Introduction
The prognosis of patients with advanced non-small
cell lung cancer (NSCLC), particularly the non-squamous subtype,
could be improved. Studies by Mitsudomi et al (1) and Maemond et al (2) found that patients with lung cancer who
were selected by epidermal growth factor receptor (EGFR) mutations
have a significantly longer progression-free survival rate if they
are treated with gefitinib compared with treatment with
cisplatin-docetaxel or carboplatin-paclitaxel. Recent studies
(3,4) have shown that the overall survival
(OS) time in two former Japanese studies (1,2) was ≥2
years in the gefitinib and platinum doublet groups.
While several studies (5–9)
retrospectively defined a ≥2-year survival time in patients with
advanced NSCLC as long-term survival, however, recently, other
patients with advanced NSCLC have been encountered who have
survived ≥5 years (10). Kaira
et al (11) also reported
the survival of patients with advanced NSCLC for ≥5 years.
In the present study, the factors associated with
extended survival time were examined along with the clinical
features, types of treatments administered and EGFR mutations in
patients with metastatic NSCLC who had survived for ≥5 years.
Patients and methods
Study approval
The present retrospective study was approved by the
Institutional Review Board of the Osaka Prefectural Medical Center
for Respiratory and Allergic Diseases (Osaka, Japan) on June 19,
2012 (approval no. 596).
Criteria
Of the 360 patients with NSCLC in our previous study
(10), those patients with stage
IIIA cancer (n=27), relapse following chemoradiation therapy (n=22)
or thoracic radiation therapy (n=2), local recurrence following
thoracic surgery (n=5) and stage IIIB cancer without pleural
disseminations or malignant pleural effusion (n=36) were excluded
from the current study. Patients with pleural dissemination or
malignant pleural effusion were considered as stage IV according
the seventh edition of the tumor-node-metastasis (TNM)
classification of the International Association for the Study of
Lung Cancer (12). Overall, the
clinical records of 268 NSCLC patients with distant metastasis who
underwent first-line chemotherapy between January 1, 2004, and
December 31, 2007, and had been observed for ≥5 years as of
December 31, 2012, were retrospectively examined. For inclusion in
the current study, all patients met the following criteria: A
diagnosis of histopathologically-confirmed primary NSCLC
(adenocarcinoma, squamous cell carcinoma, large cell carcinoma or
unclassified NSCLC), the presence of distant metastasis at the time
of diagnosis or recurrence following thoracic surgery according to
the seventh edition of the TNM Classification of the International
Association for the Study of Lung Cancer (12), treatment with systemic cytotoxic
agents, either cytotoxic chemotherapy or EGFR-tyrosine kinase
inhibitor (TKI) therapy, and perioperative chemotherapy that was
not regarded as first-line chemotherapy. In the present study,
unilateral multiple lung metastases were defined as distant
metastasis.
Baseline demographic information
Baseline demographic data, including gender, age,
Eastern Cooperative Oncology Group performance status (PS),
histology, stage and smoking status at the initiation of first-line
chemotherapy, were obtained for each patient. At the time of
analysis, the following data were available for all patients: A
complete patient history with results from a physical examination,
surgical and pathological reports, the results of mediastinoscopy,
fiberoptic bronchoscopy, thoracoscopy and imaging (chest
radiography and computed tomography or magnetic resonance imaging,
and bone scintigraphy or positron emission tomography) and the
number of metastatic organs and metastatic sites.
Best response to first-line
chemotherapy
The best response to first-line chemotherapy was
determined by a review of the patient records compiled by
physicians during weekly cancer conferences held at the Osaka
Prefectural Medical Center for Respiratory and Allergic Diseases
and based upon the Response Evaluation Criteria in Solid Tumors
(RECIST) (13). Based on RECIST,
the tumor response to cytotoxic agents was categorized as a partial
response (PR), stable disease (SD) and progressive disease (PD). A
tumor response that could not be evaluated was described as not
evaluable (NE).
Treatment
In addition to the data from our previous study
(10), the data regarding the
subsequent treatment of each patient were added to the database,
including those regarding regimen, number of cycles, dosage and
date of regimen initiation and termination.
Palliative radiotherapy (RT)
While the palliative RT administered at the Osaka
Prefectural Medical Center for Respiratory and Allergic Diseases
had consisted of RT to the bone, whole brain and other sites,
palliative RT at other institutions had consisted of stereotactic
radiosurgery (SRS) to the brain metastases. All relevant data were
collected from the patient clinical records.
Survival
Survival time was defined as the period from the
date of initiation of first-line chemotherapy to the date of
mortality or last follow-up, and survival data were last updated on
December 31, 2012. Subsequent to the estimation of the survival
rates using the Kaplan-Meier method, the patients were classified
into three groups for comparison of their demographic and clinical
characteristics as follows: Those who had survived ≥5 years (≥5
years group), those who had survived ≥2 years, but <5 years
(≥2–5 years group) and those who had survived <2 years (<2
years group).
Genetic testing for EGFR and other
NSCLC-driving mutations
Tissue samples from surviving patients with NSCLC in
the present study were sent to Mitsubishi Chemical Medience
Corporation (Tokyo, Japan) for peptide nucleic acid-locked nucleic
acid polymerase chain reaction clamp-based testing between June 1,
2007, and December 31, 2012. Per the protocol of the previous WJTOG
3405 (1) and WJTOG 0403 (14) clinical trials at the Osaka
Prefectural Medical Center for Respiratory and Allergic Diseases,
screening for drug-sensitive EGFR mutations, including a deletion
in exon 19 or an L858R substitution in exon 21, was conducted.
Additionally, the anaplastic lymphoma kinase (ALK) translocations
were determined via fluorescence in situ hybridization and
K-ras mutations as driver mutations in patients who had survived ≥5
years.
Statistical analysis
Statistical analyses were performed using software
package R (15). Patient background
data were compared using the χ2 test and Fisher’s exact
test for categorical factors. Patient treatment data were compared
using the Mann-Whitney U test. P<0.05 was considered to indicate
a statistically significant difference. Prognostic factors were
analyzed by univariate and multivariate analyses using the Cox
proportional hazards model. Differences among survival curves were
assessed using the log-rank test. Multivariate analysis was
performed among selected prognostic factors when P<0.005 in
univariate analysis. A small number of significant prognostic
factors in univariate analysis were excluded from multivariate
analysis.
Results
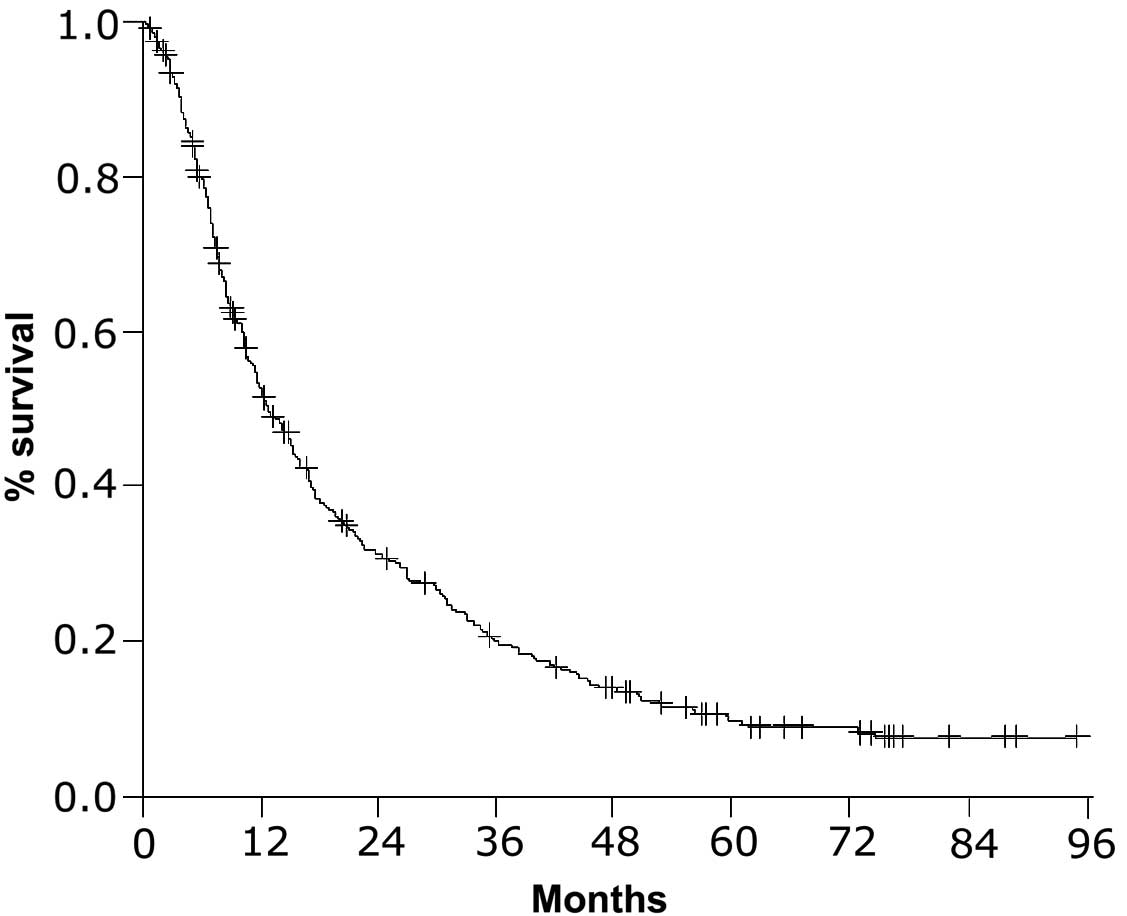
Overall survival
As shown in Fig. 1,
the median survival time (MST) of the 268 NSCLC patients with
distant metastasis examined in the present study was 14 months (95%
confidence interval, 11.4–15.3). Based on a review of the survival
data, 22 patients (8.2%) were placed in the ≥5 years group, 48
patients (17.9%) were placed in the ≥2–5 years group and 198
patients (73.9%) were placed in the <2 years group.
Prognostic factors
As shown in Table I,
by univariate analysis, gender, smoking status, PS, histology,
relapse following thoracic surgery and number of metastatic organs
were identified as significant prognostic factors (P=0.0003,
P<0.0001, P<0.0001, P=0.0091, P=0.0017 and P=0.0460,
respectively). The patients with metastasis to the intra-thoracic
organs, including lungs, pleura and pericardium, had a
significantly improved prognosis compared with those with other
types of metastasis (P=0.0007). By contrast, the patients with
metastasis to the abdominal organs, including adrenal glands,
liver, kidney and other sites, had a significantly worse prognosis
than those with other types of metastasis (P<0.0001).
Multivariate analysis was performed among selected prognostic
factors, including gender, smoking status, PS, relapse following
thoracic surgery, metastasis to intra-thoracic organs and
metastasis to abdominal organs in univariate analysis, which were
confirmed as significant prognostic factors (P=0.0009, P<0.0001,
P<0.0001, P=0.0009 and P=0.0006, respectively).
 | Table IUnivariate and multivariate analysis
of prognostic factors (n=268). |
Table I
Univariate and multivariate analysis
of prognostic factors (n=268).
| | Univariate | Multivariate |
|---|
| |
|
|
|---|
| Variables | n (%) | P-value | HR (95% CI) | P-value | HR (95% CI) |
|---|
| Gender | | 0.0003 | 1.72
(1.278–2.314) | 0.577 | 1.106
(0.776–1.577) |
| Male | 186 (69) | | | | |
| Female | 82 (31) | | | | |
| Age, years | | 0.51 | 0.92
(0.703–1.192) | | |
| >66 | 137 (51) | | | | |
| <66 | 131 (49) | | | | |
| Smoking status | |
1.2×10−7 | 2.23
(1.659–3.409) | 0.0009 | 1.86
(1.290–2.675) |
| Never | 87 (32) | | | | |
| Ever | 181 (68) | | | | |
| PS | |
4.1×10−5 | 2.02
(1.442–2.822) |
5.6×10−6 | 2.21
(1.564–3.106) |
| 0–1 | 213 (79) | | | | |
| 2–3 | 55 (21) | | | | |
| Histology | | 0.0091 | 1.59
(1.123–2.261) | | |
| Ad | 220 (82) | | | | |
| Non-Ad | 48 (18) | | | | |
| Relapse following
surgery | | 0.0017 | 1.77
(1.238–2.519) |
1.48×10−5 | 2.28
(1.571–3.317) |
| Yes | 49 (18) | | | | |
| No | 219 (82) | | | | |
| Number of metastatic
organs | | 0.0460 | 1.32
(1.005–1.732) | | |
| 1 | 161 (60) | | | | |
| ≥2 | 107 (40) | | | | |
| Metastatic sites | | | | | |
| Intra-thoracic
organs | | 0.0007 | 0.607
(0.456–0.810) | 0.0009 | 0.593
(0.435–0.808) |
| Yes | 185 (69) | | | | |
| No | 83 (31) | | | | |
| Abdominal
organs | |
2.6×10−5 | 2.07
(1.474–3.649) | 0.0006 | 1.88
(1.311–2.689) |
| Yes | 55 (21) | | | | |
| No | 213 (79) | | | | |
| Brain | | 0.48 | 1.13
(0.807–1.584) | | |
| Yes | 55 (21) | | | | |
| No | 213 (79) | | | | |
| Bone | | 0.0592 | 1.38
(0.997–1.899) | | |
| Yes | 58 (22) | | | | |
| No | 210 (78) | | | | |
| Lymph nodes
(distant) | | 0.6 | 1.12
(0.741–1.684) | | |
| Yes | 29 (11) | | | | |
| No | 239 (89) | | | | |
Demographic characteristics according to
survival duration
Table II summarizes
the patient demographic characteristics of the three survival
groups according to gender, histology and the significant
prognostic factors determined by multivariate analysis. All 22
patients in the ≥5 years group, 41 out of 48 patients in the ≥2–5
years group and 157 out of 198 patients in the <2 years group
had histologically-confirmed adenocarcinoma. Although the
demographical data of the patients in the ≥5 and ≥2–5 years groups
were extremely similar, analysis revealed a significantly greater
number of patients that had never smoked in the ≥5 years group when
compared with the ≥2–5 years group (P=0.0020). By contrast, the
variables of female gender, never smoking, PS, relapse following
thoracic surgery and metastasis to intra-thoracic organs were
significant in the ≥5 years group when compared with the <2
years group (P=0.0017, P<0.0001, P=0.0158, P=0.0200 and
P=0.0220, respectively). A significantly greater number of patients
with a PS of 0 or 1 who had relapsed following thoracic surgery
experienced metastasis to the intra-thoracic organs, and a
significantly smaller number of patients who experienced abdominal
metastasis were found in the ≥2–5 years group compared with the
<2 years group (P=0.0269, P=0.0008, P=0.0469 and P=0.0133,
respectively).
 | Table IIPatient characteristics according to
survival duration. |
Table II
Patient characteristics according to
survival duration.
| Variables | ≥5 years, n | ≥2–5 years, n | <2 years, n |
|---|
| Gender |
| Male | 9 | 32 | 145 |
| Female | 13a | 16 | 53 |
| Smoking status |
| Never | 17a,b | 18 | 53 |
| Ever | 5 | 30 | 145 |
| PS |
| 0 or 1 | 22a | 43c | 148 |
| 2 or 3 | 0 | 5 | 50 |
| Histology |
| Ad | 22 | 41 | 157 |
| Non-ad | 0 | 7 | 41 |
| Relapse following
thoracic surgery |
| Yes | 7a | 16c | 26 |
| No | 15 | 32 | 172 |
| Metastatic
site |
| Intra-thoracic
organs | | | |
| Yes | 20a | 38c | 127 |
| No | 2 | 10 | 71 |
| Abdominal
organs |
| Yes | 1 | 3c | 51 |
| No | 21 | 45 | 147 |
| EGFR mutation |
| Wild-type | 8 | 9 | 13 |
| Exon19
deletion | 5 | 10 | 3 |
| Exon21L858R | 2 | 1 | 0 |
| Other | 2 | 0 | 2 |
| Unknown | 5 | 28 | 180 |
A total of 55 (20.5%) patients underwent EGFR
mutation testing. Of these patients, 30 had wild-type EGFR, 21 had
drug-sensitive mutations (18 with a deletion in exon 19 and three
with the L858R mutation), and four had other types of mutations,
consisting of one with a deletion in exon 19 plus a T790M mutation,
one with a L861Q mutation in exon 21 and two with a point mutation
in exon 18. The remaining patients were unable to undergo testing
due to the inability to obtain either insurance approval or an
adequate tissue sample.
Treatment efficacy, EGFR-TKI therapy
duration and number of cycles of cytotoxic agent therapy according
to survival duration
Of the 268 patients, 165 (61.6%) underwent at least
second-line chemotherapy, 96 (35.8%) at least third-line
chemotherapy and 54 (20.1%) underwent at least fourth-line
chemotherapy. As shown in Table
III, compared with the patients in the <2 years group, the
patients in the ≥5 years and ≥2–5 years groups experienced a PR or
SD significantly more frequently (P=0.0011 and P=0.0002,
respectively), underwent a significantly greater number of regimens
(P<0.0001 and P<0.0001, respectively) and underwent EGFR-TKI
therapy (63.6% of the ≥5 years group and 56.2% of the ≥2–5 years
group vs. 29.8% of the <2 years group) significantly more
frequently (P=0.0014 and P=0.0006, respectively). Patients in the
≥5 years group underwent significantly more total months of
EGFR-TKIs treatment in the ≥2–5 years and <2 years groups
(P=0.0068 and P<0.0001, respectively) and significantly more
cycles of cytotoxic agent therapy (P=0.0045, and P<0.0001,
respectively). By contrast, compared with the patients in the <2
years group, those in the ≥2–5 years group underwent significantly
more total months of EGFR-TKIs treatment and cycles of cytotoxic
agent therapy (P=0.0003 and P<0.0001, respectively). As shown in
Table III, 142 (53.0%) of the 268
patients underwent palliative RT, including SRS to brain
metastases, whole brain RT, RT to bone metastasis and RT to other
metastatic sites. No significant differences were found among the
three survival groups regarding frequency of RT to each site.
 | Table IIITreatment efficacy, duration of
EGFR-TKI therapy and number of cycles of cytotoxic agents according
to survival duration. |
Table III
Treatment efficacy, duration of
EGFR-TKI therapy and number of cycles of cytotoxic agents according
to survival duration.
| Variables | ≥5 years | ≥2–5 years | <2 years |
|---|
| Response to
first-line chemotherapy, n |
| PR or SD | 20a | 39b | 103 |
| PD or NE | 2 | 9 | 95 |
| Number of
regimens |
| Median | 3.5a | 4b | 2 |
| Range | 1–13 | 1–9 | 1–7 |
| EGFR-TKI
therapy |
| Number of
patients, n (%) | 14 (63.6)a | 27 (56.3)b | 59 (29.8) |
| Total treatment
months |
| Median | 40.1a,c | 11.0b | 1.6 |
| Range | 0.4–93.6 | 0.2–60.2 | 0.1–11.6 |
| Cytotoxic agent
therapy |
| Number of
patients, n (%) | 19 (86.4) | 47 (97.9) | 187 (94.4) |
| Total treatment
cycles, n |
| Median | 36a,c | 16b | 4 |
| Range | 4–92 | 1–52 | 1–18 |
| Palliative RT |
| Number of
patients, n (%)d | 13 (59.1) | 30 (62.5) | 99 (50.0) |
| Whole brain RT,
n | 3 | 10 | 25 |
| SRS to brain
metastasis, n | 5 | 7 | 25 |
| RT to bone
metastasis, n | 5 | 20 | 56 |
| RT to other
metastasis, n | 4 | 0 | 19 |
Driver mutations in and treatment
administered to the ≥5 years group
As summarized in Table
IV, the 22 patients in the ≥5 years group were classified into
four groups (A-D) according to their response to EGFR-TKIs and
cytotoxic agent therapy. Five patients (group A) responded mainly
to EGFR-TKI therapy, five patients (group B) responded to EGFR-TKI
and cytotoxic agent therapy and eight patients (group C) responded
mainly to cytotoxic agent therapy. Four patients (group D)
exhibited indolent tumors and did not undergo cytotoxic agent
therapy in the long term. Of the 17 patients in the ≥5 years group
who had undergone driver mutation testing, one tested positive for
ALK translocation. Seven patients tested negative for EGFR
mutations, ALK translocation or K-ras mutations.
 | Table IVDriver mutations in and treatment of
patients who survived ≥5 years according to response to EGFR-TKI
and cytotoxic agent. |
Table IV
Driver mutations in and treatment of
patients who survived ≥5 years according to response to EGFR-TKI
and cytotoxic agent.
| A, Responders to
mainly EGFR-TKI therapy |
|---|
|
|---|
| Case | Driver
mutation | Cytotoxic agents,
cycles | EGFR-TKIs,
months |
|---|
| 1 | EGFR: L858R | 0 | 93.6 |
| 2 | - | 0 | 67.4 |
| 3 | EGFR: del19 | 5 | 51.1 |
| 4 | - | 9 | 61.4 |
| 5 | EGFR: del19 | 0 | 67.1 |
|
| B, Responders to
both EGFR-TKI and cytotoxic agent therapy |
|
| Case | Driver
mutation | Cytotoxic agents,
cycles | EGFR-TKIs,
months |
|
| 6 | EGFR: del19 | 54 | 38.0 |
| 7 | - | 29 | 42.3 |
| 8 | EGFR: L858R | 43 | 22.0 |
| 9 | EGFR: del19 | 28 | 25.1 |
| 10 | EGFR: del19 | 16 | 49.5 |
|
| C, Responders to
mainly cytotoxic agent therapy |
|
| Case | Driver
mutation | Cytotoxic agents,
cycles | EGFR-TKIs,
months |
|
| 11 | Triple
negative | 87 | 9.2 |
| 12 | ALK
translocation | 92 | 5.5 |
| 13 | - | 64 | 3.2 |
| 14 | Triple
negative | 52 | 0.0 |
| 15 | Triple
negative | 58 | 0.0 |
| 16 | - | 36 | 0.0 |
| 17 | EGFR:
del19/T790M | 43 | 0.4 |
| 18 | Triple
negative | 68 | 0.0 |
|
| D, Patients with
indolent tumors |
|
| Case | Driver
mutation | Cytotoxic agents,
cycles | EGFR-TKIs,
months |
|
| 19 | Triple
negative | 10 | 0.0 |
| 20 | Triple
negative | 10 | 0.0 |
| 21 | EGFR: L861Q | 4 | 0.0 |
| 22 | Triple
negative | 10 | 0.0 |
Discussion
In a study by Van Damme et al (9), long-term survivors were defined as
patients who survived >2 years, and it was concluded that there
are extremely few clinical factors at the time of diagnosis that
can distinguish survivors of >2 years from survivors of ≤2
years. Compared with these results, the present study showed PS,
relapse following thoracic surgery and metastatic sites as
significant prognostic factors, which distinguished the ≥2–5 years
group from the <2 years group. For achieving ≥5 years of
survival, the never-smoked status characteristic was the most
significant prognostic factor in the present study. Furthermore, in
a study of 112 patients who had experienced recurrence following
surgery, Yamazaki et al (16) reported a good prognosis (MST, 25.6
months) and identified the significant prognostic factors to be
histology, age, PS and abdominal metastasis. In this study and the
present study, patients with abdominal metastasis exhibited a poor
survival time, which may have been due to the lack of effective RT
as a local therapy, as there is no effective treatment for
abdominal metastasis.
With regard to treatment-related factors, compared
with the patients in the <2 years group, the patients in the ≥5
years and ≥2–5 years groups experienced a PR or SD to first-line
chemotherapy significantly more frequently. The previous studies of
Van Damme et al (9) and
Giroux Leprieur et al (8),
as well as the present study, indicated that the response to
first-line chemotherapy was a significantly important variable for
long-term survival of >2 years.
In the present study, it appears that the various
regimens used following progression subsequent to first-line
chemotherapy contributed to the extended survival rate, leading to
a relatively long MST (14 months) and facilitating the survival of
70 patients (26.1%) for ≥2 years and 22 patients (8%) for ≥5 years.
As the study by Hotta et al (17) indicated that survival
post-progression has become more closely associated with the OS
rate by intensive treatment following progression, the current
study indicated that chemotherapy subsequent to progression
following first-line chemotherapy would be extremely important
variables for achieving ≥5 years of survival.
Kaira et al (11) found that 10 patients (8%) survived
for ≥5 years in a study of 124 patients with advanced NSCLC treated
with chemotherapy, the same as the current study. Accordingly,
Kaira et al concluded that a favorable PS, the presence of
adenocarcinoma and the use of EGFR-TKI therapy were significant
factors in patients surviving >5 years. Only two of the 10
patients described in the aforementioned study underwent EGFR
mutation testing. Therefore, there is no information from the study
about the correlation between treatment and EGFR mutation in
patients who survived for ≥5 years. In the present study, of the 17
patients in the ≥5 years group who underwent EGFR mutation testing,
seven tested positive for drug-sensitive EGFR mutations, two for
other types of EGFR mutations and eight for wild-type EGFR. All
seven patients with drug-sensitive EGFR mutations were placed in
groups A or B. No patients in groups C and D had drug-sensitive
EGFR mutations. This study showed a clear correlation between
treatment and EGFR mutation status in a higher number of patients
than the study by Kaira et al (11). In the present study, seven patients
with EGFR drug-sensitive mutations achieved ≥5 years of survival.
Since patients with drug-sensitive EGFR mutations would potentially
survive for ≥5 years, it is extremely important to select patients
for EGFR-TKI therapy by screening for drug-sensitive EGFR
mutations. Notably, in the present study certain patients without
EGFR drug-sensitive mutations would have achieved ≥5 years of
survival by continuing long-term effective cytotoxic agent
treatments.
The limitations of the study were that it was
retrospective, conducted in a single center and normally, patients
with improved prognoses would have received more aggressive
treatments. Furthermore, patients with a longer survival time would
have received multiple regimens and long-term treatments. The study
consisted of consecutive and unselected patients at the Osaka
Prefectural Medical Center for Respiratory and Allergic Diseases,
and reflected the daily practical treatments of NSCLC patients with
distant metastasis who received first-line chemotherapy between
2004 and 2007.
In conclusion, achieving ≥5 years of survival in
NSCLC patients with distant metastasis was associated with the
never-smoked status, response to first-line chemotherapy, EGFR-TKI
therapy according to genetic testing, continuing effective
cytotoxic regimens and RT as local therapy.
Acknowledgements
The present study was supported by funds from the
Japanese Clinical Oncology Group.
References
|
1
|
Mitsudomi T, Morita S, Yatabe Y, et al;
West Japan Oncology Group. Gefitinib versus cisplatin plus
docetaxel in patients with non-small-cell lung cancer harbouring
mutations of the epidermal growth factor receptor (WJTOG3405): an
open label, randomised phase 3 trial. Lancet Oncol. 11:121–128.
2010.
|
|
2
|
Maemondo M, Inoue A, Kobayashi K, et al;
North-East Japan Study Group, West Japan Thoracic Oncology Group.
Gefitinib or chemotherapy for non-small-cell lung cancer with
mutated EGFR. N Engl J Med. 362:2380–2388. 2010.
|
|
3
|
Mitsudomi T, Morita S, Yatabe Y, et al:
West Japan Thoracic Oncology Group: Updated overall survival
results of WJTOG 3405, a randomized phase III trial comparing
gefitinib (G) with cisplatin plus docetaxel (CD) as the first-line
treatment for patients with non-small cell lung cancer harboring
mutations of the epidermal growth factor receptor (EGFR). J Clin
Oncol. 30(Suppl): 75212012.
|
|
4
|
Inoue A, Kobayashi K, Maemondo M, et al;
North-East Japan Study Group. Updated overall survival results from
a randomized phase III trial comparing gefitinib with
carboplatin-paclitaxel for chemo-naïve non-small cell lung cancer
with sensitive EGFR gene mutations (NEJ002). Ann Oncol. 24:54–59.
2013.
|
|
5
|
Okamoto T, Maruyama R, Shoji F, et al:
Long-term survivors in stage IV non-small cell lung cancer. Lung
Cancer. 47:85–91. 2005.
|
|
6
|
Satoh H, Ishikawa H, Ohara G, et al:
Long-term survivors after chemotherapy in advanced non-small cell
lung cancer. Anticancer Res. 27:4457–4460. 2007.
|
|
7
|
Dujon C, Azarian R and Petitpretz P:
Long-term survivors of advanced non-small-cell lung cancer:
characterisation and prognostic factors in a retrospective study.
Rev Mal Respir. 26:952–960. 2009.(In French).
|
|
8
|
Giroux Leprieur E, Lavole A, Ruppert AM,
et al: Factors associated with long-term survival of patients with
advanced non-small cell lung cancer. Respirology. 17:134–142.
2012.
|
|
9
|
Van Damme V, Govaerts E, Nackaerts K, et
al: Clinical factors predictive of long-term survival in advanced
non-small cell lung cancer. Lung Cancer. 79:73–76. 2013.
|
|
10
|
Hirashima T, Suzuki H, Kobayashi M, et al:
Long-term chemotherapy may prolong survival in advanced
non-small-cell lung cancer among responders to first-line
chemotherapy. Med Oncol. 29:1629–1637. 2012.
|
|
11
|
Kaira K, Takahashi T, Murakami H, et al:
Long-term survivors of more than 5 years in advanced non-small cell
lung cancer. Lung Cancer. 67:120–123. 2010.
|
|
12
|
Goldstraw P, Crowley J, Chansky K, et al;
International Association for the Study of Lung Cancer
International Staging Committe; Participating Institutions. The
IASLC Lung Cancer Staging Project: proposals for the revision of
the TNM stage groupings in the forthcoming (seventh) edition of the
TNM Classification of malignant tumours. J Thorac Oncol. 2:706–714.
2007.
|
|
13
|
Therasse P, Arbuck SG, Eisenhauer EA, et
al: New guidlines to evaluate the response to treatment in solid
tumors. European Organization for Research and Treatment of Cancer,
National Cancer Institute of the United States, National Cancer
Institute of Canada. J Natl Cancer Inst. 92:205–216. 2000.
|
|
14
|
Tamura K, Okamoto I, Kashii T, et al; West
Japan Thoracic Oncology Group. Multicentre prospective phase II
trial of gefitinib for advanced non-small cell lung cancer with
epidermal growth factor receptor mutations: results of the West
Japan Thoracic Oncology Group trial (WJTOG0403). Br J Cancer.
98:907–914. 2008.
|
|
15
|
R Development Core Team. The R Project for
Statistical Computing. 2010, http://www.r-project.org.
Accessed January 4, 2013
|
|
16
|
Yamazaki K, Sugio K, Yamanaka T, et al:
Prognostic factors in non-small cell lung cancer patients with
postoperative recurrence following third-generation chemotherapy.
Anticancer Res. 30:1311–1315. 2010.
|
|
17
|
Hotta K, Kiura K, Fujiwara Y, et al: Role
of survival post-progression in phase III trials of systemic
chemotherapy in advanced non-small-cell lung cancer: a systematic
review. PLoS One. 6:e266462011.
|