Introduction
Gastric cancer (GC) is the most common malignancy
and the third most common cause of cancer-related mortality in
Korea (1). Although leptomeningeal
carcinomatosis (LMC) does not occur as frequently as with other
malignancies, such as lung and breast carcinoma, gastric cancer may
follow a complex course including metastasis to the brain
parenchyma or meninges (2).
Irrespective of the primary site of the cancer, LMC is a rare but
devastating complication. The prevalence of LMC in GC is as low as
0.1–0.24% (3,4). Internal auditory canal (IAC)
metastasis from GC has rarely been reported (5) and, to the best of our knowledge, IAC
metastasis due to LMC has never been reported in GC.
The rate of Her2 positivity in GC is 22%, which is
similar to the rate of that in breast cancer (BC) (6). Although increasing incidences of
central nervous system (CNS) metastases have been reported in
Her2-overexpressing BC due to the high anticancer effect of
systemic trastuzumab (Her2 monoclonal antibody) without penetration
of the blood-brain barrier, it is uncertain whether Her2 positivity
in GC increases the risk of CNS metastases (7). LMC in Her2-positive GC has rarely been
reported (8). The patient in the
present case experienced LMC including IAC metastasis from
Her2-positive GC. To the best of our knowledge, this is the first
report of IAC metastasis in Her2-positive GC. Consent was obtained
from the family of the patient.
Case report
A 56-year-old male who had been diagnosed with
Her2-positive advanced GC with multiple lymph node metastases,
including left supraclavicular, paraaortic and retroperitoneal
lymph nodes, underwent 12 cycles of combination chemotherapy
composed of trastuzumab (Her2 monoclonal antibody), capecitabine
and cisplatin at the Konkuk University Medical Center (Seoul,
Korea). Cisplatin was discontinued after the eighth cycle due to
cumulative peripheral neuropathy. Only capecitabine and trastuzumab
were continued due to their clinical benefits. The response was a
partial remission according to Response Evaluation Criteria In
Solid Tumors (9).
After the 10th cycle of chemotherapy, the patient
was referred to the Department of Otorhinolaryngology-Head and Neck
Surgery at the Konkuk University Medical Center, Konkuk University
School of Medicine (Seoul, Korea) for an evaluation of right ear
fullness, which had been persisting for 15 days. Otitis media with
effusion was diagnosed by an otoendoscopic examination, and the
nasopharyngeal examination revealed no specific finding. Bone
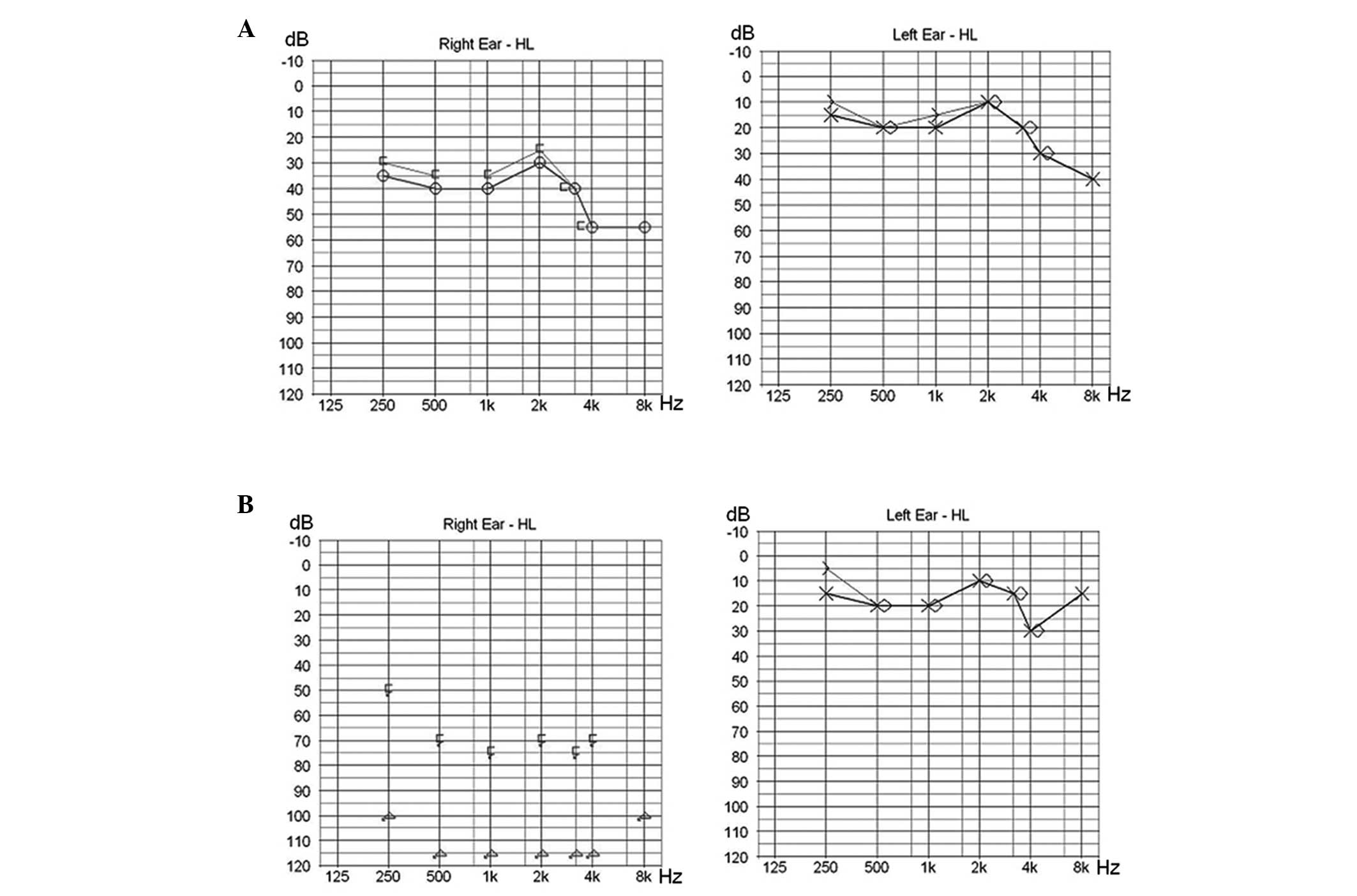
conduction pure tone audiometry after the treatment of the otitis
media with effusion revealed mild (35dB) sensorineural hearing loss
on the right side (Fig. 1A).
Two weeks later, the patient suddenly developed a
total hearing loss (Fig. 1B) and
facial weakness on the right side, accompanied by severe vertigo.
Physical examination revealed left-beating spontaneous nystagmus
and peripheral-type facial palsy of House-Brackmann grade IV on the
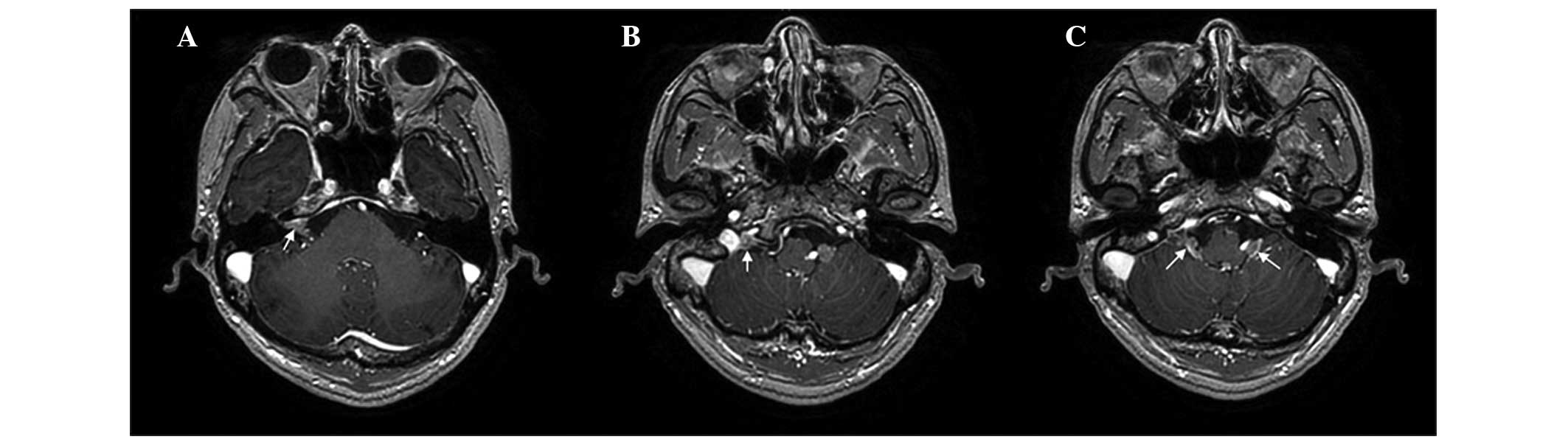
right side (10). Magnetic
resonance imaging (MRI) of the brain revealed enhancing lesions in
the right IAC (Fig. 2A), right
jugular fossa (Fig. 2B) and
bilateral cerebellomedullary cistern (Fig. 2C), and multifocal small enhancing
nodules in other brain regions. The patient was diagnosed with LMC,
and received whole-brain radiotherapy and palliative chemotherapy
containing irinotecan, which is known to penetrate the blood-brain
barrier (11). Following
whole-brain radiotherapy, neurological symptoms including facial
palsy and vertigo andnystagmus were improved, although the right
hearing loss did not recover. However, the patient succumbed to
rapid aggravation of his systemic metastases 8 weeks following the
diagnosis of LMC with IAC. The interval from the date of diagnosis
of GC to the date of diagnosis of LMC was 7 months. The patient’s
survival time following the diagnosis of advanced GC was 9
months.
Discussion
Sudden hearing loss, vertigo and ipsilateral facial
palsy caused by IAC metastasis are uncommon initial presenting
symptoms in patients with LMC. Recently, IAC metastasis due to
direct invasion into the IAC from the metastatic lesion in the
petrous apex was reported, which was a different spread pattern to
that in the present case (5). LMC,
hematogenous dissemination, and direct extension from the adjacent
areas are considered as the possible routes of IAC metastasis
(12). The present study reports
the case of a patient with Her2-overexpressing GC who developed IAC
metastasis and LMC despite systemic partial remission status with
trastuzumab containing chemotherapy. This clinical condition may be
the result of the neurotropism of Her2-overexpressing GC cells, as
trastuzumab cannot penetrate th blood-brain barrier (13,14).
Early diagnosis of LMC is important in order to
prevent irreversible neurological deficits. The most common
symptoms of IAC metastasis include facial nerve palsy, hearing loss
and tinnitus, and these symptoms are rapidly progressive in nature
(12). Although a diagnosis of LMC
including IAC involvement was not difficult to determine in this
patient, the diagnosis would have been made earlier if the brain
MRI had been performed when the patient showed mild sensorineural
hearing loss. Sensorineural hearing loss, although mild, on the
right side may have been caused by metastatic invasion into the IAC
in this patient. In the present study, LMC was not suspected
earlier as the patient developed LMC despite primary tumor and
lymph node metastases which were controlled well by chemotherapy.
The mild hearing impairment was not considered to be associated
with the LMC, but instead due to cisplatin-induced ototoxicity or
isolated ear problems. This case showed that the systemic response
and response of the brain or leptomeninges may differ. Systemically
well-controlled Her2-positive GC may develop as LMC and therefore,
mild hearing impairments must be considered as a possible sign of
LMC or brain metastases as prompt suspicion and timely therapy may
improve patient outcome. This finding suggests that physicians
should be attentive to patients with stable systemic disease for
the timely diagnosis of LMC, rather than solely focusing on
patients with systemically progressive disease or terminal disease
status.
LMC in Her2-positive GC was first reported by
Cavanna et al (8). Despite
whole-brain radiotherapy and intrathecal (IT)trastuzumab, the
patient died 3 months after the diagnosis of LMC. The patient in
the present case also died within months (2 months) of the
diagnosis of LMC. In the study by Cavanna et al, the
researchers reported LMC and confusion, cognitive impairment and
ataxia without hearing loss, which are different symptoms to those
identified in the present case. IT trastuzumab therapy has been
investigated in Her2-positive BC, and case reports indicate that
this is a promising experimental treatment for patients with
symptomatic LMC (7,15,16).
However, it is unclear whether IT trastuzumab may have a clinical
benefit in LMC of Her2-positive GC. In the present case, IT
trastuzumab was not administered due to the patient’s general
condition; rapid aggravation of the patient’s systemic metastases
occurred immediately following discontinuation of chemotherapy.
Aggressive treatment of LMC is particularly justified in patients
whose disease is systemically well-controlled. Lapatinib, a
tyrosine kinase inhibitor that targets Her2, has demonstrated
clinical activity against CNS metastases in Her2-overexpressing BC
(17). Lapatinib may be a
therapeutic option for LMC in Her2-positive GC. Early diagnosis and
optimal treatment of LMC including IAC metastasis is a crucial
challenge. Future studies are warranted to establish optimal
treatment of LMC in Her2-positive GC.
In conclusion, a clinical history of sudden
sensorineural hearing loss raises the possibility of IAC
metastasis, which may be a consequence of LMC, in Her2-positive GC.
Prompt suspicion and an MRI are greatly helpful in the diagnosis of
metastatic carcinoma to the IAC. We would like to emphasize that if
hearing impairment is suspected in Her2-positive GC, LMC should be
considered as a differential diagnosis, and early diagnosis and
concerted therapeutic efforts are important for the management of
LMC in Her2-positive GC.
References
|
1
|
Jung KW, Park S, Kong HJ, Won YJ, Lee JY,
Seo HG, et al: Cancer statistics in Korea: incidence, mortality,
survival, and prevalence in 2009. Cancer Res Treat. 44:11–24.
2012.
|
|
2
|
Lee JL, Kang YK, Kim TW, Chang HM, Lee GW,
Ryu MH, et al: Leptomeningeal carcinomatosis in gastric cancer. J
Neurooncol. 66:167–174. 2004.
|
|
3
|
Giglio P, Weinberg JS, Forman AD, Wolff R
and Groves MD: Neoplastic meningitis in patients with
adenocarcinoma of the gastrointestinal tract. Cancer.
103:2355–2362. 2005.
|
|
4
|
Oh SY, Lee SJ, Lee J, Lee S, Kim SH, Kwon
HC, et al: Gastric leptomeningeal carcinomatosis: multi-center
retrospective analysis of 54 cases. World J Gastroenterol.
15:5086–5090. 2009.
|
|
5
|
Han JK, Park KH, Lee MS and Lee CK:
Gastric carcinoma metastasis to the internal auditory canal. Otol
Neurotol. 33:e19–e20. 2012.
|
|
6
|
Bang YJ, Van Cutsem E, Feyereislova A,
Chung HC, Shen L, Sawaki A, et al: Trastuzumab in combination with
chemotherapy versus chemotherapy alone for treatment of
HER2-positive advanced gastric or gastro-oesophageal junction
cancer (ToGA): a phase 3, open-label, randomised controlled trial.
Lancet. 376:687–697. 2010.
|
|
7
|
Mir O, Ropert S, Alexandre J, Lemare F and
Goldwasser F: High-dose intrathecal trastuzumab for leptomeningeal
metastases secondary to HER-2 overexpressing breast cancer. Ann
Oncol. 19:1978–1980. 2008.
|
|
8
|
Cavanna L, Rocchi A, Gorgni S, Ambroggi M,
Foroni RP, Ubbiali A, et al: Cerebrospinal fluid cytology diagnosis
of HER2-positive leptomeningeal carcinomatosis from HER2-positive
metastatic gastric cancer: case report. J Clin Oncol. 29:e367–e368.
2011.
|
|
9
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, Kaplan RS, Rubinstein L, et al: New guidelines to
evaluate the response to treatment in solid tumors. European
Organization for Research and Treatment of Cancer, National Cancer
Institute of the United States, National Cancer Institute of
Canada. J Natl Cancer Inst. 92:205–216. 2000.
|
|
10
|
House JW and Brackmann DE: Facial nerve
grading system. Otolaryngol Head Neck Surg. 93:146–147. 1985.
|
|
11
|
Friedman HS, Keir ST and Houghton PJ: The
emerging role of irinotecan (CPT-11) in the treatment of malignant
glioma in brain tumors. Cancer. 97(9 Suppl): 2359–2362. 2003.
|
|
12
|
Streitmann MJ and Sismanis A: Metastatic
carcinoma of the temporal bone. Am J Otol. 17:780–783. 1996.
|
|
13
|
Lampson LA: Monoclonal antibodies in
neuro-oncology: Getting past the blood-brain barrier. MAbs.
3:153–160. 2011.
|
|
14
|
Mehta AI, Brufsky AM and Sampson JH:
Therapeutic approaches for HER2-positive brain metastases:
circumventing the blood-brain barrier. Cancer Treat Rev.
39:261–269
|
|
15
|
Mego M, Sycova-Mila Z, Obertova J, Rajec
J, Liskova S, Palacka P, et al: Intrathecal administration of
trastuzumab with cytarabine and methotrexate in breast cancer
patients with leptomeningeal carcinomatosis. Breast. 20:478–480.
2011.
|
|
16
|
Platini C, Long J and Walter S: Meningeal
carcinomatosis from breast cancer treated with intrathecal
trastuzumab. Lancet Oncol. 7:778–780. 2006.
|
|
17
|
Lin NU, Diéras V, Paul D, Lossignol D,
Christodoulou C, Stemmler HJ, et al: Multicenter phase II study of
lapatinib in patients with brain metastases from HER2-positive
breast cancer. Clin Cancer Res. 15:1452–1459. 2009.
|