalysis of
the IRIS study. Blood. 111:4022–4028. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ajimura TO, Borges KB, Ferreira AF, de
Castro FA and de Gaitani CM: Capillary electrophoresis method for
plasmatic determination of imatinib mesylate in chronic myeloid
leukemia patients. Electrophoresis. 32:1885–1892. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jamroziak K, Młynarski W, Balcerczak E, et
al: Functional C3435T polymorphism of MDR1 gene: an impact on
genetic susceptibility and clinical outcome of childhood acute
lymphoblastic leukemia. Eur J Haematol. 72:314–321. 2004.
View Article : Google Scholar
|
|
25
|
Shitara K, Matsuo K, Ito S, et al: Effects
of genetic polymorphisms in the ABCB1 gene on clinical outcomes in
patients with gastric cancer treated by second-line chemotherapy.
Asian Pac J Cancer Prev. 11:447–452. 2010.
|
|
26
|
Deenen MJ, Cats A, Beijnen JH and
Schellens JH: Part 2: pharmacogenetic variability in drug transport
and phase I anticancer drug metabolism. Oncologist. 16:820–834.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dulucq S, Bouchet S, Turcq B, et al:
Multidrug resistance gene (MDR1) polymorphisms are associated with
major molecular responses to standard-dose imatinib in chronic
myeloid leukemia. Blood. 112:2024–2027. 2008. View Article : Google Scholar
|
|
28
|
Hung CC, Tai JJ, Lin CJ, Lee MJ and Liou
HH: Complex haplotypic effects of the ABCB1 gene on epilepsy
treatment response. Pharmacogenomics. 6:411–417. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wong M, Evans S, Rivory LP, et al: Hepatic
technetium Tc 99m-labeled sestamibi elimination rate and ABCB1
(MDR1) genotype as indicators of ABCB1 (P-glycoprotein) activity in
patients with cancer. Clin Pharmacol Ther. 77:33–42. 2005.
View Article : Google Scholar
|
|
30
|
Aarnoudse AJ, Dieleman JP, Visser LE, et
al: Common ATP-binding cassette B1 variants are associated with
increased digoxin serum concentration. Pharmacogenet Genomics.
18:299–305. 2008. View Article : Google Scholar
|
|
31
|
Keskitalo JE, Kurkinen KJ, Neuvoneni PJ
and Niemi M: ABCB1 haplotypes differentially affect the
pharmacokinetics of the acid and lactone forms of simvastatin and
atorvastatin. Clin Pharmacol Ther. 84:457–461. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Xu P, Jiang ZP, Zhang BK, Tu JY and Li HD:
Impact of MDR1 haplotypes derived from C1236T, G2677T/A and C3435T
on the pharmacokinetics of single-dose oral digoxin in healthy
Chinese volunteers. Pharmacology. 82:221–227. 2008. View Article : Google Scholar
|
|
33
|
Wu H, Kang H, Liu Y, et al: Roles of ABCB1
gene polymorphisms and haplotype in susceptibility to breast
carcinoma risk and clinical outcomes. J Cancer Res Clin Oncol.
138:1449–1462. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kim RB, Leake BF, Choo EF, et al:
Identification of functionally variant MDR1 alleles among European
Americans and African Americans. Clin Pharmacol Ther. 70:189–199.
2001. View Article : Google Scholar
|
|
35
|
Tapaninen T, Neuvonen PJ and Niemi M:
Effect of ABCB1 haplotypes on the pharmacokinetics and
renin-inhibiting effect of aliskiren. Eur J Clin Pharmacol.
66:865–870. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Jensen BP, Roberts RL, Vyas R, Bonke G,
Jardine DL and Begg EJ: Influence of ABCB1 (P-glycoprotein)
haplotypes on nortriptyline pharmacokinetics and
nortriptyline-induced postural hypotension in healthy volunteers.
Br J Clin Pharmacol. 73:619–628. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Marsh S, Paul J, King CR, Gifford G,
McLeod HL and Brown R: Pharmacogenetic assessment of toxicity and
outcome after platinum plus taxane chemotherapy in ovarian cancer:
the Scottish Randomised Trial in Ovarian Cancer. J Clin Oncol.
25:4528–4535. 2007. View Article : Google Scholar
|
|
38
|
Picard S, Titier K, Etienne G, et al:
Trough imatinib plasma levels are associated with both cytogenetic
and molecular responses to standard-dose imatinib in chronic
myeloid leukemia. Blood. 109:3496–3499. 2007. View Article : Google Scholar
|
|
39
|
Marin D, Bazeos A, Mahon FX, et al:
Adherence is the critical factor for achieving molecular responses
in patients with chronic myeloid leukemia who achieve complete
cytogenetic responses on imatinib. J Clin Oncol. 28:2381–2388.
2010. View Article : Google Scholar
|
|
40
|
Takahashi N, Wakita H, Miura M, et al:
Correlation between imatinib pharmacokinetics and clinical response
in Japanese patients with chronic-phase chronic myeloid leukemia.
Clin Pharmacol Ther. 88:809–813. 2010. View Article : Google Scholar
|
|
41
|
Yamakawa Y, Hamada A, Nakashima R, et al:
Association of genetic polymorphisms in the influx transporter
SLCO1B3 and the efflux transporter ABCB1 with imatinib
pharmacokinetics in patients with chronic myeloid leukemia. Ther
Drug Monit. 33:244–250. 2011.PubMed/NCBI
|
|
42
|
Gurney H, Wong M, Balleine RL, et al:
Imatinib disposition and ABCB1 (MDR1, P-glycoprotein) genotype.
Clin Pharmacol Ther. 82:33–40. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Dey S: Single nucleotide polymorphisms in
human P-glycoprotein: its impact on drug delivery and disposition.
Expert Opin Drug Deliv. 3:23–35. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Rautio J, Humphreys JE, Webster LO, et al:
In vitro p-glycoprotein inhibition assays for assessment of
clinical drug interaction potential of new drug candidates: a
recommendation for probe substrates. Drug Metab Dispos. 34:786–792.
2006. View Article : Google Scholar
|
|
45
|
Hoffmeyer S, Burk O, von Richter O, et al:
Functional polymorphisms of the human multidrug-resistance gene:
multiple sequence variations and correlation of one allele with
P-glycoprotein expression and activity in vivo. Proc Natl Acad Sci
USA. 97:3473–3478. 2000. View Article : Google Scholar
|
|
46
|
Tsai CJ, Sauna ZE, Kimchi-Sarfaty C,
Ambudkar SV, Gottesman MM and Nussinov R: Synonymous mutations and
ribosome stalling can lead to altered folding pathways and distinct
minima. J Mol Biol. 383:281–291. 2008. View Article : Google Scholar : PubMed/NCBI
|