Introduction
Inflammatory pseudotumor is a benign, non-neoplastic
and tumor-like tissue mass (1).
Inflammatory pseudotumor affects both genders and all races, and
occurs in patients aged from 1 to 73 years (2,3).
Inflammatory pseudotumor mainly arises in the lung and the orbit,
but can occur in a variety of organs, including the thyroid,
pleura, liver, kidney, common bile ducts, spinal cord, testis,
scrotum and other soft tissues (4–7). To
the best of our knowledge, only one case of inflammatory
pseudotumor of the thymus has been reported in the literature to
date (8). Generally, due to the
complexity of the mediastinum, inflammatory pseudotumor of the
thymus is commonly confused with thymoma and difficult to diagnose,
particularly when it causes inflammation in the surrounding
organs.
This report presents a case of inflammatory
pseudotumor of the thymus, which caused bilateral reactive
pulmonary inflammation and pleural effusion. To the best of our
knowledge, this is the second case of inflammatory pseudotumor of
the thymus with reactive inflammation spreading to the lung. In
this study, we describe the diagnosis and treatment of the present
case, and discuss the potential factors contributing to the
development of pseudotumors. The patient provided written informed
consent.
Case report
A 54-year-old male was referred to The First
Hospital of Jilin University (Changchun, China) complaining of
chest pain and intermittent degrees of irregular fever, night
sweats, morning phlegm (without bleeding) and dysphagia for 12
days. The patient had visited a local clinic and received
anti-inflammation treatment one week earlier. Although his fever
had been temporarily resolved for two days, symptoms recurred three
days ago. The patient had no history of chronic disease, surgery,
regular smoking, exposure to occupation-related industry dust or
recent travel to other cities. The patient did not show obvious
weight loss and none of the patient’s family members had a history
of similar symptoms and signs.
Physical examination of the patient revealed the
following: Temperature, 38.5°C; heart rate, 75 beats per min;
respiration rate, 26 breaths per min; and blood pressure, 135/75
mmHg. Bilateral lymphadenopathy was detected in the neck, but not
in the axillary and inguinal lymph nodes. The left enlarged node
was ~8×3 mm in size, while the right enlarged node was ~9×3 mm in
size. The nodes had an intermediate degree of hardness and tension,
but without obvious pain in response to touch. The thorax appeared
symmetrical, the intercostal space was bilaterally normal and, on
auscultation, no abnormal breath sounds were observed.
Laboratory tests revealed no abnormal changes in
full blood counts, differential counts or the concentrations of
serum alkaline phosphatase, blood lipids, transaminase, urea
nitrogen and creatinine. The patient displayed negative responses
to the purified intermediate protein derivative of tuberculin.
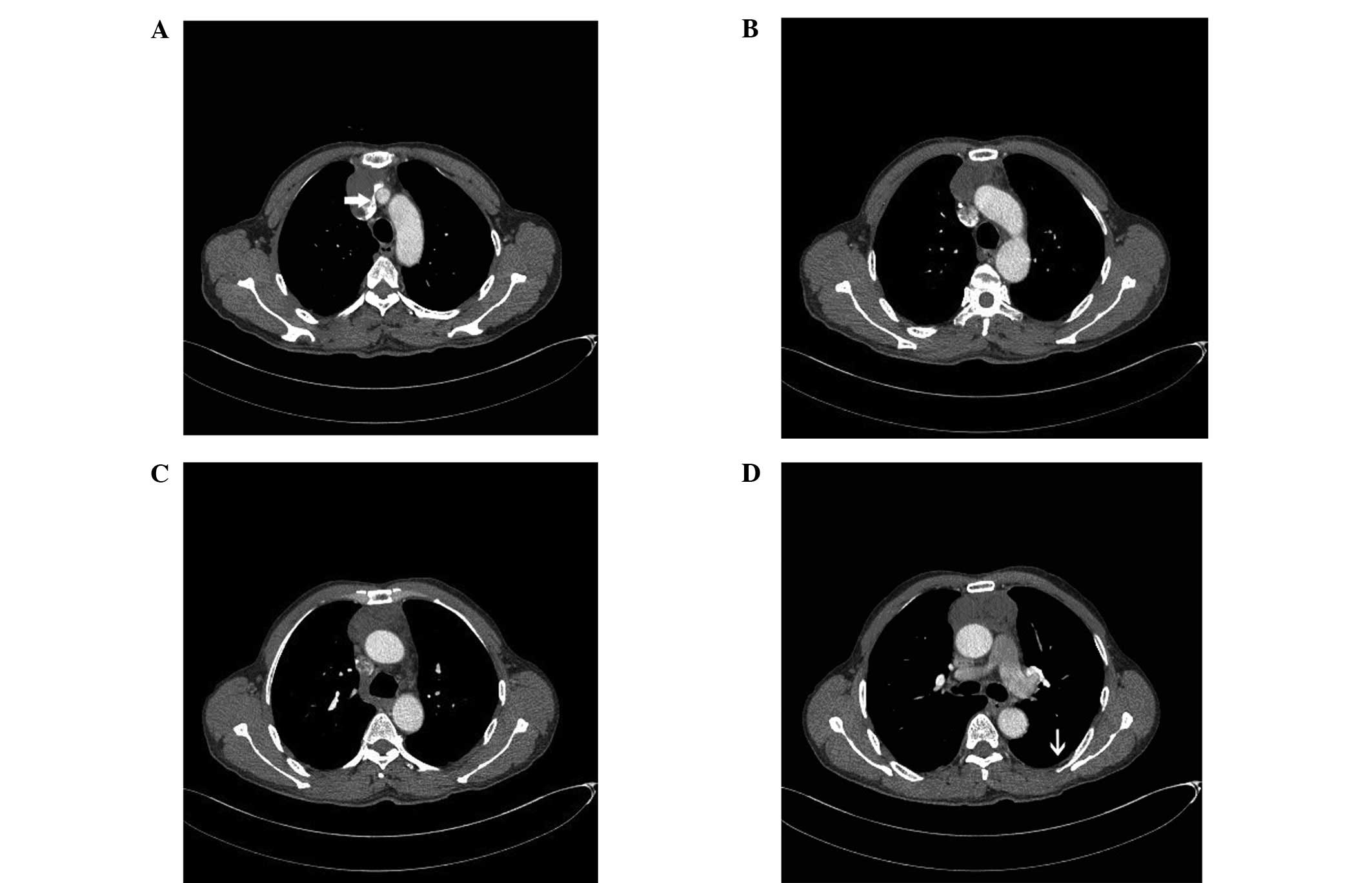
Enhanced computed tomography (CT) revealed an
anterior mediastinal irregular solid and cystic mass of ~8.3×6×3.5
cm (Fig. 1), extending posteriorly
towards the left innominate vein with heterogeneous enhancement.
This was accompanied by an unclear plane separating the mass from
the aorta and the superior vena cava, several inflammatory sites in
both sides of the lung and a trace of pleural effusion.
Accordingly, the patient was suspected to have a
thymoma, thymic carcinoma or teratoma. Given the diagnostic
uncertainty and the persistent symptoms, the patient was subjected
to a median sternotomy. This revealed an ~8.3×6×3.5 cm, hard,
well-circumscribed, irregular mass that almost replaced the whole
thymus, extending towards the thyroid and posteriorly to the
aortico-pulmonary window. The mass invaded the bilateral parietal
pleura, pericardium and adhered to the roots of the aorta and
superior vena cava. The mass was carefully freed from the left and
right mediastinal pleura, and the dorsal aspect of the tumor was
separated from the ascending aorta, superior vena cava and left
innominate vein, as the tumor was loosely adherent to these. The
entire tumor was resected with the bilateral mediastinal pleura and
part of the pericardium (Fig. 2A).
The mass appeared to be irregular in shape and was covered by a
light-yellow, thick fibrotic membrane-like tissue.
 | Figure 2Histological analysis of the mass. The
mass (8.3×6.0×3.5 cm) was surgically removed from the mediastinal
pleura and subjected to histological and immunohistochemical
analyses. Briefly, tissue sections were stained with H&E or
anti-CD68, -CD21, -MUM-1, -S-100, -CK or-CD1a overnight at 4°C. The
control sections were treated with the same isotype IgG or sera
from healthy animals. Subsequently, the bound antibodies were
detected with horseradish peroxidase-conjugated secondary
antibodies and visualized with 3,3′-diaminobenzidine. (A)
Photograph of the gross mass; (B) H&E staining of the tissue
section (magnification, ×200: scale bar, 50 μm). (C)
Immunohistochemical analysis of CD68, CD21, MUM-1, S-100 and CK
(magnification, ×100; scale bar, 20 μm), and CD1a (magnification,
×200; scale bar, 50 μm). Data are representative images and the
control sections show no specific staining (data not shown).
H&E, hematoxylin and eosin; CD, cluster of differentiation;
MUM, multiple myeloma oncogene; CK, cytokeratin. |
During surgery, the mass was considered to be a
thymoma or thymic carcinoma. However, histological examination
revealed that the tissue sections contained a number of necrotic
regions, connective tissue fiber hyperplasia, numerous inflammatory
cell infiltrates and an aggregation of foam cells (Fig. 2B). There were no obvious cell
characteristics of thymoma or thymic carcinoma. Immunohistochemical
analysis revealed that the tissue sections contained a number of
cluster of differentiation (CD)68+, multiple myeloma
oncogene (MUM)-1+, cytokeratin (CK)+ and
CD1a+ cells, but there was no detectable anti-S-100 or
anti-CD21 staining (Fig. 2C). These
findings, together with the inflammatory reactive responses in the
lung, aided the diagnosis of inflammatory pseudotumor of the
thymus.
The patient was treated postoperatively with 2 g
ceftezole sodium twice per day for seven days. Symptoms were
resolved and the patient was discharged from hospital without any
obvious complications. During the six-month follow-up period, the
patient did not experience fever, night-sweats or chest pain and
there was no evidence of relapse or lung inflammation.
Discussion
Inflammatory pseudotumor is a rare disease and is
characterized by the excess growth of inflammatory cells. The
majority of inflammatory pseudotumors occur in the lung, although
there have been cases in other organs, such as the thyroid, pleura,
gastrointestinal and central nerve systems, spinal cord, kidney,
testis, scrotum and other soft tissues (4–7).
Patients with an inflammatory pseudotumor commonly exhibit no
specific symptoms, and their clinical symptoms and signs are
dependent on the location and size. To the best of our knowledge,
this report describes the second case of inflammatory pseudotumor
of the thymus. The patient presented with low degrees of irregular
fever and night sweats, similar to those experienced in the
previous case (8). The patient also
complained of morning phlegm without bleeding, as well as
dysphagia, but these symptoms were not present in the previous case
(8). By contrast, the patient in
the present report did not experience myalgias or dyspnoea, as
observed in the previous case. Furthermore, the previous case had a
significantly elevated serum alkaline phosphatase level; however,
this was normal in the present case. This discrepancy may stem from
the severity of pulmonary reactive inflammation. Indeed, the
previous case had a large amount of yellow exudate in the pleura
and diverse inflammation in the lung, whereas our case only showed
marginal pleural effusion and mild pulmonary inflammation. Notably,
these clinical symptoms may occur in patients with several types of
upper respiratory infection and malignancies, such as the early
stage of pneumonia, tuberculosis and lung cancer. Therefore,
patients with an inflammatory pseudotumor of the thymus can present
with a variety of clinical symptoms, which may increase the
difficulty in diagnosing inflammatory pseudotumors in the clinic.
Physicians assessing patients with these symptoms should consider
the possibility of an inflammatory pseudotumor.
Epidemiological investigations have revealed that
inflammatory pseudotumors occur in male and female patients at a
variety of ages. A previous study showed that almost 25% of cases
with inflammatory pseudotumors are individuals <18 years of age
(9). The currently available cases
are distributed worldwide and there are no significant differences
in the geographic distribution. Although we should not exclude the
possibility of previous misdiagnosis, to the best of our knowledge,
this is the first case of inflammatory pseudotumor of the thymus to
be reported in China. Due to the nature of this rare disease,
currently there is no information regarding the prevalence and
incidence of inflammatory pseudotumor worldwide.
Inflammatory pseudotumors are difficult to diagnose
preoperatively and may present with various clinical and
radiological characteristics. The diagnosis of an inflammatory
pseudotumor is based on histopathological and immunohistochemical
examinations. Histological findings include acute and chronic
inflammatory infiltrates with varying degrees of fibrosis (5,10).
Radiological examination of the present case revealed a mediastinal
mass, multiple sites of pulmonary inflammation and pleural
effusion. Accordingly, our patient was wrongly diagnosed with
thymoma, thymic carcinoma or teratoma preoperatively. Thymoma is a
neoplasm in the anterior mediastinum and is frequently associated
with indolent growth and a variety of paraneoplastic syndromes,
such as myasthenia gravis. Thymomas appear to have malignant
potential and should be considered in the differential diagnosis of
a mediastinal mass (11,12). Histologically, thymoma usually
displays neoplastic epithelial cells with spindle- and/or
oval-shaped nuclei. Thymoma cells may also have a dendritic or
plump (epithelioid) appearance (13). Although our preoperative diagnosis
was understandable, the misdiagnosis may have been prevented by
considering the short disease period with no obvious systemic
deterioration and the multiple sites of mild pulmonary lesions.
Histologically, inflammatory pseudotumors are usually composed of
plasma cell granulomas, pulmonary xanthomas, xanthogranulomas,
xanthomatous pseudotumor, fibrous histocytomas, plasmacytoma and
others (5). The mass sections from
our case contained a number of necrotic regions, connective tissue
fiber hyperplasia, numerous inflammatory infiltrates and an
aggregation of foam cells, which is similar to the mass in the
previous case (8). There were no
obvious cell characteristics of thymoma or thymic carcinoma.
Notably, immunohistochemistry revealed that the tissue sections
contained a number of CD68+, MUM-1+, CK+ and CD1a+ cells, but there
was no detectable anti-S-100 or anti-CD21 staining. These findings
support the diagnosis of an inflammatory pseudotumor of the
thymus.
Currently, a complete surgical resection of the
inflammatory pseudotumor remains the best treatment. Other
non-surgical therapeutic modalities, such as radiotherapy,
chemotherapy and steroids, may be useful for individuals with an
incomplete surgical resection, multifocal disease, tumor recurrence
or contraindication to lung resection (14–16).
As the mediastinal mass was completely removed, anti-inflammatory
treatment was only provided for a short period. The patient
recovered soon after surgery without any surgical complications and
no recurrence or other relevant abnormalities were observed during
the six-month follow-up period. Our findings suggest that when the
inflammatory pseudotumor is completely removed by surgery, it may
be not necessary to use other tumor-related therapies.
The number of available studies regarding the
etiology of inflammatory pseudotumors is currently limited.
Previous studies have suggested that the development of an
inflammatory pseudotumor is non-specific in terms of inflammatory
reactions, autoimmune responses, trauma or paraneoplastic syndrome
(9,17,18).
In addition, infection may contribute to the development of an
inflammatory pseudotumor and these infectious micropathogens may
include influenza, measles, cytomegalovirus and other herpes
viruses, mycobacterium tuberculosis, syphilis, brucellosis and
Kawasaki disease. Although these infections may result in thymitis,
which is associated with the development of an inflammatory
pseudotumor of the thymus (8,19), the
present case showed no evidence of infection with any of these
micropathogens. However, we should not exclude the possibility of
unknown endogenous or exogenous viral infection in our patient.
In summary, this report describes a case of
inflammatory pseudotumor of the thymus. The patient displayed no
specific clinical symptoms or signs and an enhanced CT scan
revealed a mediastinal mass and multiple sites of mild pulmonary
inflammation. The patient also exhibited marginal pleural effusion,
which led to the confusion with thymoma and other solid tumors in
the thymus. However, histological and immunohistochemical analysis
provided evidence of inflammation, but not neoplastic changes in
the thymus sections, and surgical resection of the full mass
resulted in a resolution of clinical symptoms and reactive
pulmonary responses. Therefore, we propose that physicians should
consider an inflammatory pseudotumor when a patient presents with
unexplained fever, night sweats and chest pain.
References
|
1
|
Alexiou C, Obuszko Z, Beggs D and Morgan
WE: Inflammatory pseudotumors of the lung. Ann Thorac Surg.
66:948–950. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gorospe L, Fernández-Gil MA, Torres I,
Tovar J, García-Miguel P and Tejerina E: Misleading lead:
inflammatory pseudotumor of the mediastinum with digital clubbing.
Med Pediatr Oncol. 35:484–487. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Topçu S, Taştepe I, Alper A, et al:
Inflammatory pseudotumors of the lung: a clinical study of eleven
patients. J Thorac Cardiovasc Surg. 119:180–182. 2000.
|
|
4
|
Kim JH, Cho JH, Park MS, et al: Pulmonary
inflammatory pseudotumor: a report of 28 cases. Korean J Intern
Med. 17:252–258. 2002.PubMed/NCBI
|
|
5
|
Narla LD, Newman B, Spottswood SS, Narla S
and Kolli R: Inflammatory pseudotumor. Radiographics. 23:719–729.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Loeffler-Ragg J, Bodner J, Freund M,
Steurer M, Uprimny C, Zelger B and Kähler CM: Diagnostic and
therapeutic challenges of a large pleural inflammatory
myofibroblastic tumor. Case Rep Pulmonol.
2012:1021962012.PubMed/NCBI
|
|
7
|
Torres Gomez FJ, Fernández Machín P and
Garcia Suarez RM: Right orchiectomy: inflammatory testicular
pseudotumor. Arch Esp Urol. 65:641–642. 2012.(In Spanish).
|
|
8
|
Harpaz N, Gribetz AR, Krellenstein DJ and
Marchevsky AM: Inflammatory pseudotumor of the thymus. Ann Thorac
Sur. 42:331–333. 1986. View Article : Google Scholar
|
|
9
|
Cerfolio RJ, Allen MS, Nascimento AG,
Deschamps C, Trastek VF, Miller DL and Pairolero PC: Inflammatory
pseudotumors of the lung. Ann Thorac Surg. 67:933–936. 1999.
View Article : Google Scholar
|
|
10
|
Batsakis JG, el-Naggar AK, Luna MA and
Goepfert H: ‘Inflammatory pseudotumor’: what is it? How does it
behave? Ann Otol Rhinol Laryngol. 104:329–331. 1995.
|
|
11
|
Kojima K, Yokoi K, Matsuguma H, Kondo T,
Kamiyama Y, Mori K and Igarashi S: Middle mediastinal thymoma. J
Thorac Cardiovasc Surg. 124:639–640. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Monden Y, Nakahara K, Iioka S, Nanjo S,
Ohno K, Fujii Y, Hashimoto J, Kitagawa Y, Masaoka A and Kawashima
Y: Recurrence of thymoma: clinicopathological features, therapy,
and prognosis. Ann Thorac Surg. 39:165–169. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Okumura M, Ohta M, Tateyama H, Nakagawa K,
Matsumura A, Maeda H, Tada H, Eimoto T, Matsuda H and Masaoka A:
The World Health Organization histologic classification system
reflects the oncologic behavior of thymoma: a clinical study of 273
patients. Cancer. 94:624–632. 2002. View Article : Google Scholar
|
|
14
|
Corneli G, Alifano M, FortiParri S, Lacava
N and Boaron M: Invasive inflammatory pseudotumor involving the
lung and the mediastinum. Thorac Cardiovasc Surg. 49:124–126. 2001.
View Article : Google Scholar
|
|
15
|
Melloni G, Carretta A, Ciriaco P, et al:
Inflammatory pseudotumor of the lung in adults. Ann Thorac Surg.
79:426–432. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim TS, Han J, Kim GY, Lee KS, Kim H and
Kim J: Pulmonary inflammatory pseudotumor (inflammatory
myofibroblastic tumor): CT features with pathologic correlation. J
Comput Assist Tomogr. 29:633–639. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hosler GA, Steinberg DM, Sheth S, Hamper
UM, Erozan YS and Ali SZ: Inflammatory pseudotumor: a diagnostic
dilemma in cytopathology. Diagn Cytopathol. 31:267–270. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Arber DA, Weiss LM and Chang KL: Detection
of Epstein-Barr virus in inflammatory pseudotumor. Semin Diagn
Pathol. 15:155–160. 1998.PubMed/NCBI
|
|
19
|
Amano S, Hazama F, Kubagawa H, Tasaka K,
Haebara H and Hamashima Y: General pathology of Kawasaki disease.
On the morphological alterations corresponding to the clinical
manifestations. Acta Pathol Jpn. 30:681–694. 1980.
|