Introduction
The overall rate of brain metastasis from
gastrointestinal malignant tumors, including colorectal, gastric,
pancreatic, esophageal and gastrointestinal cancer, is reported as
3–8% (1–3). Notably, esophageal carcinomas account
for 1–5% of these brain metastases (4,5).
Neuroendocrine carcinoma of the esophagus is a rare malignant tumor
originating from the neuroendocrine cells. Depending on the degree
of differentiation, the tumors are classified as carcinoid
(well-differentiated), atypical carcinoid
(moderately-differentiated) and neuroendocrine small cell carcinoma
(poorly-differentiated). Neuroendocrine carcinomas account for
0.15–2.8% of esophageal carcinomas (6,7).
According to previous studies, the pathological types of brain
metastases originating from esophageal carcinoma are generally
squamous carcinoma in Asian countries and adenocarcinoma in Western
countries (4,5,8). The
incidence of esophageal cancer in China is high, and reports of
brain metastasis of esophageal cancer in China in the international
literature are rare. Due to the low incidence and lack of specific
clinical manifestations, brain metastases from esophageal carcinoma
usually remain undiagnosed and are treated incorrectly. Cases of
simultaneous metastases occurring in the cerebellum, brainstem and
spinal cord are extremely rare. The current study reports such a
case. Patient provided written informed consent.
Case report
Primary tumor (esophageal cancer)
diagnosis and treatment
A 74-year-old male presented to the Zhejiang Cancer
Hospital (Hangzhou, China) with complaints of swallowing
difficulties that had been apparent for three months. Gastroscopy
revealed the presence of two nodules of 1.5 cm in diameter, with
deep ulceration and eruption of the surrounding esophageal mucous
membrane, at 22–25 and 27–35 cm from the incisor teeth.
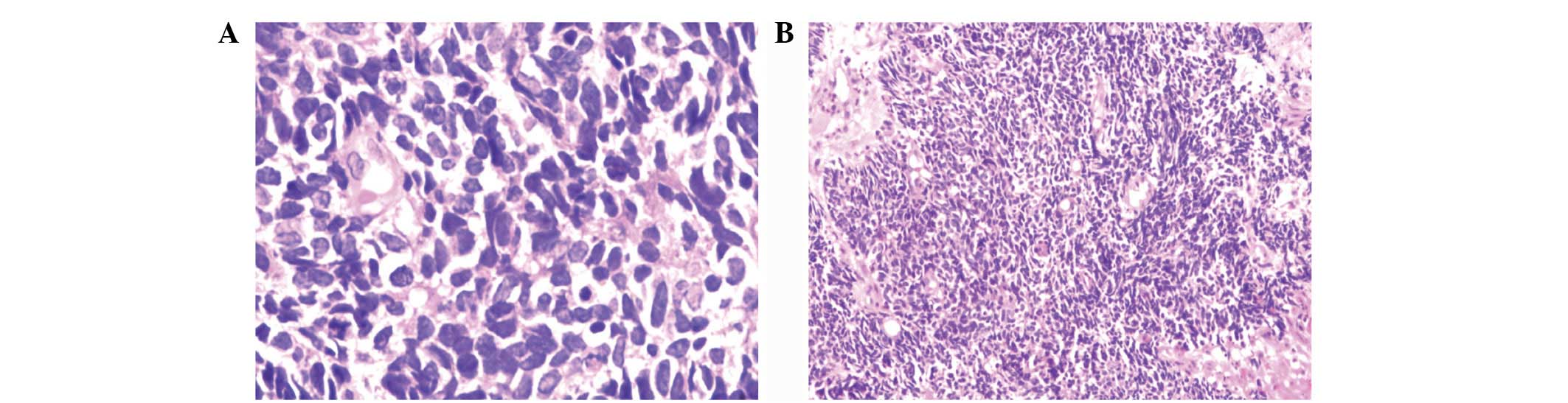
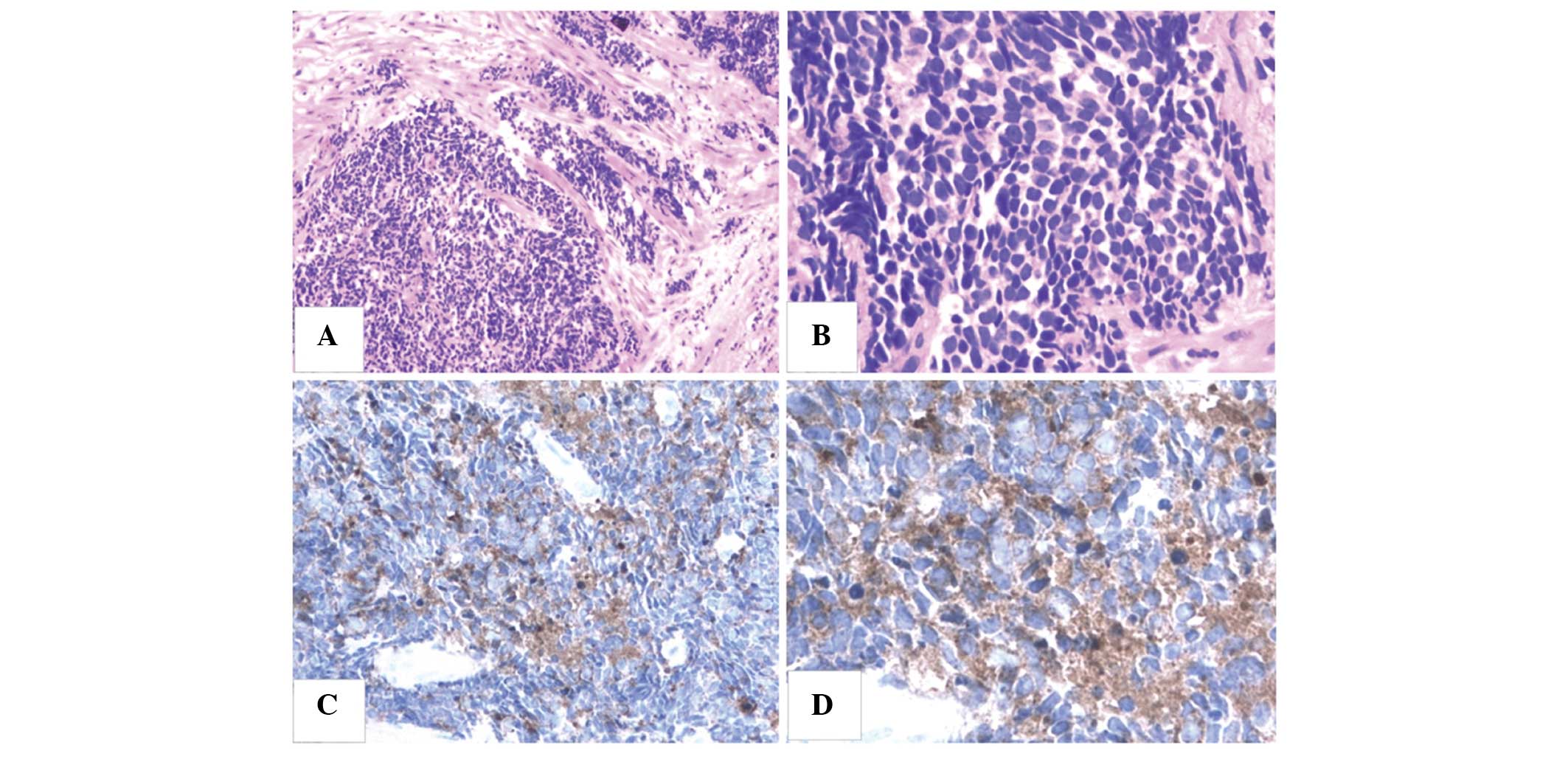
Pathological evaluation indicated malignant epithelial tumors
described as poorly-differentiated neuroendocrine carcinoma or
basal cell squamous carcinoma (Fig.
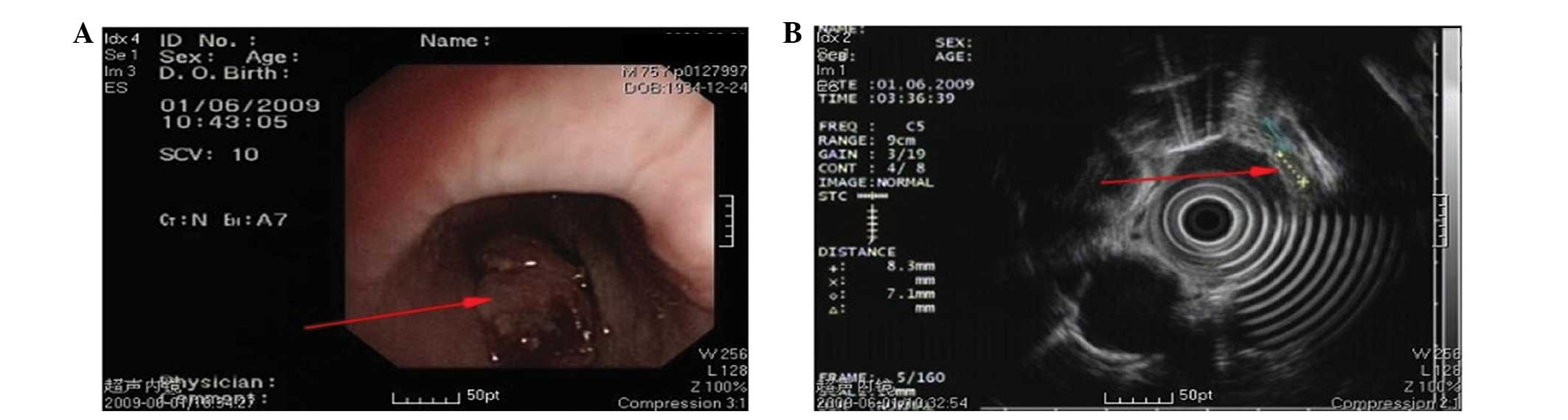
1). Endoscopic ultrasound revealed damage to five layers of the
esophageal wall, with lesions invading the outer membrane and
muscular layer; multiple enlarged lymph nodes were also observed
(Fig. 2). Ultrasound revealed
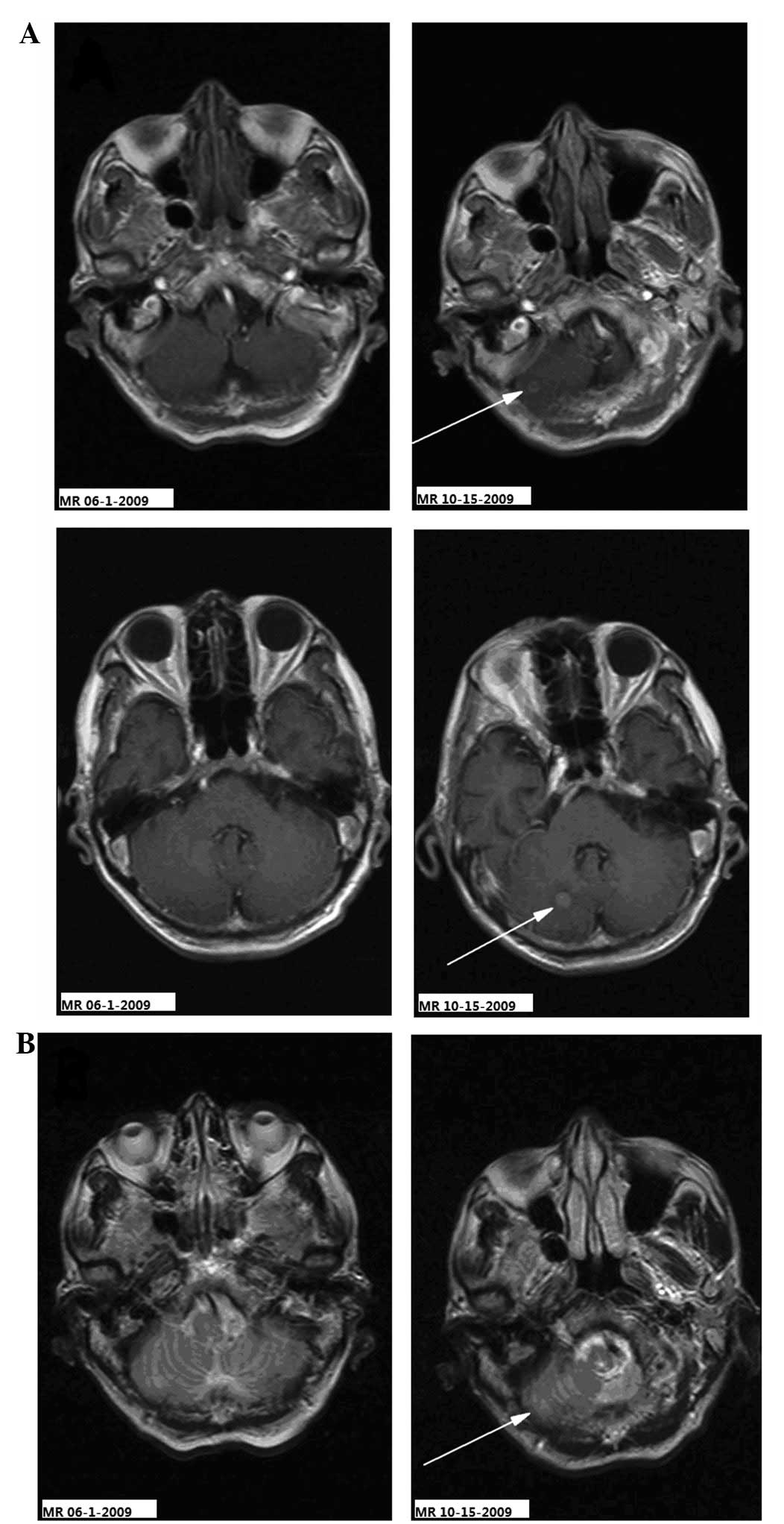
supraclavicular lymph node metastasis. No abnormal signals were
observed by contrast-enhanced magnetic resonance imaging (MRI) of
the brain and via whole body bone imaging (Figs. 3–5).
The diagnosis was of esophageal carcinoma with supraclavicular
metastasis. Radiotherapy was administered to the esophageal lesions
and supraclavicular area, with a total dose of 64 Gy/32 fractions
of 2 Gy per fraction. The swallowing difficulty symptom improved,
and a follow-up enhanced chest computed tomography (CT) scan
revealed slight thickening of the upper segment of the esophagus
following radiotherapy.
Diagnosis of central nervous system
metastasis and treatment
The patient complained of constant occipital
headache with slight pain in the bilateral upper arm and fatigue,
but no nausea or vomiting, for 2.7 months after the treatment of
the primary lesion. The Karnofsky performance status (KPS) score
was 70 and no pathological reflexes were observed on physical
examination. Brain MRI revealed two nodules (0.35 and 0.8 cm in
diameter) in the right cerebellar hemisphere. The signal was
slightly lower in the unenhanced T1-weighted images and slightly
higher in the T2-weighted images. The lesions showed clear
ring-like, uniform hardening on signal-enhanced scans, and mild
edema was observed surrounding the larger lesion. The diagnosis was
of a cerebellar metastasis from the esophageal cancer following
treatment (Figs. 3–5). Following whole brain radiotherapy of a
total dose of 30 Gy/20 fractions of 1.5 Gy per fraction by
hyperfractionation (two fractions per day), the patient’s occipital
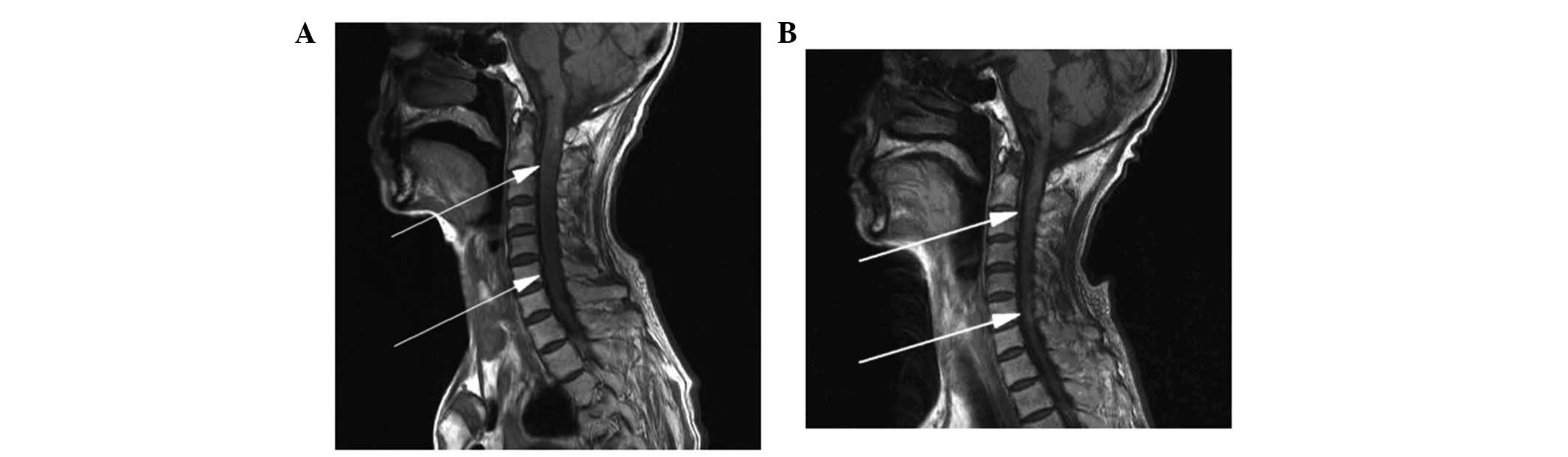
headache was relieved, however, the neck numbness was aggravated. A
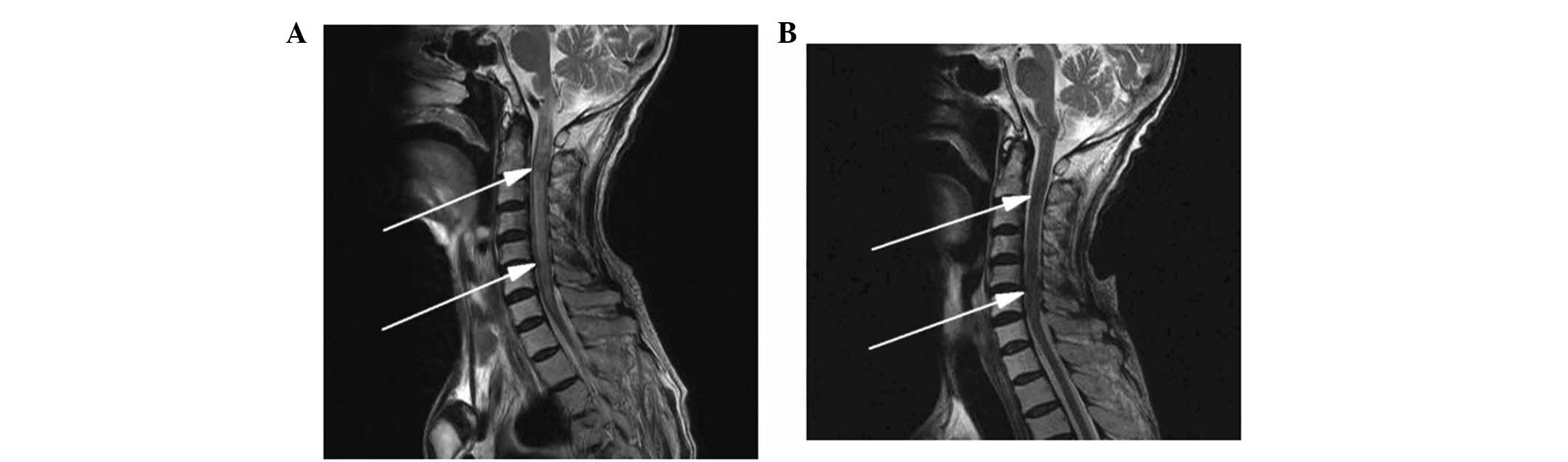
cervical MRI examination revealed enlargement of the medulla
oblongata and spinal cord, with slightly increased T1 and T2
signals. A signal-enhanced scan showed heterogeneous enhancement in
a region considered to be the metastasis. The patient continued
with the planned whole brain radiotherapy, together with nedaplatin
chemotherapy (40 mg on days one to three of the radiotherapy
period). At the end of the first period of chemotherapy, the
patient’s occipital headaches were alleviated and the neck numbness
was markedly improved. One month later, the patient’s head and neck
symptoms had further improved and a neck MRI revealed that the
abnormal signal foci in the medulla oblongata and cervical cord had
also markedly improved (Figs. 6 and
7). To strengthen the effects of
the treatment, the patient was treated with palliative radiotherapy
(total dose of 26 Gy/13 fractions of 2 Gy per fraction) to the
cervical spinal cord. Following treatment, the patient’s head and
neck pain and numbness symptoms had almost disappeared. The patient
was discharged with oral etoposide (VP-16) capsules (50 mg daily
for 20 days).
Prognosis of patient and follow-up
Once discharged, the patient refused to return to
the hospital for further treatment and follow-up. The occipital
headache symptoms recurred, and the patient’s condition gradually
deteriorated. The patient succumbed to systemic organ failure on
April 16, 2010, six months after the diagnosis of brain
metastasis.
Discussion
A limitation of this case was the lack of autopsy
tissue pathology and cerebrospinal fluid cytology to support the
diagnosis. A review of the literature on the brain metastasis of
esophageal cancer found that, with the exception of cases that
underwent surgical resection of the brain metastatic lesions, the
patients were treated with chemotherapy and diagnosed by imaging
(4–6,8–12).
Evidence from MRI and improvements in the clinical symptoms of the
patient following radiotherapy determine the diagnosis of
cerebellar, brainstem or spinal cord metastasis of esophageal
cancer. The most common clinical signs and chief complaints for
brain metastases of esophageal carcinoma are weakness (58%),
headache (28%), epilepsy (22%) and cerebellar dysfunction (14%)
(8).
In the present case, following the treatment of the
primary esophageal tumor, the main positive central nervous system
signs were fatigue, headaches and neck pain. Takeshima et al
(11) reported on the
characteristic cyst structure of metastatic brain tumors of
squamous cell esophageal carcinoma. On T1-weighted images,
following the administration of the gadolinium with
diethylenetriaminepentaacetic acid contrast agent, the majority of
lesions appear as thin-walled cysts with slightly higher signals
than those of the brain tissues. Signals from the interior of the
cysts are similar to those of the cerebrospinal fluid, however, the
walls of the cystic tumors exhibit high signal reflection (11). In the present case, the brain MRI
did not exhibit thin-walled cysts, but showed the appearance of
solid nodules. Esophageal cancers may become necrotic,
characterized by rapid growth, solid tumors that have an inadequate
blood supply and the development of focal necrosis in the center of
the tumor, resulting in a cyst-like appearance. Prior to the end of
the 20th century, brain metastases of esophageal carcinoma were
confirmed primarily by pathological examination at autopsy. Central
nervous system metastasis of esophageal cancer is also extremely
rare. Ogawa et al reported brain metastasis in 36 (1.4%) of
2,554 esophageal cancer patients (8). Gabrielsen et al (4) observed that the incidence of brain
metastasis of esophageal cancer was 3.6% (4), and Weinberg et al (5) reported 27 cases of brain metastasis
(1.7%) in 1,588 esophageal cancer patients. There are no literature
reports of brainstem and spinal cord metastasis of esophageal
cancer.
Due to the low incidence of brain metastasis, there
is generally no requirement for an MRI examination of the brain and
cervical spine of patients with esophageal cancer; Japanese studies
have even opposed the routine brain CT examination of patients with
esophageal cancer (4). Ogawa et
al (8) suggested that with the
rapid development of medical imaging technology, particularly the
application of MR and the use of enhanced contrast agents in
neuroimaging, faster and earlier detection of brain metastasis of
esophageal carcinoma has become possible (5,8,9).
Currently, for the detection and evaluation of tumor lesions, MRI
is superior to CT. Therefore, the prompt use of MRI is necessary
for the early detection of brainstem and spinal cord metastatic
lesions. Certain studies have considered the use of adjuvant
chemotherapy following the resection of esophageal carcinoma to
increase the risk of brain metastasis (6,12).
It has been confirmed that the distant metastasis of
esophageal cancer depends predominantly on the lymphatic and blood
systems. The most common pathway for brain metastasis of esophageal
cancer is hematogenous dissemination through the arterial
circulation. In 1940, the Batson venous plexus was proposed as a
pathway for the brain metastasis of esophageal carcinoma (13). However, the role of the vertebral
venous system in the brain metastasis of esophageal cancers is
supported by a more recent study (8). The present case may be more
illustrative of the importance of the vertebral vascular system for
cerebellar, brainstem and spinal cord metastases from esophageal
cancer, as all three regions are anatomically associated with the
same vertebral vascular system, which is distinct from the venous
system of the thoracic and lumbar spine and brain.
Brain metastases are often treated with multiple
therapies, including surgery, radiation and chemotherapy. Complete
removal of the lesions is the goal of surgical treatment and may
improve survival rates. However, this generally only applies to
patients with a high KPS score or to those with single, solitary
tumors (8,10).
Ogawa et al (8) reported that patients treated with
surgery and radiation treatment have a median survival time of 9.6
months, while patients receiving only radiation treatment have a
median survival time of only 1.8 months. In the present case, due
to multiple metastases to the cerebellum, brainstem and spinal
cord, a combined treatment of local irradiation and chemotherapy
was used. The symptoms were significantly improved following
treatment, with a survival time of 3.9 months.
Brain metastasis of esophageal cancer may also
involve the brainstem and spinal cord, for which local and
comprehensive treatments may improve the efficacy of therapy and
therefore prolong survival time.
Acknowledgements
This study was supported by grants from the Zhejiang
Province Science and Technology Project of Traditional Chinese
Medicine (grant no. 2011ZB017) and the Talent Project of Medical
and Health Sciences Fund of Zhejiang Province (grant no.
2012RCB005).
References
|
1
|
Salvati M, Cervoni L, Paolini S and
Delfini R: Solitary cerebral metastases from intestinal carcinoma.
Acta Neurochir (Wien). 133:181–183. 1995.
|
|
2
|
Flickinger JC, Kondziolka D, Lunsford LD,
et al: A multi-institutional experience with stereotactic
radiosurgery for solitary brain metastasis. Int J Radiat Oncol Biol
Phys. 28:797–802. 1994.
|
|
3
|
Hammoud MA, McCutcheon IE, Elsouki R,
Schoppa D and Patt YZ: Colorectal carcinoma and brain metastasis:
distribution, treatment, and survival. Ann Surg Oncol. 3:453–463.
1996.
|
|
4
|
Gabrielsen TO, Eldevik OP, Orringer MB and
Marshall BL: Esophageal carcinoma metastatic to the brain: clinical
value and cost-effectiveness of routine enhanced head CT before
esophagectomy. AJNR Am J Neuroradiol. 16:1915–1921. 1995.
|
|
5
|
Weinberg JS, Suki D, Hanbali F, Cohen ZR,
Lenzi R and Sawaya R: Metastasis of esophageal carcinoma to the
brain. Cancer. 98:1925–1933. 2003.
|
|
6
|
Pantvaidya GH, Pramesh CS, Deshpande MS,
Jambhekar NA, Sharma S and Deshpande RK: Small cell carcinoma of
the esophagus: the Tata Memorial Hospital experience. Ann Thorac
Surg. 74:1924–1927. 2002.
|
|
7
|
Linan Padilla A, Milla Sabas A, Abad
Zamora JM, et al: Oat-cell carcinoma of the esophagus: presentation
of two cases and literature review. Rev Esp Enferm Dig. 99:415–419.
2007.
|
|
8
|
Ogawa K, Toita T, Sueyama H, et al: Brain
metastases from esophageal carcinoma: natural history, prognostic
factors, and outcome. Cancer. 94:759–764. 2002.
|
|
9
|
Khuntia D, Sajja R, Chidel MA, et al:
Factors associated with improved survival in patients with brain
metastases from esophageal cancer: a retrospective review. Technol
Cancer Res Treat. 2:267–272. 2003.
|
|
10
|
Koga H, Mukawa J, Miyagi K, et al:
Treatment of metastatic brain tumor from esophageal
carcinoma--report of four cases. Neurol Med Chir (Tokyo).
31:518–522. 1991.
|
|
11
|
Takeshima H, Kuratsu J, Nishi T, et al:
Metastatic brain tumours from oesophageal carcinoma: neuro-imaging
and clinicopathological characteristics in Japanese patients. Acta
Neurochir (Wien). 143:31–36. 2001.
|
|
12
|
Kawabata R, Doki Y, Ishikawa O, et al:
Frequent brain metastasis after chemotherapy and surgery for
advanced esophageal cancers. Hepatogastroenterology. 54:1043–1048.
2007.
|
|
13
|
Batson OV: The function of the vertebral
veins and their role in the spread of metastases. Ann Surg.
112:138–149. 1940.
|