Introduction
Although the occurrence of nasopharyngeal carcinoma
(NPC) is rare in the Western hemisphere, it is a common malignancy
in Southern China (1,2). Compared with other head and neck
squamous cell carcinomas, NPC is associated with the highest rates
of regional lymph node and distant metastasis (3). The most common site of metastasis is
the cervical lymph nodes (4), and
the majority of NPCs have already metastasized at the point of
diagnosis. Radiotherapy is considered to be the predominant regimen
for the treatment of almost all NPC cases, with a five-year overall
survival (OS) rate of 87–96% for stage I-II and 67–77% for stage
III-IVB (5). However, local
recurrence remains the major cause of treatment failure following
conventional radiotherapy, and distant metastasis is often observed
following conventional treatment. Although NPC is known for its
high rate of metastasis, metastasis to the breast is extremely
rarely and, to the best of our knowledge, only four well-documented
cases have been reported in the literature to date. The four female
cases include two cases reported in 1991, one case reported in
2004, which was one of 15 cases of extramammary breast metastases,
and a case that was reported in 2007 (6–8). Thus
far, no male cases of breast metastasis from NPC have been
reported. Therefore, to the best of our knowledge, the current
study reports the first case of male breast metastasis from
NPC.
Case report
A 49-year-old male presented to Qianfoshan hospital
affiliated to Shandong University (Jinan, China) in August 2009
with a lump in the right upper neck region, which had been growing
for four months. Physical examination identified multiple circular
lumps, which were palpable on the right upper third of the neck on
the sternocleidomastoid (facies medialis). The largest lump,
measuring 5×4 cm, had a hard texture and was adhered to the
surrounding tissue. In the right supraclavicular fossa, multiple
active bilateral nodes with a hard texture were identified.
Fiberoptic nasopharyngoscopy revealed lifting the right side of the
tonsillar crypts and the surface was rough (fiberoptic instruments:
OTVS7PRO, CLVS4OPRO and OTV-StPro; Laryngoscopic lens, ENF-VQ
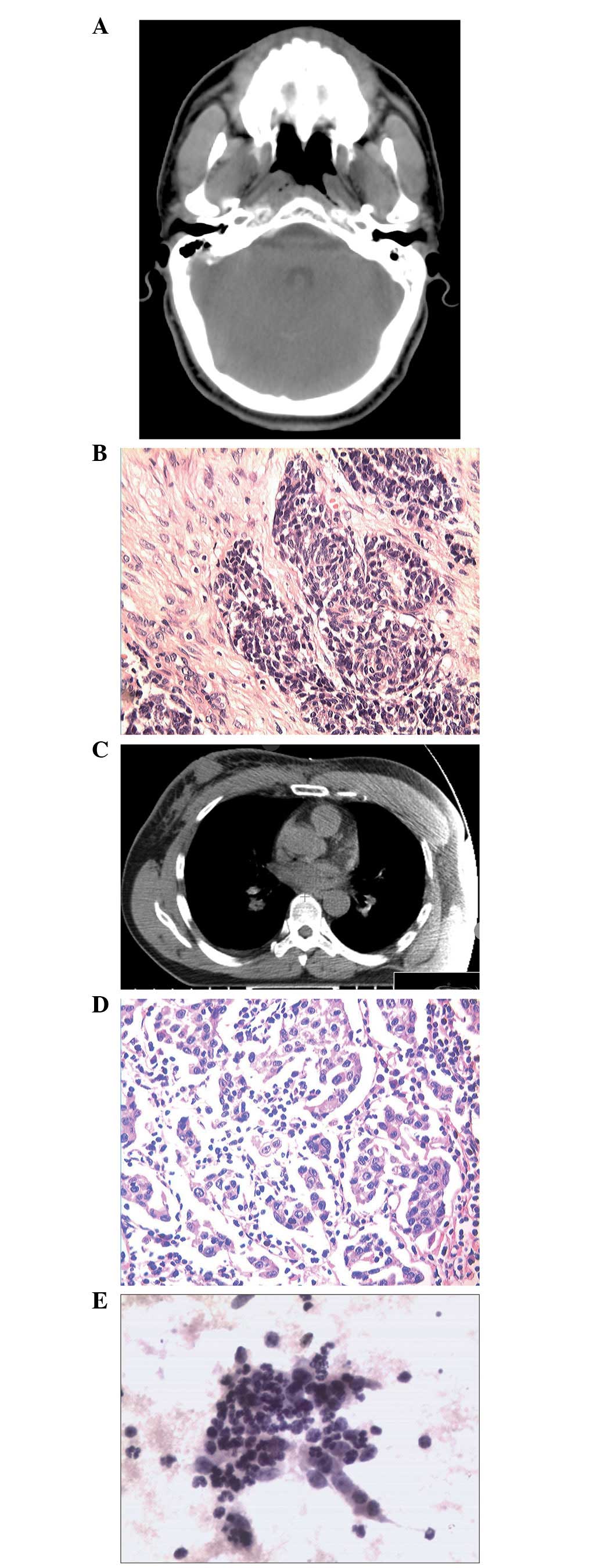
2440288, Olympus Corporation, Tokyo, Japan). Examination of the
head and neck by computed tomography (CT) showed thickening of the
soft tissues of the right wall of the nasopharynx (Fig. 1A) and bilateral cervical
lymphadenopathy with a maximum node size of ~2.9×1.3 cm.
Histopathological examination [hemotoxylin and eosin (H&E),
Beijing Solarbio Science & Technology Co., Ltd., Beijing,
China] of the nasopharynx specimen, viewed under a microscope
(IX71, Olympus Corporation) confirmed the diagnosis of
undifferentiated squamous cell carcinoma (Fig. 1B) at stage T3N3M0 (9). The patient provided written informed
consent.
In the present case. the treatment strategy for the
patient involved 3D-conformal radiotherapy of the nasopharynx and
cervical lymph nodes (total dose, 70 Gy) concurrent with three
cycles of docetaxel/nedaplatin chemotherapy. However, in April
2011, the patient presented with multiple lymph nodes that were
tumefied in the two sides of the axillary, generally without fever
or pain, although pain was experienced during heavy manual labor.
Five months later, the patient identified a mass developing in the
right breast. Physical examination confirmed the mass in the right
breast and revealed lymphadenopathy on two sides of the axillary.
Ultrasonic examination showed thick gland-like tissues behind the
right nipple. Chest CT revealed that local tissues of the right
chest wall were thickened (Fig. 1C)
and also revealed multiple tumid lymph nodes on two sides of the
axillary. Histopathological examination (H&E staining) of the
right axillary lymph nodes revealed poorly differentiated
metastatic squamous carcinoma (Fig.
1D) and breast fine needle aspiration confirmed an abundance of
metastatic squamous cells within the thickened tissue (Fig. 1E). In addition, immunohistochemical
analysis revealed the apparent expression of cytokeratin (CK)
5/6(+), CK7(−), CK20(−), estrogen receptor(−), thyroid
transcription factor 1(−), gross cystic disease fluid protein-15(−)
and villin(−). In November 2011, the patient was administered a
total dose of 50 Gy palliative radiotherapy to the right axillary
and breast in combination with docetaxel plus 5-fluorouracil (FU)
and cisplatin chemotherapy for four cycles. In May 2012, the neck
and chest CT examination revealed no increase of lymphadenopathy on
the two sides of the axillary compared with the previous CT
examinations.
Discussion
NPC is a malignancy endemic to South China with an
annual incidence of between 10 and 50 per 100,000 individuals
(1), with a tendency to occur in
young and middle-aged adults. In contrast to other head and neck
tumors, NPC is curable despite regional lymph node spread. Although
histologically the common subtypes of NPC are non-keratinizing,
keratinizing and undifferentiated, the majority of NPC are
undifferentiated. Similar to other head and neck squamous cell
carcinomas, NPC is known for its high rate of lymph node
metastasis. Due to its presentation below the nasopharyngeal
mucosa, which is rich in lymphatics, a lymphatic network
subsequently results in lymphatic drainage to the cervical lymph
nodes. Therefore, the appearance of cervical lymph node metastases
in early NPC is common.
NPC is notably sensitive to chemotherapy and
radiotherapy, however, due to anatomical restrictions and
radiosensitivity, definitive radiotherapy is regarded as the
standard treatment despite the poor response of locoregionally
advanced NPC (5). In a previous
intergroup 0099 study, concurrent chemoradiotherapy plus adjuvant
chemotherapy achieved a 31% increase in three-year OS (10), thus, the authors considered this
regimen to be the standard care for advanced NPC. Recently, a phase
three multicenter randomized controlled trial revealed that
adjuvant cisplatin and FU chemotherapy did not significantly
improve failure-free survival in locoregionally advanced NPC
following concurrent chemoradiotherapy (11). This result lead the authors to
conclude that adjuvant chemotherapy must not be administered
following concurrent chemotherapy in patients with locally advanced
NPC. Lymphatic metastasis to the cervical lymph nodes is most
commonly observed and is a major factor associated with prognosis
and treatment outcomes (5).
Considering the predominance of cervical lymph node metastasis in
NPC, irradiation is commonly administered to the entire neck region
in an attempt to control regional recurrence. However, despite the
administration of conventional radiotherapy to the irradiation
field, including the common sites of local recurrence (such as the
clivus and ethmoid), the incidence of distant metastasis following
treatment is high. Furthermore, retrospective analysis of the
clinical outcomes and patterns of treatment failure for NPC with
distant metastasis following intensity-modulated radiation therapy
remains challenging (12).
Nevertheless, distant metastasis to the breast from NPC is rare, as
breast metastasis usually occurs as a result of a disseminated
disease that is indicated by extramammary neoplasms (13). In the current study, two years
following the initial treatment the patient received definitive
treatment due to the first presentation of axillary lymph node
metastasis, which was followed a few months later by tumefaction of
the right breast. The tumefaction indicated that the NPC had
metastasized to the breast, perhaps as a result of the axillary
lymph node metastasis. Although a search of the English literature
using PubMed retrieved four previously reported cases of breast
metastasis from NPC, all four cases were female and no male cases
had been reported. Therefore, the current study established that
NPC may also metastasize to the breast in males and highlights the
importance of breast examination in the follow-up of NPC
patients.
In patients with recurrent or distant metastatic
NPC, platinum-based chemotherapy is considered to be the preferred
regimen for first-line treatment (14). However, no standard strategy has
been established for local recurrence or metastasis. To prolong the
survival time of such patients, a series of studies have been
performed to identify effective and tolerable regimens. In a
previous phase II study of gemcitabine-vinorelbine chemotherapy in
metastatic NPC patients that were pretreated with platinum-based
chemotherapy (15), the overall
response rate was 37.7%, with an OS of 14.1 months and
progression-free survival (PFS) of 5.2 months. In addition, the
hematologic and non-hematologic toxicities were mild. Therefore,
the authors concluded that this strategy is effective and safe for
the treatment of such patients. In an additional phase II study of
ifosfamide in the treatment of recurrent NPC patients, 5-FU and
leucovorin was used as the second-line regimen. The one-year
survival rate of the patients was 51% and PFS was 6.5 months, in
addition, none of the patients developed grade 3/4 toxicities. In
the current report, nasopharyngeal examination of the patient did
not reveal local recurrence, but did establish distant metastasis.
Therefore, the patient was administrated docetaxel, cisplatin, 5-FU
and leucovorin combined with radiotherapy to control the distant
metastasis. Following radiotherapy and four cycles of chemotherapy,
the condition was evaluated and showed complete remission. Although
docetaxel plus platinum was used as the first-line regimen, a
docetaxel plus cisplatin combined 5-FU and leucovorin regimen with
concurrent radiotherapy achieved improved local control. Compared
with previous strategies, this treatment may be effective as a
second-line regimen to treat recurrent or distant metastasis.
Epidermal growth factor receptor (EGFR) overexpression has been
identified in ~85% NPCs, however, a previous phase II trial
(16) administered erlotinib, which
acts on EGFR, as a maintenance treatment in NPC patients with
recurrent and/or metastatic disease following a
gemcitabine-platinum regimen and revealed that the treatment was
not effective as a maintenance or second-line therapy following
chemotherapy. Further studies are required to identify whether, as
well as which, molecular targeted agents and strategies are
effective for recurrent or metastatic NPC.
In conclusion, the current report confirmed that NPC
may also metastasize to the breast in males. In addition, the high
rate of NPC metastasis demonstrated an urgent requirement for
identifying effective and safe strategies.
References
|
1
|
Luo J, Chia KS, Chia SE, et al: Secular
trends of nasopharyngeal carcinoma incidence in Singapore, Hong
Kong and Los Angeles Chinese populations, 1973–1997. Eur J
Epidemiol. 22:513–521. 2007.PubMed/NCBI
|
|
2
|
Jia WH, Huang QH, Liao J, et al: Trends in
incidence and mortality of nasopharyngeal carcinoma over a 20–25
year period (1978/1983–2002) in Sihui and Cangwu counties in
southern China. BMC Cancer. 6:1782006.PubMed/NCBI
|
|
3
|
Sham JS, Choy D and Wei WI: Nasopharyngeal
carcinoma: orderly neck node spread. Int J Radiat Oncol Biol Phys.
19:929–933. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ho FC, Tham IW, Earnest A, et al: Patterns
of regional lymph node metastasis of nasopharyngeal carcinoma: a
meta-analysis of clinical evidence. BMC Cancer. 12:982012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yi JL, Gao L, Huang XD, et al:
Nasopharyngeal carcinoma treated by radical radiotherapy alone:
ten-year experience of a single institution. Int J Radiat Oncol
Biol Phys. 65:161–168. 2006.
|
|
6
|
Sham JS and Choy D: Breast metastasis from
nasopharyngeal carcinoma. Eur J Surg Oncol. 17:91–93. 1991.
|
|
7
|
Yeh CN, Lin CH and Chen MF: Clinical and
ultrasonographic characteristics of breast metastases from
extramammary malignancies. Am Surg. 70:287–290. 2004.PubMed/NCBI
|
|
8
|
Driss M, Abid L, Mrad K, et al: Breast
metastases from undifferentiated nasopharyngeal carcinoma.
Pathologica. 99:428–430. 2007.PubMed/NCBI
|
|
9
|
Edge SB, Byrd DR, Compton CC, et al: AJCC
Cancer Staging Manual. 7th edition. Lippincott-Raven; Philadelphia,
PA, USA: 2009
|
|
10
|
Al-Sarraf M, LeBlanc M, Giri PG, et al:
Chemoradiotherapy versus radiotherapy in patients with advanced
nasopharyngeal cancer: phase III randomized intergroup study 0099.
J Clin Oncol. 16:1310–1317. 1998.
|
|
11
|
Chen L, Hu CS, Chen XZ, et al: Concurrent
chemoradiotherapy plus adjuvant chemotherapy versus concurrent
chemoradiotherapy alone in patients with locoregionally advanced
nasopharyngeal carcinoma: a phase 3 multicentre randomised
controlled trial. Lancet Oncol. 13:163–171. 2012. View Article : Google Scholar
|
|
12
|
Ng WT, Lee MC, Hung WM, et al: Clinical
outcomes and patterns of failure after intensity-modulated
radiotherapy for nasopharyngeal carcinoma. Int J Radiat Oncol Biol
Phys. 79:420–428. 2011. View Article : Google Scholar
|
|
13
|
Domanski HA: Metastases to the breast from
extramammary neoplasms. Acta Cytol. 40:1293–1300. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li YH, Wang FH, Jiang WQ, et al: Phase II
study of capecitabine and cisplatin combination as first-line
chemotherapy in Chinese patients with metastatic nasopharyngeal
carcinoma. Cancer Chemother Pharmacol. 62:539–544. 2008. View Article : Google Scholar
|
|
15
|
Chen C, Wang FH, Wang ZQ, et al: Salvage
gemcitabine-vinorelbine chemotherapy in patients with metastatic
nasopharyngeal carcinoma pretreated with platinum-based
chemotherapy. Oral Oncol. 48:1146–1151. 2012. View Article : Google Scholar
|
|
16
|
You B, Le Tourneau C, Chen EX, et al: A
Phase II trial of erlotinib as maintenance treatment after
gemcitabine plus platinum-based chemotherapy in patients with
recurrent and/or metastatic nasopharyngeal carcinoma. Am J Clin
Oncol. 35:255–260. 2012. View Article : Google Scholar
|